Abstract
As many as 9% of preschoolers suffer from an anxiety disorder, and earlier onset of disorder is associated with more intractable forms of psychopathology in later life. At present there is a relative dearth of empirical work examining the development of evidence-based treatments for anxiety disorders presenting in early childhood. Building on previous work supporting extensions of PCIT for separation anxiety disorder, the present study examines the preliminary feasibility and efficacy of an anxiety-based modification of PCIT (The CALM Program; Coaching Approach behavior and Leading by Modeling) for the treatment of youth between the ages of three and eight presenting with separation anxiety disorder, social anxiety disorder, generalized anxiety disorder, and/or specific phobias (N=9; Mage=5.4 years, ranging 4–8 years; 55.6% of families endorsing racial or ethnic minority status). Intent-to-treat (ITT; N=9) and treatment completer (N=7) analyses were conducted to evaluate diagnostic and functional response across participants. Pre- and posttreatment structured diagnostic interviews were conducted (ADIS-C/P), and clinical impression measures were completed (e.g., CGI, CGAS). Roughly 80% of the sample completed all treatment sessions. All treatment completers were categorized as global treatment responders by independent evaluators, with all but one showing full diagnostic improvements, and all but one showing meaningful functional improvements. These findings lend preliminary support for the promising role of live parent coaching for the treatment of a range of anxiety disorders that present in early childhood. Future work is needed to replicate the present findings in larger samples utilizing randomized controlled comparisons.
Keywords: Anxiety, Anxiety disorders, PCIT, Parent training, Preschool
1. Introduction
Anxiety disorders are the most prevalent category of mental health problems in the general population, collectively affecting up to 18% of individuals in a given year and 25% of individuals over a lifetime (Kessler, Chiu, Demler, & Walters, 2005; Kessler et al., 1994). Onset occurs mainly during childhood (Kessler et al., 2005) and is associated with considerable impairment in academic performance, peer relations, and family functioning (Grills & Ollendick, 2002). Children with anxiety disorders experience greater peer victimization and neglect (e.g., Storch et al., 2006) and are at elevated risk for the development of depression, sleep disturbance, and problematic substance use (e.g., Alfano, Ginsburg, & Kingery, 2007; Kaplow, Curran, Angold, & Costello, 2001; Kendall, Safford, Flannery-Schroeder, & Webb, 2004). When left untreated, childhood anxiety disorders can persist into adulthood, during which time they are associated with the presence of other psychiatric conditions (e.g., Compton, Thomas, & Stinson, 2007; Conway, Compton, & Stinson, 2006; Kessler et al., 2005) chronic physical comorbidities (Roy-Byrne et al., 2008), reduced health-related quality of life (Comer et al., 2011), and suicidality (Borges, Angst, Nock, Ruscio, & Kessler, 2008; Kessler, Borges, & Walters, 1999; Weissman, Klerman, Markowitz, & Ouellete, 1989). Earlier onset of disorder is associated with more intractable forms of psychopathology in later life (Kessler et al., 2005), and research suggests that as many as 9% of preschoolers suffer from an anxiety disorder (Egger & Angold, 2006).
Psychosocial treatments for childhood anxiety disorders have garnered strong empirical support for children over the age of seven (see Kendall, Furr, & Podell, 2010; Ollendick & King, 1998; Silverman, Pina, & Viswesvaran, 2008). These supported treatments are cognitive-behavioral in nature and help children to recognize bodily symptoms of anxiety, identify and adjust maladaptive cognitions in anxiety-provoking situations, and develop a repertoire of coping strategies. After learning this new skill set, treatment shifts to providing children with opportunities to practice these newly acquired skills in increasingly anxiety-provoking situations in the context of a therapeutically supportive relationship. Approximately 60–70% of youth over the age of seven treated with cognitive-behavioral therapies no longer meet criteria for an anxiety disorder following treatment (Kendall et al., 1997; Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008; Silverman et al., 1999; Walkup et al., 2008) and treatment gains are often maintained into adolescence and young adulthood (Kendall et al., 2004).
Unfortunately, there is a relative dearth of work examining the treatment of anxiety disorders in early childhood. Much of the published data on the treatment of anxiety disorders in early childhood to date is limited to descriptive presentations of individual cases (i.e., case reports) or case series focusing on an individual anxiety disorder (e.g., Choate, Pincus, Eyberg, & Barlow, 2005; Pincus, Eyberg, & Choate, 2005). Such work provides in-depth and theoretically rich direction for future work, but individual cases are limited in the extent to which findings can be generalized to inform clinical practice. Emerging data from controlled trials of selective prevention programs for very young children at risk for the development of anxiety disorders show enormous promise (Rapee, Kennedy, Ingram, Edwards, & Sweeney, 2010), but may be limited in the extent to which they can inform the treatment young children with diagnosed anxiety disorders at baseline. In recent years, a small handful of research groups have begun to show support for the use of developmentally sensitive downward extensions of treatments found to work with older youth in controlled trials with preschoolers diagnosed with anxiety disorders (e.g., Hirshfeld-Becker et al., 2010; Kennedy, Rapee, & Edwards, 2009), providing rigorous empirical support that early anxiety disorders are treatable. These treatments share a focus on greater parental involvement in treatment, directly targeting parenting practices believed to maintain child anxiety, parental anxiety management, and a higher emphasis on the role of parental modeling.
The limited focus on treating anxiety disorders in very young children, relative to in older children, is likely due in part to the fact that treatments demonstrating efficacy with youth above the age of seven rely heavily on strategies and tasks that are beyond the developmental capacities of younger children. Treatment tasks focusing on recognizing bodily symptoms of anxiety and identifying and adjusting maladaptive cognitions in anxiety-provoking situations require sophisticated metacognitive and receptive and expressive language abilities that are not present at earlier stages of cognitive development (Flavell, Miller, & Miller, 2001). In-session tasks that have children reflect on how other children might differentially construe feared situations require perspective-taking abilities that do not fully emerge until later childhood (Flavell et al., 2001; Zhang & Zheng, 1999). Moreover, restricted attention and organization skills characteristic of early childhood limit the extent to which young children are able to participate in homework tasks that are critical components of cognitive-behavioral therapies that have demonstrated efficacy with older youth (Shaw et al., 2007). Thus, therapies that place high emphasis on information processing and abstract thinking (i.e., those that have demonstrated great support with older youth) are likely limited in the extent to which they can effectively treat disorders in younger children (Kendall, Lerner, & Craighead, 1984; Shirk, 1999; Weisz & Weersing, 1999). In short, these effective child-focused treatments require a higher level of cognitive development than found in early childhood.
In contrast to the child anxiety disorders treatment literature, substantial gains have been made in the treatment of young children (i.e., ages 2–7) with disruptive behavior disorders (i.e., oppositional defiant disorder, conduct disorder) (Eyberg, Nelson, & Boggs, 2008). Notably, Parent-Child Interaction Therapy, or PCIT (Eyberg, 2010; McNeil & Hembree-Kigin, 2011), targets children’s maladaptive behavior by modifying parents’ behavior. Rather than directly engaging young children who have yet to develop key cognitive developmental abilities, PCIT focuses on reshaping the primary context in which young children’s development unfolds—specifically interactions between parent and child. PCIT incorporates components of play therapy into behavioral parent training. In this treatment, parent-training emphasizes positive attention, consistency, problem solving, and effective communication in parent-child interactions. Treatment provides real-time, in-session coaching of parents as the therapist monitors parent-child interactions from an observation room and provides live and individualized coaching via a bug-in-the-ear receiver worn by the parent. Early sessions focus on strengthening a positive and mutually rewarding parent-child relationship (Child Directive Interaction, or CDI). Parents learn to use selective attention to shape children’s functioning (e.g., praising wanted behavior, ignoring unwanted behavior) as well as incidental teaching (i.e., reinforcing children’s spontaneous positive behavior to increase the frequency). Treatment subsequently shifts to focus on consistency, effective communication, parent direction, and child compliance (Parent Directed Interaction, or PDI). Research supports the utility of PCIT in children ages 2–7, demonstrating its efficacy in treating disruptive behavior disorders (Eyberg et al., 2001; Hood & Eyberg, 2003; Nixon, Sweeny, Erickson, & Touyz, 2003). . Seventy percent of treated youth evidence clinical significant improvements, and treatment gains are maintained across time (Hood & Eyberg, 2003; Nixon, Sweeny, Erickson, & Touyz, 2004).
