Abstract
The high prevalence of methicillin-resistant Staphylococcus aureus (MRSA) ST398 among pigs in certain European countries and North America and its occurrence in other animal species raises a question concerning the molecular mechanisms mediating the success of this lineage. In this study a panel of S. aureus strains belonging to sequence type (ST) 5 (n = 4), ST8 (n = 5), ST15 (n = 5), ST22 (n = 8), clonal complex (CC) 30 (n = 8), CC97 (n = 8), CC130 (n = 4), CC151 (n = 4) and ST398 (n = 18) were screened by DNA microarray and PCR for the carriage of virulence and antimicrobial resistance genes. Isolates belonging to the same sequence type/clonal complex (ST/CC) were found to share similar virulence gene profiles. The ST398 lineage displayed the lowest content of virulence genes, which consisted mainly of genes detected among the majority or all of the analysed lineages. All MRSA ST398 isolates lacked accessory virulence genes that were detected in other ST/CC. In contrast to virulence genotype, the antimicrobial resistance genes profiles varied between isolates belonging to the same ST/CC and profile similarities could be observed for isolates from different lineages. MRSA ST398 isolates in particular displayed significant diversity and high content of antimicrobial resistance genes. This was comparable with certain MRSA belonging to other sequence types particularly the equine MRSA ST8. The apparent lack of significant virulence genes among MRSA ST398 strains, demonstrates that the lineage features a unique genetic background but no ST398-specific virulence markers could be identified.
Introduction
Molecular epidemiological studies on S. aureus in humans has shown that the population consists of several prevalent lineages [1], which are best illustrated by the hospital- and community-acquired methicillin-resistant S. aureus strains where specific clonal complexes are dominant. The existence of such lineages among animal-associated isolates has also been identified and can be exemplified by strains causing mastitis in cattle. Whole genome sequence analysis of cattle-associated strains belonging to CC133 and CC151 has revealed evidence of genomic adaptations towards the bovine host, more specifically the bovine udder environment [2], [3]. S. aureus lineages associated with other animal species have also been described such as CC5 which is highly prevalent among poultry and CC8 that is commonly isolated from horses [4], [5].
Animal-associated isolates of S. aureus that are methicillin-resistant are of both veterinary and medical interest and have been the subject of extensive research over the past 5 years. The MRSA ST398 emerged as primarily a pig-associated strain, which has been found to be highly prevalent among pig herds in several countries in Europe and North America [6]–[9]. However, MRSA ST398 has also been isolated from other animal species such as cattle, poultry and horses [10]–[12]. Transfer of MRSA ST398 between animals and humans has been reported but the strain has also been isolated from persons with no history of livestock contact [13]–[15]. This exemplifies a probable lack of host specificity of this S. aureus strain. Nevertheless, the apparent recent emergence and rapid dissemination of MRSA ST398 among food-producing animals raises the question of what factors might have mediated the success of this lineage as livestock coloniser. Factors associated with pig husbandry such as movement of animals between different types of pig farms, use of antimicrobials and contact between animals and colonized personnel/veterinarians have been shown to be significant in occurrence and transmission of MRSA ST398 [16]. However, the molecular characteristics of ST398 should also be considered. The genomic analysis of various clonal complexes demonstrated clearly that S. aureus is an evolving pathogen and that around 22% of S. aureus genome consists of strain-specific elements that can mediate host or niche adaptation [17]. Identification of genetic markers that distinguish the ST398 lineage might help in determining and understanding the mechanisms behind MRSA ST398 capacity for livestock colonisation.
In this study S. aureus isolates consisting of MRSA ST398 as well as MSSA and MRSA belonging to other ST/CC prevalent among either humans or animals, were characterised for virulence and antimicrobial resistance gene profiles. The comparator panel consisted of: ST5, ST8, ST15, ST22, CC30, CC97, CC130 and CC151. Strains belonging to ST5 have been previously reported as common among community acquired (CA) isolates [18] whereas ST15 has been reported to represent a successful lineage among CA- and hospital-acquired (HA) MSSA isolates [19]–[21]. ST22 and CC30 represent the two dominant HA-MRSA lineages that have become epidemic in the UK hospitals [22] whereas CC97, CC130 and CC151 represent predominant bovine-specific lineages [23]–[28]. ST8 is a successful lineage of both CA- and HA-MRSA [29] although in this study the ST8 group consisted of human MSSA and horse MRSA. The aim of the study was to conduct inter-lineage comparative analysis to determine whether MRSA ST398 strains carry any lineage-specific molecular markers. We also wanted to investigate the similarities and variations in virulence and antimicrobial resistance genotypes between ST398 and other analysed ST/CC to determine if MRSA ST398 shares any significant similarities with other prevalent lineages of S. aureus.
