Abstract
Objective
Behavioral weight loss programs (BWL) provide limited instruction on how to change the environmental context of weight-regulating behaviors, perhaps contributing to regain. Drawing on social ecological models, this trial evaluated a comprehensive weight loss program that targeted both an individual’s behavior and their physical and social home environment.
Methods
Overweight and obese adults (N=201; 48.9±10.5 years; 78.1% women) were randomized to BWL or to BWL plus home environment changes (BWL+H). Groups met weekly for 6 months and bi-monthly for 12 months. BWL+H participants were given items to facilitate healthy choices in their homes (e.g., exercise equipment, portion plates) and attended treatment with a household partner. Weight loss at 6 and 18 months was the primary outcome.
Results
BWL+H changed many aspects of the home environment and produced better 6 month weight losses than BWL (p=.017). At 18 months, no weight loss differences were observed (p=.19) and rates of regain were equivalent (p=.30). Treatment response was moderated by gender (6 month p=.01; 18 month p=.006). Women lost more weight in BWL+H than BWL at 6 and 18 months, whereas men in BWL lost more weight than those in BWL+H at 18 months. Partners, regardless of gender, lost more weight in BWL+H than BWL at both time points (ps<.0001).
Conclusion
The home food and exercise environment is malleable and targeting this microenvironment appears to improve initial weight loss, and in women, 18-month outcomes. Research is needed to understand this gender difference and to develop home-focused strategies with more powerful and sustained weight loss effects.
Keywords: weight loss, home environment, maintenance
The prevalence of overweight and obesity in U.S. adults now exceeds 65% (Flegal, Carroll, Ogden, & Curtin, 2010) with current estimates suggesting that the entire U.S. adult population will reach an unhealthy weight status by 2048 (Wang, Beydoun, Liang, Caballero, & Kumanyika, 2008). Drivers of this trend are multi-faceted, ranging from individual behavioral choices to community land-use planning decisions to global food production practices that promote energy imbalance (e.g., Swinburn et al., 2011). Behavioral weight loss treatment (BWL), the treatment of choice for overweight to moderately obese individuals, includes nutrition and physical activity education and instruction in behavioral strategies to facilitate change, and produces weight losses of approximately 9.0 kg over 6 months of treatment (e.g., Wing, Gorin, & Tate, 2006). While BWL’s modest weight losses and accompanying physical activity and dietary changes produce meaningful health improvements (e.g., Diabetes Prevention Program Research Group, 2002; Look AHEAD Research Group, 2007), participants typically regain 30–50% of their weight loss over the next 3 to 5 years despite ongoing intervention (e.g., Look AHEAD Research Group, 2010).
One possible explanation for this weight regain is that BWL focuses primarily on the individual participant, with lesser attention paid to the environmental context in which eating and exercise occurs. While behavioral theory and early weight loss programs emphasized the impact of environmental antecedents and consequences on behavior (e.g., Stuart & Davis, 1972), in current practice, individuals are given limited instruction on how to modify their surroundings to support weight-regulating behaviors. In a standard 6-month program, 1 to 2 sessions are typically dedicated to stimulus control skills (e.g. placing fruits and vegetables in prominent locations), (Wing, Gorin, & Tate, 2006). If weight loss participants are unable to use these skills to alter their personal environments, unhealthy cues and temptations may remain making it extremely difficult to establish and maintain the behavioral changes necessary to produce long-term weight loss (e.g., Bouton, 2000; Lowe, 2003).
This individual-level approach to weight management is inconsistent with the growing recognition of the environment’s contribution to the obesity epidemic (e.g., French, Story, & Jeffery, 2001; Swinburn et al., 2011). American adults are described as living in a “toxic environment” that encourages passive overeating and physical inactivity (Wang & Brownell, 2005). Social ecological models of health promotion (Breslow, 1996; Stokols, 2000) identify several levels of environmental influence on diet and physical activity, ranging from familial to global factors. At the most proximal level, there is increasing evidence that the home microenvironment can be obesogenic. Both physical (e.g., type of food available) and social (e.g., support from family) factors in this setting have been associated with weight, dietary habits, and activity patterns (e.g., Campbell, Crawford, Salmon, Carver, Garnett, & Baur, 2007; Gorin, Phelan, Raynor, & Wing, 2011). Demonstrated links between the physical home environment and behavior include relationships between high fat foods available and fat intake (Fulkerson et al., 2008), access to home exercise equipment and activity levels (Gattshall et al., 2008; Jakicic, Wing, Butler, & Jeffery, 1997), and number of televisions and amount of TV viewing (Dennison, Erb, & Jenkins, 2002). With regards to social factors, adults within the same household can serve as powerful behavioral cues and either facilitate or hinder adoption of healthy habits. For example, both weight gain and weight loss appear to spread among spouses (Christakis & Fowler, 2007; Gorin et al., 2008) and correlations have been reported between husbands and wives in caloric intake, dietary restraint, and exercise frequency (e.g., Macken et al., 2000; Markey, Markey, & Birch, 2001).
Given that approximately two-thirds of daily calories are consumed in the home and a large percentage of leisure time is spent in this environment (Biing-Hwan, Geuthri, & Frazao, 1999; Robinson & Godbey, 1997), modifying households to promote healthy choices is a logical step in moving toward a broader ecological model of weight management. Weight loss programs that have included home environment modifications such as food provision, provision of exercise equipment, and involving spouses in treatment have produced better overall weight losses for up to 18 months than standard behavioral programs, particularly in women (Black, Gleser, & Kooyers, 1990; Jakicic, Winters, Lang, & Wing, 1999); however these strategies have been largely unsuccessful in producing better maintenance of weight loss. Environmental manipulations to date have typically focused on either a single physical factor in the home (such as provision of food or exercise equipment) or on the social climate of the home (spouse involvement in treatment). This singular focus may not change the overall obesogenic nature of the household, leaving participants vulnerable to environmental influence. Moreover, this singular focus does not address the interaction between physical and social factors within the home (e.g., food provision may be unsuccessful if family members bring tempting foods into the home). Ecological models suggest that interventions will be most effective in changing behavior if they address multiple factors within a given environment, thus to examine the true potential of home environment manipulations in obesity treatment, a more comprehensive intervention targeting several aspects within the household may be needed.
The primary aim of this randomized controlled trial was to examine the long-term impact of a comprehensive home-focused behavioral weight control program designed to directly modify both the physical and social home environments of weight loss participants. To our knowledge, this is the first weight loss program to intervene simultaneously on multiple levels of the home environment while also teaching participants core behavioral skills. We hypothesized that by extending the focus of treatment from the individual participant to the participant plus their home environment, the intervention would enhance initial and long-term weight loss outcomes and improve maintenance of weight loss compared to standard behavioral weight loss treatment. Prior research has suggested that women may benefit more from a home-based approach (Wing, Marcus, Epstein, & Jawad, 1991), thus secondary analyses explored gender as a potential treatment moderator. We also examined potential effects on household partners and hypothesized that greater weight loss and behavior changes would be observed in partners who were actively included in the intervention.
