Abstract
Objective
This study examines whether patient-reported indicators of a quality medical home are associated with measures of health among Latino children in low-income families.
Data Sources
Data on 3,258 children ages 2–18 years are from a cross-sectional survey of parents of children affiliated with California's Healthy Kids insurance.
Study Design
Medical home quality was assessed using the Parents' Perception of Primary Care and was associated with health-related quality of life (HRQOL) overall and in four domains (physical, emotional, social, and school/daycare) and four measures of school engagement.
Principal Findings
A higher total medical home score was associated with a higher total Pediatric Quality of Life Inventory score and scores in four subdomains (total beta [B]=1.77, physical B = 1.71, social B = 1.36, emotional B = 2.22, and school/daycare B = 1.69, all p<0.001). It was also associated with missing fewer than three school days due to illness (odds ratio [OR]=1.12, 95 percent confidence intervals [CI]: 1.05, 1.19), excellent/above average school performance overall (OR=1.10, 95 percent CI: 1.03, 1.17) and performance in reading (OR=1.13, 95 percent CI: 1.06, 1.20) and math (OR=1.10, 95 percent CI: 1.03, 1.16).
Conclusions
Patient-reported medical home quality indicators are favorably associated with HRQOL and measures of school engagement among Latino children in low-income families.
Keywords: Primary care, health-related quality of life, access to care
The provision of a medical home for children is now a major focus of pediatric health care practice and policy, and it is promoted in the recent major health care reforms contained in the Patient Protection and Affordable Care Act of 2010. The medical home is an approach to the delivery of primary care that facilitates partnerships between patients and physicians, embraced by most major physician organizations including the American Academy of Pediatrics (AAP) (Kellerman and Kirk 2007). In describing the medical home, the AAP emphasizes seven defining features, specifying that care should be accessible, continuous, comprehensive, coordinated, family-centered, compassionate, and culturally effective (Medical Home Initiatives for Children with Special Health Needs Project Advisory Committee 2002). A medical home is anticipated to improve the quality of care a patient receives, helping improve the health of the patient over time.
Some evidence exists for the benefits of certain medical home features. For children, better primary care access and continuity are linked with greater receipt of preventive care (Starfield and Shi 2004; Zuckerman et al. 2004) and fewer emergency department visits (Christakis et al. 2001; Bermudez and Baker 2005). In general, there is limited empirical data linking these and other features of a medical home with measures of children's health. Among school-age children with asthma, reports of medical home quality have been associated with some aspects of engagement in school and after-school activity participation (e.g., exercising regularly, etc.) (Stevens, Pickering, and Laqui 2010). In part, this may be due to the difficult task of observing an effect of primary care on individual health, because most children are healthy and substantial time may be required for the benefits to manifest. Moreover, most data sources available to evaluate primary care collect only global health measures (e.g., general health status) that may not be sufficiently sensitive to changes in clinical care, or proxy health measures too rare for most children (e.g., hospitalizations) (National Research Council and Institute of Medicine 2004).
Needed are evaluations of the medical home concept using child health measures that are able to capture a wider range of aspects of health and are potentially more responsive to changes in clinical care, and the use of proxy health measures that reflect more of the daily experiences of children affected by changes in health (e.g., school participation and engagement measures). Measures of health-related quality of life (HRQOL) are becoming preferred to global health measures in health services research and clinical trials because they examine functioning in multiple aspects of life (e.g., physical, emotional, social) and arguably offer a more complete view of child health than global measures (e.g., general health status), disease parameters, or physicians' assessment of disease states alone (Patrick and Deyo 1989; Spieth and Harris 1996; Kaplan 2001).
The major pediatric HRQOL tools also have a body of literature accumulating to show that they effectively distinguish between a range of disease states, respond to changes in clinical care, and detect outcomes of intervention studies and clinical trials (Loonen, Derkx, and Otley 2001; Raat, Mohangoo, and Grootenhuis 2006; Varni and Limbers 2009). The Pediatric Quality of Life Inventory (PedsQL) used in this study, for example, has been used in a national evaluation of a chronic disease care model for children with asthma (Mangione-Smith et al. 2005), an evaluation of a family problem-solving skills training for vulnerable children with asthma (Seid et al. 2010), and a statewide evaluation of child enrollment in California's Children's Health Insurance Program (Seid et al. 2006). In these studies, the PedsQL was used to detect clinically meaningful changes in response to changes in access or processes of care, similar to the goal of the current study.
The purpose of this study is to examine whether patient-reported indicators of a quality medical home (i.e., patient experiences that are consistent with a medical home model) are associated with better health among Latino children in low-income families as measured through HRQOL that includes physical, emotional, social, and school/daycare domains of functioning. Additionally, for children of school age, we examine the relationship of parent-reported medical home quality with four measures of school engagement thought to be affected by child health (i.e., missed school days due to illness and perceived school performance). We also sought to understand whether the relationship between medical home quality and child health measures might vary according to demographic (age and language) and health care factors (frequency of utilization and setting of care), given that these factors are likely to affect experiences in using a medical home and potentially the ability of a medical home to impact health (Stevens et al. 2010). For example, older children tend to use health care less often than younger children (Elixhauser et al. 2002); thus, there may be less of an opportunity for the experience of a medical home (even if perceived to be high quality) to impact child health.
METHODS
Study Setting: Healthy Kids Programs
Data for this analysis came from a cross-sectional survey of parents of children in low-income, mostly Latino families enrolled in, or on a waiting list for, a safety-net health insurance program in California known as Healthy Kids. Healthy Kids programs are private health insurance products developed by county-based coalitions in California, known as Children's Health Initiatives. Healthy Kids programs combine private and public dollars in order to provide coverage to children ages 0–18 years up to 300 percent of the Federal Poverty Level (FPL) who are ineligible for Medicaid or the Children's Health Insurance Program, regardless of their immigration status. First formed in Santa Clara County in 2001, nearly identical Healthy Kids programs were offered in 24 of California's 58 counties (covering 70,700 children) at the time of data collection. All provided comprehensive medical, dental, and vision coverage.