Results
Genetic Background of the Strains
The main genotypic features of isolates (spa type, multilocus sequence type, clonal complex and SCCmec type) are summarised in Table 1. 33 spa types and 13 MLST were detected. Spa type t011 was the most prevalent among MRSA ST398 isolates (n = 10). t034 and t567 were identified in 3 isolates each, with t1451 and t4872 detected in single isolate only. Considerable spa type variation was observed for MSSA isolates belonging to ST5, ST15, CC30 and CC97 where each spa type was detected in no more than two isolates. All human ST8 isolates carried spa type t008 whereas both animal isolates were t064. The majority of ST22 isolates belonged to spa type t032 (n = 4) and all but one of CC130 isolates were t843 (n = 3). All CC151 isolates carried spa type t529. The most prevalent SCCmec among MRSA strains was type IV (n = 20), which was detected in all ST8, ST22 and CC30 MRSA strains as well as majority of ST398. SCCmec type V was also detected but only among ST398 (n = 6). Three ST398 strains were non-typeable (NT).
Table 1. Genotypic features of strains characterised in this study.
| No | ID | Host | spa | STa | CCb | mecA c | SCCmec d |
| 1 | 25 | Human | t002 | 5 | 5 | – | – |
| 2 | 8 | Human | t179 | 5 | 5 | – | – |
| 3 | 17 | Human | t442 | 5 | 5 | – | – |
| 4 | 19 | Human | t442 | – | (5) | – | – |
| 5 | 6 | Human | t008 | 8 | 8 | – | – |
| 6 | 11 | Human | t008 | – | (8) | – | – |
| 7 | 16 | Human | t008 | – | (8) | – | – |
| 8 | 200 | Horse | t064 | 8 | 8 | + | IVd |
| 9 | 201 | Horse | t064 | – | (8) | + | IVd |
| 10 | 10 | Human | t084 | 15 | 15 | – | – |
| 11 | 21 | Human | t084 | – | (15) | – | – |
| 12 | 23 | Human | t228 | 15 | 15 | – | – |
| 13 | 60 | Human | t360 | 15 | 15 | – | – |
| 14 | 24 | Human | t491 | 15 | 15 | – | – |
| 15 | 38 | Human | t020 | 22 | 22 | + | IVh |
| 16 | 44 | Human | t032 | 22 | 22 | + | IVh |
| 17 | 28 | Human | t032 | – | (22) | + | IVh |
| 18 | 32 | Human | t032 | – | (22) | + | IVh |
| 19 | 40 | Human | t032 | – | (22) | + | IVh |
