Abstract
Objectives
We conducted a proof of concept study to determine the feasibility of using an individual psychotherapy, Interpersonal and Social Rhythm Therapy (IPSRT), as monotherapy for the acute treatment of bipolar II depression.
Methods
Unmedicated individuals (n = 17) meeting DSM-IV criteria for bipolar II disorder and currently depressed received weekly psychotherapy (IPSRT) for 12 weeks. After 12 weeks of acute treatment, individuals received an additional 8 weeks of follow-up treatment consisting of continued weekly IPSRT with supplementary lamotrogine for IPSRT non-responders.
Results
By week 12, 41% (n = 7) of the sample responded to IPSRT monotherapy (defined as ≥50% reduction in depression scores without an increase in mania scores), 41% (n = 7) dropped out of or were removed from the study, and 18% (n = 3) did not respond to treatment. By week 20, 53% (n = 9) had achieved a response and 29% (n = 5) achieved a full remission of symptoms.
Conclusions
Interpersonal and Social Rhythm Therapy appears to be a promising intervention for a subset of individuals with bipolar II depression. A randomized controlled trial is needed to systematically evaluate the efficacy of IPSRT as an acute monotherapy for bipolar II depression.
Keywords: affective disorder, bipolar disorder, interpersonal psychotherapy, psychotherapy
Bipolar II disorder (BPII) is a common psychiatric illness with a reported lifetime prevalence of 0.5–11% (1–3). Characterized by multiple, protracted depressive episodes and mixed mood states, evidence suggests that BPII is at least as disabling as bipolar I disorder (BPI). In contrast to individuals with BPI, individuals with BPII may experience higher rates of rapid cycling, shorter ‘well’ periods, and greater impairment from subthreshold symptoms (4–8). Despite the fact that this is a prevalent condition associated with marked morbidity and impairment, few treatments for this disorder have been systematically evaluated (9). The specific role of psychotherapy in the management of individuals suffering from BPII is unknown.
To our knowledge, there are no published trials of psychotherapy specifically for the treatment of BPII—with or without medication. Recently published data showed the addition of any of three intensive psychosocial interventions [Interpersonal and Social Rhythm Therapy (IPSRT), family-focused therapy, or cognitive behavioral therapy] to pharmacotherapy offered advantages in time-to-recovery relative to a control condition in a group of depressed subjects meeting criteria for both BPI and BPII, although investigators did not examine separate outcomes in the subgroup meeting criteria for BPII (10). Similarly, the addition of care management interventions (with psychosocial components) to usual care (including pharmacotherapy) in mixed BPI and BPII populations resulted in improved long-term outcomes relative to usual care in managed care and Veterans Affairs settings, respectively (11–13). Although these trials demonstrate that there are advantages to adding psychotherapy to pharmacotherapy in pooled groups of subjects with both BPI and BPII diagnoses, they do not provide information on the feasibility of using psychotherapy as monotherapy for the treatment of BPII.
This lacuna in the evidence base is notable for several reasons. Firstly, BPII exists phenotypically on a continuum of affective disorders between unipolar and bipolar I disorders. As several psychotherapies have demonstrated efficacy as monotherapy for unipolar depression (14), it raises the possibility that at least a subset of individuals with this disorder may also respond to psychotherapy alone. Secondly, individuals suffering from BPII struggle with many issues that would be appropriately addressed by psychotherapy, such as declines in interpersonal and vocational functioning because of chronic untreated symptoms, difficulty distinguishing among mood states, including inability to recognize hypomania (15), and skepticism about working with a medical establishment that has repeatedly failed to recognize their illness (16) and has little to offer them in the way of informed treatment options (9, 17). Finally, all currently available pharmacotherapy for bipolar spectrum disorder is associated with problematic side effects (18), raising the possibility that those who do not tolerate medications will benefit from psychotherapy alone. It is therefore surprising that psychosocial interventions for BPII have received so little research attention.
The goal of this study was to demonstrate the feasibility of using an empirically tested psychotherapy for bipolar disorder, IPSRT (19), as a treatment for unmedicated individuals meeting criteria for BPII, currently depressed. IPSRT is based on the principles of interpersonal psychotherapy for unipolar depression (20) and the demonstrated relationship between mood episodes and life events (21). It addresses patients’ sleep/wake cycles and levels of activation, thereby directly targeting the underlying circadian rhythm perturbations associated with bipolar disorder (22). It has now been shown to be efficacious when used with pharmacotherapy for the treatment of acute bipolar depression (10) and in the prevention of recurrence in patients with BPI (23). This was considered a proof of concept study in that, to our knowledge, there are no prior reports of psychotherapy as monotherapy for the management of acute bipolar II depression. The modest goals of a proof of concept study include demonstration of feasibility and establishment of directions for future research.