Modifying PCIT for the treatment of anxiety disorders in young childhood may be of tremendous clinical utility (e.g., Choate et al., 2005; Pincus et al., 2005). PCIT shapes children’s functioning by targeting parent behavior rather than directly engaging young children who have yet to develop key cognitive developmental capacities. In contrast to supported treatments for older youth with anxiety, PCIT does not require metacognitive or perspective taking abilities of the child, nor does it require the child to engage in abstract problem solving. In addition, research documents the profound influence parenting has on the development and maintenance of anxiety in children. Overinvolved, intrusive, overprotective, and controlling parenting is associated with anxiety disorders in youth (Hudson, Comer, & Kendall, 2008; McLeod, Wood, & Weisz, 2007; Moore, Whaley, & Sigman, 2004; Rapee, 1997; Siqueland, Kendall, & Steinberg, 1996; Wood, McLeod, Sigman, Hwang, & Chu, 2003). These studies find parents of anxious children grant less autonomy and take over tasks that children can normatively perform independently. In addition, parents of anxious youth are more likely to offer approval of children’s avoidance strategies during problem-solving activities (Dadds, Barrett, & Rapee, 1996). Such parenting behaviors limit children’s exposure to anxiety-provoking situations and their resolution and deny children mastery opportunities (i.e., opportunities to demonstrate for themselves that they can effectively navigate age-appropriate situations) (see Chorpita & Barlow, 1998 for a comprehensive review and model).
To date, no study has examined the efficacy of parent training and real-time, in-session coaching of parent-child interactions in the treatment of a range of anxiety disorders in early childhood. Initial case reports (Choate et al., 2005; Pincus et al., 2005) and a recently completed clinical trial limited solely to separation anxiety disorder (Pincus et al., 2010) suggest that modifying PCIT to treat anxiety in early childhood may produce diagnostic improvements at posttreatment and subsequent follow-up assessment. In these reports, children showed substantial reductions in fear and avoidance behavior as parents provided increased praise for children’s approach (i.e., non-anxious) behaviors. In a randomized controlled trial, Pincus et al. (under review) found separation anxious youth receiving modified PCIT showed significantly greater improvements in clinical severity and interference of their separation anxiety disorder relative to those in a waitlist condition. At posttreatment, 73% of children no longer met criteria for a clinical diagnosis of SAD, which was maintained at 3-month follow-up. No participants in the waitlist condition were diagnosis-free by at post-waitlist evaluation. Importantly, these evaluations were entirely confined to children presenting with separation anxiety—only one of the anxiety disorders that can present in early childhood.
Building on previous work supporting extensions of PCIT for separation anxiety disorder, the present study examines the preliminary feasibility and efficacy of the CALM Program (Coaching Approach behavior and Leading by Modeling), a modification of PCIT for the treatment of anxiety disorders in youth between the ages of three and eight, in an open pilot series (N=9). It was hypothesized that the CALM Program would prove to be acceptable to families—as demonstrated by minimal-to-standard attrition—and that the program would show success in redressing the problems of anxiety disorders in the young sample. Based on supported gains identified in older anxious children treated with behavioral and cognitive-behavioral interventions (Beidel, Turner, & Morris, 2000; Kendall et al., 2010; Walkup et al., 2008), and in treated children of similar age ranges (Hirshfeld-Becker et al., 2010; Pincus et al., 2010), we predicted that treated children in the present pilot study would show meaningful diagnostic and functional response. Specifically, we hypothesized that the majority of treated children would show at least principal diagnostic response (i.e., at posttreatment, child does not meet diagnostic criteria for principal disorder diagnosed in pretreatment diagnostic profile), and functional response as assessed via standard clinician rating scales.
2. Method
2.1. Participants
Participants included a racially and ethnically diverse sample of nine young children (6 females, 3 males) between the ages of 4 and 8 (Mage = 5.4, SD = 1.3), and their parents. Recruitment efforts sought children as young as 3 years of age, but no families with eligible three-year-old children presented to the clinic during the study period. Participating families sought treatment for their child’s anxiety at the Columbia University Clinic for Anxiety and Related Disorders (CUCARD). To maximize external validity, youth presenting with other diagnoses (e.g., oppositional defiant disorder) of lower clinical severity than a principal anxiety disorder were included. Inclusion criteria were: (1) child is between 3–8 (inclusive); (2) child meets diagnostic criteria for a principal anxiety disorder, as assessed by structured diagnostic interview; (3) child and participating parents are English-speaking, as the treatment to be administered was provided in English. Criteria for exclusion were: (1) presence of mood, attention, or disruptive behavior disorders in child that are more impairing than child anxiety disorder; (2) child currently receiving treatment for anxiety or mood symptoms elsewhere; (3) pervasive developmental disability concerns in child, as assessed by the Social Communication Questionnaire (Rutter, Bailey, & Lord, 2003); (4) severe functional impairments as assessed by a Children’s Global Assessment Scale (Shaffer et al., 1983) score < 55; (5) presence of medically related sleep or reflux disorder, as assessed by phone screen; and (6) the existence of an open case on the family in the NYC Administration for Children’s Services. Three families consented to study procedures but did not meet eligibility criteria. All three of these children met for a principal diagnosis of oppositional defiant disorder (i.e., with greater severity and impairment than all other diagnostic conditions), and two did not meet diagnostic criteria for any anxiety disorder. Racial and/or ethnic minority youth comprised 55.6% of the sample. In 88.9% of cases, both parents participated in treatment; for one case only the mother participated. Table 1 presents demographic characteristics by each participant. All procedures were approved by the Institutional Review Board of the New York State Psychiatric Institute.
Table 1.
Participant demographic characteristics
| ID | Gender | Age | Race/ethnicity | Parent participant(s) |
|---|---|---|---|---|
| 1 | Male | 4 years | Asian American | Mother, Father |
| 2 | Female | 4 years | Non-Hispanic White | Mother, Father |
| 3 | Female | 7 years | Non-Hispanic White | Mother, Father |
| 4 | Female | 5 years | African American | Mother, Father |
| 5 | Male | 8 years | Non-Hispanic White | Mother, Father |
| 6 | Male | 5 years | Latino | Mother |
| 7 | Female | 5 years | Non-Hispanic White | Mother, Father |
| 8 | Female | 6 years | Latino | Mother, Father |
| 9 | Female | 5 years | Latino | Mother, Father |
2.2. Measures
2.2.1. Diagnostic Outcomes
The Anxiety Disorders Interview Schedule for Children and Parents for DSM–IV (ADIS-C/P; Silverman & Albano, 1996) is a semistructured diagnostic interview that assesses child psychopathology in accordance with DSM–IV criteria, with a particularly thorough focus on internalizing disorders. In the present sample, we administered the ADIS-P (parent version) to collect data on parent reports of the child’s anxiety, mood, and disruptive behavior disorder symptoms. Diagnosticians assign diagnoses as per DSM-IV criteria and clinician severity ratings (CSRs) for each diagnosis on the basis of interview data and clinical judgment. CSRs range from 0 to 8; a CSR ≥ 4 denotes that the child meets full diagnostic criteria for that disorder (see Silverman & Albano, 1996). The anxiety disorders section of the ADIS-C/P for DSM–IV has demonstrated strong concurrent validity (Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). The interview has demonstrated good reliability for parent (κ= range from .65 to .88) (Silverman & Ollendick, 2005; Silverman, Saavedra, & Pina, 2001). In previous research on age ranges comparable to the present sample, the ADIS-P has been used successfully and has demonstrated favorable psychometric properties (Kennedy, Rapee, & Edwards, 2009; Rapee, Kennedy, Ingram, Edwards, & Sweeney, 2005, 2010; Pincus, Santucci, Ehrenreich, & Eyberg, 2008). As in these studies some ADIS items were slightly modified for developmental compatibility and impairment was judged from a developmentally sensitive perspective for young children. For example, while maintaining the structure and scoring system of the original ADIS-P, questions about dating, homework, tests, and staying home alone are omitted, and questions about anxiety and avoidance during circle time, when in a different store aisle from a parent, and when not holding a parent’s hand are added.