Methods
Participants
Participants were recruited through advertisements in the local media and direct mailings in the Providence, Rhode Island area. To be eligible, individuals had to be between 21–70 years old, have a body mass index (BMI) between 25–50 kg/m2, and have a household member willing to participate in the study as a support partner. These partners had to reside in the same home as the participant, be between 15–70 years old, have a BMI between 25–50 kg/m2, and be interested in weight loss. With the exception of the lower age limit, the same inclusion and exclusion criteria applied to both participants and partners. Individuals were excluded from participation if they reported a heart condition, chest pain during periods of activity or rest, loss of consciousness, being unable to walk 2 blocks without stopping, current participation in another weight loss program and/or taking weight loss medication, current pregnancy or planning on becoming pregnant in the next 18 months, or any condition that in the judgment of the research team made it unlikely the individual would complete the study protocol (i.e., plans to relocate, substance abuse). Individuals endorsing joint problems, prescription medication usage, or other conditions that could limit exercise were required to obtain written physician consent to participate. The study was approved by The Miriam Hospital’s Institutional Review Board.
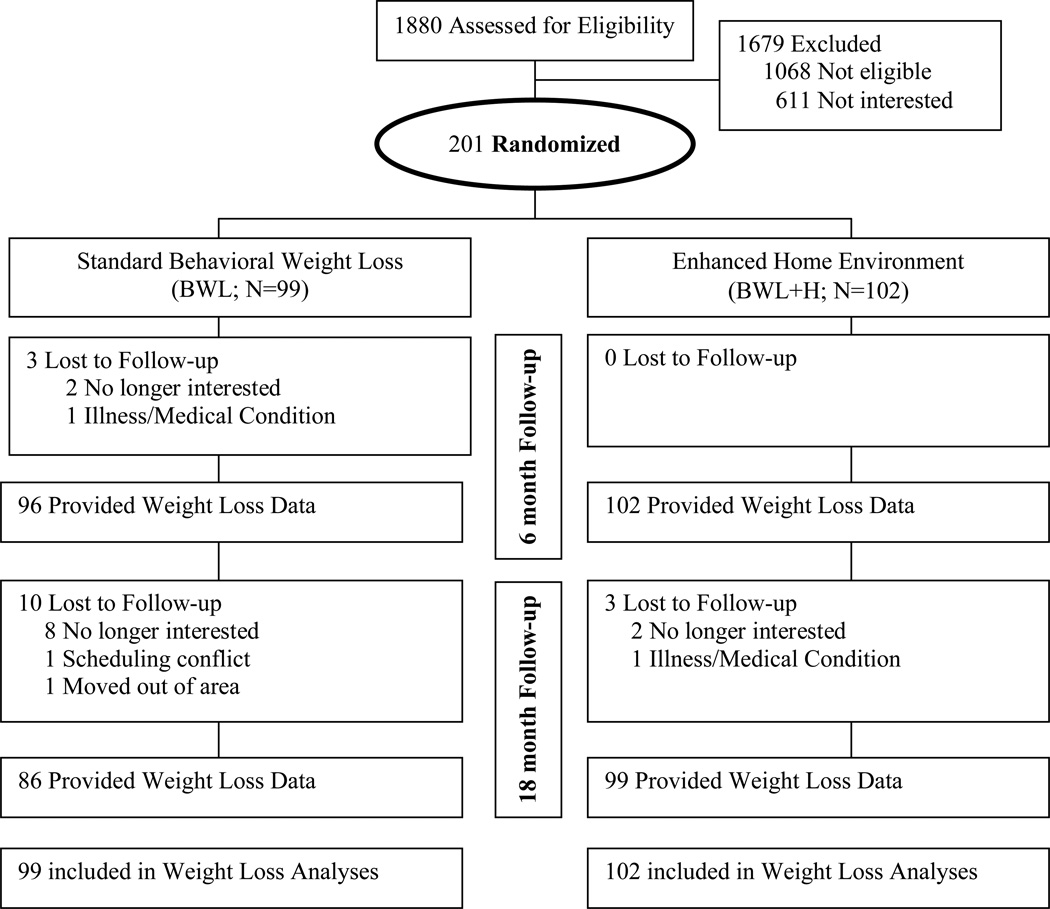
A total of 1880 individuals were screened by telephone to determine initial eligibility (see Figure 1). If an individual was eligible, they were asked to provide contact information for their partner who was then screened for eligibility. Eligible pairs were invited to attend an orientation at the clinic where the study was described in detail and informed consent was obtained.
Figure 1.
Participant flow in the study
Study Design
Participants were randomly assigned to one of two 18-month behavioral weight control programs: standard behavioral weight loss treatment (BWL) or BWL plus modifications to the home environment (BWL+H). In BWL, only participants received treatment while in BWL+H both participants and partners received treatment. Participants and partners in both conditions were assessed at baseline, 6, and 18 months and each received $25 for completing the 6 month assessment and $50 for completing the 18 month assessment.
Interventions
Common elements of BWL and BWL+H
Both conditions had weekly group meetings for 6 months followed by bi-weekly meetings for 12 months. Interventionists had an advanced degree in nutrition, exercise physiology, or behavioral psychology and experience providing weight loss treatment. Dietary and exercise prescriptions and behavior change skills were modeled after recent trials (Wadden et al., 2006; Subak et al., 2009), with the exception that meal replacement products were not provided. To achieve the 10% weight loss goal, all participants were placed on a standard caloric and fat restricted diet (e.g., 1200–1800 kcals/day and 30% fat, depending on initial weight) and given sample meal plans and a calorie guidebook. Participants were instructed to gradually increase their physical activity until they achieved ≥200 minutes of moderate intensity physical activity per week. Brisk walking was encouraged and participants were allowed to accumulate exercise minutes via multiple short bouts or longer continuous bouts. Participants received a pedometer with the goal of reaching 10,000 steps per day (Wilde, Sidman, & Corbin, 2001). Participants in both conditions received instruction in core behavioral skills. They were provided with daily diaries and instructed to record all food and beverage intake, the corresponding calories and fat grams, minutes of physical activity, daily steps, and their weight. Interventionists provided written feedback weekly. Participants were taught basic skills in stimulus control, problem solving, goal setting, cognitive restructuring, and relapse prevention. The focus of treatment shifted to weight loss maintenance in the latter months of the program. Keys to long-term success were reviewed and participants were taught a problem-solving approach (Perri, Mckelvey, Renjilian, Nezu, Shermer, & Viegener, 2001).