Methods
Study design
All study procedures were reviewed and approved by the Biomedical Institutional Review Board of the University of Pittsburgh. Potential subjects provided informed written consent after receiving a complete description of the study, including a full description of risks associated with study participation. Subjects were recruited by word of mouth from other investigators and clinicians.
Thirty-three potential subjects consented to screening for inclusion in the protocol during the study period (13 October 2005–31 October 2006). A total of 17 subjects were deemed eligible for inclusion in the protocol based on the following criteria: (i) age 18–65; (ii) lifetime diagnosis of BPII, currently depressed; (iii) Hamilton Rating Scale for Depression (HRSD) (24) score ≥ 15; and (iv) Young Mania Rating Scale (YMRS) (25) score ≤ 10. Subjects were excluded from the study if they met any of the following criteria: (i) currently receiving treatment with psychoactive medications; (ii) diagnosis of substance abuse or dependence within the prior six months; (iii) diagnosis of borderline or antisocial personality disorder; or (iv) unstable medical condition that could produce symptoms that would confound accurate assessment of mood symptoms (e.g., untreated thyroid disease). Two of the 17 eligible subjects were receiving medication (paroxetine and bupropion, respectively) prior to study entry. They were tapered off of medication and reassessed to determine continued eligibility. One week off of psychotropic medications, both subjects continued to meet all eligibility criteria.
Demographic data and psychiatric treatment history were recorded on standardized research forms. Lifetime and current psychiatric diagnoses were assigned using the Structured Clinical Interview for DSM-IV, Clinician Version (SCID) (26). Depressive symptoms were assessed using the 17-item HRSD (HRSD-17), the expanded 25-item version of the HRSD (HRSD-25) that includes reverse neurovegetative symptoms (27), and the Montgomery-Åsberg Depression Rating Scale (MADRS) (28). Mania symptoms were rated using the YMRS. Global functioning was evaluated using the Clinical Global Impressions Scale, Bipolar Version (CGI-BP) (29), which includes separate clinician ratings for depression and mania on two 7-point likert-type scales. Research assessments were conducted by raters who were not involved in the subjects’ treatment. Inter-rater reliability as measured by intraclass correlations (ICC) was acceptable: ICC = 0.96, 0.92, and 0.80 for YMRS, HRSD-25, and HRSD-17, respectively. Satisfaction with the intervention was assessed at Visits 12 and 20 with the 8-item Client Satisfaction Questionnaire (CSQ-8) (30), which yields scores ranging from 8 to 32, with higher scores indicating greater levels of satisfaction.
Subjects were scheduled for weekly, 45-min, individual psychotherapy sessions. IPSRT is described in greater detail in the manual (19). Briefly, IPSRT is comprised of three components: psychoeducation, social rhythm therapy (SRT), and interpersonal psychotherapy (IPT). Psychoeducation focuses on (i) the illness and its consequences, (ii) treatment options and associated side effects, and (iii) prodromal symptoms/detection of early warning symptoms. SRT is based on the theory that stable daily rhythms lead to enhanced stability of mood. This component of treatment focuses on developing strategies to promote regular, rhythm-entraining, daily schedules. It also encourages patients to modulate the amount of stimulation in their daily lives—including attending to the intensity of interpersonal interactions and recognizing the impact of maladaptive novelty-seeking behaviors on mood states. The IPT component, based on standard IPT for unipolar depression (20), focuses on links between mood and problematic interpersonal relationships, helping patients to function more effectively in interpersonal realms. In order to meet the needs of patients with BPII, the psychoeducation component of IPSRT was modified to reflect information regarding the diagnosis, treatment, and course of BPII (rather than BPI) (15). IPSRT sessions were delivered by one psychiatrist (HAS) and four master’s level therapists.