2.2.2. Global Functioning, Impairment, and Severity
The Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983) is a widely used measure of overall severity of child disturbance, providing a clinician-rated index of functioning. Scores range from 0–100, with higher scores indicating higher levels of functioning and lower scores indicating greater functional impairments. The CGAS has been used successfully to assess preschool functional impairment (e.g., Lavigne et al., 1996). The Clinical Global Impression-Severity and Improvement Scales (CGI-S and I) is the most widely used clinician-rated measure of treatment-related changes in functioning (Guy & Bonato, 1970). The CGI-S score rates illness severity on a 7-point scale, ranging from 1 (“normal”) to 7 (“among the most severely ill patients”). The CGI-I rates clinical improvement on a 7-point scale, ranging from 1 (“very much improved”) to 7 (“very much worse”).
2.3. Description of Intervention
The CALM Program (Puliafico, Comer, & Albano, 2008) is a 12-session manual-based modification of Parent-Child Interaction Therapy (PCIT; Eyberg, 2010; McNeil & Hembree-Kigin, 2011) for the treatment of anxious youth between the ages of three and eight. Building on previous success in modifying PCIT for the treatment of early separation anxiety disorder (Choate et al., 2005; Pincus et al., 2005, 2010), the CALM Program was designed to target young children presenting with separation anxiety disorder, social anxiety disorder, generalized anxiety disorder, and/or specific phobias. As in standard PCIT, the CALM Program provides behavioral parent training via real-time in-session coaching of parents as the therapist monitors parent-child interactions from an observation room and provides live and individualized coaching via a bug-in-the-ear receiver worn by the parent. Unlike standard PCIT and the work of Pincus and colleagues, the CALM Program does not address effective discipline practices (Parent-Directed Interaction, or PDI). Given the critical importance of exposure tasks in the treatment of child anxiety (Kendall et al., 2005, 2008; Silverman et al., 2008), the CALM program incorporates eight in-session exposure sessions during which time parents are live-coached in the promotion of brave child behaviors (e.g., approaching a feared situation—such as petting a large dog, talking to a stranger, entering a dark room, holding a spider, or talking to an unfamiliar peer) in increasingly challenging exposure tasks using a bug-in-the-ear receiver.
Table 2 presents an overview and outline of treatment components across the protocol. As in standard PCIT, early sessions in the CALM Program focus on strengthening a positive and mutually rewarding parent-child relationship (Child Directive Interaction, or CDI). Parents learn to use selective attention to shape children’s functioning (e.g., praising wanted behavior, ignoring unwanted behavior) as well as incidental teaching (i.e., reinforcing children’s spontaneous positive behavior to increase the frequency). Early sessions also incorporate psychoeducation about the nature of child anxiety, and involve the development of an individualized fear hierarchy, which in turn serves as a roadmap for the subsequent engagement in graduated exposure tasks.
Table 2.
CALM session content
| Session | Attending | Content |
|---|---|---|
| 1 | P only | CDI Teach + Exposure hierarchy building: (1) Orient parents to program; (2) Psychoeducation about anxiety and the family; (3) Introduce structure of exposure therapy and develop individualized fear hierarchy; (4) Teach parents CDI skills (Praise, Reflection, Imitation, Description, Enthusiasm); (4) Role play CDI skills; (5) Assign at-home CDI |
| 2 | P, C | CDI Coach 1: (1) Orient child to program; (2) Review child’s anxiety, child’s behavior, and at-home CDI from previous week; (3) Orient family to bug-in-the-ear coaching format; (4) Code parent CDI skills; (5) Live-coach parents in CDI; (6) Provide parent feedback; (7) Assign at-home CDI |
| 3 | P, C | CDI Coach 2 + Exposure preparation: (1) Review child’s anxiety, child’s behavior, and at-home CDI from previous week; (2) Code parent CDI skills; (3) Live-coach parents in CDI; (4) Provide parent feedback; (5) Prepare family for upcoming low-level in-session exposure; (6) Assign at-home CDI |
| 4 | P, C | CDI Coach 3 + Exposure session 1: (1) Review child’s anxiety, child’s behavior, and at-home CDI from previous week; (2) Code parent CDI skills; (3) Live-coach parents in CDI; (4) Live-coach parents in low-level exposure task; (5) Provide parent feedback; (6) Prepare family for upcoming low-level in-session exposure; (7) Assign at-home CDI |
| 5 | P, C | CDI Coach 4 + Exposure session 2: (1) Review child’s anxiety, child’s behavior, and at-home CDI from previous week; (2) Code parent CDI skills; (3) Live-coach parents in CDI; (4) Live-coach parents in low-level exposure task; (5) Provide parent feedback; (6) Prepare family for upcoming parent-only didactic session regarding the promotion of brave child behaviors in moderate-to-high level exposure tasks; (7) Assign at-home CDI |
| 6 | P only | DADS Teach session: (1) Review child’s anxiety, child’s behavior, and at-home CDI from previous week; (2) Introduce and teach parents DADS steps for the promotion of brave child behaviors; (3) Role-play DADS steps; (4) Prepare family for upcoming moderate-level exposure task; (5) Assign at-home CDI |
| 7 | P, C | DADS Coach 1 + Exposure session 3: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in moderate-level exposure task using DADS steps; (5) Provide parent feedback; (6) Prepare family for upcoming moderate-level in-session exposure; (7) Assign at-home CDI and at-home DADS practice in out-of-session exposure tasks |
| 8 | P, C | DADS Coach 2 + Exposure session 4: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in moderate-level exposure task using DADS steps; (5) Provide parent feedback; (6) Prepare family for upcoming high-level in-session exposure; (7) Assign at-home CDI and at-home DADS practice in out-of-session exposure tasks |
| 9 | P, C | DADS Coach 3 + Exposure session 5: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in high-level exposure task using DADS steps; (5) Provide parent feedback; (6) Prepare family for upcoming high-level in-session exposure; (7) Assign at-home CDI and at-home DADS practice in out-of-session exposure tasks |
| 10 | P, C | DADS Coach 4 + Exposure session 6: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in high-level exposure task using DADS steps; (5) Provide parent feedback; (6) Prepare family for upcoming high-level in-session exposure; (7) Assign at-home CDI and at-home DADS practice in out-of-session exposure tasks |
| 11 | P, C | DADS Coach 5 + Exposure session 7: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in high-level exposure task using DADS steps; (5) Provide parent feedback; (6) Prepare family for upcoming high-level in-session exposure; (7) Prepare family for upcoming final session; (7) Assign at-home CDI and at-home DADS practice in out-of-session exposure tasks |
| 12 | P, C | DADS Coach 6 + Exposure session 8: (1) Review child’s anxiety, child’s behavior, and at-home DADS practice from previous week; (2) Code parent CDI skills; (3) Brief live-coach of CDI; (4) Live-coach parents in high-level exposure task using DADS steps; (5) Provide parent feedback; (6) Review child’s progress in treatment; (7) Encourage continued practice of skills learned in treatment; (8) Graduation ceremony for family |
Note: CALM = Coaching Approach behavior and Leading by Modeling; CDI = Child Directed Interactions, P = Parent; C = Child; DADS steps = Describe situation, Approach situation, give Direct Command for child to join situation, provide Selective attention based on child’s performance.