Treatment components specific to the BWL+H condition
BWL+H targeted the individual plus physical and social cues within their homes. While many BWL+H strategies have been used in prior weight loss programs with some success (e.g., Black et al., 1990; Jakicic et al., 1999), a unique element of this study is that BWL+H offered these components in a comprehensive treatment package that simultaneously manipulated physical and social aspects within participants’ households. BWL+H components aimed to modify the type and amount of food consumed, the availability of exercise equipment and sedentary activities, the saliency of the consequences of eating and activity choices, and to create a positive model for healthy eating and exercise in the home.
Modifying the type and amount of food consumed in the home
Once a month, BWL+H participants were instructed to participate in a “Cabinet Cleanout” exercise. A checklist of high-calorie, high-fat foods (e.g., potato chips) was provided and participants were instructed to search for these items in their home and remove them if found. A complementary “Filling Up with Fit Foods” exercise was completed monthly. Participants were provided with a checklist of foods that were consistent with their dietary prescription (e.g., oatmeal) and encouraged to have these items at home to promote dietary adherence. To increase cues for healthy food choices, participants were provided a low-calorie cookbook, a subscription to a healthy recipe magazine and motivational posters related to healthy eating. To limit portions and decrease passive overeating, participants were given serving size appropriate dishware and glasses (e.g., 8 oz. glasses), a food scale, and set of measuring cups and spoons. Finally, to limit impulse purchases while grocery shopping, participants were encouraged to use a commercially available online grocery ordering and home food delivery service (Gorin, Raynor, Maguire, Ferguson, & Wing, 2007). Participants paid for their own groceries and were reimbursed for the delivery fee.
Modifying the availability of exercise equipment and sedentary activities in the home
BWL+H participants were provided with a treadmill or stationary bicycle for home use. To reduce home-based sedentary activity, BWL+H participants were asked to restrict their viewing to one location in the home and to decrease the overall amount of time spent watching TV. The intervention staff outfitted each TV in the home with a TV Allowance®, a programmable device, often used in childhood obesity programs (Gorin et al., 2006; Robinson, 1999) that provided participants with objective feedback about their weekly viewing habits. BWL+H participants were also provided a subscription to an exercise-related magazine, exercise videotapes, resistance bands, and motivational posters to further increase cues for physical activity.
Increasing the saliency of the consequences of eating and exercise choices
BWL+H participants were given a digital body weight scale and a full length mirror. They were instructed to place these items in a prominent location in their home to serve as daily cues to self-weigh and to limit overeating and engage in physical activity.
Creating a positive model for healthy eating and exercise in the home
During the screening process, all participants were required to identify another member from their home who was also overweight and willing to participate in the program. In BWL+H, these partners were encouraged to attend all weight loss groups and make the same diet and exercise changes as the participants. Partners were given a 10% weight loss goal, expected to use the same behavioral tools, and model healthy eating and exercise behaviors in the home.
Data Collection
Participants and partners were assessed at baseline, 6, and 18 months via clinic and home visits. The primary outcome was body weight, measured in street clothes with shoes removed using a calibrated digital scale (Tanita BWB 800) and recorded to the nearest 0.1 kg. Height was measured at baseline to the nearest centimeter using a calibrated, wall-mounted stadiometer. BMI was calculated as kg/m2. Demographic characteristics were obtained by self-report.
Measures of the home environment
Type and placement of food in the home
The Household Food Inventory, a 117-item checklist with acceptable test-retest and inter-rater reliability (Raynor, Polley, & Wing, 2004; Gorin et al., 2008), was used to assess foods currently available in the home. The checklist includes foods listed on the Block Food Frequency Questionnaire (Block, Woods, Potosky, & Clifford, 1990) and additional low-fat food choices (e.g., reduced-fat cakes). During home visits, research assistants searched through food storage areas and indicated if a given food category was present, regardless of quantity (e.g., apples were counted as present whether there were 1 or 5 apples in the house). Responses were categorized as high-fat snacks (e.g., regular potato chips), high-fat spreads (e.g., regular mayonnaise), high-fat dairy (e.g., regular milk), fruits and vegetables, low-fat spreads (e.g., reduced-fat mayonnaise), low-fat dairy (e.g., reduced-fat cheese), low-fat cereals (e.g., cold cereals such as Corn Flakes, Kix) and low-fat snacks (e.g., reduced-fat potato chips). Analyses examined overall number of foods, total number of both high-fat and low-fat items, and subcategory scores.
Availability of exercise equipment
The 14-item Exercise Environment Questionnaire (Jakicic et al., 1997) was used to assess the presence of exercise equipment and related items in the home. Subscales include aerobic exercise equipment (e.g., stationary bike; 4 items), individual recreation equipment (e.g., roller skates; 4 items), individual sports equipment (e.g., golf clubs; 2 items), team sports equipment (e.g., baseball glove; 3 items), and athletic shoes. The measure has high levels of test-retest reliability, as well as high inter-rater reliability between family members (Jakicic et al., 1997). In addition to this information, the placement of any major piece of home exercise equipment (e.g., treadmill, stationary bicycle) was recorded.
Other items in home
Number of TVs in the home and the presence of healthy eating and exercise magazines, a body weight scale, and a full length mirror were assessed via self-report.
Social support
Participants completed the Sallis Social Support Scales in reference to their partners’ behaviors (Sallis, Grossman, Pinski, Patterson, & Nader, 1987). Subscales included encouragement for healthy eating, discouragement for healthy eating, participation in exercise, and use of rewards or punishment for exercise. The scales have adequate reliability and validity and show some associations with exercise and eating behaviors (Hagler, Norman, Zabinski, Sallis, Calfas, & Patrick, 2007; Trost, Owen, Bauman, Sallis, & Brown, 2002).
Perceived helpfulness of home environment components
At the completion of the 18-month program, BWL+H participants rated the helpfulness of various aspects of the intervention on a 7-point Likert scale ranging from 1=not at all helpful to 7=extremely helpful.
Behaviors
Dietary intake
The Block Food Frequency Questionnaire measured changes in daily caloric intake and percent of total calories consumed from fat. While underreporting is a problem with self-reported intake, the Block has been used in previous studies with a 6-month reporting interval and found to correspond with dietary records and has been validated against 3-day records (Block, Harman, Dresser, Carroll, Gannon, & Gardner, 1986; Block et al., 1990).
Physical activity
The Paffenbarger Activity Questionnaire (PAQ) provided estimates of total energy expended in physical activity per week. Participants reported their involvement in activities of light (5 kcal/min), medium (7.5 kcal/min), and high (10 kcal/min) intensity over the past week, which were then summed to produce an estimate of total energy expended in activity. The PAQ has high test-retest reliability (Paffenbarger, Wing, & Hyde, 1978) and is significantly correlated with measures of cardiovascular fitness (Siconolfi, Lasater, & Snow, 1985). Previous studies have shown that reported changes in exercise on the PAQ are predictive of weight change (Harris, French, Jeffery, McGovern, & Wing, 1994).