| 20 | 39 | Human | t379 | 22 | 22 | + | IVh |
| 21 | 18 | Human | t608 | 22 | 22 | – | – |
| 22 | 20 | Human | unknown | 22 | 22 | – | – |
| 23 | 5 | Human | t012 | 30 | 30 | – | – |
| 24 | 13 | Human | t012 | – | (30) | – | – |
| 25 | 34 | Human | t018 | 36 | 30 | + | IVh |
| 26 | 65 | Human | t018 | – | (30) | + | IV |
| 27 | 51 | Human | t019 | 30 | 30 | – | – |
| 28 | 62 | Human | t021 | 30 | 30 | – | – |
| 29 | 1 | Human | t122 | 30 | 30 | – | – |
| 30 | 31 | Human | t1675 | 36 | 30 | + | IV |
| 31 | 174 | Cattle | t131 | 1527 | 97 | – | – |
| 32 | 189 | Cattle | t224 | 97 | 97 | – | – |
| 33 | 198 | Cattle | t224 | – | (97) | – | – |
| 34 | 177 | Cattle | t267 | 118 | 97 | – | – |
| 35 | 197 | Cattle | t267 | – | (97) | – | – |
| 36 | 190 | Cattle | t359 | 97 | 97 | – | – |
| 37 | 195 | Cattle | t359 | – | (97) | – | – |
| 38 | 175 | Cattle | t521 | 97 | 97 | – | – |
| 39 | 173 | Cattle | t6220 | 130 | 130 | + | – |
| 40 | 178 | Cattle | t843 | 1245 | 130 | + | – |
| 41 | 181 | Cattle | t843 | – | (130) | + | – |
| 42 | 182 | Cattle | t843 | – | (130) | + | – |
| 43 | 179 | Cattle | t529 | 1074 | 151 | – | – |
| 44 | 193 | Cattle | t529 | – | (151) | – | – |
| 45 | 194 | Cattle | t529 | – | (151) | – | – |
| 46 | 199 | Cattle | t529 | – | (151) | – | – |
| 47 | 90 | Chicken | t011 | 398 | 398 | + | IVc |
| 48 | 91 | Chicken | t011 | – | (398) | + | V 5C2&5 |
| 49 | 92 | Chicken | t011 | – | (398) | + | IVa |
| 50 | 99 | Horse | t011 | – | (398) | + | IVa |
| 51 | 102 | Rat | t011 | – | (398) | + | IVa |
| 52 | 103 | Rat | t011 | – | (398) | + | V 5C2&5 |
| 53 | 105 | Cattle | t011 | – | (398) | + | IVa |
| 54 | 106 | Cattle | t011 | – | (398) | + | V 5C2&5 |
| 55 | 108 | Pig | t011 | – | (398) | + | V 5C2&5 |
| 56 | 109 | Pig | t011 | – | (398) | + | IVa |
| 57 | 95 | Human | t034 | 398 | 398 | + | V 5C2&5 |
| 58 | 96 | Human | t034 | – | (398) | + | IVc |
| 59 | 111 | Pig | t034 | – | (398) | + | IVa |
| 60 | 101 | Horse | t1451 | 398 | 398 | + | IVa |
| 61 | 104 | Rat | t4872 | 398 | 398 | + | V 5C2&5 |