The study included 21 of the 24 counties with Healthy Kids. Counties included in the study were Colusa, El Dorado, Fresno, Kern, Los Angeles, Merced, Napa, Orange, Placer, Riverside, Sacramento, San Bernardino, San Joaquin, San Luis Obispo, San Mateo, Santa Barbara, Santa Cruz, Solano, Sonoma, Yolo, and Yuba. Three other Healthy Kids programs (San Francisco, Santa Clara, and Tulare) did not participate due to insufficient staffing. The 21 participating counties accounted for 81 percent of all Healthy Kids members statewide.
Study Design
The data for this analysis are from a cross-sectional survey of parents of 4,011 children ages 0–18 years affiliated with the Healthy Kids program. Our sampling frame consisted mostly of Latino children in low-income, undocumented, and predominantly Spanish-speaking families. The sample was stratified in three groups to enable a larger evaluation of Healthy Kids programs (within which the current work was completed): established enrollees (those continuously enrolled for at least 1 year), new enrollees (those enrolled for <1 year), and children eligible for the program but placed on the waitlist due to insufficient program funding. We also stratified by county to reflect differences in program size and by child age to obtain a roughly equal distribution of children ages 0–5 and 6–18 years for our two funders (who requested sample sizes to be sufficient for separate evaluations for children 0–5 and 6–18 years). For this analysis, we only include children ages 2 years and older because the measure of HRQOL was only validated for children this age, and only asked questions about medical home for children who had at least one acute or preventive health care visit in the past year. Thus, the final analytic sample consisted of 3,258 children ages 2–18 years. The USC Office for the Protection of Research Subjects approved the study.
Data Collection
Data collection was completed between December 9, 2008 and September 21, 2009. Each Healthy Kids program provided us with contact information for members meeting our eligibility criteria. A total of 3,924 respondents participated by telephone while 87 without a telephone completed a self-administered questionnaire. Interviews and questionnaires were available and completed in Spanish (91.2 percent) and English (8.8 percent).
The most conservative calculation of the response rate is 55.6 percent, reflecting the number of respondents that completed an interview divided by the total sample listings drawn. About one-fifth of all telephone listings provided were unusable because the phone number was disconnected or otherwise incorrect. A very small proportion of families (1.4 percent of our total sampling frame) could not complete the survey in Spanish or English and were considered ineligible for participation. The response rate calculated among listings considered eligible (i.e., English or Spanish speaking) and usable (i.e., not a disconnected number) is 71.3 percent. The cooperation rate, or response among households that were reached, was 94.9 percent.
Measures
Medical Home Total Score and Its Features. We used the Parents' Perception of Primary Care (P3C) instrument to assess patient-reported indicators of medical home quality. The P3C was only administered for children who had at least one acute or preventive health care visit in the past year. The P3C has good reliability and validity in Spanish and English, and it consists of 23 items that constitute six features of primary care, mostly overlapping with the AAP definition of a medical home. These are (1) access, (2) continuity, (3) comprehensiveness, (4) contextual knowledge, (5) communication, and (6) coordination. The AAP does not specify contextual knowledge or communication as key features of a medical home, but the Institute of Medicine identifies them as features of high-quality primary care (Donaldson et al. 1996), and the measures used to assess them are similar to measures of family-centered care (an AAP-defined feature) in national surveys.
Each medical home feature was measured using two to five questions (see supporting information Appendix SA2). Responses for most questions were scored as follows: never=0, sometimes=3, often=6, almost always=9, and always=12. The two continuity questions were scored as no source of care=0, had the source for <6 months=3, 6 months to 1 year=6, 1–2 years=9, or more than 2 years=12. A summary value for each medical home feature was computed as the average of all nonmissing questions in each feature. However, at least half of the questions for a feature must have been answered in order to compute a score. Therefore, feature scores were not computed for between 0.1 percent (for continuity) and 6 percent (for coordination) of the sample. A total medical home score was calculated by averaging all nonmissing values of the six features (i.e., an average of averages).
HRQOL. We used a short form of the PedsQL version 4.0 to assess the child's HRQOL. This 15-item instrument has good reliability and validity. The PedsQL assesses four subdomains of HRQOL—physical health (five items), emotional health (four items), social functioning (three items), and school/daycare functioning (three items)—by asking parents “how much of a problem” certain issues have been with their child in the past month (e.g., walking or running). Responses were scored on a scale of 0–100 (100 is best) using response options of never=100, almost never=75, sometimes=50, often=25, and almost always=0. If more than 50 percent of the subdomain items had missing data, a missing value was generated. Otherwise, subdomain scores were computed as the mean of nonmissing items. The total PedsQL score was computed as the average of all the nonmissing items, and at least half of the PedsQL items must have been answered in order to compute a total score.
School Engagement Measures. Among school-age children (those 6 years and older), we assessed missed school days due to illness or injury and perceived school performance. First, the number of missed school days was measured for children whose parents said their child attended school, by asking, “In the past 12 months, how many days did your child miss school due to illness or injury?” Responses were dichotomized at the mean value (i.e., fewer than 3 days, and 3 or more days). Second, three questions drawn from the 2007 National Survey of Children's Health were used to assess the parent's perception of the child's school performance overall, in reading/language arts and in math (Blumberg et al. 2009). For each, parents rated the child's performance as excellent, above average, average, below average, or failing; and we dichotomized responses into “excellent/above average” versus “average, below average or failing.”