Data Analysis
All statistical analyses were performed using PASW Statistics 18, Release 18.0.0 (©SPSS, Inc., 2009, Chicago, IL, www.spss.com). Baseline group differences were examined using chi-square and t-tests. Subsequent analyses controlled for age. The primary analyses examined group differences in weight change at 6 and 18 months using ANCOVA models with baseline weight and age entered as covariates. Missing weights at follow-up visits were replaced with baseline weight and intent to treat analyses are reported. We considered adding further weight gain, as used in some other recent trials, to the imputed missing values (e.g., Wadden, Berkowitz, Womble, et al., 2005), however, given the slightly higher dropout rates in BWL, this adjustment would have created an artifact of differentially favoring BWL+H. Similar ANCOVA models examined group differences in behavioral outcomes and home environment changes at 6 and 18 months, gender as a moderator of treatment response, and weight loss in partners.
Results
Baseline Characteristics
Of the 1880 participants screened by telephone, 1679 were excluded and 201 were randomized (Figure 1; BWL, n=99; BWL+H n=102). BWL+H participants were younger than BWL participants but did not differ on other demographic variables. There were no demographic differences between partners in the two conditions (see Table 1). Most participant-partner pairs were comprised of spouses or significant others (77.2%), with smaller numbers of parent-adult child pairs (17.4%), other relative pairings (3.0%), and roommates (2.5%).
Table 1.
Characteristics of participants and partners by treatment condition
| Characteristic | Participants | Partners | ||||
|---|---|---|---|---|---|---|
| Total (N=201) |
BWL (N=99) |
BWL+H (N=102) |
Total (N=201) |
BWL (N=99) |
BWL+H (N=102) |
|
| Age (yrs), mean (±SD) | 48.9 (±10.5) | 50.4 (±9.3) | 47.5 (±11.3) | 47.8 (±13.1) | 47.9 (±13.3) | 47.8 (±13.0) |
| Female, n (%) | 157 (78.1) | 78 (78.8) | 79 (77.5) | 94 (46.8) | 47 (47.5) | 47 (46.1) |
| White race, n (%) | 164 (82.4) | 78 (78.8) | 86 (84.3) | 161 (80.5) | 78 (78.8) | 83 (82.2) |
| Hispanic or Latino, n (%) | 14 (7.0) | 7 (7.1) | 7 (6.9) | 13 (6.5) | 5 (5.1) | 8 (7.9) |
| Education ≥High School, n (%) | 79 (81.4) | 79 (79.8) | 86 (84.3) | 154 (78.6) | 78 (80.4) | 76 (76.8) |
| Married/Partnered, n (%) | 163 (81.1) | 83 (83.8) | 80 (78.4) | 163 (81.1) | 78 (78.8) | 85 (83.3) |
| Baseline BMI (kg/m2), mean (±SD) | 36.4 (±6.1) | 36.1 (±6.1) | 36.7 (±6.2) | 32.9 (±5.9) | 33.1 (±5.7) | 32.8 (±6.1) |
P>0.05 for comparison of BWL and BWL+H for all variables except for participants’ age where P=.0
Retention
Weight data were available from 98.5% and 92.0% of participants at 6 and 18 months, with complete weight data available for 91.5% of participants. BWL+H participants were more likely to have complete weight data than BWL participants (97.1% of BWL+H vs. 85.9% BWL, p=.004) and participants with complete weight data were significantly older (p<.0001) and had more years of formal schooling (p=.024) than participants with missing weight data. Weight data were available from 94.5% and 90.5% of partners at 6 and 18 months. Complete weight data were available from 90.0% of partners (97.1% BWL+H vs. 82.8% BWL, p<.001) and partners with complete data were older (p=.009) than partners with missing weight data.
Changes in the Home Environment
To determine if BWL+H was effective in changing the home environment as designed, we compared the homes of BWL+H and BWL participants at baseline, 6, and 18 months. Prior to the start of treatment, BWL+H and BWL homes were similar in the types of food available, the amount and type of exercise equipment present, the availability of scales, full length mirrors, and health focused magazines, and in the amount of support provided by their partners (see Table 2). At 6 months, BWL+H participants had greater access to full length mirrors (p<.0001), healthy eating magazines (p<.0001), and had more pieces of exercise equipment (p<.0001) that were more likely to be stored in a high-traffic, visible location (p<.01). While BWL participants had greater decreases in the overall number of foods in their home (p=.04), analyses of specific food categories showed that BWL+H participants had greater decreases in the number of high-fat spreads (p=.01) and greater increases in the amount of low-fat foods (p=.004 for total low-fat items, with greater increases in low-fat spreads, p=.01; and cereal, p=.012). No differences were observed in fruits and vegetables (p=.056), high or low-fat dairy (ps>.40) or high or low-fat snacks (ps>.90). In terms of the social home environment, at 6 months, partners’ participation in exercise increased in BWL+H and decreased in BWL (p<.0001) and BWL+H participants reported greater decreases in how much their partners discouraged healthy eating (p<.0001) (see Table 3). There were no differences in partners’ encouragement of healthy eating (p=.17) or use of rewards or punishment for exercise (p=.47).
Table 2.