What distinguishes the CALM Program from other family-based cognitive-behavioral therapies for early child anxiety (Hirshfeld-Becker et al., 2010; Pincus et al., 2010) is the systematic incorporation of real-time bug-in-the-ear parent-coaching during in-session exposure tasks. The therapist unobtrusively monitors the family during prepared exposure tasks from an adjacent observation room, providing live and individualized feedback to parents on the promotion of brave/approach behavior. Throughout, emphasis is placed on parental modeling of approach behaviors, effective communication in anxious situations, the provision of clear and direct expectations from parents about child approach behavior, and the key roles of praise following brave child behaviors and selective ignoring when confronted with anxious, avoidant, and whining child behaviors.
Parent-coached low-level exposures are initiated in the third session of treatment, and parents are encouraged to use CDI skills (Selective attention, Praise, Reflection, Imitation, Description) to begin differentially responding to children’s brave and anxious behavior. Prior to engagement in moderate-to-high exposure tasks, parents learn more directive and specific steps for promoting brave child behaviors during exposure tasks and in their lives—specifically, the DADS steps (Describe situation, Approach situation, give Direct Command for child to join situation, provide Selective attention based on child’s performance, such as labeled praise for bravery and selective ignoring for avoidant responses). As in supported exposure-based treatments for older anxious youth (Kendall et al., 2010), the family progresses toward increasingly feared items and situations on the child’s exposure hierarchy, gradually moving up to high-level exposure tasks by the end of treatment. A more thorough articulation of the treatment and case example is provided elsewhere (Puliafico, Comer, & Albano, 2011).
2.4. Procedure
Participating families were referred to CUCARD for child anxiety problems via community outreach efforts, including mailings to pediatricians to inform them of the study, presentations to school personnel and parenting groups, and media advertisements. Potential participants were screened by phone prior to scheduling of a baseline assessment to review their family’s appropriateness for the study. For those treatment-seeking families meeting initial criteria, an initial baseline assessment during which time the ADIS-P interview was conducted by an Independent Evaluator (IE)—a Ph.D.-level postdoctoral research fellow in clinical psychology with expertise in the assessment and treatment of pediatric anxiety disorders. The IE was blind to all treatment-related data across the study (e.g., therapist’s impressions; family’s compliance with treatment) and was directly trained on administration of the interview by one of the developers of the ADIS-P. The IE assigned diagnoses in accordance with the DSM-IV-TR, and completed the CGAS and CGI-S. To ensure stability of diagnoses and impairment prior to the initiation of treatment, a second baseline assessment (Baseline 2) was conducted prior to the first treatment session. The interval between Baseline 1 and Baseline 2 was determined randomly, ranging from 1 to 4 weeks (1-week interval: n=1; 2-weeks interval: n=4; 3-weeks interval: n=1; 4-weeks interval: n=3). The same IE conducted evaluations for each family across the three study points.
Between Baseline 2 and the posttreatment assessment (Posttreatment) participating families completed the CALM Program (Puliafico et al., 2011) as outlined above. Therapists included five Ph.D.-level clinical psychologists specializing in the treatment of pediatric anxiety disorders. Therapists completed 4 months of training in the treatment protocol, followed by weekly video-review supervision from the lead author of the CALM protocol. All treatment and assessment was provided to families free of cost. Study families completed an average of 10.3 treatment sessions (the two drop-outs completed an average of 4.5 sessions; treatment completers attended all 12 sessions).
2.5. Analysis
With participants beginning treatment at varying and randomly determined lengths from initial baseline assessment, the effect of an intervention is demonstrated when a change in each participant’s symptoms is obtained after treatment, and not before. The absence of change during the baseline interval demonstrates the stability of diagnosis and impairment prior to treatment onset; changes from pre-to-post-treatment are thus interpreted as treatment-related changes.
Participant responder status was determined across three dimensions: diagnostic responder status, functional responder status, and treatment responder status. Full diagnostic responders were those who met full diagnostic criteria for DSM-IV disorders at Baseline 1 and Baseline 2, but did not meet diagnostic criteria for any disorders at Posttreatment, as assessed by the ADIS-P. Principal disorder response referred to cases in which full diagnostic criteria for a principal disorder was met at Baseline 1 and Baseline 2, but not at Posttreatment. Comorbid disorder response referred to cases in which full diagnostic criteria were met for non-principal disorders at Baseline 1 and Baseline 2, but not at Posttreatment. In addition to evaluating diagnostic response at the participant level, we also computed the rate of response for each diagnosis across the sample.
Functional response was determined for each participant via the CGAS. With CGAS anchors set at 10-point intervals (Shaffer et al., 1983), we categorize functional responders as those participants whose CGAS score improved at least 10 points from Baseline 2 to Posttreatment. Treatment responders were those did not improve on the CGI-S or CGI-I during the baseline interval, but who scored ≤ 3 on the CGI-S (‘3’= mildly ill, ‘2’ = borderline ill, ‘1’ = normal, not ill at all) and the CGI-I (‘3’= minimally improved, ‘2’ = much improved, ‘1’ = very much improved) at Posttreatment.
Responder rates were calculated within the intent-to-treatment (ITT) sample (N=9) as well as within the subset of treatment completers (N=7; 77.8% of full sample). For ITT analyses, cases of attrition were conservatively counted as non-responders for all diagnostic, functional, and treatment responder outcomes. The two participants who withdrew from treatment were an average of 6 years of age (relative to 5.3 years for completers) and presented with an average of 3.5 disorders (relative to 2 disorders for completers). Both cases of attrition were female, relative to 57.1% of completers being female. Both cases of attrition were non-Hispanic white, whereas 71% of the completers endorsed ethnic or racial minority status. Both participants were assigned a CSR of 7 for their principal diagnosis, showed high comorbidity, and exhibited the lowest level of baseline global functioning included in the study.
3. Results
3.1. Diagnostic outcomes
Table 3 presents principal and comorbid diagnoses, by participant, at Baseline 1, Baseline 2, and Posttreatment. At Pretreatment, 66.7% of the sample met criteria for a principal or co-principal diagnosis of separation anxiety disorder, 33.3% had a principal or co-principal diagnosis of social anxiety disorder, and 11.1% had a principal diagnosis of specific phobia (natural environment – thunder/lightening). At Pretreatment, clinical severity ratings for principal diagnoses ranged from 4–7, with an average of 6.1 (SD=1.0). Comorbid diagnoses were common, with only two participants presenting with only a single anxiety disorder. Regardless of randomized baseline interval, no participants showed diagnostic profile changes in either direction from Baseline 1 to Baseline 2. Despite efforts to retain the entire sample across treatment, two participating families dropped out of treatment early and declined to participate in a Posttreatment assessment.
Table 3.
