Abstract
BACKGROUND:
With increasing knowledge of chronic pain, clinicians have attempted to assess chronic pain patients with lengthy assessment tools.
OBJECTIVES:
To describe the functional and emotional status of patients presenting to a tertiary care pain clinic; to assess the reliability and validity of a diagnostic classification system for chronic pain patients modelled after the Multidimensional Pain Inventory; to provide psychometric data on a modified Comprehensive Pain Evaluation Questionnaire (CPEQ); and to evaluate the relationship between the modified CPEQ construct scores and clusters with Diagnostic and Statistical Manual, Fourth Edition – Text Revision Pain Disorder diagnoses.
METHODS:
Data on 300 new patients over the course of nine months were collected using standardized assessment procedures plus a modified CPEQ at the Comprehensive Pain Program, Toronto Western Hospital, Toronto, Ontario.
RESULTS:
Cluster analysis of the modified CPEQ revealed three patient profiles, labelled Adaptive Copers, Dysfunctional, and Interpersonally Distressed, which closely resembled those previously reported. The distribution of modified CPEQ construct T scores across profile subtypes was similar to that previously reported for the original CPEQ. A novel finding was that of a strong relationship between the modified CPEQ clusters and constructs with Diagnostic and Statistical Manual, Fourth Edition – Text Revision Pain Disorder diagnoses.
DISCUSSION AND CONCLUSIONS:
The CPEQ, either the original or modified version, yields reproducible results consistent with the results of other studies. This technique may usefully classify chronic pain patients, but more work is needed to determine the meaning of the CPEQ clusters, what psychological or biomedical variables are associated with CPEQ constructs or clusters, and whether this instrument may assist in treatment planning or predict response to treatment.
Keywords: Chronic pain, Comprehensive Pain Evaluation Questionnaire, DSM-IV Pain Disorder
Abstract
HISTORIQUE :
Les cliniciens, qui connaissent de mieux en mieux la douleur chronique, ont tenté d’évaluer les patients ayant des douleurs chroniques au moyen de longs outils d’évaluation
OBJECTIFS :
Décrire l’état fonctionnel et affectif des patients qui consultent à une clinique de la douleur chronique de soins tertiaires, évaluer la fiabilité et la validité d’un système de classement diagnostique des patients atteints de douleur chronique inspiré de l’inventaire multidimensionnel de la douleur, fournir des données psychométriques sur un questionnaire d’évaluation détaillée de la douleur (QÉDD) modifié et évaluer le lien entre les indices et les grappes de construits du QÉDD et les diagnostics de troubles de la douleur du Manuel diagnostique et statistique des troubles mentaux, Quatrième édition – Révision textuelle.
MÉTHODOLOGIE :
Les chercheurs ont amassé des données sur 300 nouveaux patients pendant une période de neuf mois, au moyen de démarches d’évaluation standardisées ainsi que d’un QÉDD modifié, dans le cadre du programme détaillé de la douleur du Toronto Western Hospital deToronto, en Ontario.
RÉSULTATS :
L’analyse par grappes du QÉDD modifié a permis de dégager trois profils de patients, soit les résilients, les dysfonctionnels et les personnes en détresse interpersonnelle, qui ressemblent étroitement à ceux déclarés auparavant. La répartition des indices T de construits du QÉDD modifié entre les sous-types de profils était similaire à ceux déclarés auparavant à l’aide du QÉDD original. Selon une nouvelle observation, il existait un lien solide entre les grappes et les construits du QÉDD modifié et les diagnostics de troubles de la douleur du Manuel diagnostique et statistique des troubles mentaux, Quatrième édition – Révision textuelle.
EXPOSÉ ET CONCLUSIONS :
Le QÉDD, dans sa version originale ou modifiée, suscite des résultats reproductibles qui sont conformes aux résultats d’autres études. Cette technique peut être utile pour classer les patients atteints de douleur chronique, mais d’autres travaux s’imposent pour déterminer la signification des grappes du QÉDD, les variables psychologiques ou biomédicales qui s’associent aux construits ou aux grappes du QÉDD et si cet instrument peut contribuer à planifier le traitement ou à prédire la réponse au traitement.
With an increasing understanding of chronic pain as a complex biopsychosocial phenomenon, investigators and clinicians have attempted to assess chronic pain patients with multiple and often lengthy assessment tools. Although the use of these tools leads to a more comprehensive assessment, it may be cumbersome and time consuming, and many pain clinics do not have the resources for such assessment.
The Comprehensive Pain Evaluation Questionnaire (CPEQ) (1) was designed as a brief inventory that could quickly and easily be applied in the setting of a chronic pain clinic. The CPEQ is modelled after the Multidimensional Pain Inventory (MPI) (2), one of the most commonly used measures of chronic pain (3). A vast amount of research concerning the classification of chronic pain patients has focused on the MPI as an assessment tool. In one such study, Turk and Rudy (4) reviewed 140 consecutive new patients referred to an outpatient pain clinic in Pittsburgh, Pennsylvania (USA), and presented an empirically derived pain patient taxonomy based on scores from the MPI, plus other measures. Using cluster analysis, Turk and Rudy identified three distinct profiles of pain patients. These patient profiles were labelled as ‘Dysfunctional’, ie, patients who reported relatively high levels of pain severity, pain-related interference in life activities, and psychological distress plus lower perceived ability to control their lives, and low activity levels but good social support; ‘Interpersonally Distressed’, ie, patients who reported that their significant others were not as supportive as those in the other two groups whereas other measures were intermediate between those of the other two groups; and ‘Adaptive Copers/Minimizers’, ie, patients who reported relatively low levels of pain, less perceived interference of pain in life activities and affective distress, as well as higher levels of daily activity and life control plus good social support. Subsequent studies have further validated this classification system in a broad range of chronic pain patients, including patients with fibromyalgia (5), low back pain (6), spinal cord injuries (7), lupus (8), whiplash-associated disorders (9), nonorganic chest pain (10) and temporomandibular disorder (11).
Whereas the MPI consists of 52 items, the CPEQ contains 15 items that measure four constructs: pain-related activity interference (AI), emotional distress (ED), pain intensity (PI) and pain-related social support (SS) (1). Cluster analyses of these four constructs revealed three profiles similar to those reported by Turk and Rudy with the MPI (4), supporting the generalizability of the MPI classification system in another sample of chronic pain patients with a somewhat different instrument. The development of a reliable and valid assessment instrument that can easily be administered, such as the CPEQ, may lead to an improved understanding of chronic pain patients.