Physical home environment at baseline, 6, and 18 months by treatment condition, mean (±SE) or n (%)
| Variable | BWL | BWL+H | p |
|---|---|---|---|
| Food Environment, M (±SE) | |||
| Number foods, total, baseline | 18.3 (±0.4) | 17.8 (±0.3) | .32 |
| Δ Baseline to 6 months | −1.6 (±0.4) | −0.4 (±0.3) | .02 |
| Δ Baseline to 18 months | −1.9 (±0.4) | −1.9 (±0.5) | .89 |
| Low-fat foods, total, baseline | 12.1 (±0.3) | 11.7 (±0.3) | .34 |
| Δ Baseline to 6 months | −0.9 (±0.3) | 0.4 (±0.3) | .02 |
| Δ Baseline to 18 months | −0.8 (±0.4) | −0.7 (±0.3) | .85 |
| High-fat foods, total, baseline | 6.2 (±0.2) | 6.1 (±0.2) | .63 |
| Δ Baseline to 6 months | −0.7 (±0.2) | −0.8 (±0.2) | .56 |
| Δ Baseline to 18 months | −1.1 (±0.2) | −1.3 (±0.2) | .56 |
| Exercise Environment, M (+SE) | |||
| Baseline | 4.5 (±0.3) | 4.5 (±0.3) | .94 |
| Δ Baseline to 6 months | 0.6 (±0.2) | 1.3 (±0.2) | .02 |
| Δ Baseline to 18 months | 0.6 (±0.2) | 1.4 (±0.2) | .004 |
| Major piece of exercise equipment, n (%) | |||
| Baseline | 51 (51.5) | 54 (52.9) | .84 |
| 6 Months | 50 (64.1) | 92 (96.8) | <.0001 |
| 18 Months | 47 (63.5) | 91 (94.8) | <.0001 |
| Exercise equipment in visible location, n (%) | |||
| Baseline | 28 (54.9) | 39 (72.2) | .065 |
| 6 Months | 33 (66.0) | 84 (91.3) | <.0001 |
| 18 Months | 31 (58.5) | 72 (79.1) | .008 |
| Scale, n (%) | |||
| Baseline | 86 (86.9) | 82 (80.4) | .22 |
| 6 Months | 83 (97.6) | 101 (100) | .12 |
| 18 Months | 76 (97.4) | 98 (100) | .11 |
| Full length mirror, n (%) | |||
| Baseline | 72 (72.9) | 80 (78.4) | .35 |
| 6 Months | 64 (75.3) | 96 (95.0) | <.0001 |
| 18 Months | 62 (79.5) | 94 (95.9) | .001 |
| Healthy Eating Magazines, n (%) | |||
| Baseline | 49 (49.5) | 53 (52.0) | .73 |
| 6 Months | 44 (51.8) | 92 (91.1) | <.0001 |
| 18 Months | 50 (64.1) | 96 (98.0) | <.0001 |
| Exercise/Health Magazines, n (%) | |||
| Baseline | 25 (25.3) | 18 (17.6) | .19 |
| 6 Months | 19 (22.4) | 25 (24.8) | .70 |
| 18 Months | 20 (25.6) | 60 (61.2) | <.0001 |
Table 3.
Perceived support from partners at baseline, 6, and 18 months by treatment condition, mean (±SE)
| Variable | BWL | BWL+H | p |
|---|---|---|---|
| Encouragement of healthy eating | |||
| Baseline | 15.2 (±0.5) | 14.0 (±0.5) | .12 |
| Δ Baseline to 6 months | 1.9 (±0.5) | 2.8 (±0.4) | .17 |
| Δ Baseline to 18 months | 0.3 (±0.5) | 1.1 (±0.4) | .22 |
| Discouragement of healthy eating | |||
| Baseline | 12.4 (±0.4) | 10.7 (±0.4) | .003 |
| Δ Baseline to 6 months | 0.8 (±0.4) | −1.7 (±0.4) | .000 |
| Δ Baseline to 18 months | 0.2 (±0.5) | −0.4 (±0.4) | .29 |
| Participation in exercise | |||
| Baseline | 24.6 (±1.0) | 22.9 (±0.9) | .23 |
| Δ Baseline to 6 months | −0.2 (±0.9) | 4.6 (±0.8) | .00 |
| Δ Baseline to 18 months | −1.4 (±1.0) | 2.3 (±0.9) | .012 |
| Use of rewards/punishment for exercise | |||
| Baseline | 3.8 (±0.1) | 3.5 (±0.1) | .016 |
| Δ Baseline to 6 months | 0.4 (±0.2) | 0.2 (±0.1) | .47 |
| Δ Baseline to 18 months | 0.4 (±0.2) | 0.3 (±0.2) | .96 |
By 18 months, fewer differences between BWL+H and BWL home environments were observed. BWL+H participants still had more exercise equipment in the home (p<.0001) and were more likely to store the equipment in a visible location (p<.01) but there were no group differences in home access to a scale, full length mirror, healthy eating or exercise magazines. The home food environments looked remarkably similar between groups at 18 months; BWL+H participants had greater increases in the number of low-fat spreads (p=.02) but no other differences emerged. BWL+H participants continued to report more support from their partners on measures of participation in exercise (p=.017) but not on other measures of partner support.
BWL+H reported that many of the home environment intervention components were helpful in their weight loss process. Participants rated the body weight scale as most helpful (6.8±0.7 on a 7-point scale), followed by involvement of their partner in treatment (6.2±1.4), receiving a treadmill for home use (5.9±1.5), and provision of a food scale (5.9±1.5) and measuring cups (5.7±1.5). Ratings of helpfulness were lowest for the online grocery ordering and delivery service (2.9±2.0) and the use of the TV Allowances (2.0±1.5).
Weight Loss and Behavioral Outcomes
Weight loss and behavioral outcomes are reported in Table 4. At 6 months, we found a significant weight loss benefit for BWL+H compared to BWL (−9.1±0.7 vs. −6.8±0.7 kgs, p=.017) but at 18 months, this advantage was no longer observed (−7.3±1.0 vs. −5.5±1.0 kgs, p=.19). Participants regained an average of 1.6±0.4 kgs from 6 to 18 months, with no differences between conditions (p=.30).
Table 4.
Weight and behavior changes by treatment condition, mean (±SE)
| Variable | Overall | BWL | BWL+H | p |
|---|---|---|---|---|
| Weight Change (kg) | ||||
| Baseline | 101.5 (±1.5) | 101.7 (±2.2) | 101.2 (±2.1) | .95 |
| Δ Baseline to 6 months | −8.0 (±0.5) | −6.8 (±0.7) | −9.1 (±0.7) | .017 |
| Δ Baseline to 18 months | −6.4 (±0.7) | −5.5 (±1.0) | −7.3 (±1.0) | .19 |
| Energy Intake (kcal/day) | ||||
| Baseline | 1933.8 (±61.6) | 1939.5 (±86.1) | 1930.1 (±86.8) | .94 |
| Δ Baseline to 6 months | −481.8 (±43.4) | −414.8 (±65.9) | −548.8 (±57.9) | .13 |
| Δ Baseline to 18 months | −409.1 (±49.5) | −379.8 (±77.2) | −438.4 (±64.1) | .57 |
| Fat Intake (% kcal/day) | ||||
| Baseline | 38.7 (±0.5) | 38.5 (±0.8) | 38.8 (±0.8) | .73 |
| Δ Baseline to 6 months | −5.2 (±0.6) | −3.5 (±0.9) | −6.8 (±0.8) | .005 |
| Δ Baseline to 18 months | −3.7 (±0.6) | −2.1 (±1.0) | −5.3 (±0.8) | .012 |
| Physical Activity (kcals/week) | ||||
| Baseline | 813.9 (±82.0) | 764.8 (±117.4) | 861.5 (±115.7) | .56 |
| Δ Baseline to 6 months | 590.1 (±117.2) | 663.2 (±174.1) | 517.0 (±160.2) | .54 |
| Δ Baseline to 18 months | 396.4 (±120.7) | 214.2 (±179.9) | 578.5 (±163.5) | .14 |
BWL+H participants reported greater reductions in dietary fat intake than BWL participants at 6 and 18 months (ps = .005 and .012, respectively) but did not differ in overall caloric intake at either time point (ps>.10). No group differences were observed on total energy expended in physical activity at 6 or 18 month (ps=.54 and .14, respectively).