Covariates. We selected a priori a set of covariates based on prior work on disparities in child health care access, quality, and health status (Stevens and Shi 2003; Bauman, Silver, and Stein 2006; Flores and Tomany-Korman 2008). Covariates included child age, gender, race/ethnicity (Latino, White, and Asian/other), interview language (Spanish versus English), number of years living in the United States, and Healthy Kids affiliation (enrollee or waitlist). We also measured child activity limitations due to medical, behavioral, or other health issues to reflect underlying health need that is expected to strongly affect having a medical home, utilization, and child health status. Health system covariates included other insurance the child had in the past year—public (Medicaid or Children's Health Insurance Plan) and private insurance—because waitlisted children and some Healthy Kids enrollees may have had temporary safety-net insurance (e.g., emergency Medi-Cal) or they may have purchased private insurance, the setting of care (doctor's office, clinic or health center, and other setting), and number of acute health care visits in the past year. We also adjusted for county, entered as dummy variables with Los Angeles as the reference group. We did not measure income because prior work had shown that income level is quite homogenous within the program, with 86 percent of all enrollees living in families with incomes <100 percent of FPL and nearly all the remaining under 200 percent. We did not assess immigration status because most (92 percent) enrollees are noncitizens (Hill et al. 2008).
Analysis
All analyses were conducted using Stata 10. Data were weighted to be representative of the population of children affiliated with Healthy Kids in the 21 participating counties (both enrolled and waitlisted) and “survey” procedures were invoked to account for the survey design that was stratified by county, child age, and enrollments status. Descriptive statistics are presented in Table 1, with appropriate proportions, means, and standard errors.
Table 1.
Descriptive Statistics Weighted to Reflect Children in the 21 Participating Healthy Kids Programs, Ages 2 Years and Older with Any Health Care Visit in the Past Year (n = 3,258)
| % or Mean | SE | |
|---|---|---|
| Child demographics | ||
| Age in years (mean) | 8.6 | 0.10 |
| Female gender | 46.3 | 0.01 |
| Race/ethnicity | ||
| Latino | 95.9 | <0.01 |
| White, non-Latino | 1.9 | <0.01 |
| Asian, non-Latino | 1.6 | <0.01 |
| Other, non-Latino | 0.6 | <0.01 |
| Spanish language interview | 93.4 | <0.01 |
| Years lived in the U.S. (mean) | 5.5 | 0.08 |
| Health care system | ||
| Years enrolled in Healthy Kids | 2.25 | 0.07 |
| Had Medicaid/CHIP in past year | 23.0 | 0.01 |
| Had private insurance in past year | 2.7 | <0.01 |
| Has a regular source of care | 88.6 | 0.01 |
| Setting of health care | ||
| Doctor's office | 26.0 | 0.01 |
| Clinic or health center | 56.5 | 0.01 |
| Other | 17.6 | 0.01 |
| Medical home (mean, range: 0–12, 12=best) | ||
| Total score | 7.9 | 0.06 |
| Access | 7.3 | 0.08 |
| Continuity | 7.4 | 0.09 |
| Comprehensiveness | 7.5 | 0.08 |
| Contextual knowledge | 8.3 | 0.08 |
| Communication | 10.1 | 0.07 |
| Coordination | 6.7 | 0.09 |
| Child health measures | ||
| PedsQL total (mean, range 0–100, 100=best) | 78.6 | 0.38 |
| Physical (mean) | 84.0 | 0.46 |
| Social (mean) | 78.9 | 0.51 |
| Emotional (mean) | 74.7 | 0.46 |
| School/daycare (mean) | 75.4 | 0.57 |
| Activity limitation due to medical, behavioral, or other health issue | 0.03 | <0.01 |
| Missed school days in past year (mean) | 3.1 | 0.16 |
| School performance (excellent or above average) | ||
| Overall | 61.3 | 0.01 |
| Reading | 56.9 | 0.01 |
| Math | 59.2 | 0.01 |
CHIP, Children's Health Insurance Program.
Association of Medical Home with HRQOL. We conducted multivariable linear regressions to test the association of parent-reported indicators of medical home quality with the total PedsQL scale and four subdomains, controlling for the study covariates (Table 2). Separate regressions were run for the total medical home score and for the set of six medical home features, but they are presented in one table for simplicity. The coefficients presented for the study covariates are from the regression that simultaneously included the six medical home features, and they were very similar to those in the regression involving the total medical home score. Beta coefficients (B) and standard errors (SE) are presented.
Table 2.
Multiple Regression of the Relationship of Medical Home Quality with Health-Related Quality of Life, Children Ages 2 and Older (n = 3,258)
| PedsQL Total | PedsQL Physical | PedsQL Social | PedsQL Emotional | PedsQL School/Daycare | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | B | SE | |
| Medical home quality | ||||||||||
| Total score§ | 1.77‡ | 0.15 | 1.71‡ | 0.18 | 1.36‡ | 0.22 | 2.22‡ | 0.22 | 1.69‡ | 0.24 |
| Access | 0.49‡ | 0.11 | 0.44† | 0.13 | 0.62† | 0.19 | 0.34* | 0.16 | 0.67† | 0.20 |
| Continuity | 0.00 | 0.10 | 0.02 | 0.11 | −0.14 | 0.16 | 0.00 | 0.14 | 0.14 | 0.17 |
