Abstract
The in vitro activity of PA-824 and BTZ043 against 30 Nocardia brasiliensis isolates was tested. The MIC50 and MIC90 values for PA-824 were both >64 μg/ml. The same values for BTZ043 were 0.125 and 0.250 μg/ml. Given the MIC values for benzothiazinone (BTZ) compounds, we consider them good candidates to be tested in vivo against N. brasiliensis.
TEXT
Nocardia brasiliensis is a natural inhabitant of the soil that in some cases gains entry to human skin by trauma with splinters or wood material contaminated with this bacterium (17). Once in the subcutaneous tissues, the bacteria proliferate, producing local inflammation, abscesses, and fistulae, and may affect subjacent organs, depending on the topographic localization of the lesions. The production of chronic inflammation and scarring of tissue makes it difficult for antimicrobials to penetrate and act against the bacteria. Several antimicrobials, including sulfonamides, aminoglycosides, beta-lactams, etc., have been used in the treatment of actinomycetoma (2, 5, 17). However, in some cases cure is not obtained, making it important to evaluate in vitro and in vivo the activity of new antimicrobials.
Given the close phylogenetic relationship among actinobacteria, it is possible that some antitubercular agents are active against nocardiae. Among the most recently developed antitubercular compounds, PA-824 {(S)-2-nitro-6-[4-(trifluoromethoxy)benzyloxy]-6,7-dihydro-5H-imidazo[2,1-b][1,3] oxazine} has shown the best and most promising results (4, 12). In vitro, those compounds present MIC values for Mycobacterium tuberculosis isolates similar to those of isoniazid (MIC of PA-824, 0.015 to 0.25 μg/ml; MIC of isoniazid, 0.03 to 0.06 μg/ml) (12). PA-824 acts as a prodrug activated through a bioreduction process within the M. tuberculosis cell, and it is efficient against both latent and replicating M. tuberculosis. Transcriptional analysis has revealed a mixed potential mechanism of action that operates both by affecting cell wall synthesis and by chemical poisoning. The latter is achieved by increasing the intracellular amount of toxic nitric oxide (NO) (7, 10, 11). The development of M. tuberculosis mutants and its whole-genome resequencing showed the importance of a gene named ddn (Rv3547) in PA-824 resistance. This gene encodes a 151-amino-acid protein, a deazaflavin-dependent nitroreductase (Ddn); orthologous genes have been found in other actinobacteria (7).
1,3-Benzothiazin-4-one (benzothiazinone [BTZ]) compounds have been recently described that have excellent activity against actinobacteria, including Corynebacterium, Mycobacterium, Rhodococcus, and Nocardia (6). They are particularly active against Mycobacterium tuberculosis in vitro and in vivo, with BTZ043 showing a MIC of 1 ng/ml for the control strain M. tuberculosis H37Rv. This value is far below that of other active drugs, including rifampin and isoniazid. The biochemical target, the decaprenyl-phosphoribose-2′-epimerase (encoded by gene dprE1), is commonly distributed among actinobacteria (6, 13).
In the present work, we analyze the susceptibility of 30 N. brasiliensis isolates from human mycetoma to these compounds by a broth microdilution method.
We studied 30 isolates from the collection of the Laboratorio Interdisciplinario de Investigación Dermatológica (LIID) of the Servicio de Dermatología, Hospital Universitario, Universidad Autónoma de Nuevo León (UANL), including N. brasiliensis HUJEG-1 utilized previously in other in vitro and in vivo assays (1, 9, 15). All the isolates came from human cases of actinomycetoma and were identified as N. brasiliensis by biochemical methods and by nucleotide sequence analysis of a fragment of the 16S rRNA gene as described before (14).
PA-824 was kindly donated by the Global Alliance for TB Drug Development; BTZ043 was provided by one of the authors of the present study.
The broth microdilution method based on the CLSI M24-A2 document that we used has been described before (3). As external controls, we used Escherichia coli ATCC 25922 and Staphylococcus aureus ATCC 29213. PA-824 was tested at concentrations of 64 to 0.25 μg/ml. In the case of BTZ043, the lowest concentration used was 0.0015 μg/ml. M. tuberculosis H37Rv was used also as a control.