Subjects who experienced sleep disturbances that could not be managed with behavioral strategies alone could receive low doses of a benzodiazepine at any point during the study. At Session 12, all subjects who had not responded to IPSRT were prescribed lamotrigine according to the manufacturer’s guidelines. Subjects who did not respond to lamotrigine or did not tolerate lamotrigine remained in the study and received alternative standard-of-care pharmacotherapy. Response was defined as a 50% reduction in the HRSD-17 from baseline score with YMRS < 10. Remission was defined as three consecutive visits where the average scores for the HRSD-17 and YMRS each averaged <7.
Assessment time points were determined by session number rather than by number of weeks in the study. Median number of weeks to Visit 12 was 13.2 (±5.7). Median number of weeks to Visit 20 was 24 (±7.7).
Data analysis
For baseline demographic and clinical characteristics, t-tests and chi-square tests were used to compare continuous and categorical variables, respectively. Longitudinal data were analyzed using an intent-to-treat approach with repeated-measures mixed-effect statistical models. Subject and linear time were random effects in the models.
Results
Baseline demographic and clinical characteristics of the sample are displayed in Table 1, and there were no significant differences between groups. One subject met all study eligibility requirements but did not come to a single treatment session. One subject was hospitalized at Visit 2 for acute suicidal ideation. Twenty-nine percent (n = 5) dropped out after having had at least one study visit (mean number of visits prior to drop out = 4.2 ± 3.3; range 1–9). Fifty-nine percent (10/17) completed the 20-visit study. Six subjects (35%) were prescribed either low-dose lorazepam (0.5–2 mg) or clonazepam (1 mg) for a median of 3.5 weeks (range 1–5).
Table 1.
Baseline demographic and clinical characteristics of responders and non-responders
| Responders at Visit 12 (n = 7) | Non-responders at Visit 12 (n = 10) | |||
|---|---|---|---|---|
| Variable | Mean (SD) or n (%) | Median [range] | Mean (SD) or n (%) | Median [range] |
| Age | 38.2 (17.1) | 38.9 [21.0–62.6] | 41.6 (13.9) | 45.5 [21.7–57.8] |
| Female | 5 (71%) | 5 (50%) | ||
| Education (years) | 13.9 (2.0) | 14 [12–18] | 14.8 (2.4) | 14 [12–19] |
| Marital status | ||||
| Married | 2 (29%) | 3 (30%) | ||
| Never married | 3 (43%) | 5 (50%) | ||
| Separated or divorced | 2 (29%) | 2 (20%) | ||
| Employment | ||||
| Full time, part time, homemaker | 3 (43%) | 2 (20%) | ||
| Student | 2 (29%) | 3 (30%) | ||
| Disabled, unemployed | 2 (29%) | 5 (50%) | ||
| Hamilton Rating Scale for Depression-17 | 18.3 (2.6) | 18 [15–22] | 18.3 (3.9) | 18.5 [11–23] |
| Hamilton Rating Scale for Depression-25 | 23.1 (3.0) | 24 [19–28] | 22.8 (4.2) | 23 [17–30] |
| Young Mania Rating Scale | 6.3 (2.6) | 7 [3–9] | 5.6 (2.0) | 5.5 [2–8] |
| Montgomery-Åsberg Depression Rating Scale | 21.7 (7.5) | 21 [12–32] | 24.5 (5.2) | 23 [16–32] |
| Duration of index depressive episode (weeks) | 14 [3–36] | 95 [2–950] | ||
| Number of prior depressive episodes (lifetime) | 9 [3–99] | 16 [1–99] | ||
| Number of prior hypomanic episodes (lifetime) | 14 [4–99] | 8.5 [1–99] | ||
| History of prior treatment with at least one antidepressant medicationa | 4 (57%) | 5 (50%) | ||
| History of prior treatment with at least one mood stabilizing medicationb | 1 (14%) | 2 (20%) | ||
| DSM-IV Axis I comorbidities | ||||
| Alcohol use disorder (lifetime) | 1 (14%) | 4 (40%) | ||
| Opiod use disorder (lifetime) | 0 | 1 (10%) | ||
| Cannabis use disorder (lifetime) | 1 (14%) | 0 | ||
| Generalized anxiety disorder | 2 (29%) | 5 (50%) | ||
| Panic disorder (current) | 0 | 4 (40%) | ||
| Social phobia (current) | 3 (44%) | 2 (20%) | ||
| Obsessive compulsive disorder (current) | 1 (14%) | 1 (10%) | ||
| Posttraumatic stress disorder (current) | 1 (14%) | 1 (10%) | ||
| Specific phobia (current) | 1 (14%) | 0 | ||
| Eating disorder NOS (current) | 1 (14%) | 0 | ||
Fluoxetine, sertraline, escitalopram, mirtazapine, paroxetine, venlafaxine, amitriptyline, imipramine, fluvoxamine, or buproprion.