| Comprehensiveness | 0.47‡ | 0.14 | 0.47† | 0.15 | 0.07 | 0.22 | 0.72‡ | 0.20 | 0.54* | 0.24 |
| Contextual knowledge | 0.15 | 0.13 | 0.10 | 0.15 | 0.00 | 0.22 | 0.33 | 0.18 | 0.19 | 0.23 |
| Communication | 0.52† | 0.20 | 0.71† | 0.21 | 0.35 | 0.29 | 0.75† | 0.27 | 0.10 | 0.31 |
| Coordination | 0.14 | 0.11 | 0.03 | 0.12 | 0.41* | 0.17 | 0.07 | 0.14 | 0.09 | 0.20 |
| Child/family demographics | ||||||||||
| Age in years | −0.25* | 0.12 | −0.28* | 0.13 | 0.17 | 0.19 | −0.41* | 0.17 | −0.38 | 0.20 |
| Female gender | 1.25 | 0.64 | −0.14 | 0.70 | −0.67 | 0.98 | 1.31 | 0.88 | 5.39‡ | 1.04 |
| Race/ethnicity (versus Latino) | ||||||||||
| White (non-Latino) | 1.61 | 1.97 | 0.24 | 1.90 | 5.92* | 2.59 | 0.73 | 3.12 | 2.14 | 3.12 |
| Asian/Other (non-Latino) | −0.92 | 1.76 | −1.11 | 2.05 | −2.10 | 2.84 | 0.97 | 2.79 | −1.17 | 3.39 |
| Spanish language interview | −4.23‡ | 1.18 | −5.47‡ | 1.25 | −5.89† | 1.92 | 0.00 | 2.00 | −6.00† | 2.01 |
| Years lived in the U.S. | 0.00 | 0.15 | 0.02 | 0.15 | 0.25 | 0.23 | 0.09 | 0.21 | −0.40 | 0.23 |
| Has activity limitation | −15.31‡ | 2.38 | −24.71‡ | 3.72 | −11.58† | 3.56 | −10.07† | 2.90 | −11.22† | 4.16 |
| Health care system factors | ||||||||||
| Acute visits in past year | −0.74‡ | 0.14 | −0.77‡ | 0.16 | −1.04‡ | 0.23 | −0.49† | 0.18 | −0.77‡ | 0.21 |
| Preventive visits in past year | −0.36 | 0.26 | −0.57 | 0.36 | −0.45 | 0.37 | −0.10 | 0.34 | −0.31 | 0.37 |
| Setting of health care (versus doc) | ||||||||||
| Clinic or health center | 0.40 | 0.80 | 0.19 | 0.88 | 1.5 | 1.19 | 0.21 | 1.09 | 0.11 | 1.30 |
| Other setting | 3.56‡ | 1.09 | 4.55‡ | 1.22 | 3.24 | 1.69 | 3.65* | 1.53 | 2.33 | 1.73 |
| Years in Healthy Kids | −0.15 | 0.22 | −0.06 | 0.25 | −0.14 | 0.34 | −0.30 | 0.31 | −0.03 | 0.36 |
| Had public ins. in past year | −1.14 | 0.75 | −0.78 | 0.83 | −1.70 | 1.26 | −1.53 | 0.98 | −0.33 | 1.18 |
| Had private ins. in past year | −3.69* | 1.78 | −3.95 | 2.78 | −5.09 | 2.97 | −2.45 | 2.04 | −4.32 | 2.58 |
Note. All models are additionally adjusted for the 21 counties, but the estimates are not shown here. All statistically significant results at p<.05 are bolded for ease of identification.
p<.05,
p<0.01,
p<0.001.
A regression model was created for the total medical home score separately from a regression model that for the five medical home features, but for simplicity of presentation, the total medical home score is presented in the same table. The odds ratios that are presented for the covariates in this table are only for the regression model for the five medical home features (not the total medical home score).
B, beta coefficient, SE, standard error.
Association of Medical Home with School Engagement. For children of school age (6 years and older), multivariable logistic regressions were carried out to predict having fewer than three missed school days in the past year and excellent or above average school performance in three areas (Table 3), controlling for the study covariates. As before, the coefficients presented for the study covariates are from the regression that simultaneously included six medical home features. Odds ratios (OR) and 95 percent confidence intervals (CI) are presented.
Table 3.
Multiple Regression of the Relationship of Medical Home Quality with Missed School Days and School Performance, Children Ages 6 and Older (n = 1,845)
| Missed<3 School Days Due to Illness/Injury in Past Year | Overall School Performance (Excellent/Above Average) | Reading Performance (Excellent/Above Average) | Math Performance (Excellent/Above Average) | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Medical home quality | ||||||||
| Total score* | 1.12 | 1.05–1.19 | 1.10 | 1.03–1.17 | 1.13 | 1.06–1.20 | 1.10 | 1.03–1.16 |
| Access | 1.05 | 1.00–1.10 | 1.06 | 1.01–1.12 | 1.11 | 1.06–1.17 | 1.05 | 1.00–1.11 |
| Continuity | 1.03 | 0.98–1.08 | 1.02 | 0.97–1.06 | 1.00 | 0.95–1.04 | 0.99 | 0.94–1.04 |
| Comprehensiveness | 1.07 | 1.00–1.14 | 1.03 | 0.97–1.10 | 1.04 | 0.98–1.10 | 1.03 | 0.97–1.09 |
| Contextual knowledge | 0.99 | 0.93–1.05 | 1.01 | 0.95–1.08 | 1.02 | 0.96–1.08 | 0.98 | 0.93–1.04 |
| Communication | 1.02 | 0.95–1.09 | 0.98 | 0.90–1.06 | 0.96 | 0.89–1.04 | 1.03 | 0.96–1.11 |
| Coordination | 0.98 | 0.93–1.04 | 1.01 | 0.95–1.06 | 1.01 | 0.96–1.06 | 1.02 | 0.97–1.07 |
| Child/family demographics | ||||||||
| Age in years | 1.01 | 0.95–1.06 | 0.94 | 0.90–0.99 | 0.99 | 0.95–1.04 | 0.93 | 0.88–0.97 |
| Female gender | 1.04 | 0.78–1.39 | 1.41 | 1.07–1.87 | 1.54 | 1.17–2.04 | 0.91 | 0.68–1.20 |
| Race/ethnicity (versus Latino) | ||||||||
| White (non-Latino) | 4.98 | 0.91–27.2 | 4.10 | 0.58–28.93 | 1.47 | 0.22–10.02 | 1.96 | 0.17–22.48 |
| Asian/Other (non-Latino) | 1.54 | 0.25–9.38 | 3.51 | 0.78–15.86 | 2.48 | 0.48–12.73 | 3.74 | 0.54–26.08 |
| Spanish language interview | 1.64 | 0.40–6.69 | 1.01 | 0.30–3.37 | 0.68 | 0.17–2.67 | 1.64 | 0.38–7.10 |
| Years lived in the U.S. | 0.98 | 0.93–1.03 | 0.98 | 0.93–1.03 | 1.03 | 0.98–1.08 | 0.99 | 0.94–1.04 |
| Has activity limitation | 0.22 | 0.10–0.52 | 0.31 | 0.12–0.81 | 0.54 | 0.20–1.49 | 0.64 | 0.27–1.49 |
| Health care system factors | ||||||||