Gender as a Moderator
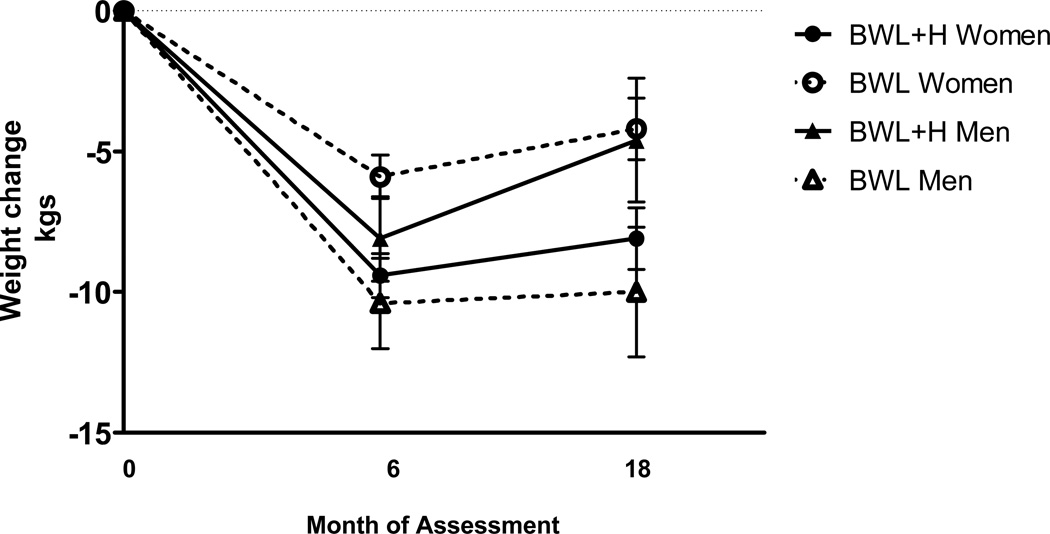
Gender moderated treatment response at both 6 and 18 months (Group × Gender at 6 months, p=.011; at 18 months, p=.006; see Figure 2). Women lost significantly more weight in BWL+H than BWL at 6 months (−9.4±0.8 vs. −5.9±0.8 kgs, p=.001) and 18 months (−8.1±1.1 vs. −4.2±1.1 kgs, p=.014), while men lost equivalent amounts of weight in BWL+H and BWL at 6 months (−8.1±1.5 vs. −10.4±1.6 kgs, p=.26) and tended to lose more weight in BWL at 18 months (−4.6±2.2 vs. −10.0±2.3 kgs, p=.065). Gender did not moderate weight regain (p=.23) with men and women in both groups regaining at equivalent rates.
Figure 2.
Weight change by treatment condition and gender at 6 and 18 months
Partner effects
Weight loss and behavioral outcomes for partners are reported in Table 5. BWL+H partners lost more weight than BWL partners, regardless of gender, at 6 (−9.8±0.6 vs. −3.4±0.6 kgs, p<.001) and 18 months (−6.7±0.8 vs. −2.3±0.8 kgs, p<.001). Partners’ weight regain from 6 to 18 months did not differ between groups (p=.17), and was not moderated by gender (p=.62). BWL+H partners reported greater decreases in fat intake at 6 and 18 months (p<.001 and .03, respectively) but did not differ from BWL on changes in energy intake or physical activity.
Table 5.
Partners’ weight and behavior changes by treatment condition, mean (±SE)
| Variable | Overall | BWL | BWL+H | p |
|---|---|---|---|---|
| Weight Change (kg) | ||||
| Baseline | 96.6 (±1.5) | 97.5 (±2.1) | 95.6 (±2.0) | .52 |
| Δ Baseline to 6 months | −6.6 (±0.4) | −3.4 (±0.6) | −9.8 (±0.6) | <.001 |
| Δ Baseline to 18 months | −4.5 (±0.6) | −2.3 (±0.8) | −6.7 (±0.8) | <.001 |
| Energy Intake (kcal/day) | ||||
| Baseline | 1921.8 (±69.0) | 1981.7 (±98.5) | 1861.8 (±96.6) | .39 |
| Δ Baseline to 6 months | −374.7 (±44.9) | −287.7 (±68.4) | −461.8 (±58.4) | .06 |
| Δ Baseline to 18 months | −251.7 (±52.7) | −226.9 (±79.9) | −276.5 (±68.8) | .64 |
| Fat Intake (% kcal/day) | ||||
| Baseline | 38.3 (±0.5) | 39.0 (±0.7) | 37.7 (±0.7) | .22 |
| Δ Baseline to 6 months | −3.2 (±0.6) | −.92 (±0.9) | −5.5 (±0.8) | <.001 |
| Δ Baseline to 18 months | −2.0 (±0.6) | −.69 (±0.9) | −3.2 (±0.7) | .03 |
| Physical Activity (kcals/week) | ||||
| Baseline | 1128.6 (±119.0) | 991.7 (±169.6) | 1261.4 (±167.1) | .26 |
| Δ Baseline to 6 months | 126.5 (±131.7) | −31.7 (±196.6) | 284.8 (±176.0) | .23 |
| Δ Baseline to 18 months | 170.6 (±168.9) | −48.8 (±253.2) | 390.0 (±225.7) | .19 |
Discussion
This innovative, multi-level home environment intervention which simultaneously targeted both physical (e.g., types of food, exercise equipment) and social (involvement of a support partner) factors was effective in changing many aspects of the home environment, particularly during the first 6 months of treatment. The enhanced intervention had a positive impact on initial weight losses, resulting in a 33% increase in weight loss at 6 months compared to the standard program. At 18 months, the home environment intervention continued to be associated with greater weight loss in women; however, men tended to lose more weight in the standard program than in the home environment intervention at 18 months.
As ecological models of behavior change advance, some have argued that demographic moderators such as gender need to be considered when examining the link between the environment and behavior (Kremers et al, 2006). Prior work has suggested that gender can indeed moderate response to weight loss treatment (e.g., Espeland et al., 2009; Presnell, Pells, Stout, & Mustante, 2008). Most relevant is Wing and colleagues (1991) report comparing a standard behavioral weight loss program to one that involved spouses in treatment. The spouse involvement condition resulted in greater weight losses only for women. Our findings echo this earlier work and suggest that women may uniquely benefit from an intervention that involves partner support and modifications to the physical home environment. There are several possible reasons for this gender effect, all of which are speculative at this time. If women are the primary grocery shoppers or meal preparers for their family, having another adult in their household who is following the same plan may eliminate preparation of extra meals or decrease the purchasing of foods that are inconsistent with their dietary goals. Conversely, men may respond better to a standard, individual focused intervention because by attending group alone, they may assume more personal responsibility for their behavior change. Reasons for the gender differences observed in the present trial need further investigation. In addition, there are other factors beyond the scope of this paper, such as eating style, restraint and disinhibiting tendencies, and characteristics of the partner relationship and/or household structure, that should be explored as potential moderators of treatment response.