Unfortunately, little research has been conducted with the CPEQ since its development. The present study attempted to further the understanding of the CPEQ and its usefulness in the classification of chronic pain patients. For our purposes, slight modifications were made to the original CPEQ to reflect the unique interests and practices of the Comprehensive Pain Program, Toronto Western Hospital, Toronto, Ontario, where the present study was conducted.
Physicians at the Comprehensive Pain Program commonly classify chronic pain patients in accordance to the three Pain Disorder diagnostic groups detailed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision (DSM-IV-TR) (12):
Group I – Pain Disorder Associated with a General Medical Condition, in which pain results from a general medical condition and psychological factors are judged to play either no role or a minimal role in the onset, severity, exacerbation or maintenance of the pain.
Group 2 – Pain Disorder Associated with both Psychological Factors and a General Medical Condition, in which both psychological factors and a general medical condition are judged to have important roles in the onset, severity, exacerbation or maintenance of the pain.
Group 3 – Pain Disorder Associated with Psychological Factors, in which psychological factors are judged to have the major role in onset, severity, exacerbation or maintenance of the pain. General medical conditions play either no role or a minimal role in the onset, severity, exacerbation or maintenance of the pain.
Because the DSM-IV-TR does not specify what psychological factors might be affecting pain and related disability, our group has generated (13,14) a detailed system of psychological factors that, based on our experience, are associated with pain and related disability. This classification system has shown consistent differences with regard to measurements of pain and opioid consumption between diagnostic groups in groups of patients (14), and has also served to guide treatment in the clinic. However, no previous studies have attempted to discern whether a relationship exists between the CPEQ construct scores or clusters and the three diagnostic groups detailed in the DSM-IV-TR.
The objectives of the present study were to describe the demographic characteristics as well as the functional and emotional status of patients presenting to a tertiary care hospital-based pain clinic affiliated with the University of Toronto (Ontario); assess the reliability and validity of the MPI/CPEQ cluster analysis and diagnostic classification system for chronic pain patients; provide psychometric data regarding a modified CPEQ; and, finally, evaluate the relationship between the modified CPEQ construct scores and clusters with DSM-IV-TR Pain Disorder diagnoses.
METHODS
Participants
Data were collected from a consecutive series of 300 new patients who agreed to participate in the study and who did not have a language barrier preventing them from completing standardized questionnaires and psychometrics. All patients had been referred to the Comprehensive Pain Program of the Toronto Western Hospital, a teaching hospital that is part of the University Health Network and affiliated with the University of Toronto. Data collection and analysis for research purposes were approved by the University Health Network Research Ethics Board. All patients who participated provided informed consent.
All new patients assessed at the Comprehensive Pain Program over the course of nine months within the 2008 to 2009 timeframe were approached at the time of first consultation and asked to participate in a research study. All participants were suffering from chronic pain lasting longer than three months. New patients were excluded if they declined to participate or if there was no interpreter in the case of a language barrier. Approximately 85% of new patients agreed to participate in the study and spent approximately 30 min completing a standard intake form. This form is routinely collected in the process of a Comprehensive Pain Program assessment, and contains demographic information (sex, marital status, level of education, country of birth and employment status), body maps where patients mark their pains and a verbal descriptor rating scale of pain intensity words based on the McGill Pain Questionnaire, and a modified CPEQ.
Procedure
Modifications made to the original CPEQ are described below. AI was measured using the seven items from the original 1994 CPEQ, which included work, performing household chores, yard work or shopping, socializing with friends, recreation and hobbies, having sexual relations and physical exercise. Two additional items, sleep and mental efficiency, were added to the modified CPEQ because the Comprehensive Pain Program is particularly interested in assessing these functions. It is well known that pain and related problems can interfere with cognitive function (15–17) and that sleep disturbance is a common problem with many chronic pain patients (18–20). Patients were instructed to rate the degree to which pain interfered with these activities on a five-point scale (1 = not at all to 5 = extremely). Patients who were unable to work in their usual occupation were asked to rank how much they believed pain would interfere with their usual work-related duties, while those who did not usually work outside the home were instructed to leave this question blank. SS was measured using the two items from the original CPEQ. Patients rated the extent to which their spouse or other family/significant others were supportive and encouraging (1 = always to 5 = never) and how often their significant others became angry or ignored them when they were in pain (1 = never to 5 = always). ED was measured using the three items from the original CPEQ. Patients rated the extent to which they felt tense or anxious, depressed or discouraged, and irritable or upset over the past month on a five-point scale (1 = not at all to 5 = extremely). To assess PI, the items that were used in the original CPEQ were replaced by an 11-point numerical rating scale (NRS, from 0 to 10, with 0 = no pain and 10 = the worst possible pain) for the average pain severity over the past month of the patient’s primary pain problem, because physicians at the clinic routinely record this pain score. The NRS pain severity scale is widely used and correlates well with other PI measurement instruments in several pain populations although it, as any other pain scale, is not without problems (21–27). The CPEQ was modified for the convenience of the Comprehensive Pain Program to specifically relate to the Program practice and population of patients (Appendix 1). The CPEQ and other routinely administered documents were used to assess each patient.
DSM-IV-TR diagnosis (groups I, II or III) was based on the clinical interview, physical examination, behavioural observations, review of relevant files and investigations, and presence of relevant psychiatric or psychological reports from previous encounters. Group I patients were considered to suffer from a biomedical cause responsible for their pain and related disability. Group II patients had a combination of biomedical causes and psychological factors recognized by the pain clinicians as important contributors to their pain and related disability. Group III patients had no detectable biomedical cause, but identifiable psychological factors considered relevant for their pain and related disability. Notably, in the authors’ practice, a group III diagnosis is not a diagnosis of exclusion, ie, it is not made solely on the basis of absence of detectable physical pathology to account for the patient presentation. Rather, such a diagnosis requires a combination of detailed clinical information by history and physical examination, absence of positive biomedical investigations (eg, computed tomography scans, magnetic resonance imaging, electrophysiological investigations, bone scans, operative reports delineating surgical findings, etc), and behavioural observations, including but not limited to, degree of disability or pain severity and its concordance with clinical findings and investigations. (28) The authors’ clinic has described and used for publications a detailed system of psychological factors that they believe contribute to the presentation (13,14).