| Acute visits in past year | 0.80 | 0.73–0.88 | 0.99 | 0.95–1.04 | 0.97 | 0.92–1.02 | 0.98 | 0.92–1.03 |
| Preventive visits in past year | 0.98 | 0.85–1.14 | 0.99 | 0.88–1.13 | 0.98 | 0.86–1.10 | 1.11 | 0.97–1.26 |
| Setting of health care (versus doc) | ||||||||
| Clinic or health center | 0.82 | 0.57–1.17 | 1.20 | 0.85–1.69 | 0.89 | 0.63–1.27 | 1.01 | 0.72–1.42 |
| Other setting | 1.20 | 0.75–1.94 | 1.16 | 0.73–1.84 | 1.08 | 0.67–1.74 | 0.84 | 0.53–1.33 |
| Years in Healthy Kids | 1.08 | 0.98–1.18 | 1.09 | 0.99–1.19 | 1.09 | 1.01–1.20 | 1.05 | 0.96–1.15 |
| Had public ins. in past year | 0.85 | 0.60–1.20 | 1.07 | 0.76–1.51 | 0.78 | 0.56–1.09 | 1.01 | 0.72–1.41 |
| Had private ins. in past year | 0.52 | 0.23–1.18 | 0.93 | 0.43–2.01 | 0.80 | 0.37–1.77 | 0.88 | 0.40–1.93 |
Note. All models are additionally adjusted for the 21 counties, but the estimates are not shown here. All statistically significant results at p<.05 are bolded for ease of identification.
A regression model was created for the total medical home score separately from a regression model that for the five medical home features, but for simplicity of presentation, the total medical home score is presented in the same table. The odds ratios that are presented for the covariates in this table are only for the regression model for the five medical home features (not the total medical home score).
B, beta coefficient, SE, standard error.
Lastly, we explored whether the relationship between medical home quality and child health held across selected population subgroups (child age, interview language, Healthy Kids enrollment status, the setting of the child's regular source of care, and number of acute visits in the past year). We conducted a final set of five multivariable linear regressions predicting the total PedsQL score, adjusting for the study covariates, each including an interaction term between the total medical home score and the subpopulation group of interest. Beta coefficients for total medical home quality variable for each population subgroup are presented in Figure 1, along with 95 percent CI. P-values for each interaction term between medical home quality and the subpopulation group are also presented.
Figure 1.
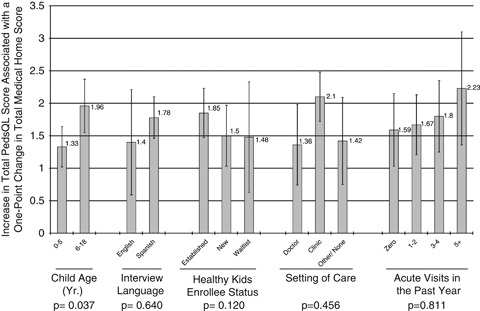
Stratified Analysis of Total Medical Home Quality Score on Pediatric Quality of Life Inventory (PedsQL) Total Score
Note: Values on the y-axis are regression beta coefficients for the interaction term of total medical home quality with each of the population subgroups. Results are adjusted for all of the study covariates and county.
RESULTS
Table 1 shows that the majority of children were of Latino race/ethnicity (95.9 percent) and had a regular source of care (88.6 percent). Medical home scores for the children ranged between 7 and 10 with contextual knowledge (8.3) and communication ranking the highest (10.1). The PedsQL total mean was substantial (78.6) and overall mean scores for physical, mental, social, and emotional health ranged from 74 to 84. Missed school days in the past year averaged 3.1 and school performance that was considered to be “excellent” or “above average” had an overall mean of 61.3, with individual subject means for reading (56.9) and math (59.2).
Table 2 shows that after adjustment for the study covariates, higher total medical home quality scores were associated with higher total PedsQL scores and for all four subdomains of HRQOL (total B = 1.77, physical B = 1.71, social B = 1.36, emotional B = 2.22, and school/daycare B = 1.69, all p<0.001). Additionally, the medical home access feature was positively associated with all PedsQL measures (total B = 0.49, p<0.001; physical B = 0.44, p<0.01; social B = 0.62, p<.01; emotional B = 0.34, p<.05; and school/daycare B = 0.67, p<0.01). Comprehensiveness was positively associated with all PedsQL domains except social functioning, and communication with three PedsQL domains. Among the covariates, having an activity limitation and a higher number of acute visits was associated with a lower PedsQL score for every measure.
Table 3 shows that the total medical home quality score is positively associated with all four school-related measures, which include missing less than three school days due to illness or injury in the past year (OR=1.12, 95 percent CI: 1.05, 1.19), excellent or above average overall school performance (OR=1.10, 95 percent CI: 1.03, 1.17), reading (OR=1.13, 95 percent CI: 1.06, 1.20), and math (OR=1.10, 95 percent CI: 1.03, 1.16). However, few of the individual medical home features were associated with school-related measures. Medical home access was associated with higher odds of excellent or above average overall school and reading performance (OR=1.06, 95 percent CI: 1.01–1.12; OR=1.11, 95 percent CI: 1.06, 1.17). Activity limitation and acute visits in the past year were negatively associated with missing less than three school days due to illness or injury in the past year (i.e., missed more school days). Activity limitation was also negatively associated with overall school performance, and years in the Healthy Kids Program was positively associated with reading performance.