We were successful in designing an intervention that resulted in many desired environmental changes in the initial intervention period including greater access to low-fat food options and exercise equipment for home use, more cues for healthy eating and activity choices (e.g., greater visibility of exercise equipment, presence of a full length mirror and healthy eating and exercise magazines), and more support from partners for healthy choices. In general, participants rated many aspects of the home environment intervention as very helpful for their weight loss with provision of scales, treadmills, and the involvement of their partner in treatment at the top of list. Some of the anticipated changes, however, were not realized and many of the initial improvements were not maintained. This is likely due to underutilization of some of the home environment strategies. The use of TV Allowances and online ordering of groceries, for example, were associated with positive behavior changes in pilot testing (Gorin et al., 2006, 2007) but were not well received in this trial. Also, many positive changes were seen in the homes of participants in the standard condition, even in the absence of explicit instruction. This finding is consistent with Krukowski and colleagues (2010) as well as on our own earlier work (2008) which suggests that weight loss participants naturally decrease the number of high fat foods in their home while in a lifestyle program. Our home environment intervention may not have been powerful enough to further improve upon these already occurring reductions.
While our results suggest that a home environment approach to weight loss holds promise, many questions remain about who this approach works best for and what household modifications should be emphasized. We have identified one important moderator of treatment response, gender, and it is likely that there are other relevant person and behavior level variables to consider. Our results suggest that direct modifications to the home (e.g., bringing a partner to treatment, provision of a treadmill) may be easier to initiate and maintain, and perceived as more helpful, than activities requiring more conscious effort by participants (e.g., use of online ordering service). It also might be beneficial to involve the entire household in treatment, not just the participant and a partner, similar to the weight gain prevention approach used recently by French and colleagues (2011). Or, perhaps, more sustained effects would be observed if home environment changes were augmented with modifications to other influential contexts such as work environments.
Some limitations of this efficacy trial are concerns regarding generalizability and translatability. Participation was limited to healthy adults who were likely to adhere to the study protocol and who also lived with an overweight or obese adult who was willing and eligible to participate in the study. Of those screened, approximately 11% were enrolled in the trial, a percentage that is consistent with many recent trials of lifestyle weight management programs (e.g., Subak et al., 2009) but nonetheless suggests that the sample might not be representative of the overweight/obese population as a whole. Also of concern is the potential for translation of the intervention outside of the research setting. Many of the home environment treatment elements incur additional costs, however, over the course of the intervention, these added expenses equate to less than $1.65/day per person. Effectiveness studies will be needed to determine whether the treatment package can be disseminated to the larger community.
Evidence that the environment influences food choice and activity habits continues to build (e.g., Papies & Hamstra, 2010; Thomas, Dosti, Crosby, & Lowe, 2011). We recently reported that the homes of overweight and obese individuals differ from the homes of normal weight individuals, with greater availability of high-fat foods and televisions and less access to fruits and vegetables and exercise equipment (Gorin et al., 2011). Many of these same elements distinguished successful weight loss maintainers from overweight and obese individuals seeking weight loss treatment (Phelan et al., 2009), suggesting that the home environment may be an important target of intervention. The present study provides some support for the viability of a home-focused weight loss program. More research is needed to determine how best to intervene in the homes of weight loss participants to create sustained environmental and behavioral changes that lead to weight loss maintenance.
Acknowledgements
The authors wish to thank Andrea Bruni, Mark Campbell, Julia Casasanto-Ferro, Craig Dandrow, Jill Donnelly, Michael Gutierrez, and Dylan Wykes for their assistance in recruiting and assessing participants; Barbara Bancroft, Elizabeth Jackvony, Pamela Rogers Coward, and Eva Serber for delivering the intervention; Jason Peng and Carl Robitaille for data management support; Kristen Whitehead for administrative support; and LEAP participants. This research was supported by the National Heart, Lung, Blood Institute HL77082.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/HEA
Contributor Information
Amy A. Gorin, Department of Psychology, Center for Health, Intervention, and Prevention, University of Connecticut
Hollie A. Raynor, Department of Nutrition, University of Tennessee
Joseph Fava, The Miriam Hospital, Weight Control and Diabetes Research Center.
Kimberly Maguire, The Miriam Hospital, Weight Control and Diabetes Research Center.
Erica Robichaud, The Miriam Hospital, Weight Control and Diabetes Research Center.
Jennifer Trautvetter, The Miriam Hospital, Weight Control and Diabetes Research Center.
Melissa Crane, Department of Health Behavior & Health Education, Gillings School of Global Public Health, University of North Carolina at Chapel Hill.