Data analysis
All data were analyzed with SPSS version 16.0 (IBM Corporation, USA). The Kolmogorov-Smirnov test was used to assess whether the modified CPEQ constructs were normally distributed. Because each of these were found to be normally distributed (P<0.01, two-tailed), parametric statistics are reported; nonparametric statistics are also reported because these variables are likely of an ordinal level of measurement. Statistical relationships were therefore evaluated with both parametric (ANOVA, Pearson r) and nonparametric (Mann-Whitney U, Kruskal-Wallis, Kolmogorov-Smirnov, Kendall’s tau-b, Pearson χ2) statistics as appropriate. A two-sided P<0.05 was used to define minimal statistical significance. Where ANOVAs were statistically significant, effect sizes are reported using eta squared (eta2). A two-step cluster analysis was conducted on the four modified CPEQ construct scores (AI, PI, SS and ED). The SPSS two-step statistical clustering technique was used because it provides an optimal statistical solution for the number of clusters without specifying the number of clusters or choosing different solutions as required in a k-means solution or hierarchical clustering.
RESULTS
Of the 300 patients who participated in the present study, 166 were women and 134 were men (female to male ratio of 1.24:1). The majority of patients (61.3%) were born in Canada. The remainder were born outside Canada, primarily in southern Europe, the Caribbean, south central Asia and northern Europe. At time of presentation, the mean (± SD) age for all patients was 48.9±14.5 years (range 17 to 89 years). More than one-half of patients were married or in common-law relationships (57.7%). The remaining 42.3% were divorced, separated, widowed or never married, and were considered ‘single’. Approximately 17% had received only some grade school education, 42% had completed a high school education or at least some high school, 22% had some college education or had obtained a college degree, and 18% had achieved some university education or completed a university degree. Only 24.2% of patients were employed (full or part time) at first consultation, 49.8% were unemployed due to pain or related problems, and the remaining 26% consisted of students, housewives, retirees or others who did not usually work. The study participants reported the following primary pain areas: back (27%), head/neck (13%), arms/ shoulders (13%), hips/legs (13%), foot/ankle (10%), knees (5%), hands/wrists (4%), chest (4%), abdomen (3%) and other (8%). Eighty-seven per cent of participants experienced pain for longer than one year in duration. Of the 300 participants, only 268 had completed all 14 items of the CPEQ and were included in the analysis of the CPEQ and cluster analysis. Similarly, 274 of the 300 participants were given a DSM-IV-TR diagnostic classification and could be included in the analysis.
CPEQ
The strength of the relationship between the items of the original AI construct used by Jamison et al (1) and the items of the modified AI construct presented in the present study was assessed by conducting an analysis of the same participants (n=268) who completed all items, with and without the two additional items. There was a high degree of correspondence between the two measures (Kendall’s tau-b=0.825, P<0.001; Pearson’s r=0.955; P<0.001). As it could be expected that there would be a high correlation of the pain-related disability items, with and without the two additional items, an assessment of the internal consistency of all items was also conducted. The Cronbach’s alpha of 0.777 indicated overall acceptable internal consistency. However, whereas sleep and mental efficiency correlated well with most other items, recreation/hobbies and sexual relations did not (Table 1).
TABLE 1.
Interitem correlation matrix – activity interference items
| Work | Household chores | Shopping | Social activities | Recreational activities | Sexual relations | Physical exercise | Sleep | Mental efficiency | |
|---|---|---|---|---|---|---|---|---|---|
| Work | 1 | 0.660 | 0.598 | 0.484 | 0.057 | 0.031 | 0.611 | 0.502 | 0.304 |
| Household chores | 0.660 | 1 | 0.731 | 0.568 | 0.023 | −0.036 | 0.608 | 0.569 | 0.460 |
| Shopping | 0.598 | 0.731 | 1 | 0.525 | 0.033 | −0.023 | 0.557 | 0.540 | 0.421 |
| Social activities | 0.484 | 0.568 | 0.525 | 1 | 0.045 | −0.055 | 0.393 | 0.418 | 0.376 |
| Recreational activities | 0.057 | 0.023 | 0.033 | 0.045 | 1 | 0.505 | 0.008 | 0.021 | −0.112 |
| Sexual relations | 0.031 | −0.036 | −0.023 | −0.055 | 0.505 | 1 | −0.024 | −0.036 | −0.135 |
| Physical exercise | 0.611 | 0.608 | 0.557 | 0.393 | 0.008 | −0.024 | 1 | 0.488 | 0.347 |
| Sleep | 0.502 | 0.569 | 0.540 | 0.418 | 0.021 | −0.036 | 0.488 | 1 | 0.469 |
| Mental efficiency | 0.304 | 0.460 | 0.421 | 0.376 | −0.112 | −0.135 | 0.347 | 0.469 | 1 |
Overall, patients reported a moderate degree of AI (mean ± SD 3.9±0.7), PI (6.4±2.0), ED (3.7±0.9) and SS (1.9±0.99) at time of first consultation with the Comprehensive Pain Program clinicians. Of note, for the SS construct, a lower score is more favourable, indicating better SS.
Table 2 presents the Kendall tau-b and Pearson r correlation coefficients for each of the four CPEQ constructs. Similar to the results reported by Jamison et al (1), the four constructs displayed small to moderate intercorrelations. The correlations were found to range in magnitude from −0.004 to 0.339 (Kendall’s tau-b) and −0.025 to 0.434 (Pearson’s r), indicating that sufficient discriminate distinctiveness existed among the four constructs.
TABLE 2.