Valproate or lamotrigine.
NOS = not otherwise specified.
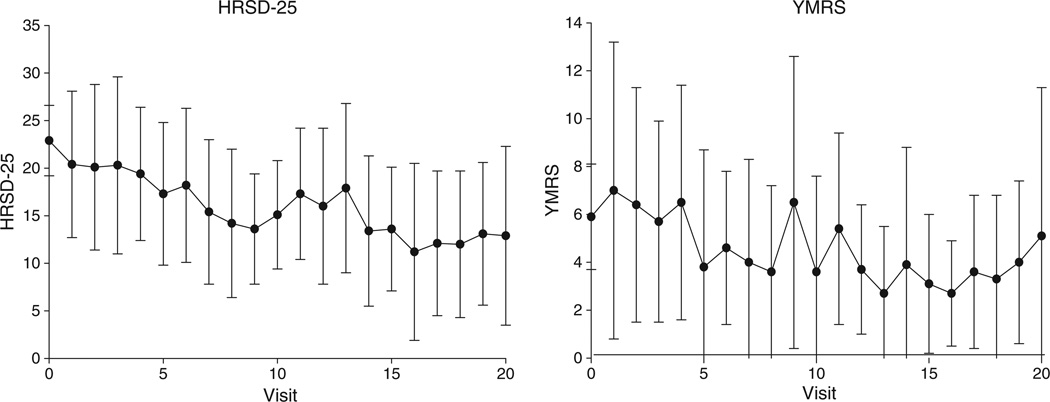
As shown in Fig. 1, there were significant improvements over time in both depressive and manic symptoms as measured by the HRSD-25 [F(1,15) = 13.27, p = 0.002], HRSD-17 [F(1,15) = 12.62, p = 0.003], YMRS [F(1,15) =6.46, p = 0.022], and MADRS [F(1,9) = 20.5, p = 0.001]; and in overall illness severity as measured by CGI-severity [F(1,14) = 4.87, p =0.045]. The decline in YMRS scores is notable because entry criteria limited YMRS scores to ≤10. There was, however, considerable variability in YMRS scores over time, even though the population was required to meet criteria for a depressive episode at study entry. Six subjects (35%) reached YMRS score ≥ 14 at least once during the trial.
Fig. 1.
Depression and mania scores decline over time with psychotherapy (error bars indicate ±1 standard deviation). HRSD-25 = 25-item version of the Hamilton Rating Scale for Depression; F(1,15) = 13.27, p = 0.002. YMRS = Young Mania Rating Scale; F(1,15) = 6.46, p = 0.022.
On categorical dimensions, by Visit 12, 41% (n = 7) of the sample responded to IPSRT monotherapy (defined as ≥50% reduction in depression scores and YMRS scores remaining ≤10). Eighteen percent (n = 3) did not respond to treatment. Because of patient safety concerns, one of these subjects had been declared a non-responder at Visit 8 and was placed on lamotrigine at that time. The other two subjects were started on lamotrigine at Visit 12. One of these two subjects refused to take medication and subsequently met criteria for response at Visit 14 with psychotherapy alone.
By Visit 20, 53% (9/17) achieved a response and 29% (5/17) achieved a full remission of symptoms. One responder at Visit 12 was symptomatic again at Visit 13 and was started on lamotrigine. This subject remained symptomatic for the remainder of the protocol and was no longer classified as a responder at Visit 20, despite addition of medication. Another responder at Visit 12 received lamotrigine from Visits 13 to 16 because of clinical worsening but was unable to tolerate the medication, then discontinued it at Visit 17 and met responder criteria at Visit 20 off of medication. Two of the non-responders at Visit 12 were classified as responders at Visit 20 (one subject was receiving lamotrigine and IPSRT; the other was receiving IPSRT alone). Eight of the nine subjects (89%) classified as responders and two of the three subjects (66%) classified as remitters at Visit 20 were on IPSRT monotherapy. Mean CSQ-8 scores were 26.8 (±5.1) and 27.6 (±5.9) at Visits 12 and 20, respectively.