Diagnostic Outcomes across Baseline 1, Baseline 2, and Posttreatment
| ID | Pretreatment | Posttreatment | |
|---|---|---|---|
| Baseline 1 Diagnoses | Baseline 2 Diagnoses | Posttreatment Diagnoses | |
| 1 | Separation Anxiety Disorder (P) | Separation Anxiety Disorder (P) | No diagnosis |
| 2 | Social Anxiety Disorder (P) Separation Anxiety Disorder (C) |
Social Anxiety Disorder (P) Separation Anxiety Disorder (C) |
No diagnosis No diagnosis |
| 3 | Separation Anxiety Disorder (P) Generalized Anxiety Disorder (C) Obsessive-Compulsive Disorder (C) |
Separation Anxiety Disorder (P) Generalized Anxiety Disorder (C) Obsessive-Compulsive Disorder (C) |
[Attrition after session 3] |
| 4 | Social Anxiety Disorder (P) Generalized Anxiety Disorder (C) Separation Anxiety Disorder (C) |
Social Anxiety Disorder (P) Generalized Anxiety Disorder (C) Separation Anxiety Disorder (C) |
No diagnosis No diagnosis No diagnosis |
| 5 | Specific Phobia (Natural Environment) (P) | Specific Phobia (Natural Environment) (P) | Specific Phobia (P) |
| 6 | Separation Anxiety Disorder (P) | Separation Anxiety Disorder (P) | No diagnosis |
| 7 | Social Anxiety Disorder (P) Separation Anxiety Disorder (P) Oppositional Defiant Disorder (C) Selective Mutism (C) |
Social Anxiety Disorder (P) Separation Anxiety Disorder (P) Oppositional Defiant Disorder (C) Selective Mutism (C) |
[Attrition after session 6] |
| 8 | Separation Anxiety Disorder (P) Oppositional Defiant Disorder (C) School Refusal (C) Selective Mutism (C) |
Separation Anxiety Disorder (P) Oppositional Defiant Disorder (C) School Refusal (C) Selective Mutism (C) |
No diagnosis No diagnosis No diagnosis No diagnosis |
| 9 | Separation Anxiety Disorder (P) School Refusal (C) |
Separation Anxiety Disorder (P) School Refusal (C) |
No diagnosis No diagnosis |
Note: P = Principal Diagnosis; C = Comorbid Diagnosis
Among treatment completers, 85.7% (N=6) were full diagnostic responders, meeting full diagnostic criteria for DSM-IV anxiety disorders at Baseline 1 and Baseline 2, but not meeting diagnostic criteria for any disorders at Posttreatment. Accordingly, 85.7% of participants also showed principal disorder response and comorbid disorder response. Across completers, the average CSR reduction for principal diagnoses was 3.6 (SD=1.5). Among the completer sample, diagnostic response was 100% for the following disorders: separation anxiety disorder, social anxiety disorder, generalized anxiety disorder, selective mutism, and oppositional defiant disorder.
Within the ITT sample, 66.7% (N=6) were full diagnostic responders, meeting full diagnostic criteria for DSM-IV anxiety disorders at Baseline 1 and Baseline 2, but not meeting diagnostic criteria for any disorders at Posttreatment. Accordingly, 66.7% of participants also showed principal disorder response and comorbid disorder response. Across the ITT sample, the average CSR reduction for principal diagnoses was 2.8 (SD=2.0). Among the ITT sample, diagnostic response was 75% for separation anxiety disorder, 66.7% for social anxiety disorder, and 50% for selective mutism, generalized anxiety disorder, and oppositional defiant disorder.
3.2. Functional Outcomes and Global Response
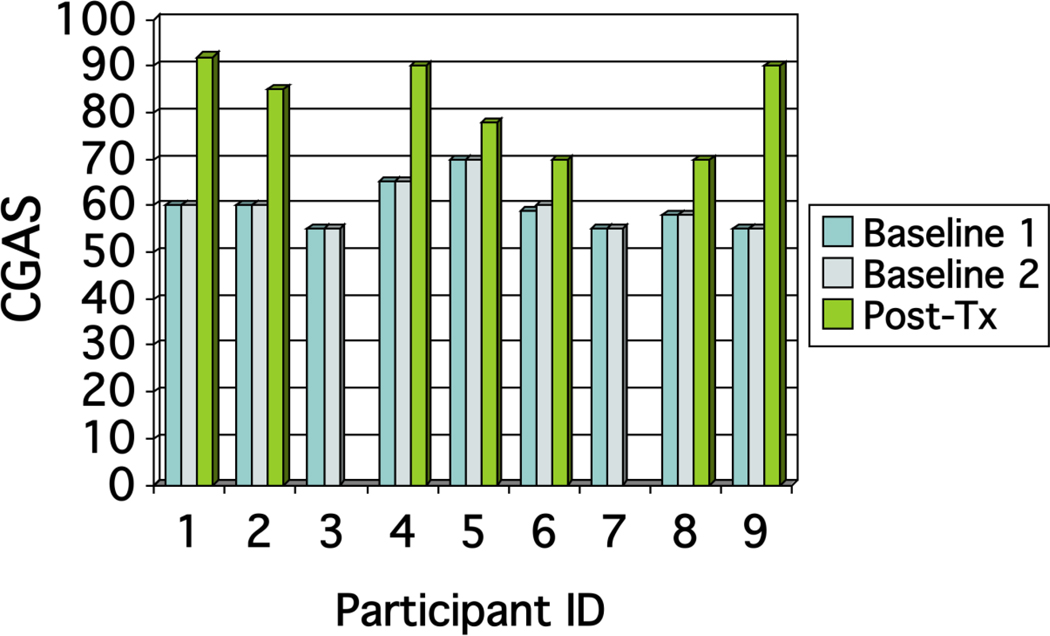
Figure 1 presents CGAS scores, by participant, at Baseline 1, Baseline 2, and Posttreatment. At Pretreatment, children’s global functioning was stable across the two baseline assessments, with a mean Pretreatment CGAS score of 61.4, which falls just above the category “Variable functioning with sporadic difficulties or symptoms in several but not all areas…” (Shaffer et al., 1983). Among treatment completers, children’s global functioning improved for all participants, with a mean improvement of 21.0 CGAS points (SD=11.0). The mean Posttreatment CGAS score across completers was 82.1, which falls in the category of “No more than slight impairments in functioning at home, at school, or with peers” (Shaffer et al., 1983). Among completers, 85.7% (N=6) were categorized as showing functional response—i.e., CGAS score improved at least 10 points from Baseline 2 to Posttreatment. The one treatment completer who was not categorized as a functional responder improved 8 CGAS points from Pre-to-Posttreatment. Among the ITT sample, when categorizing cases of attrition as functional non-responders, 66.7% of participants were functional responders.
Figure 1.