Figure 1 shows that there are very few differences in the relationship of medical home quality with total PedsQL score for the selected subpopulation groups. The only exception may be child age, where the variable created for the statistical interaction of medical home quality and child age was statistically significant (p = 0.037) both before (not shown) and after adjustment for study covariates. An examination of the CI of the regression coefficients for medical home quality on total PedsQL score for children 0–5 years versus 6–18 years does not fully confirm this interaction (because they overlap slightly), but it does suggest that stratified analyses (presented) may be important in considering the current results and in future work.
DISCUSSION
This cross-sectional study suggests that among children in low-income, mostly Latino, undocumented families, patient experiences that are consistent with a high-quality medical home were associated with a child's HRQOL and school engagement. While controlling for demographics and other factors, the medical home total score was favorably correlated with all PedsQL and school engagement measures. For example, for every one-point increase in total medical home quality score, the PedsQL total score increased by 1.77 points. Similarly, for every one-point increase in the medical home total score, the odds of missing fewer than three school days due to illness or injury in the past school year increased by 12 percent.
As a point of reference for the PedsQL, previous work has shown that 4.5 points should be considered the minimally clinically important difference. This is the smallest difference in score that parents of general pediatric patients would be able to detect in the health of their child and that might require a change in the patient's care or management (Varni et al. 2003). Thus, for medical home quality to affect a change in HRQOL that is considered minimally clinically significant, results suggest it would require a difference in the total medical home score of about 2.5 points on the 12-point scale. This reflects a relatively large change in medical home quality (of about 20 percent). To get a rough sense of scale, a recent study has shown that family practices participating in the National Demonstration Project on Practice Transformation to a Patient-Centered Medical Home increased adoption of medical home components by about 25 percent over a 2-year period (although patient assessments of quality did not change) (Jaen et al. 2010). Fully transitioning to high-quality medical homes may take much longer, as it often requires major retooling and technical assistance (Nutting et al. 2009).
Among the patient-reported indicators of medical home quality in our study, the access feature was most strongly and consistently associated with higher scores among all subdomains of the PedsQL and measures of school engagement. These findings also concur with previous research showing an association between access to primary care and child health outcomes (Starfield and Shi 2004; Seid et al. 2006; Szilagyi et al. 2006). More effort placed into this aspect of medical home provision may have the largest impact on children's health. Some ways to improve access might include adjusting business hours, locating within closer proximity to public transportation hubs to make travel to and from the office easier for low-income families, or using a scheduling system to facilitate walk-ins, such as Advanced Access (Murray and Berwick 2003; Murray et al. 2003; Ralston et al. 2009). Federally qualified community health centers, which are commonly included in the provider networks of Healthy Kids programs across the state, already offer enhanced evening or weekend hours and are usually accessible by public transportation (Shi, Stevens, and Politzer 2007). They may serve as models to improve access in other settings.
In analyses stratified by selected subpopulation characteristics, there was some indication that the relationship may be larger for children ages 6–18 years than 0–5 years. This is interesting because we had originally hypothesized that older children may not benefit as much from a quality medical home because they tend to use health services less. It is not clear why this relationship might exist. It is possible that older children who do regularly use health services tend to have more complex health problems that could might benefit more from a quality medical home. But no other interaction terms for other subgroups were found to be significant including the number of acute visits (which could reflect the level of need), so this possible age interaction effect is in need of confirmation in other work.
In 2008, the National Committee for Quality Assurance (NCQA) released standards for a recognition program called “Physician Practice Connections- Patient-Centered Medical Home,” becoming the first movement to certify primary care practices as patient-centered medical homes (NCQA 2010). As of April 2009, NCQA had recognized 416 practices with 4,358 physicians practicing in line with medical home standards, though none of which were in the Healthy Kids networks. Recognizing medical homes has the potential to promote and improve medical home quality for patients receiving care (Kilo and Wasson 2010; Rosenthal et al. 2010). It is still unclear, however, whether the NCQA process will change how individuals perceive indicators of medical home quality, as measured in this study, and there is a need to understand how well patient perceptions of quality reflect practice alignment with such standards (Hoff 2010). The P3C captures some of the medical home indicators that are reportable by patients, but other features that are included in the NCQA standards (and derived from the Joint Principles of the Patient Centered Medical Home released in 2007) may not be easily or even appropriately assessed by patients (Kellerman and Kirk 2007). These features (such as physician-directed medical practice and use of evidence-based medicine and clinical information tools) should also be evaluated for their potential contributions to child health.
There are several limitations to the study. First, the data are cross-sectional, only allowing for a demonstration of association not causation. The presence of a similar medical home “effect” in most of the subpopulations we studied (Figure 1) lends some additional validity to the results, but this does not confirm causality. The one exception is for child age where there was some indication that the relationship of medical home quality with PedsQL may be different (larger) among children ages 6–18 years than among 0–5 years. Second, the data were collected from a unique population (mostly children in low-income, Latino, undocumented, and Spanish-speaking families) and so the results may not be fully generalized to other children.
Third, features we used to assess patient-reported indicators of medical home quality align closely (but not perfectly) with the AAP medical home definition and the NCQA measures, and so does not reflect a complete measure of medical home quality. Though we do include access, continuity, comprehensiveness, and coordination, the P3C instrument used to measure medical home includes features of contextual knowledge and communication that reflect many of the same questions used to assess family-centered care, but it does not measure compassionate care or culturally effective care that are included in the AAP definition. Fourth, the P3C continuity measure, which assesses the length of a relationship with a regular source of care, is somewhat different from other continuity measures that evaluate the reliance on a single versus multiple sources of primary care. This P3C measure has been used and reported elsewhere (Seid, Stevens, and Varni 2003; Seid and Stevens 2005; Seid and Varni 2005), but it may be important for readers to note the difference in measurement.