Correlation matrix of modified Comprehensive Pain Evaluation Questionnaire constructs
|
Activity interference
|
Pain intensity
|
Social support
|
Emotional distress
|
|||||
|---|---|---|---|---|---|---|---|---|
| Pearson’s r | Kendall’s tau-b | Pearson’s r | Kendall’s tau-b | Pearson’s r | Kendall’s tau-b | Pearson’s r | Kendall’s tau-b | |
| Activity interference | 1.000 | 1.000 | ||||||
| Pain intensity | 0.224** | 0.313** | 1.000 | 1.000 | ||||
| Social support | −0.004 | 0.049 | −0.036 | −0.025 | 1.000 | 1.000 | ||
| Emotional distress | 0.339** | 0.434** | 0.256** | 0.284** | 0.145* | 0.230** | 1.000 | 1.00 |
P<0.01 (two-tailed);
P<0.001 (two-tailed)
Relationship of demographics with the modified CPEQ constructs
There were several statistically significant relationships between demographic variables and modified CPEQ constructs. Older patients tended to report less ED (Kendall’s tau-b=−0.130, P<0.005; Pearson’s r=−0.202, P<0.001) and AI (Pearson’s r=−0.119, P<0.05) than younger patients. Female patients reported better SS than male patients (F=4.7, P<0.05, eta2=0.016) and those who were married or in common-law relationships reported significantly better SS than single patients (Kruskal Wallis = 5.3, P<0.05; F=4.9, P<0.05, eta2=0.017). There were no statistically significant differences in AI, PI, SS or ED based on education level, although the relationship between educational level and AI interference approached significance with those having at least some university education reporting slightly less AI. A significantly higher degree of pain was reported by foreign-born patients compared with Canadian-born ones (Mann-Whitney = −2.4, P<0.05; F=5.1, P<0.05, eta2=0.018). A patient’s employment status was related to the amount of AI (Kruskal Wallis = 35.8, P<0.001; F=18.9, P<0.001, eta2=0.124), ED (Kruskal Wallis = 24.8, P<0.001; F=12.6, P<0.001, eta2=0.087) and PI (Kruskal Wallis = 11.9, P<0.005; F=6.6, P<0.005, eta2=0.049) that they experienced. Post hoc tests revealed significant differences in ED, AI and PI between patients who were not working due to pain or related problems and both patients who were employed full or part time and patients who were not usually working. No statistically significant differences were apparent between patients who were employed full or part time and patients who were not usually working (housewives, students and retirees). Patients not working due to pain or medical reasons reported more ED than patients employed full or part time (P<0.005), as well as patients not usually working (P<0.001). They also reported more AI than patients employed full or part time (P<0.001) and patients not usually working (P<0.001), as well as more PI than patients employed full or part time (P<0.05) and patients not usually working (P<0.05).
Cluster analysis
Responses to the 14 items included in the modified CPEQ were used to divide the patients into clusters. Patients who did not respond to all 14 items were excluded from the cluster analysis. Complete data were available for 268 patients; 89% of these patients could be classified into one of three clusters approximating those initially identified using the MPI. The first cluster, identified as the ‘Dysfunctional’ subtype, contained 39.9% (n=107) of individuals. The second cluster, identified as the ‘Adaptive Coper/Minimizer’ subtype, contained 35.4% (n=95) of patients, and the third cluster, identified as the ‘Interpersonally Distressed’ subtype, contained 24.6% (n=66).
The means and SDs of the modified CPEQ constructs for the three patient profiles are displayed in Table 3. Figure 1 plots the standardized T scores (50±10) of the modified CPEQ constructs for the three clusters. Adaptive Copers had relatively low levels of AI, PI and ED in comparison with the other two subtypes. The Dysfunctional patients had the highest levels of AI and PI. They also had high levels of ED, although the Interpersonally Distressed patients had the highest level of ED. The Interpersonally Distressed patients had intermediate levels of AI and PI and very poor SS in comparison with the other two groups, while the Dysfunctional patients reported the best SS.
TABLE 3.
Cluster analysis of modified Comprehensive Pain Evaluation Questionnaire constructs for the three patient profiles (n=268)
| Activity interference | Pain intensity* | Social support | Emotional distress | |
|---|---|---|---|---|
| Dysfunctional | 4.36±0.35 | 3.73±0.66 | 1.41±0.47 | 4.12±0.66 |
| Adaptive Coper | 3.38±0.64 | 2.52±1.01 | 1.57±0.64 | 2.93±0.78 |
| Interpersonally Distressed | 3.99±0.59 | 3.43±0.83 | 3.36±0.68 | 4.23±0.66 |
Data presented as mean ± SD.
Transformed from an 11-point scale to a five-point scale to make comparisons with the other constructs
Figure 1).
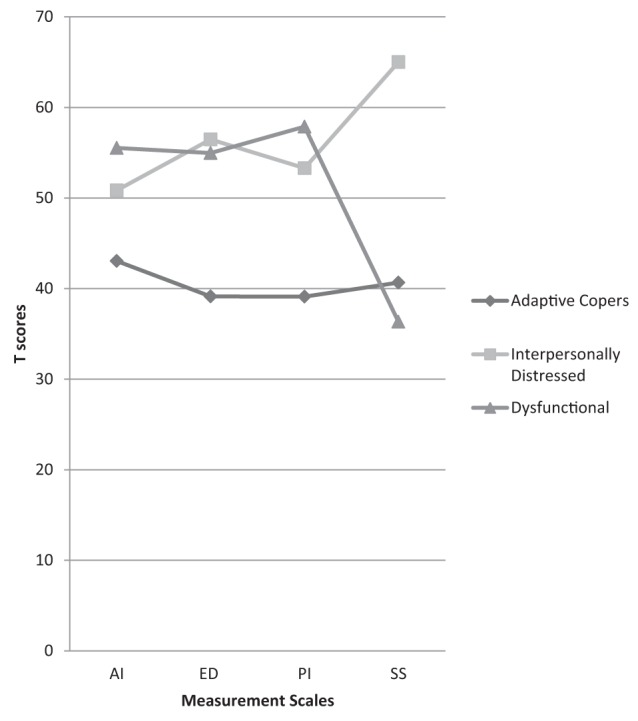
Standardized T scores for the two-step cluster analysis of the modified Comprehensive Pain Evaluation Questionnaire constructs. AI Activity interference; ED Emotional distress; PI Pain intensity; SS Social support
There were no statistically significant differences between the clusters with respect to sex, marital status, education, age or country of origin. There was, however, a significant difference for employment status (χ2=14.7, P<0.01). More of the Interpersonally Distressed (33%) were at work on some basis in comparison with the Adaptive Copers (28%) or the Dysfunctional (20%) patients. More Dysfunctional patients were off work due to pain or related problems (60%) than either the Interpersonally Distressed (51%) or the Adaptive Copers (34%). There were more Adaptive Copers who did not usually work (38%) than either the Dysfunctional (20%) or the Interpersonally Distressed (16%) subtypes.