Improvements in global functioning by participant, across Baseline 1, Baseline 2, and Posttreatment
Note: CGAS= Children’s Global Assessment Scale; Post-Tx=Posttreatment; Participant 3 dropped out after session 3 (no posttreatment data available); Participant 7 dropped out after session 6 (no posttreatment data available)
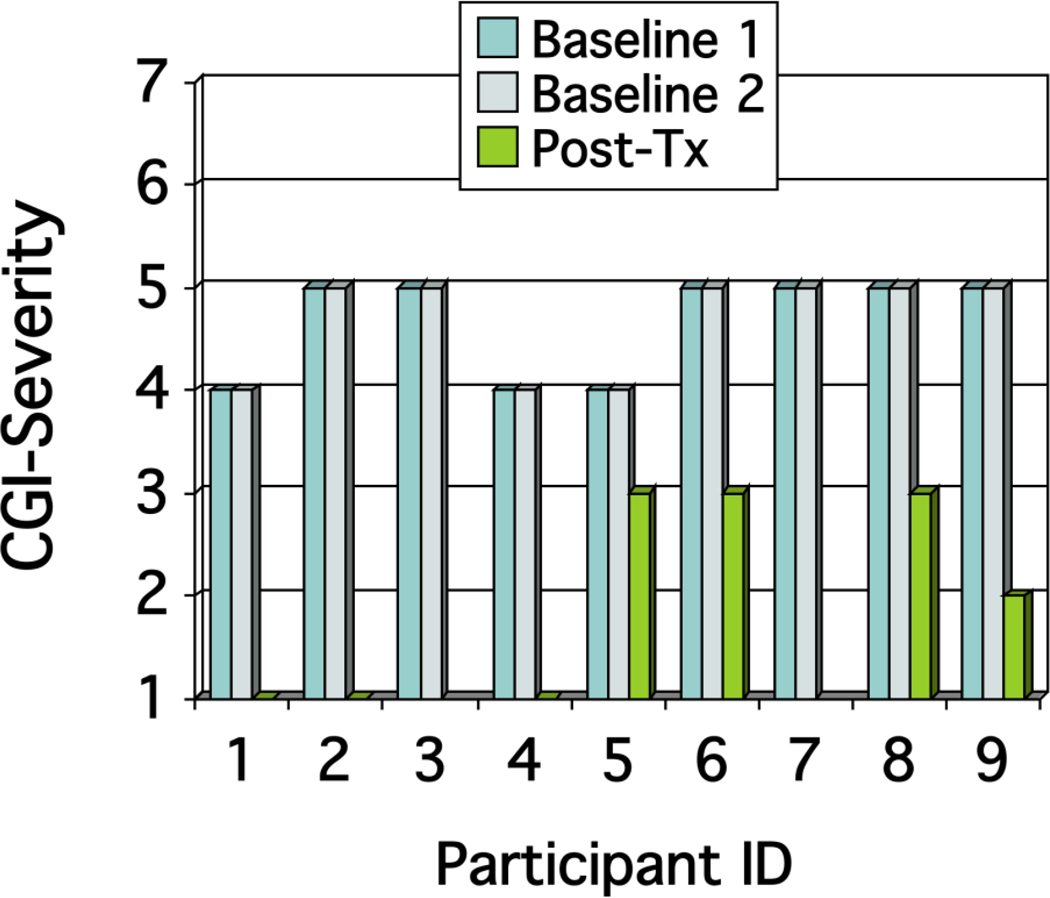
Figure 2 presents CGI-S scores, by participant, at Baseline 1, Baseline 2, and Posttreatment. At Pretreatment, children’s global severity was stable across the two baseline assessments, with a mean Pretreatment severity rating of 4.7 (SD=0.5), which characterizes the sample at Pretreatment as between the “Moderately ill” and “Markedly ill” categories (Guy & Bonato, 1970). Among treatment completers, children’s CGI-S ratings improved for all participants, with a mean improvement of 2.6 severity points on the 7-point CGI-S (SD=1.0). The mean Posttreatment CGI-S score across completers was 1.6, which falls between the category of “Normal, not at all ill” and “Borderline ill” (Guy & Bonato, 1970). Among completers, 100% scored lower than a 3 on the CGI-I at Posttreatment: 29% = 3 (“very much improved”), 29% = 2 (“much improved”), and 42% = 1 (“minimally improved”). No participants got worse, and no participants showed ‘no change. ’ Among treatment completers, 100% (N=7) were categorized as treatment responders—i.e., participants who did not improve on the CGI-S or CGI-I during the baseline interval, but who scored ≤ 3 on the CGI-S (‘3’= mildly ill, ‘2’ = borderline ill, ‘1’ = normal, not ill at all) and the CGI-I (‘3’= minimally improved, ‘2’ = much improved, ‘1’ = very much improved) at Posttreatment. Among the ITT sample, when categorizing cases of attrition as treatment non-responders, 77.8% of participants were treatment responders.
Figure 2.
Improvements in global severity by participant, across Baseline 1, Baseline 2, and Posttreatment
Note: CGI= Clinical Global Impression; CGI-Severity Key: 7 = Extremely ill, 6 = Severely ill, 5 = Markedly ill, 4 = Moderately ill, 3 = Mildly ill, 2 = Borderline ill, 1 = Normal not at all ill; Participant 3 dropped out after session 3 (no Posttreatment data available); Participant 7 dropped out after session 6 (no Posttreatment available)
4. Discussion
The present findings are promising in providing preliminary support for the feasibility and utility of modifying PCIT for the treatment of a range of anxiety disorders presenting in early childhood. Roughly 80% of the sample completed all treatment sessions, a retention rate comparable to that found in trials evaluating established treatments for older anxious youth (Kendall et al., 2008; Pina, Silverman, Weems, Kurtines, & Goldman, 2003). All treatment completers were categorized as global treatment responders, with all but one participant showing full diagnostic improvements on both principal and comorbid diagnoses that were stable at pretreatment, and all but one showing meaningful functional improvements. When considering the full sample regardless of dropout status, diagnostic and functional response rates were still comparable to those found in evaluations of established treatments for older anxious youth (Hudson et al., 2009; Kendall et al., 2008; Silverman et al., 2008; Walkup et al., 2008).
The present findings build on the innovative work of Pincus and colleagues modifying PCIT for the treatment of early separation anxiety (Choate et al., 2005; Pincus et al., 2005; Pincus et al., 2008), and support the promising role of live parent-coaching for the treatment of anxiety disorders that present in early childhood. The present study was novel in broadening the target of modified PCIT to include a range of common anxiety disorders, as well as in actually incorporating live, unobtrusive parent coaching during in vivo exposure tasks. Given the many anxiety disorders that present in early childhood (Egger & Angold, 2006), evaluating modified PCIT for a range of anxiety disorders may more fully address the needs of anxious youth in the community. The extent to which the incorporation of live bug-in-the-ear parent-coaching during in vivo exposure tasks is directly linked to treatment outcomes will require future empirical attention.
Notably, the one case of diagnostic and functional non-response among treatment completers presented with a principal diagnosis of specific phobia (natural environments – thunder/lightning). Importantly, there is evidence that among the specific phobias in childhood, specific phobias of natural environments may be particularly resistant to treatment (Ollendick, Raishevich, Davis, Sirbu, & Ost, 2009). It may be that specific phobias of natural environmental stimuli are more difficult to treat because of the difficulty inherent in creating realistic, anxiety-provoking exposure material in-session for these phobias. Future work with larger samples is needed to evaluate whether the different anxiety disorders are differentially responsive to the CALM Program, and to examine how the present transdiagnostic approach compares to single-disorder treatment approaches in this age group.
We conjecture that improvements in children associated with the CALM Program in our study were due in large part to the direct modifications made to parenting practices and parental reinforcement contingencies. Controlled evaluations with larger samples are needed to elucidate active mechanisms of treatment-related change, and to evaluate the extent to which parenting changes do indeed mediate child outcomes in CALM-treated families. Component analyses can also be useful in identifying which specific treatment ingredients are most associated with child changes. For example, our clinical experience supports the utility of live parent-coaching in exposure tasks for children in this age range, but less involved strategies for reshaping parenting practices may prove equally effective in reducing child anxiety symptoms. Moreover, given the role of parents as gatekeepers to child therapy, and as active participants in parent training programs such as the CALM Program, it will be important to evaluate any interactions between treatment outcome and parental sociodemographic and clinical characteristics (e.g., parent education, parent diagnostic status).
The CALM Program does not include teaching and coaching of Parent-Directed Interactions (PDI), which is a central component of traditional PCIT for oppositional youth. In PDI, parents are taught effective parental discipline techniques aimed at promoting child obedience and compliance. In the present PCIT modification, PDI sessions were not included so as to maximize the number of sessions in which families are engaged in exposure-based tasks. Notably, the PCIT modifications of Pincus and colleagues for early anxiety do include PDI sessions (Pincus et al., 2008). The extent to which it is necessary to systematically incorporate effective parental discipline practices into the treatment of early child anxiety remains unclear. Building on the promise of modularized therapies supported in the treatment of older youth (Chorpita, 2006), future research may do well to evaluate a modularized program in the treatment of early child anxiety, whereby the focus on effective parental discipline is incorporated only when the child presents with co-occurring disruptive behavior problems.
The present study is not without limitations. The design included multiple baseline assessments separated by randomly determined intervals, which demonstrates the effect of a treatment by showing that symptoms are stable prior to the implementation of treatment, and that change accompanies the introduction of treatment at different points in time. Participant symptoms across the baseline interval function as the participants own comparison data. This design provides incremental strengths over case studies, single case experimental designs, and ABAB designs (Kazdin, 2003), but the absence of a control condition equal in length to the duration of treatment cannot rule out the possibility that maturation and/or expectancy effects may have been associated with the observed changes, and the absence of an attention/support condition cannot rule out the possibility that nonspecific treatment factors may have been associated with changes. In addition, although the IE was blind to all treatment-related matters, he IE was not blind to assessment period. And thus it is possible that IE expectations could have exerted an influence on findings. Replication in larger samples is required before the effects identified can be interpreted as reflecting treatment efficacy (Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006), and future work is needed to evaluate the CALM Program utilizing randomized controlled comparisons and incorporating parent-report measures and structured behavioral observations.