Fifth, an element of endogeneity may exist in the results because the independent and dependent measures were reported by the same individual. For example, an individual who has a positive outlook may report positive responses on both medical home quality and the child health measures regardless of actual experiences. While we cannot rule it out, potential endogeneity is reduced somewhat by the use of more reporting type measures (e.g., how long has this been your child's source of medical care?) rather than those based on more subjective satisfaction measures (e.g., how satisfied are you with your child's source of care?). Lastly, our survey included only self-reported measures of school engagement that may be susceptible to some recall bias, though we do not expect these factors to affect the internal validity of the results.
CONCLUSION
In conclusion, this cross-sectional study preliminarily suggests that medical home quality as perceived by parents of children in low-income, mostly Latino and undocumented families is favorably related to multiple dimensions of HRQOL and measures of school engagement. Additional work involving longitudinal study designs and sensitivity analyses with other child populations is needed to assess causality and generalizability in order to evaluate the impact of medical home quality on children's health.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The data collection for this research project was funded by The California Endowment and First 5 California. All authors contributed to the design of the study, analysis and interpretation, and writing or revision of the manuscript. The authors have no conflicts of interest in this research, financial or otherwise.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2. Parents' Perceptions of Primary Care Instrument.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Bauman LJ, Silver EJ, Stein RE. “Cumulative Social Disadvantage and Child Health”. Pediatrics. 2006;117(4):1321–8. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- Bermudez D, Baker LC. “The Relationship between SCHIP Enrollment and Hospitalizations for Ambulatory Care Sensitive Conditions in California”. Journal of Health Care for the Poor and Underserved. 2005;16(1):96–110. doi: 10.1353/hpu.2005.0003. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Foster EB, Frasier AM, Skalland BJ, Nysse-Carris KL, Chowdhury SR, O'Conner KS. Vital and Health Statistics Series 1. National Center for Health Statistics; 2009. “Design and Operation of the National Survey of Children's Health, 2007.”; pp. 1–75. [PubMed] [Google Scholar]
- Christakis D, Mell L, Koepsell T, Zimmerman F, Connell F. “Association of Lower Continuity of Care with Greater Risk of Emergency Department Use and Hospitalization in Children”. Pediatrics. 2001;107(3):524–9. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- Donaldson M, Yordy K, Lohr K, Vanselow N. Primary Care: America's Health in a New Era. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- Elixhauser A, Machlin SR, Zodet MW, Chevarley FM, Patel N, McCormick MC, Simpson L. “Health Care for Children and Youth in the United States: 2001 Annual Report on Access, Utilization, Quality, and Expenditures”. Ambulatory Pediatrics. 2002;2(6):419–37. doi: 10.1367/1539-4409(2002)002<0419:hcfcay>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Flores G, Tomany-Korman SC. “Racial and Ethnic Disparities in Medical and Dental Health, Access to Care, and Use of Services in US Children”. Pediatrics. 2008;121(2):e286–98. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- Hill I, Dubay L, Kenney GM, Howell EM, Courtot B, Palmer L. “Improving Coverage and Access for Immigrant Latino Children: The Los Angeles Healthy Kids Program”. Health Affairs. 2008;27(2):550–9. doi: 10.1377/hlthaff.27.2.550. [DOI] [PubMed] [Google Scholar]
- Hoff T. “The Patient-Centered Medical Home: What We Need to Know More about”. Medical Care Research and Review. 2010;67(4):383–92. doi: 10.1177/1077558710368550. [DOI] [PubMed] [Google Scholar]
- Jaen CR, Ferrer RL, Miller WL, Palmer RF, Wood R, Davila M, Stewart EE, Crabtree BF, Nutting PA, Stange KC. “Patient Outcomes at 26 Months in the Patient-Centered Medical Home National Demonstration Project”. Annals of Family Medicine. 2010;8(suppl 1):S57–67. doi: 10.1370/afm.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan R. “Quality of Life in Children: A Health Care Policy Perspective.”. In: Koot H, Wallander J, editors. Quality of Life in Child and Adolescent Illness: Concepts, Methods, and Findings. East Sussex, UK: Brunner-Routledge; 2001. pp. 89–120. [Google Scholar]
- Kellerman R, Kirk L. “Principles of the Patient-Centered Medical Home”. American Family Physician. 2007;76(6):774–5. [PubMed] [Google Scholar]
- Kilo CM, Wasson JH. “Practice Redesign and the Patient-Centered Medical Home: History, Promises, and Challenges”. Health Affairs. 2010;29(5):773–8. doi: 10.1377/hlthaff.2010.0012. [DOI] [PubMed] [Google Scholar]
- Loonen HJ, Derkx BH, Otley AR. “Measuring Health-Related Quality of Life of Pediatric Patients”. Journal of Pediatric Gastroenterology and Nutrition. 2001;32(5):523–6. doi: 10.1097/00005176-200105000-00006. [DOI] [PubMed] [Google Scholar]
- Mangione-Smith R, Schonlau M, Chan KS, Keesey J, Rosen M, Louis TA, Keeler E. “Measuring the Effectiveness of a Collaborative for Quality Improvement in Pediatric Asthma Care: Does Implementing the Chronic Care Model Improve Processes and Outcomes of Care?”. Ambulatory Pediatrics. 2005;5(2):75–82. doi: 10.1367/A04-106R.1. [DOI] [PubMed] [Google Scholar]
- Medical Home Initiatives for Children with Special Health Needs Project Advisory Committee. “The Medical Home”. Pediatrics. 2002;110(1):184–86. [Google Scholar]
- Murray M, Berwick DM. “Advanced Access: Reducing Waiting and Delays in Primary Care”. Journal of the American Medical Association. 2003;289(8):1035–40. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- Murray M, Bodenheimer T, Rittenhouse D, Grumbach K. “Improving Timely Access to Primary Care: Case Studies of the Advanced Access Model”. JAMA. 2003;289(8):1042–6. doi: 10.1001/jama.289.8.1042. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance (NCQA) 2010. “Physician Practice Connections Patient-Centered Medical Home” [accessed March 3, 2010]. Available at http://www.ncqa.org/tabid/631/Default.aspx.