DSM-IV-TR diagnostic group classification
Information regarding diagnostic classification was available for 274 patients. Just less than one-half (49%) of the sample were considered to present with both significant medical and psychological factors (group II), whereas 31% were considered to present primarily with biomedical factors (group I), and 20% were considered to present with primarily psychological factors (group III). There were no statistically significant differences in terms of distribution of diagnostic groups with respect to sex, education, marital status or country of origin. However, statistically significant age differences existed for the three diagnostic groups (Kruskal Wallis = 27.4, P<0.001; F=16.1, P<0.001, eta2=0.106). Post hoc tests revealed that there were significant differences between group I and both group II and group III (P<0.001), but not between groups II and III. Those with demonstrable biomedical pathology and no significant psychological factors (group I) were older (55±15 years) than those in group II (47±13 years) or group III (42±11 years).There were also significant differences with respect to diagnoses and employment status (χ2=24.6, P<0.001). Whereas only 27% of those in group I were not working due to pain or related problems, the figures rose to 64% and 58% of those in group II and group III, respectively.
Table 4 presents ANOVAs that showed significant differences between diagnostic groups and AI (Kruskal Wallis = 28.3, P<0.001; F=13.9, P<0.001, eta2=0.093), ED (Kruskal Wallis = 20.1, P<0.001; F=9.6, P<0.001, eta2=0.066) and PI (Kruskal Wallis = 28.4, P<0.001; F=16.2, P<0.001, eta2=0.111). Post hoc analysis revealed significant differences between group I and both groups II and III in terms of AI, ED and PI, but not between groups II and III. Patients with a group I diagnosis had lower levels of AI (P<0.001), ED (P<0.005) and PI (P<0.001) than patients with either a group II or group III diagnosis. There were no significant differences in SS based on diagnostic classification.
TABLE 4.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision diagnostic classification and modified Comprehensive Pain Evaluation Questionnaire (CPEQ) constructs (n=274)
| CPEQ construct | Diagnosis | Mean | Kruskal-Wallis |
|---|---|---|---|
| Activity interference | Group I | 3.6 | 0 |
| Group II | 4.1 | ||
| Group III | 4.1 | ||
| Emotional distress | Group I | 3.4 | 0 |
| Group II | 3.9 | ||
| Group III | 3.9 | ||
| Social support | Group I | 1.8 | 0.092 |
| Group II | 1.9 | ||
| Group III | 2.2 | ||
| Pain intensity | Group I | 5.4 | 0 |
| Group II | 6.8 | ||
| Group III | 6.7 |
Group I – Pain Disorder Associated with a General Medical Condition, in which pain results from a general medical condition and psychological factors are judged to play either no role or a minimal role in the onset, severity, exacerbation or maintenance of the pain; Group 2 – Pain Disorder Associated with both Psychological Factors and a General Medical Condition, in which both psychological factors and a general medical condition are judged to have important roles in the onset, severity, exacerbation or maintenance of the pain; Group 3 – Pain Disorder Associated with Psychological Factors, in which psychological factors are judged to have the major role in onset, severity, exacerbation or maintenance of the pain. General medical conditions play either no role or a minimal role in the onset, severity, exacerbation, or maintenance of the pain
Table 5 summarizes the relationship of DSM-IV-TR Pain Diagnoses and cluster analysis. Two hundred forty-eight patients who completed the modified CPEQ questionnaires and were assigned a group diagnosis were included in this analysis. The difference in distribution of clusters among diagnostic groups was significant (χ2=40.1, P<0.001). The majority of group I patients were Adaptive Copers (55%), the majority of Dysfunctional patients (56%) fell in group II, and the Interpersonally Distressed patients were more equally distributed across the diagnostic groups although relatively more of these patients fell in group III.
TABLE 5.
Relationship of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision diagnostic classification and cluster analysis
| Diagnosis | Adaptive Coper | Interpersonally Distressed | Dysfunctional | Total, n |
|---|---|---|---|---|
| Group I | 43 (55) | 20 (26) | 15 (19) | 78 |
| Group II | 21 (17) | 32 (27) | 68 (56) | 121 |
| Group III | 12 (25) | 18 (37) | 19 (39) | 49 |
| Total | 76 (31) | 70 (28) | 102 (41) | 248 |
Data presented as n (%) unless otherwise indicated. Group I – Pain Disorder Associated with a General Medical Condition, in which pain results from a general medical condition and psychological factors are judged to play either no role or a minimal role in the onset, severity, exacerbation or maintenance of the pain; Group 2 – Pain Disorder Associated with both Psychological Factors and a General Medical Condition, in which both psychological factors and a general medical condition are judged to have important roles in the onset, severity, exacerbation or maintenance of the pain; Group 3 – Pain Disorder Associated with Psychological Factors, in which psychological factors are judged to have the major role in onset, severity, exacerbation or maintenance of the pain. General medical conditions play either no role or a minimal role in the onset, severity, exacerbation, or maintenance of the pain
DISCUSSION
The results of the present study indicate that the classification system of chronic pain patients originally proposed by Turk and Rudy (4) can be replicated using a modified version of the CPEQ in our sample of chronic pain patients attending the Comprehensive Pain Program in Toronto, Ontario. Additionally, this is the first study to investigate the relationship between CPEQ constructs and clusters and underlying diagnoses, demonstrating that AI, ED and PI were poorer in groups II and III as compared with those patients classified as suffering from a biomedical condition only (group I).
Three patient profiles, Adaptive Copers, Dysfunctional and Interpersonally Distressed, were identified and resembled those reported by Turk and Rudy (4) and Jamison et al (1). Indeed, the plot of the standardized T scores from our study is almost identical to that of Jamison et al (1). This would suggest a remarkable robustness of results utilizing these four constructs across samples of pain patients despite some alteration in the measures used. Similar to the Jamison et al (1) findings, patients in the current study who were classified as Adaptive Copers showed the least amount of AI, ED and PI, while patients classified as Dysfunctional showed the greatest amount of AI and PI, and patients classified as Interpersonally Distressed expressed the most ED. The Interpersonally Distressed patients also had the poorest SS whereas the Dysfunctional patients reported the best SS with the Adaptive Copers/Minimizers reporting only slightly poorer SS than the Dysfunctional patients. Of note, while the current study provides data on a modified CPEQ, the constructs remain the same as the original CPEQ and the MPI. This proves that measuring the amount of AI, ED, PI and SS will produce the same results regardless of the measurement tool. Therefore, the results are reproducible across somewhat different measurement techniques proving the strength and robustness of the underlying constructs.