Children ranging in age from 4 to 8 years were included, although the present sample size does not permit a detailed evaluation of treatment effects as a function of child age or developmental competencies. Notably, the one treatment completer who did not show full diagnostic improvements was the oldest child in the study. It may be that children in the upper limit of this age range benefit less from an entirely parent-focused anxiety treatment approach, and instead should be directed toward supported interventions that directly engage the child (e.g., Beidel, Turner, & Morris, 2000; Kendall et al., 2010). Future work is needed to evaluate the efficacy of the CALM Program in the context of developmental considerations, and to help identify which treatment approaches are best suited for children at the threshold of early to middle childhood.
The average pretreatment global severity rating of 4.7 fell just below the “markedly ill” range. Although the global severity of some individuals in this study certainly ranged higher, future work will be needed to evaluate the CALM Program in anxious samples showing, on average, more severe baseline global severity in order to speak to the generality of findings to more severe populations.
The attrition rate in the current trial was roughly 20%. Although this attrition rate is roughly comparable to that found in other efforts in this area (Kendall et al., 2008; Pina et al., 2003), it might nonetheless reflect needed improvements in the feasibility and/or appropriateness of the CALM Program for all families characterized by the present inclusion/exclusion criteria. Notably, the two participants who withdrew from treatment appeared to be the two most severe cases at baseline. Both participants were assigned a CSR of 7 for their principal diagnosis, showed high comorbidity, and exhibited the lowest level of baseline global functioning included in the study. In addition, one of the two cases of attrition presented with comorbid, but sub-principal, obsessive-compulsive disorder. The CALM Program does not directly target OCD symptoms, and it may be that when OCD is present in early childhood, whether it is principal or comorbid, familybased exposure and response prevention protocol should be implemented (Freeman & Garcia, 2009). Further data on treatment satisfaction and barriers to care are needed to determine the extent to which the CALM Program requires modification and/or the target population criteria requires adjustment.
The proportion of very young children prescribed psychotropic medications in outpatient care has been steadily increasing in recent years (Olfson, Blanco, Liu, Moreno, Laje, 2006; Olfson, Crystal, Huang, & Gerhard, 2010; Olfson, Marcus, Weissman, & Jensen, 2002). Recent trends, particularly in the off-label prescribing of psychotropic medications for early child anxiety disorders, may be due, in part, to the relative dearth of supported psychosocial interventions for this clinical population. Expert consensus treatment algorithms do recommend non-pharmacologic interventions as the first-line treatment for pediatric anxiety disorders presenting in the preschool years (Gleason et al., 2007), but these guidelines have nonetheless noted that empirical support for psychosocial interventions for preschoolers with non-PTSD, non-OCD anxiety disorders is limited. The current study adds to a growing body of literature supporting the use of cognitive and behavioral methods with parent involvement in the treatment of early childhood anxiety disorders (Choate et al., 2005; Freeman et al., 2007; Hirshfeld-Becker et al., 2010; Kennedy et al., 2009; Pincus et al., 2005; Pincus et al., 2008; Scheeringa, 1999; Scheeringa et al., 2007). Importantly, the emerging set of controlled evaluations in this area (Freeman et al., 2007; Hirshfeld-Becker et al., 2010; Kennedy et al., 2009; Pincus et al., 2008) have found gains comparable to gains reported in evaluations of CBTs for older youth (Hudson et al., 2009; Kendall et al., 2008; Silverman et al., 2008; Walkup et al., 2008).
Highlights.
The CALM Program (Coaching Approach behavior and Leading by Modeling) is a 12-session modification of Parent-Child Interaction Therapy (PCIT) developed for the treatment of anxious youth between the ages of three and eight presenting with separation anxiety disorder, social anxiety disorder, generalized anxiety disorder, and/or specific phobias.
The present study examined the preliminary feasibility and efficacy of the CALM Program in a sample of anxious youth ages 4–8 years (M = 5.4; N=9).
Roughly 80% of the sample completed all treatment sessions. All treatment completers were categorized as global treatment responders by independent evaluators, with all but one showing full diagnostic improvements, and all but one showing meaningful functional improvements.
Findings lend preliminary support for the promising role of live parent coaching for the treatment of a range of anxiety disorders that present in early childhood.
Acknowledgments
This project was supported by a foundation grant from the Mental Health Initiative (MINT) awarded to Jonathan S. Comer, and by the National Institutes of Health (T32 MH016434). The authors wish to thank Sheila Eyberg, Philip Kendall, Steven Kurtz, Cheryl McNeil, and Timothy Verduin for their helpful comments on earlier versions of this work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:224–232. doi: 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. Journal of Consulting and Clinical Psychology. 2000;68:1072–1080. [PubMed] [Google Scholar]
- Borges GA, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: A 10-year follow-up study using the National Comorbidity Surveys. Journal of Affective Disorders. 2008;105:25–33. doi: 10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choate ML, Pincus DB, Eyberg SM, Barlow DH. Parent-Child Interaction Therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice. 2005;12:126–135. [Google Scholar]
- Chorpita BF. Modular cognitive-behavioral therapy for childhood anxiety disorders. New York: Guilford; 2006. [Google Scholar]
- Chorpita BF, Barlow DH. The development of anxiety: The role of control in the early environment. Psychological Bulletin. 1998;124:3–21. doi: 10.1037/0033-2909.124.1.3. [DOI] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Grant B, Hasin D, Liu SM, Turner JB, Olfson M. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2011;72:43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:247–258. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Barrett PM, Rapee RM. Family process and child anxiety and aggression: An observational analysis. Journal of Abnormal Child Psychology. 1996;24:715–734. doi: 10.1007/BF01664736. [DOI] [PubMed] [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47:313–337. doi: 10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Eyberg SM. Parent-Child Interaction Therapy: Integrity Checklists and Session Materials, Version 2.10. Gainesville, FL: PCIT International; 2010. [Google Scholar]
- Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, Hood K. Parent-child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child and Family Behavior Therapy. 2001;23:1–20. [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescetn Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Flavell JH, Miller PH, Miller SA. Cognitive Development. 4th edition. New York, NY: Prentice Hall; 2001. [Google Scholar]
- Freeman JB, Choate-Summers ML, Moore PS, Garcia AM, Sapyta JJ, Leonard H, Franklin ME. Cognitive behavioral treatment for young children with obsessive-compulsive disorder. Biological Psychiatry. 2007;61:337–343. doi: 10.1016/j.biopsych.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman JB, Garcia AM. Family-based treatment for young children with OCD. New York: Oxford University Press; 2009. [Google Scholar]
- Gleason MM, Egger HL, Emslie GJ, Greenhill LL, Kowatch RA, Lieberman, Zeanah CH. Pharmacological treatment for very young children: Contexts and guidelines. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1532–1572. doi: 10.1097/chi.0b013e3181570d9e. [DOI] [PubMed] [Google Scholar]
- Grills AE, Ollendick TH. Peer victimization, global self-worth, and anxiety in middle school children. Journal of Clinical Child and Adolescent Psychology. 2002;31:59–68. doi: 10.1207/S15374424JCCP3101_08. [DOI] [PubMed] [Google Scholar]
- Guy W, Bonato, editors. Clinical Global Impressions. Chevy Chase, MD: National Institute of Mental Health; 1970. [Google Scholar]
- Hirshfeld-Becker DR, Masek B, Henin A, Blakely LR, Pollock-Wurman RA, McQuade J, Biederman J. Cognitive behavioral therapy for 4- to 7-year-old children with anxiety disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2010;78:498–510. doi: 10.1037/a0019055. [DOI] [PubMed] [Google Scholar]