Discussion
This proof of concept study demonstrates that it is feasible to treat depression in subjects suffering from BPII with IPSRT alone. Among those who remained in the study, satisfaction with the intervention was high. Response rates of 41% at Visit 12 compare favorably with trials of pharmacotherapy for bipolar depression (31), a phase of the illness that is, at least in BPI, notoriously difficult to treat (32). Interestingly, IPSRT may have contributed to significant declines in mania scores over the study period, despite the fact that subjects with elevated mania scores at baseline were excluded from the protocol. On the other hand, the high degree of fluctuation in YMRS scores over time draws attention to the importance of attending to subsyndromal hypomanic symptoms and mixed states in this population—even when one is allegedly treating individuals with ‘depression only’.
The size of the study limits the ability to detect factors that might predict those patients who are more or less likely to respond to IPSRT alone. There were no statistically significant differences between responders and non-responders in demographic or clinical characteristics, although there was a nonsignificant trend suggesting that females were more likely to respond (50%) than males (29%). Of the two subjects who were tapered off of antidepressants prior to entry to the study, one individual dropped out after Visit 2 and the other was a non-responder at both Visits 12 and 20, raising the possibility that medication taper is negatively associated with IPRST monotherapy response. Larger studies would be needed to formally evaluate moderators of outcome.
There are many limitations to this study. The small sample size and absence of a control group limit generalizability of findings. Low remission rates (29%) at Visit 20 suggest that longer treatment periods, novel treatment strategies such as sequences of medications and psychotherapy, or additional refinement of IPSRT specifically for the BPII population may be required to achieve wellness for some individuals. Nonetheless, the idea that substantial clinical gains are possible with psychotherapy alone in a subset of patients with BPII has important clinical implications, especially for individuals unable to tolerate pharmacotherapy or unwilling to incur risks associated with medications typically prescribed for this disorder, such as metabolic derangements, weight gain, or fetal teratogenicity (18). Future controlled studies will be needed to confirm the efficacy of this approach and to determine which subset of individuals is most likely to benefit from psychotherapy alone.
Acknowledgements
This work was supported by grants from the National Institute of Mental Health (K23 MH64518) and the National Alliance for Research in Schizophrenia and Affective Disorders (NARSAD Young Investigator Award to HAS).
HAS has received honoraria for CME presentations from AstraZeneca and Bristol-Myers Squibb; has served as a member of the speakers bureau for Bristol-Myers Squibb; and has served as a consultant to Novartis. EF has received grant support from Forest Research Institute and royalties from Guilford Press; has served as a consultant to and advisory board member for Eli Lilly & Co., Servier, and Novartis; and has served as a consultant to Pfizer.
Footnotes
DRF, DN and PH have no competing interests to report.
References
- 1.Regier DA, Farmer ME, Rae DS, et al. One-month prevalence of mental disorders in the United States and sociodemographic characteristics: the Epidemiologic Catchment Area study. Acta Psychiatr Scand. 1993;88:35–47. doi: 10.1111/j.1600-0447.1993.tb03411.x. [DOI] [PubMed] [Google Scholar]
- 2.Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–151. doi: 10.1016/s0165-0327(98)00142-6. [DOI] [PubMed] [Google Scholar]
- 3.Angst J, Gamma A, Benazzi F, Ajdacic V, Eich D, Rossler W. Toward a re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J Affect Disord. 2003;73:133–146. doi: 10.1016/s0165-0327(02)00322-1. [DOI] [PubMed] [Google Scholar]
- 4.Koukopoulos A, Faedda G, Proietti R, D’Amico S, de Pisa E, Simonetto C. Un syndrome depressif mixte. Encephale. 1992;18:19–21. [PubMed] [Google Scholar]
- 5.Akiskal HS, Bourgeois ML, Angst J, Post R, Moller H, Hirschfeld R. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000;59(Suppl. 1):S5–S30. doi: 10.1016/s0165-0327(00)00203-2. [DOI] [PubMed] [Google Scholar]
- 6.Benazzi F. Course and outcome of bipolar II disorder: a retrospective study. Psychiatry Clin Neurosci. 2001;55:67–70. doi: 10.1046/j.1440-1819.2001.00786.x. [DOI] [PubMed] [Google Scholar]