The percentage of the three cluster profiles differs somewhat in the published literature (1,4,29) depending on the sample examined. In the current study, approximately 40% of our patients were of the Dysfunctional subtype, 35% were Adaptive Copers/Minimizers, and 25% were Interpersonally Distressed. It is notable that in all samples studied by Turk and Rudy (4), all but one of the samples by Jamison et al (1), and in our sample, the proportion of Dysfunctional patients was always the greatest. It is therefore obvious that the relative proportions of Adaptive Copers, Dysfunctional or Interpersonally Distressed patients may vary depending on the sample studies, but these same three clusters are repeatedly found.
Assessment of the internal consistency of the items of the AI construct revealed that recreation/hobbies and sexual activity correlated with one another, but not with other items. We are not aware of this finding in other studies and will pursue research into this.
In regard to the relationship between CPEQ constructs and clusters and diagnostic groups, our study confirmed the previously reported distribution of such diagnoses in the Comprehensive Pain Program, with approximately one-half of all patients diagnosed as group II. The majority of patients diagnosed with a primarily biomedical disability (group I) were Adaptive Copers/Minimizers. In contrast, more of those in groups II and III (where psychological factors were recognized by the clinicians to play a substantial or primary role in the patients’ presentation) proved to be Dysfunctional or Interpersonally Distressed. The findings are consistent with a previous study from our program (14) that patients in group I seem to be much more in control of their pain and generally require less opioid medications despite their biomedical disorder, and have lower pain ratings. The present study also demonstrates that the application of diagnoses based on biomedical and/or psychological factors, as described in the Methods section, by experienced pain clinicians, corresponds to the constructs and clusters of the modified CPEQ. The CPEQ is sensitive to the diagnostic group classification; therefore, it is our opinion that application of our clinical diagnostic system can assist in directing treatment of chronic pain. Patients classified as having a biomedical condition only (group I) and/or those that tend to be classified as Adaptive Copers may benefit from additional medical testing and interventions. For those with pain associated with psychological factors (with or without the concomitant presence of biomedical conditions) and/or those classified as Dysfunctional or Interpersonally Distressed, treatment may be directed away from possibly harmful or unnecessary medical interventions and toward psychosocial treatments (30). Furthermore, the relationship of the diagnostic system with the cluster analysis results provides additional evidence to the construct validity of the cluster analysis.
Jamison et al (1) found that, in comparison with Interpersonally Distressed or Dysfunctional patients, physician ratings of Adaptive Copers/Minimizers indicated that these patients dramatized pain less, and that they were less nervous, depressed or irritable. Adaptive Copers/Minimizers were also found to have better psychological adjustment on another self-report inventory, used opioid or tranquilizer medications less, and had less sleep disturbance and a higher rate of employment. Thus, they appeared better adjusted. In contrast to the results of the current study, Jamison et al (1) found that Adaptive Copers were more likely to have normal musculoskeletal and neurological findings. It should be noted, however, that normal musculoskeletal and neurological examination was found in the majority of patients in all the original CPEQ subtypes in the Jamison et al study. In the current study, Adaptive Copers were more likely to have a discernible biomedical disorder (group I). Again, this may reflect the expertise of our pain clinic and our referral patterns. Turk and Rudy (4) noted that the score on a total index of pathology was related to three of the nine MPI scales, but cluster subtypes could not be accounted for solely by degree of physical pathology.
Jamison et al (1) also found that the three patient profiles did not display significant differences on basic demographic characteristics including sex, educational level, marital status or pain duration. Whereas age was significantly different in one of the samples from our study, the difference was small and considered to be nonmeaningful. Additionally, Turk and Rudy (4) demonstrated that while basic demographics including age and sex as well as duration of pain were not related to clusters, both the Jamison et al (1) and the Turk and Rudy (4) studies found that various behavioural or psychological measures were related to clusters. The current study is generally in agreement with the above cited findings (1,4) because we also found a significant relationship between employment status and clusters. Dysfunctional patients tended to more often be unemployed.
Demographic data on the 300 consecutive new patients referred to the Comprehensive Pain Program included in the present study are similar to previous literature published by our clinic (27,31). Our data consistently show that the peak age of chronic pain patients presenting to pain clinics is the mid to late 40s, suggesting that chronic pain affects a most productive age group. Additionally, we have previously reported (28) that age is related to diagnostic categories, with group I patients being older, group III the youngest and group II intermediate. It is worth stressing that our data from this and another study from our clinic (28) show that older patients specifically have much higher rates of biomedical disorders with relatively little overlying psychological factors affecting disability. We have also consistently reported a higher attendance rate of women in our pain program than men. This is in agreement with literature that women in North America have a higher rate of health care use than men (32), in addition to having a higher rate of pain problems (33,34).
The current study found several significant relationships between demographics and CPEQ construct scores. However, with the exception of employment status, effect sizes were small and statistically significant effects were not found for either the parametric or nonparametric tests for several relationships (ie, for age and AI, sex and SS, education and AI). Of note, there was generally good concordance between the results of parametric and nonparametric tests except in those cases where there were very small effect sizes. As might be expected, those who were not working due to pain and related problems reported higher levels of AI, PI and ED. It is of some interest that women tended to report a higher level of SS than men did. This may be due to differences in willingness to communicate pain experiences (35). Men seem reluctant to complain about their symptoms to prevent burdening others; this can make it difficult for significant others to understand their pain experiences (36). It is not surprising that patients who were married or in common-law relationships reported a higher amount of SS than did single patients or that patients who were unemployed due to their chronic pain reported more AI, PI and ED.