- Hood K, Eyberg SM. Outcomes of parent-child interaction therapy: Mothers’ reports on maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Comer JS, Kendall PC. Parental responses to positive and negative emotions in anxious and nonanxious children. Journal of Clinical Child and Adolescent Psychology. 2008;37:303–313. doi: 10.1080/15374410801955839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM, Deveney D, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:533–544. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. Journal of Clinical Child Psychology. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Research Design in Clinical Psychology, 4th Edition. Boston, MA: Allyn & Bacon; 2003. [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youth with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Furr JM, Podell JL. Child-focused treatment of anxiety. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolecents, 2nd Edition. New York, NY: Guilford Press; 2010. [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Lerner R, Craighead WE. Human development and intervention in childhood psychopathology. Child Development. 1984;55:71–82. [PubMed] [Google Scholar]
- Kendall PC, Robin J, Hedtke K, Suveg C, Flannery-Schroeder E, Gosch E. Considering CBT with anxious youth? Think exposures. Cognitive and Behavioral Practice. 2005;12:136–148. [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: Outcomes in adolescence and impact on substance use and depression at 7.4-year-follow-up. Journal of Consulting and Clinical Psychology. 2004;72:276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- Kennedy SJ, Rapee RM, Edwards SL. A selective intervention program for inhibited preschool-aged children of parents with an anxiety disorder: Effects on current anxiety disorders and temperament. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:602–609. doi: 10.1097/CHI.0b013e31819f6fa9. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distribution of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Gibbons RD, Christoffel KK, Arend R, Rosenbaum D, Binns H, Isaacs C. Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child Adolescent Psychiatry. 1996;35:204–214. doi: 10.1097/00004583-199602000-00014. [DOI] [PubMed] [Google Scholar]
- Manassis K, Hudson JL, Webb A, Albano AM. Beyond behavioral inhibition: Etiological factors in childhood anxiety. Cognitive and Behavioral Practice. 2004;11(1):3–12. [Google Scholar]
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007;27:155–172. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- McNeil CB, Hembree-Kigin TL. Parent-Child Interaction Therapy. New York, NY: Springer; 2011. [Google Scholar]
- Moore PS, Whaley SE, Sigman M. Interactions between mothers and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology. 2004;113:471–476. doi: 10.1037/0021-843X.113.3.471. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Sweeny L, Erickson DB, Touyz SW. Parent-child interaction therapy: A comparison of standard and abbreviated treatments for oppositional defiant preschoolers. Journal of Consulting and Clinical Psychology. 2003;71:251–260. doi: 10.1037/0022-006x.71.2.251. [DOI] [PubMed] [Google Scholar]
- Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-child interaction therapy: One- and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. Journal of Abnormal Child Psychology. 2004;32:263–271. doi: 10.1023/b:jacp.0000026140.60558.05. [DOI] [PubMed] [Google Scholar]
- Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Archives of General Psychiatry. 2006;63:679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- Olfson M, Crystal S, Huang C, Gerhard T. Trends in antipsychotic drug use by very young, privately insured children. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:13–23. doi: 10.1097/00004583-201001000-00005. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. Journal of the American Academy of Child and Adolscent Psychiatry. 2002;41:514–521. doi: 10.1097/00004583-200205000-00008. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, King NJ. Empirically supported treatments for children with phobic and anxiety disorders: Current status. Journal of Clinical Child Psychology. 1998;27:156–167. doi: 10.1207/s15374424jccp2702_3. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Raishevich N, Davis TE, Sirbu C, Ost LG. Specific phobia in youth: Phenomenology and psychological characteristics. Behavior Therapy. 2009;41:133–141. doi: 10.1016/j.beth.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Weems CF, Kurtines WM, Goldman ML. A comparison of completers and noncompleters of exposure-based cognitive and behavioral treatment for phobic and anxiety disorders in youth. Journal of Consulting and Clinical Psychology. 2003;71:701–705. doi: 10.1037/0022-006x.71.4.701. [DOI] [PubMed] [Google Scholar]
- Pincus DB, Chase R, Chow CW, Weiner CL, Cooper-Vince C, Eyberg SM. Efficacy of modified Parent-Child Interaction Therapy for young children with separation anxiety disorder. Paper presented at the the 44th annual meeting of the Association of Behavioral and Cognitive Therapies; San Francisco, CA. 2010. Nov, [Google Scholar]
- Pincus D, Eyberg SM, Choate ML. Adapting Parent-Child Interaction Therapy for Young Children with separation anxiety disorder. Education and Treatment of Children. 2005;28:163–181. [Google Scholar]
- Pincus D, Santucci LC, Ehrenreich JT, Eyberg SM. The implementation of modified Parent-Child Interaction Therapy for Youth with separation anxiety disorder. Cognitive and Behavioral Practice. 2008;15:118–125. [Google Scholar]
- Puliafico AC, Comer JS, Albano AM. Coaching Approach behavior and Leading by Modeling: The CALM Program for anxious preschoolers. New York, NY: Columbia University; 2008. [Google Scholar]
- Puliafico AC, Comer JS, Albano AM. Coaching Approach behavior and Leading by Modeling: Rationale, principals, and a case example of The CALM Program for anxious preschoolers. Manuscript under review. 2011 [Google Scholar]
- Rapee RM. Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review. 1997;17:47–67. doi: 10.1016/s0272-7358(96)00040-2. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy S, Ingram M, Edwards SL, Sweeney L. Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology. 2005;73:488–497. doi: 10.1037/0022-006X.73.3.488. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy SJ, Ingram M, Edwards SL, Sweeney L. Altering the trajectory of anxiety in at-risk young children. American Journal of Psychiatry. 2010;167:1518–1525. doi: 10.1176/appi.ajp.2010.09111619. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJG, Goodwin RD, Kubzansky L, Stein MB. Anxiety disorders and comorbid medical illness. General Hospital Psychiatry. 2008;30:208–225. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. Social Communication Questionnaire. Los Angelos, CA: Western Psychological Services; 2003. [Google Scholar]
- Scheeringa MS. Treatment for posttraumatic stress disorder in infants and toddlers. Journal of Systemic Therapies. 1999;18:20–31. [Google Scholar]
- Scheeringa MA, Salloum A, Arnberger RA, Weems CF, Amaya-Jackson L, Cohen JA. Feasibility and effectiveness of cognitive-behavioral therapy for posttraumatic stress disorder in preschool children: Two case reports. Journal of Traumatic Stress. 2007;20:631–636. doi: 10.1002/jts.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children’s Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, Rapoport JL. Attention-deficit hyperactivity disorder is characterized by a delay in cortical maturation. Proceedings of the National Academy of Sciences. 2007;104:19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirk SR. Developmental therapy. In: Silverman WK, Ollendick TH, editors. Developmental issues in the clinical treatment of children. Boston, MA: Allyn &Bacon; 1999. [Google Scholar]
- Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 1999;67:995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ollendick TH. Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:380–411. doi: 10.1207/s15374424jccp3403_2. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2008;37:105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Siqueland L, Kendall PC, Steinberg L. Anxiety in children: Perceived family environments and observed family interaction. Journal of Clinical Child Psychology. 1996;25:225–237. [Google Scholar]
- Storch EA, Ledley DR, Lewin AB, Murphy TK, Johns NB, Goodman WK, Geffken GR. Peer victimization in children with obsessive-compulsive disorder: Relations with symptoms of psychopathology. Journal of Clinical Child and Adolescent Psychology. 2006;35:446–455. doi: 10.1207/s15374424jccp3503_10. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Weersing VR. Developmental outcome research. In: Silverman WK, Ollendick TH, editors. Developmental issues in the clinical treatment of children. Boston, MA: Allyn & Bacon; 1999. [Google Scholar]
- Wood JJ, McLeod BD, Sigman M, Hwang WC, Chu BC. Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry. 2003;44:134–151. doi: 10.1111/1469-7610.00106. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Zhang WW, Zheng J. The development of children’s social perspective taking and the differences between perspective taking subtypes. Psychological Science. 1999;22:116–119. [Google Scholar]