- 7.Judd LL, Akiskal HS, Schettler PJ, et al. The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: a clinical spectrum or distinct disorders? J Affect Disord. 2003;73:19–32. doi: 10.1016/s0165-0327(02)00324-5. [DOI] [PubMed] [Google Scholar]
- 8.Maina G, Albert U, Bellodi L, et al. Health-related quality of life in euthymic bipolar disorder patients: differences between bipolar I and II subtypes. J Clin Psychiatry. 2007;68:207–212. doi: 10.4088/jcp.v68n0205. [DOI] [PubMed] [Google Scholar]
- 9.Berk M, Dodd S. Bipolar II disorder: a review. Bipolar Disord. 2005;7:11–21. doi: 10.1111/j.1399-5618.2004.00152.x. [DOI] [PubMed] [Google Scholar]
- 10.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: a 1-Year randomized trial from the Systematic Treatment Enhancement Program. Arch Gen Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simon GE, Ludman EJ, Unutzer J, Bauer MS, Operskalski B, Rutter C. Randomized trial of a population-based care program for people with bipolar disorder. Psychol Med. 2005;35:13–24. doi: 10.1017/s0033291704002624. [DOI] [PubMed] [Google Scholar]
- 12.Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: part II. Impact on clinical outcome, function, and costs. Psychiatr Serv. 2006;57:937–945. doi: 10.1176/ps.2006.57.7.937. [DOI] [PubMed] [Google Scholar]
- 13.Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: part I. Intervention and implementation in a randomized effectiveness trial. Psychiatr Serv. 2006;57:927–936. doi: 10.1176/ps.2006.57.7.927. [DOI] [PubMed] [Google Scholar]
- 14.Elkin I, Shea MT, Watkins JT, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry. 1989;46:971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- 15.Swartz HA, Frank E, Frankel DR. Psychothérapie interpersonnelle et des rhythmes sociaux (PTIRS) dans le trouble bipolaire II: structure du traitement et exemples cliniques. Santé Ment Qué. doi: 10.7202/019673ar. (in press) [DOI] [PubMed] [Google Scholar]
- 16.Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- 17.Hadjipavlou G, Mok H, Yatham LN. Pharmacotherapy of bipolar II disorder: a critical review of current evidence. Bipolar Disord. 2004;6:14–25. doi: 10.1046/j.1399-5618.2003.00086.x. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002;159(April Suppl):1–50. [PubMed] [Google Scholar]
- 19.Frank E. Treating Bipolar Disorder: A Clinician’s Guide to Interpersonal and Social Rhythm Therapy. New York: Guilford Press; 2005. [Google Scholar]
- 20.Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- 21.Malkoff-Schwartz S, Frank E, Anderson B, et al. Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes. Arch Gen Psychiatry. 1998;55:702–707. doi: 10.1001/archpsyc.55.8.702. [DOI] [PubMed] [Google Scholar]
- 22.Frank E, Swartz HA, Boland E. Interpersonal and social rhythm therapy: an intervention addressing rhythm dysregulation in bipolar disorder. Dialogues Clin Neurosci. 2007;9:325–332. doi: 10.31887/DCNS.2007.9.3/efrank. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Arch Gen Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;25:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young RC, Biggs JT, Zeigler VE, Meyer DA. A rating scale for mania: reliability, validity, and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 26.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) New York: New York State Psychiatric Institute, Biometrics Research; 1995. [Google Scholar]
- 27.Thase ME, Carpenter L, Kupfer DJ, Frank EF. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacol Bull. 1991;27:17–22. [PubMed] [Google Scholar]
- 28.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 29.Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the clinical global impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73:159–171. doi: 10.1016/s0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- 30.Attkisson CC, Greenfield TK. The client satisfaction questionnaire-8 and the service satisfaction questionnaire-30. In: Maruish M, editor. The Use of Psychological Testing for Treatment Planning and Outcome Assessment. Hillsdale, NJ: Lawrence Earlbaum Associates; 1994. pp. 402–422. [Google Scholar]
- 31.Thase ME, Sachs GS. Bipolar depression: pharmacotherapy and related therapeutic strategies. Biol Psychiatry. 2000;48:558–572. doi: 10.1016/s0006-3223(00)00980-x. [DOI] [PubMed] [Google Scholar]
- 32.Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711–1722. doi: 10.1056/NEJMoa064135. [DOI] [PubMed] [Google Scholar]