Our study has several limitations. First, it was carried out in one tertiary care pain clinic. Therefore, the results may not be generalizable to chronic pain populations seen in primary care and may not represent other pain clinic populations. Referral biases based on multiple factors (clinic expertise and reputation, location, waiting list, preferences of referring physicians, patient preferences, etc) do influence the types of patients attending the clinic and must be taken into account when interpreting the results. Secondly, clustering versus the types of pain underlying the patients’ conditions such as musculoskeletal, visceral or neuropathic was not assessed, because the underlying pain mechanism may play a role in presentation or treatment outcome. Finally, our diagnostic and management approaches may be different than those used in other pain clinics or primary care facilities.
CONCLUSION
The present study, which replicated the cluster subtypes initially proposed by Turk and Rudy (4) and subsequently replicated by Jamison et al (1) using the original CPEQ, suggests that a modified CPEQ (similar to the original CPEQ) can be administered as part of a comprehensive chronic pain patient assessment. The novel finding of the relationship between CPEQ cluster subtypes and DSM-IV-TR diagnostic classification groups depending on the presence of biomedical pathology and/or psychological factors may also guide treatment. Further investigations should explore the nature of specific psychological factors underlying the clusters and address the use of the taxonomy described in the present study to classify patients to direct them to the most appropriate treatment.
Appendix 1.
CPEQ
Name:___________________ Date:______________
I. Activity Interference
During the past month, how much did pain interfere with the following activities?
(Circle the number for each of the questions that best describes your situation.)
| Not at all | A little bit | Moderately | Quite | Extremely | |
|---|---|---|---|---|---|
| Work* | 1 | 2 | 3 | 4 | 5 |
| Performing household chores | 1 | 2 | 3 | 4 | 5 |
| Yard work or shopping | 1 | 2 | 3 | 4 | 5 |
| Socializing with friends | 1 | 2 | 3 | 4 | 5 |
| Recreation and hobbies | 1 | 2 | 3 | 4 | 5 |
| Having sexual relations | 1 | 2 | 3 | 4 | 5 |
| Physical exercise | 1 | 2 | 3 | 4 | 5 |
| Sleep | 1 | 2 | 3 | 4 | 5 |
| Mental efficiency | 1 | 2 | 3 | 4 | 5 |
If not working because of medical or other reasons, how much do you think pain would interfere with your usual work if you were to be working?
II. Pain Intensity
Using the Numerical Rating Scale where “0”= “no pain” and “10”= “the worst possible pain”, patients rated the average pain severity of their primary pain problem in the past month.
(Of note, the following two items were included in a version of the CPEQ provided to Dr. Nicholson from Dr. Jamison in 1998 (personal communication).
These may be more useful in some clinical situations.
Which of the following best describes your usual level of pain? (Circle one).
| Mild | Uncomfortable | Distressing | Very Severe | Unbearable |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
Please rate your average pain intensity on a scale from 0 = no pain to 10 = excruciating, incapacitating, worst pain possible. (Circle one)
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
III. Support
When you are in pain, how often is your husband/wife/other family supportive and encouraging?
| Never | Seldom | Sometimes | Frequently | Always |
|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 |
When you are in pain, how often does your husband/wife/other family ignore you or become angry? (Circle one).
| Never | Seldom | Sometimes | Frequently | Always |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
IV. Emotional Distress
During the past month have you been tense or anxious? (Circle one).
| Never | Seldom | Sometimes | Frequently | Always |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
During the past month have you been depressed or discouraged? (Circle one).
| Never | Seldom | Sometimes | Frequently | Always |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
During the past month have you been irritable and upset? (Circle one).
| Never | Seldom | Sometimes | Frequently | Always |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
Footnotes
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Jamison RN, Rudy TE, Penzien D, et al. Cognitive-behavioural classifications of chronic pain: Replication and extension of empirically derived patient profiles. Pain. 1994;57:277–92. doi: 10.1016/0304-3959(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 2.Kerns RD, Turk DC, Rudy TE. The West Haven Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 3.Piotrowski C. Assessment of pain: A survey of practicing clinicians. Percept Mot Skills. 1998;86:181–2. doi: 10.2466/pms.1998.86.1.181. [DOI] [PubMed] [Google Scholar]
- 4.Turk DC, Rudy TE. Toward an empirically derived taxonomy of chronic pain patients: Integration of psychological assessment data. J Consult Clin Psychol. 1988;56:233–8. doi: 10.1037//0022-006x.56.2.233. [DOI] [PubMed] [Google Scholar]
- 5.Turk DC, Okifuji A, Sinclair JD, et al. Pain, disability, and physical functioning in subgroups of patients with fibromyalgia. J Rheumatol. 1996;23:1255–62. [PubMed] [Google Scholar]
- 6.Vollenbroek-Hutton MM, Hermens HJ, Wever D, et al. Differences in outcome of multidisciplinary treatment between subgroups of chronic low back pain patients defined using two multiaxial assessment instruments: The Multidimensional Pain Inventory and lumber dynamometry. Clin Rehabil. 2004;18:566–79. doi: 10.1191/0269215504cr772oa. [DOI] [PubMed] [Google Scholar]
- 7.Widerstrom-Noga EG, Duncan R, Felipe-Cuervo E, et al. Assessment of the impact of pain and impairments associated with spinal cord injuries. Arch Phys Med Rehabil. 2002;83:395–404. doi: 10.1053/apmr.2002.28028. [DOI] [PubMed] [Google Scholar]
- 8.Greco CM, Rudy TE, Manz S. Adaptation to chronic pain in systemic lupus erythematosus: Applicability of the Multidimensional Pain Inventory. Pain Med. 2003;4:39–50. doi: 10.1046/j.1526-4637.2003.03001.x. [DOI] [PubMed] [Google Scholar]