| 62 | 93 | Chicken | t567 | 398 | 398 | + | NT |
| 63 | 107 | Cattle | t567 | – | (398) | + | NT |
| 64 | 110 | Pig | t567 | – | (398) | + | NT |
‘-‘ not determined;
determined or presumptive (based on spa type);
‘-‘ absent, ‘+’ present;
‘-‘ not applicable, NT: non-typeable.
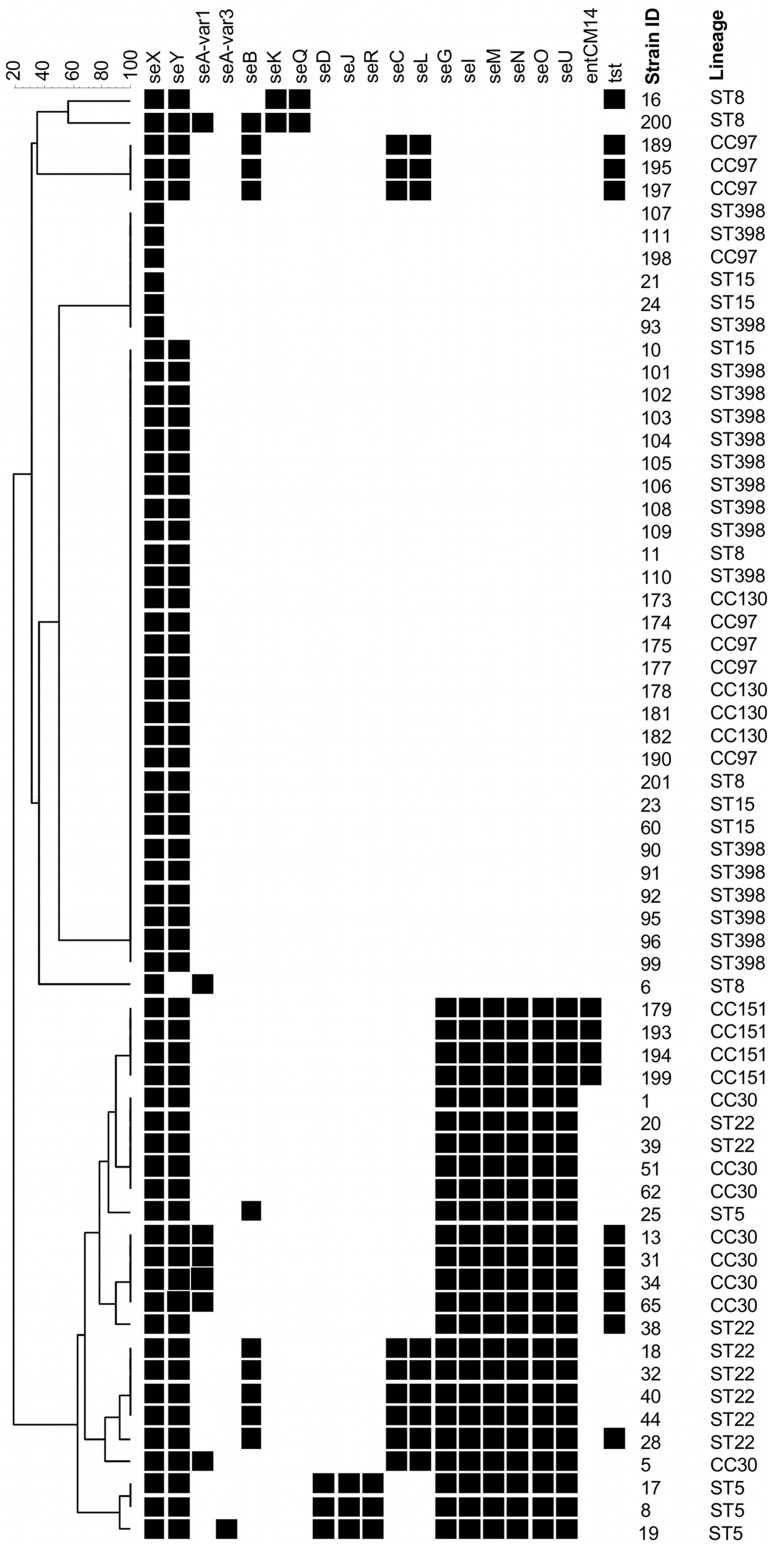
Superantigen Genes
The carriage of enterotoxin genes is presented in Figure 1 and Table 2. Enterotoxin gene seX was detected in all analysed isolates while seY was identified in all analysed ST/CC but was absent in 7 isolates from various lineages (ST8, ST15, CC97 and ST398). Enterotoxin A gene seA was detected at low prevalence in three ST/CC: ST5 (n = 1), ST8 (n = 2), CC30 (n = 5). The seB+seK+seQ enterotoxin gene cluster was detected in a single ST8 isolate, with another ST8 isolate carrying the seK+seQ only. Furthermore, several isolates belonging to various lineages were positive for seB only: ST5 (n = 1), ST22 (n = 5), CC97 (n = 3). The seD+seJ+seR cluster was identified in all but one ST5 isolates and no other ST/CC group whereas the seC+seL genes were present in 9 isolates belonging to ST22 (n = 5), CC30 (n = 1) and CC97 (n = 3). The egc cluster: seG+seI+seM+seN+seO+seU was prevalent among isolates belonging to ST5, ST22, CC30 and CC151 but absent from all other ST/CC. The entCM14 gene was present in all CC151 isolates and no other lineage. Finally, the tst gene was variably detected in several ST/CC: ST8 (n = 1), ST22 (n = 2), CC30 (n = 4), and CC97 (n = 3). All isolates were negative for seE and seH. The ST398 isolates carried no accessory enterotoxin genes, which was also observed for all ST15 and CC130 isolates.
Figure 1. Superantigen gene profiles.
UPGMA dendrogram displaying clustering and genetic similarity (using Jaccard’s coefficient) of superantigen gene profiles of analysed strains. Black box – positive; grey – ambiguous; white/blank – negative.
Table 2. Comparison of the distribution of selected virulence genes/gene clusters that were detected at high frequency among some of the analysed lineages.