Rena R. Wing, Brown Medical School, The Miriam Hospital
References
- Biing-Hwan L, Geuthri JF, Frazao E. Nutrient combination of food away from home. In: Frazao E, editor. America’s eating habits: changes and consequences. Washington, D.C.: USDA; 1999. pp. 213–242. [Google Scholar]
- Black DR, Gleser LJ, Kooyers KJ. A meta-analytic evaluation of couples weight-loss programs. Health Psychology. 1990;9:330–347. doi: 10.1037//0278-6133.9.3.330. [DOI] [PubMed] [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire design using multiple diet records. Journal of Clinical Epidemiology. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- Bouton ME. A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychology. 2000;19:57–63. doi: 10.1037/0278-6133.19.suppl1.57. [DOI] [PubMed] [Google Scholar]
- Breslow L. Social ecological strategies for promoting healthy lifestyles. American Journal of Health Promotion. 1996;10:253–257. doi: 10.4278/0890-1171-10.4.253. [DOI] [PubMed] [Google Scholar]
- Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity promoting eating behaviors in adolescence. Obesity. 2007;15:719–730. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or Metformin. New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espeland MA, Bray GA, Neiberg R, Rejeski WJ, Knowler WC, Lang W, Cheskin LJ, Williamson D, Lewis CB, Wing R Look Ahead Study Group. Describing patterns of weight changes using principal components analysis: results from the Action for Health in Diabetes (Look AHEAD) research group. Annals of Epidemiology. 2009;19:701–710. doi: 10.1016/j.annepidem.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annual Review of Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action – A group randomized trial. Obesity. 2011 doi: 10.1038/oby.2010.328. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulkerson JA, Nelson MC, Lytle L, et al. The validation of a home food inventory. International Journal of Behavioral Nutrition and Physical Activity. 2008;5:55. doi: 10.1186/1479-5868-5-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gattshall ML, Shoup JA, Marshall JA, et al. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. International Journal of Behavioral Nutrition and Physical Activity. 2008;11:53. doi: 10.1186/1479-5868-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Phelan S, Raynor HA, Wing RR. Home food and exercise environments of normal weight and overweight adults. American Journal of Health Behavior. 2011;35:618–626. doi: 10.5993/ajhb.35.5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Raynor H, Chula Maguire K, Wing RR. Decreasing household television time: A pilot study of a combined behavioral and environmental intervention. Behavioral Interventions. 2006;21:273–280. [Google Scholar]
- Gorin AA, Raynor HA, Niemeier HM, Wing RR. Home grocery delivery improves the household food environments of behavioral weight loss participants: Results of an 8-week pilot study. International Journal of Behavioral Nutrition and Physical Activity. 2007;4:58. doi: 10.1186/1479-5868-4-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Wing RR, Fava JL, et al. Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. International Journal of Obesity. 2008;32:1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagler AS, Norman GJ, Zabinski MF, Sallis JF, Calfas KJ, Patrick K. Psychosocial correlates of dietary intake among overweight and obese men. American Journal of Health Behavior. 2007;31:3–12. doi: 10.5555/ajhb.2007.31.1.3. [DOI] [PubMed] [Google Scholar]
- Harris JK, French SA, Jeffery RW, McGovern PG, Wing RR. Dietary and physical activity correlates of long-term weight loss. Obesity Research. 1994;2:307–313. doi: 10.1002/j.1550-8528.1994.tb00069.x. [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Wing RR, Butler BA, Jeffery RW. The relationship between presence of exercise equipment in the home and physical activity level. American Journal of Health Promotion. 1997;11:363–365. doi: 10.4278/0890-1171-11.5.363. [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women. Journal of the American Medical Association. 1999;282:1554–1560. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: Current status. Health Psychology. 2000;19(Suppl.):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Kremers SPJ, de Bruijn GJ, Visscher TLS, et al. Environmental influences on energy balance-related behaviors: a dual-process view. International Journal of Behavioral Nutrition and Physical Activity. 2006;3:9. doi: 10.1186/1479-5868-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krukowski RA, Harvey-Berino J, West DS. Differences in home food availability of high- and low-fat foods after a behavioral weight control program are regional not racial. International Journal of Behavioral Nutrition and Physical Activity. 2010;7:69. doi: 10.1186/1479-5868-7-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2007;30:1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AHEAD Research Group. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: Four year results of the Look AHEAD trial. Archives of Internal Medicine. 2010;170:1566–1575. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: is it feasible? Obesity Research. 2003;11(Suppl):44S–59S. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Macken LC, Yates B, Blancher S. Concordance of risk factors in female spouse of male patients with coronary heart disease. Journal of Cardiopulmonary Rehabilitation. 2000;20:361–368. doi: 10.1097/00008483-200011000-00005. [DOI] [PubMed] [Google Scholar]
- Markey CN, Markey PM, Birch LL. Interpersonal predictors of dieting practices among married couples. Journal of Family Psychology. 2001;15:464–475. doi: 10.1037//0893-3200.15.3.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Papies EK, Hamstra P. Goal priming and eating behavior: Enhancing self-regulation by environmental cues. Health Psychology. 2010;29:384–388. doi: 10.1037/a0019877. [DOI] [PubMed] [Google Scholar]
- Perri MG, Mckelvey WF, Renjilian DA, Nezu AM, Shermer RL, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. Journal of Consulting and Clinical Psychology. 2001;69:722–726. [PubMed] [Google Scholar]
- Phelan S, Liu T, Gorin AA, Lowe M, Hogan J, Fava J, Wing RR. What distinguishes weight loss maintainers from the treatment-seeking obese? Analysis of environmental, behavioral, and psychosocial variables in diverse populations. Annals of Behavioral Medicine. 2009;38:94–104. doi: 10.1007/s12160-009-9135-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presnell K, Pells J, Stout A, Musante G. Sex differences in the relation of weight loss self-efficacy, binge eating, and depressive symptoms to weight loss success in a residential obesity treatment program. Eating Behavior. 2008;9:170–180. doi: 10.1016/j.eatbeh.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Polley BA, Wing RR, et al. Is dietary fat intake related to liking or household availability of high- and low-fat foods? Obesity Research. 2004;12:816–823. doi: 10.1038/oby.2004.98. [DOI] [PubMed] [Google Scholar]
- Robinson JP, Godbey G. Time for life: the surprising ways Americans use their time. University Park, PA: Penn State Univ. Press; 1997. [Google Scholar]
- Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. Journal of the American Medical Association. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Siconolfi SF, Lasater TM, Snow RCF, et al. Self-reported physical activity compared with maximal oxygen uptake. American Journal of Epidemiology. 1985;122:101–105. doi: 10.1093/oxfordjournals.aje.a114068. [DOI] [PubMed] [Google Scholar]
- Stokols D. Social ecology and behavioral medicine: implications for training, practice, and policy. Behavioral Medicine. 2000;26:129–139. doi: 10.1080/08964280009595760. [DOI] [PubMed] [Google Scholar]
- Stuart RB, Davis B. Slim chance in a fat world: behavioral control of obesity. Champaign: Research; 1972. [Google Scholar]
- Subak LL, Wing R, West DS, et al. Weight loss to treat urinary incontinence in overweight and obese women. New England Journal of Medicine. 2009;360:481–490. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swinburn B, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- Thomas JG, Doshi S, Crosby RD, Lowe MR. Ecological momentary assessment of obesogenic eating behavior: Combining person-specific and environmental predictors. Obesity. 2011 doi: 10.1038/oby.2010.335. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Medicine and Science in Sports and Exercise. 2002;34:1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, Hesson LA, Osei SY, Kaplan R, Stunkard AJ. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine. 2005;17(353):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinology, Metabolic Clinics of North America. 2003;32:981–1003. doi: 10.1016/s0889-8529(03)00072-0. [DOI] [PubMed] [Google Scholar]
- Wadden TA, West DS, Delahanty L, et al. Look AHEAD Research Group. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SS, Brownell KD. Public policy and obesity: the need to marry science with advocacy. Psychiatric Clinics of North America. 2005;28:235–252. doi: 10.1016/j.psc.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16:2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- Wilde BE, Sidman CL, Corbin CB. A 10,000 step count as a physical activity target for sedentary women. Research Quarterly for Exercise and Sport. 2001;72:411–414. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- Wing RR, Gorin AA, Tate DF. Strategies for changing eating and exercise behavior. In: Bowman BA, Russell RM, editors. Present Knowledge in Nutrition 8th Edition. Washington, D.C.: ILSI Press; 2006. [Google Scholar]
- Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. Journal of Consulting and Clinical Psychology. 1991;59:156–162. doi: 10.1037//0022-006x.59.1.156. [DOI] [PubMed] [Google Scholar]