- 9.Olsson I, Bunketorp O, Carlsson SG, et al. Prediction of outcome in whiplash-associated disorders using West Haven-Yale Multidimensional Pain Inventory. Clin J Pain. 2002;18:238–44. doi: 10.1097/00002508-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Beck JG, Chase TJ, Berisford MA, et al. Pain profiles of patients with nonorganic chest pain: A preliminary report of the Multidimensional Pain Inventory. J Pain Symptom Manage. 1992;7:470–7. doi: 10.1016/0885-3924(92)90133-3. [DOI] [PubMed] [Google Scholar]
- 11.Epker J, Gatchel RJ. Coping profile differences in the biospsychosocial functioning of patients with temporomandibular disorder. Psychosomat Med. 2000;62:69–75. doi: 10.1097/00006842-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 12.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 13.Mailis-Gagnon A, Nicholson K, Yegneswaran B, et al. Pain characteristics of adults 65 years of age and older referred to a tertiary care pain clinic. Pain Res Manag. 2008;13:389–94. doi: 10.1155/2008/541963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mailis-Gagnon A, Lakha SF, Ou T, et al. Chronic non cancer pain: Characteristics of patients prescribed opioids by community physicians and referred to a tertiary care pain clinic. Can Fam Physician. 2011;57:97–105. [PMC free article] [PubMed] [Google Scholar]
- 15.Nicholson K, Martelli M. The confounding effects of pain, psychiatric disorder, sleep disturbance and motivational factors on neuropsychological test performance. In: Young G, Kane A, Nicholson K, editors. Psychological Knowledge in Court: PTSD, Pain and TBI. New York: Springer; 2006. pp. 36–44. [Google Scholar]
- 16.Glass JM. Review of cognitive dysfunction in fibromyalgia: A convergence on working memory and attentional control impairments. Rheum Dis Clin North Am. 2009;35:299–311. doi: 10.1016/j.rdc.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Ji G, Sun H, Fu Y, et al. Cognitive impairment in pain through amygdala-driven prefrontal cortical deactivation. J Neurosci. 2010;30:5451–64. doi: 10.1523/JNEUROSCI.0225-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Brien EM, Waxenberg LB, Atchison JW, et al. Negative mood mediates the effect of poor sleep on pain among chronic pain patients. Clin J Pain. 2010;26:310–9. doi: 10.1097/AJP.0b013e3181c328e9. [DOI] [PubMed] [Google Scholar]
- 19.Quartana PJ, Wickwire EM, Klick B, et al. Naturalistic changes in insomnia symptoms and pain in temporomandibular joint disorder: A cross-lagged panel analysis. Pain. 2010;149:325–31. doi: 10.1016/j.pain.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 20.Lunde LH, Pallesen S, Krangnes L, et al. Characteristics of sleep in older persons with chronic pain: A study based on actigraphy and self-reporting. Clin J Pain. 2010;26:132. doi: 10.1097/AJP.0b013e3181b61923. [DOI] [PubMed] [Google Scholar]
- 21.Brunelli C, Zecca E, Martini C, et al. Comparison of numerical and verbal rating scales to measure pain exacerbations inpatients with chronic cancer pain. Health Qual Life Outcomes. 2010;8:42. doi: 10.1186/1477-7525-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miró J, Castarlenas E, Huguet A. Evidence for the use of a numerical rating scale to assess the intensity of pediatric pain. Eur J Pain. 2009;13:1089–95. doi: 10.1016/j.ejpain.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Li L, Herr K, Chen P. Postoperative pain assessment with three intensity scales in Chinese elders. J Nurs Scholarsh. 2009;41:241–9. doi: 10.1111/j.1547-5069.2009.01280.x. [DOI] [PubMed] [Google Scholar]
- 24.Lorenz KA, Sherbourne CD, Shugarman LR, et al. How reliable is pain as the fifth vital sign? J Am Board Fam Med. 2009;22:291–8. doi: 10.3122/jabfm.2009.03.080162. [DOI] [PubMed] [Google Scholar]
- 25.Hjermstad MJ, Gibbins J, Haugen DF, et al. EPCRC, European Palliative Care Research Collaborative. Pain assessment tools in palliative care: an urgent need for consensus. Palliat Med. 2008;22:895–903. doi: 10.1177/0269216308095701. [DOI] [PubMed] [Google Scholar]
- 26.Krebs EE, Carey TS, Weinberger M. Accuracy of the pain numeric rating scale as a screening test in primary care. J Gen Intern Med. 2007;22:1453–1458. doi: 10.1007/s11606-007-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lundeberg T, Lund I, Dahlin L, et al. Reliability and responsiveness of three different pain assessments. J Rehabil Med. 2001;33:279–83. doi: 10.1080/165019701753236473. [DOI] [PubMed] [Google Scholar]
- 28.Mailis-Gagnon A, Yegneswaran B, Lakha SF, et al. Pain Characteristics and demographics of patients attending a university-affiliated pain clinic in Toronto, Ontario. Pain Res Manag. 2007;12:93–9. doi: 10.1155/2007/658762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turk DC, Rudy TE. The robustness of an empirically derived taxonomy of chronic pain patients. Pain. 1990;43:27–35. doi: 10.1016/0304-3959(90)90047-H. [DOI] [PubMed] [Google Scholar]
- 30.Mailis-Gagnon A, Nicholson K, Zurowski M. The future of the DSM Pain Disorder Category. Psychosomatics. 2008;42:4. doi: 10.1176/appi.psy.49.4.362. [DOI] [PubMed] [Google Scholar]
- 31.Mailis-Gagnon A, Yegneswaran B, Nicholson K, et al. Ethnocultural and sex characteristics of patients attending a tertiary care pain clinic in Toronto, Ontario. Pain Res Manag. 2007;12:100–6. doi: 10.1155/2007/425318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Health Status of Canadians: Report of the 1991 General Social Survey Cat 0836-043X, No 8. Ottawa: Statistics Canada; 1994. [Google Scholar]
- 33.Berkley K. Sex differences in pain. Behav Brain Sci. 1997;20:371–80. doi: 10.1017/s0140525x97221485. [DOI] [PubMed] [Google Scholar]
- 34.LeResche L. Epidemiologic perspectives on sex differences in pain. In: Fillingim RB, editor. Sex, Gender and Pain, Progress in Pain Research and Management, Vol 17. Seattle: IASP Press; 2000. pp. 233–49. [Google Scholar]
- 35.Robinson ME, Riley JL, III, Myers C. Psychosocial contributions to Sex related differences in pain responses. In: Fillingim RB, editor. Sex, Gender and Pain, Progress in Pain Research and Management, Vol 17. Seattle: IASP Press; 2000. pp. 41–68. [Google Scholar]
- 36.Paulson M, Danielson E, Soderberg S. Struggling for a tolerable existence: The meaning of men’s lived experiences of living with pain of fibromyalgia type. Qual Health Res. 2002;12:238–49. doi: 10.1177/104973202129119865. [DOI] [PubMed] [Google Scholar]