| Number of positive isolates | |||||||||
| ST398 | ST5 | ST8 | ST15 | ST22 | CC30 | CC97 | CC130 | CC151 | |
| (n = 18) | (n = 4) | (n = 5) | (n = 5) | (n = 8) | (n = 8) | (n = 8) | (n = 4) | (n = 4) | |
| seD+seJ+seR | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| seC+seL | 0 | 0 | 0 | 0 | 5 | 1 | 3 | 0 | 0 |
| egc | 0 | 4 | 0 | 0 | 8 | 8 | 0 | 0 | 4 |
| entCM14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| lukF-PV-P83/lukM | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| lukD/E+splA+splB | 0 | 4 | 3 | 4 | 0 | 0 | 8 | 0 | 4 |
| hlb | 9 | 0 | 2 | 0 | 1 | 0 | 6 | 4 | 4 |
| sak | 0 | 4 | 3 | 0 | 7 | 8 | 0 | 0 | 0 |
| hl-III | 18 | 4 | 5 | 5 | 0 | 8 | 6 | 0 | 0 |
| edinB | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 |
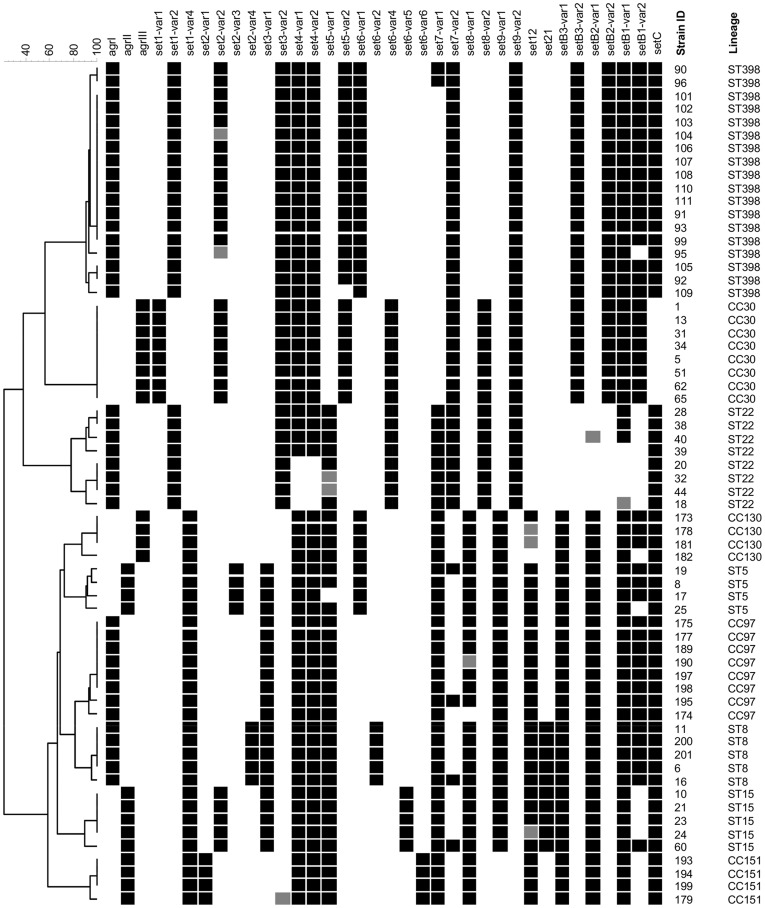
agr Locus and set Genes
The carriage of set genes and agr type is presented in Figure 2. Strains belonging to the same lineage displayed an identical accessory gene regulator (agr) type: ST8, ST22, CC97 and ST398 harboured agrI; ST5, ST15 and CC151 displayed agrII; whereas CC30 and CC130 contained agrIII. The set genes encode staphylococcal exotoxin-like proteins. The inter-lineage variation for set carriage can be defined by two factors: presence/absence of a particular gene and the allelic variant. The following genes: set1, set4, set5 and set7 were detected in all ST/CC but the allelic variant differed between lineages (all set4-positive isolates are displayed to carry both set4-var1 and set4-var2 as due to a strong cross-reactivity of the probes the true positive variant could not be identified). Other frequently identified set genes were also: set3 (not detected in CC130), set6 (not detected in CC97), set8 (not detected in ST398), set9 (not detected in CC151). For set6, the majority of isolates were found to carry one of four of the previously described allelic variants. Isolates belonging to ST15 and CC151 displayed a distinct combination of probes, different for both lineages, and were termed var5 and var6, respectively. Common but less prevalent were also: set2 (detected in ST5, ST8, ST15, CC30, CC151 and ST398) and set12 (detected in ST5, ST8, ST15, CC97, CC130 and CC151). The set21 gene was detected only in ST8 and ST15. A complete setB gene cluster, which consists of setB3, setB2 and setB1, was detected in all ST/CC except ST22. The setC gene was also highly prevalent and could be detected in all isolates apart from those belonging to CC30 group.
Figure 2. agr and set gene profiles.
UPGMA dendrogram displaying clustering and genetic similarity (using Jaccard’s coefficient) of agr and set gene profiles of analysed strains. Black box – positive; grey – ambiguous; white/blank – negative.