The dprE1 gene from N. brasiliensis was obtained by comparing the dprE1 (locus Rv3790) gene sequence of M. tuberculosis H37Rv to the entire genome sequence of N. brasiliensis HUJEG-1 obtained by our group (16) by using the BLAST program available at the NCBI Internet site. To establish the presence of a putative ddn (Rv3547) ortholog in N. brasiliensis, we utilized the M. tuberculosis H37Rv nucleotide sequence published in GenBank and compared it to the complete chromosomal sequence of N. brasiliensis HUJEG-1 by the use of the BLAST program.
The MIC50 and MIC90 values of PA-824 for the N. brasiliensis isolates were >64 μg/ml in both cases. N. carnea ATCC 6847 and N. transvalensis ATCC 6865 showed the same MIC value. As a resistant control, we tested M. smegmatis LR222, for which the drug MIC was >64 μg/ml. The MIC value for the susceptible control, M. tuberculosis H37Rv, was 0.125 μg/ml.
The BTZ043 MIC50 and MIC90 values were 0.125 and 0.25 μg/ml, respectively. The MIC for N. carnea ATCC 6847 was 0.003 μg/ml, for N. transvalensis ATCC 6865 was 0.003 μg/ml, for N. brasiliensis NCTC10300 was 0.03 μg/ml, and for N. brasiliensis HUJEG-1 was 0.125 μg/ml. The MIC value for M. tuberculosis H37Rv was 0.000976 μg/ml. The MIC values of both PA-824 and BTZ-043 were >64 μg/ml for Escherichia coli ATCC 25922 and S. aureus ATCC 29213.
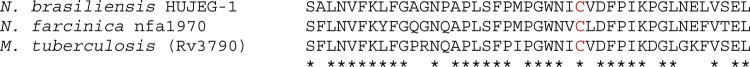
Comparing the M. tuberculosis dprE1 gene sequence to the complete sequence of N. brasiliensis, we found a sequence with 74% homology encoding a 493-amino-acid protein (accession number ZP_09840034.1) similar to the FAD binding 4 superfamily proteins of other actinobacteria, including Nocardia, Gordonia, Mycobacterium, Amycolatopsis, Corynebacterium, etc. In Fig. 1 we show the multiple alignment of the part of the DPR protein associated with BTZ043 resistance (6). The N. brasiliensis sequence presents a Cys (cysteine) in position 387 (of the M. tuberculosis H37Rv gene), which corresponds to a susceptible genotype.
Fig 1.
Alignment of the BTZ resistance-determining region of N. brasiliensis HUJEG-1 with the corresponding DPR protein sequences of N. farcinica and M. tuberculosis, both BTZ-sensitive organisms. In red we show the Cys387 amino acid related to resistance to this antimicrobial.
Analyzing the M. tuberculosis ddn gene sequence (Rv3547) by the use of the BLAST program against all the sequences reported in GenBank, only a few pertinent sequences were found, mostly from slowly growing mycobacteria. However, we could not find a ddn gene in the N. brasiliensis HUJEG-1 genome. PA-824 is one candidate for use in human cases of tuberculosis; a recent study in humans has demonstrated good early bactericidal activity and safety (4). Unfortunately, our results indicate a low susceptibility of N. brasiliensis isolates.
The emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains of M. tuberculosis has prompted the development of new antituberculosis compounds. Recently, drugs belonging to the class of benzothiazinones (BTZs) have been demonstrated to be highly active against M. tuberculosis in vitro, ex vivo, and in vivo (6). BTZs act by binding covalently to the enzyme DprE1(Rv3790) (13). This enzyme and DprE2 catalyze the conversion of decaprenylphosphoryl-d-ribose (DPR) to decaprenylphosphoryl-d-arabinose (DPA), which is essential for the building of arabinogalactan and lipoarabinomannan, important components of the mycobacterial cell wall. BTZ compounds bind to a cysteine residue at position 387 in the DprE1 active site, leading to the formation of a covalent complex. In M. tuberculosis BTZ-resistant mutants and in other mycobacteria that are naturally resistant, Cys387 of DprE1 is replaced by serine or glycine. In our case, we observed a susceptible genotype, demonstrating that the target is largely conserved among actinobacteria, and this raises the possibility that this drug is also active against N. brasiliensis ex vivo and in vivo in the experimental model of infection.