- National Research Council and Institute of Medicine. Children's Health, the Nation's Wealth: Assessing and Improving Child Health. Washington, DC: The National Academies Press; 2004. [Google Scholar]
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. “Initial Lessons from the First National Demonstration Project on Practice Transformation to a Patient-Centered Medical Home”. Annals of Family Medicine. 2009;7(3):254–60. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DL, Deyo RA. “Generic and Disease-Specific Measures in Assessing Health Status and Quality of Life”. Medical Care. 1989;27(3, suppl):S217–32. doi: 10.1097/00005650-198903001-00018. [DOI] [PubMed] [Google Scholar]
- Raat H, Mohangoo AD, Grootenhuis MA. “Pediatric Health-Related Quality of Life Questionnaires in Clinical Trials”. Current Opinion in Allergy and Clinical Immunology. 2006;6(3):180–5. doi: 10.1097/01.all.0000225157.67897.c2. [DOI] [PubMed] [Google Scholar]
- Ralston JD, Martin DP, Anderson ML, Fishman PA, Conrad DA, Larson EB, Grembowski D. “Group Health Cooperative's Transformation Toward Patient-Centered Access”. Medical Care Research and Review. 2009;66(6):703–24. doi: 10.1177/1077558709338486. [DOI] [PubMed] [Google Scholar]
- Rosenthal MB, Beckman HB, Forrest DD, Huang ES, Landon BE, Lewis S. “Will the Patient-Centered Medical Home Improve Efficiency and Reduce Costs of Care? A Measurement and Research Agenda”. Medical Care Research and Review. 2010;67(4):476–84. doi: 10.1177/1077558710368412. [DOI] [PubMed] [Google Scholar]
- Seid M, Stevens GD. “Access to Care and Children's Primary Care Experiences: Results from a Prospective Cohort Study”. Health Services Research. 2005;40(6, Part 1):1758–80. doi: 10.1111/j.1475-6773.2005.00435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seid M, Stevens GD, Varni JW. “Parents' Perceptions of Pediatric Primary Care Quality: Effects of Race/Ethnicity, Language, and Access”. Health Services Research. 2003;38(4):1009–31. doi: 10.1111/1475-6773.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seid M, Varni JW. “Measuring Primary Care for Children of Latino Farmworkers: Reliability and Validity of the Parent's Perceptions of Primary Care Measure (P3C)”. Maternal and Child Health Journal. 2005;9(1):49–57. doi: 10.1007/s10995-005-2450-8. [DOI] [PubMed] [Google Scholar]
- Seid M, Varni JW, Cummings L, Schonlau M. “The Impact of Realized Access to Care on Health-Related Quality of Life: A Two-Year Prospective Cohort Study of Children in the California State Children's Health Insurance Program”. Journal of Pediatrics. 2006;149(3):354–61. doi: 10.1016/j.jpeds.2006.04.024. [DOI] [PubMed] [Google Scholar]
- Seid M, Varni JW, Gidwani P, Gelhard LR, Slymen DJ. “Problem-Solving Skills Training for Vulnerable Families of Children with Persistent Asthma: Report of a Randomized Trial on Health-Related Quality of Life Outcomes”. Journal of Pediatric Psychology. 2010;35(10):1133–43. doi: 10.1093/jpepsy/jsp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Stevens GD, Politzer RM. “Access to Care for U.S. Health Center Patients and Patients Nationally: How Do the Most Vulnerable Populations Fare?”. Medical Care. 2007;45(3):206–13. doi: 10.1097/01.mlr.0000252160.21428.24. [DOI] [PubMed] [Google Scholar]
- Spieth LE, Harris CV. “Assessment of Health-Related Quality of Life in Children and Adolescents: An Integrative Review”. Journal of Pediatric Psychology. 1996;21(2):175–93. doi: 10.1093/jpepsy/21.2.175. [DOI] [PubMed] [Google Scholar]
- Starfield B, Shi L. “The Medical Home, Access to Care, and Insurance: A Review of Evidence”. Pediatrics. 2004;113(5, suppl):1493–8. [PubMed] [Google Scholar]
- Stevens GD, Pickering TA, Laqui SA. “Relationship of Medical Home Quality with School Engagement and After-School Participation among Children with Asthma”. Journal of Asthma. 2010;47(9):1001–10. doi: 10.1080/02770903.2010.514636. [DOI] [PubMed] [Google Scholar]
- Stevens GD, Seid M, Pickering TA, Tsai KY. “National Disparities in the Quality of a Medical Home for Children”. Maternal and Child Health Journal. 2010;14(4):580–9. doi: 10.1007/s10995-009-0454-5. [DOI] [PubMed] [Google Scholar]
- Stevens GD, Shi L. “Racial and Ethnic Disparities in the Primary Care Experiences of Children: A Review of the Literature”. Medical Care Research and Review. 2003;60(1):3–30. doi: 10.1177/1077558702250229. [DOI] [PubMed] [Google Scholar]
- Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, Bajorska A, Yoos HL. “Improved Asthma Care after Enrollment in the State Children's Health Insurance Program in New York”. Pediatrics. 2006;117(2):486–96. doi: 10.1542/peds.2005-0340. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Seid M, Skarr D. “The PedsQL 4.0 as a Pediatric Population Health Measure: Feasibility, Reliability, and Validity”. Ambulatory Pediatrics. 2003;3(6):329–41. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Varni JW, Limbers CA. “The Pediatric Quality of Life Inventory: Measuring Pediatric Health-Related Quality of Life from the Perspective of Children and Their Parents”. Pediatric Clinics of North America. 2009;56(4):843–63. doi: 10.1016/j.pcl.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Zuckerman B, Stevens GD, Inkelas M, Halfon N. “Prevalence and Correlates of High-Quality Basic Pediatric Preventive Care”. Pediatrics. 2004;114(6):1522–9. doi: 10.1542/peds.2004-0635. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