PA-824 was selected because it is being tested in clinical trials and may thus become available for tuberculosis patients. Unfortunately, the in vitro MIC values were too high against Nocardia spp., thereby decreasing the possibility of any in vivo activity. Resistance to PA-824 has been associated in M. leprae with the lack of an orthologous gene encoding Ddn, a nitro reductase (8); Ddn is essential for the anaerobic killing of M. tuberculosis by PA-824, which acts as a NO donor. Our group has recently sequenced the complete genome of N. brasiliensis HUJEG-1, which allowed us to search for a similar gene, but we did not find such a gene. The antimicrobial susceptibility of actinobacteria can be associated with common biochemical pathways such as cell-wall biogenesis (like BTZs) or with very specific genes such as ddn, found only in some mycobacteria. However, as we describe here, availability of the genome sequence can help in predicting antimicrobial susceptibility.
Footnotes
Published ahead of print 23 April 2012
REFERENCES
- 1. Almaguer-Chávez JA, et al. 2011. Decrease of virulence for BALB/c mice produced by continuous subculturing of Nocardia brasiliensis. BMC Infect. Dis. 11:290 doi:10.1186/1471-2334-11-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonifaz A, Flores P, Saúl A, Carrasco-Gerard E, Ponce RM. 2007. Treatment of actinomycetoma due to Nocardia spp. with amoxicillin-clavulanate. Br. J. Dermatol. 156:308–311 [DOI] [PubMed] [Google Scholar]
- 3. CLSI 2011. Susceptibility testing of mycobacteria, nocardia, and other aerobic actinomycetes; 108th approved standard—2nd ed. CLSI document M24 A-2 (ISBN 1-56238-746-4). Clinical and Laboratory Standards Institute, Wayne, PA: [PubMed] [Google Scholar]
- 4. Diacon AH, et al. 19 March 2012. A phase II dose-ranging trial of the early bactericidal activity of PA-824. Antimicrob. Agents Chemother. doi:10.1128/AAC.06125-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fuentes A, Arenas R, Reyes M, Fernández RF, Zacarías R. 2006. Actinomycetoma and Nocardia sp. Report of five cases treated with imipenem or imipenem plus amikacin. Gac. Med. Mex. 142:247–252 (In Spanish.) [PubMed] [Google Scholar]
- 6. Makarov V, et al. 2009. Benzothiazinones kill Mycobacterium tuberculosis by blocking arabinan synthesis. Science 8:801–804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Manjunatha U, Boshoff HI, Barry CE. 2009. The mechanism of action of PA-824: novel insights from transcriptional profiling. Commun. Integr. Biol. 2:215–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Manjunatha UH, et al. 2006. Mycobacterium leprae is naturally resistant to PA-824. Antimicrob. Agents Chemother. 50:3350–3354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Salinas-Carmona MC, Rocha-Pizaña MR. 2011. Construction of a Nocardia brasiliensis fluorescent plasmid to study Actinomycetoma pathogenicity. Plasmid 65:25–31 [DOI] [PubMed] [Google Scholar]
- 10. Singh R, et al. 2008. PA-824 kills nonreplicating Mycobacterium tuberculosis by intracellular NO release. Science 322:1392–1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stover CK, et al. 2000. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature 405:962–966 [DOI] [PubMed] [Google Scholar]
- 12. Tasneen R, et al. 2011. Sterilizing activity of novel TMC207- and PA-824-containing regimens in a murine model of tuberculosis. Antimicrob. Agents Chemother. 55:5485–5492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Trefzer C, et al. 2010. Benzothiazinones: prodrugs that covalently modify the decaprenylphosphoryl-β-D-ribose 2′-epimerase DprE1 of Mycobacterium tuberculosis. J. Am. Chem. Soc. 132:13663–13665 [DOI] [PubMed] [Google Scholar]
- 14. Vera-Cabrera L, Johnson WM, Welsh O, Resendiz-Uresti FL, Salinas-Carmona MC. 1999. Distribution of a Nocardia brasiliensis catalase gene fragment in members of the genera Nocardia, Gordona, and Rhodococcus. J. Clin. Microbiol. 37:1971–1976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vera-Cabrera L, Gonzalez E, Choi SH, Welsh O. 2004. In vitro activities of new antimicrobials against Nocardia brasiliensis. Antimicrob. Agents Chemother. 48:602–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vera-Cabrera L, Ortiz-Lopez R, Elizondo-González R, Perez-Maya AA, Ocampo-Candiani J. 2012. The complete genome sequence of Nocardia brasiliensis HUJEG-1. J. Bacteriol. 194:2761–2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Welsh O, Vera-Cabrera L, Salinas-Carmona MC. 2007. Mycetoma. Clin. Dermatol. 25:195–202 [DOI] [PubMed] [Google Scholar]