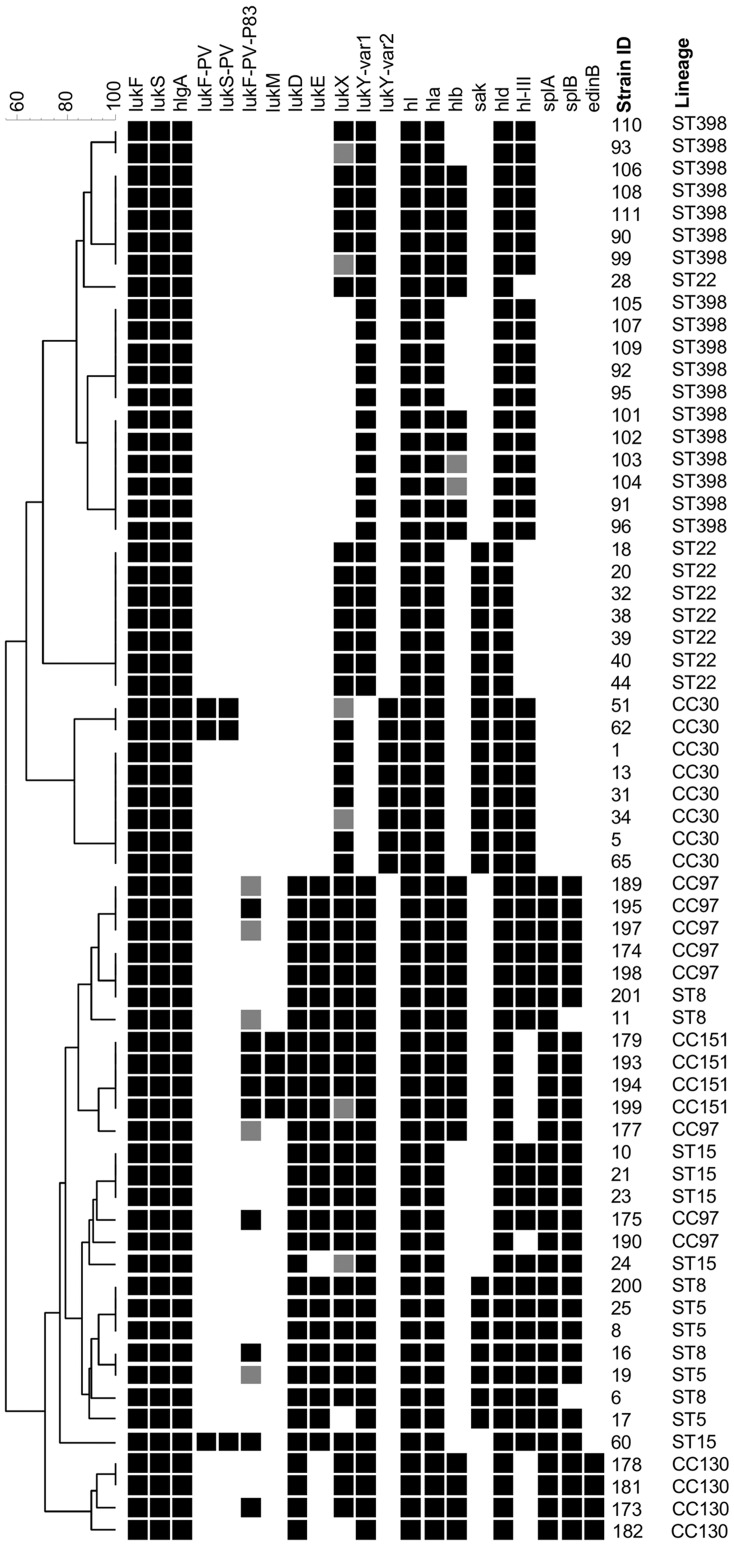
Leukocidin, Haemolysin and Other Virulence Genes
The carriage of leukocidin, haemolysin and other virulence genes is presented in Figure 3 and Table 2. All isolates carried lukF/S, hlgA, hl, hla, hld and lukY genes. lukX was detected in all ST/CC but not all analysed isolates. The lukD+lukE, splA and splB genes, known to reside together on an allelic variant of Saβ genomic island, were all detected in all or majority of isolates belonging to ST5, ST8 (two isolates splB negative), ST15 (one isolate lukE negative), CC97 and CC151. The genes, except for lukE, were also detected among CC130 isolates. The lukF-PV-P83/lukM genes were detected in all CC151 isolates and no other lineage. However, the lukF-PV-P83 only was variably detected among isolates belonging to ST5, ST8 and CC97. The PVL leukocidin genes lukF/S-PV were identified only among isolates belonging to ST15 (n = 1) and CC30 (n = 2). An intact hlb gene (not disrupted by hlb-converting bacteriophage) was present in all isolates belonging to CC130 and CC151, as well as in isolates belonging to ST8 (n = 2), ST22 (n = 1), CC97 (n = 5) and ST398 (n = 9). Among hlb-negative isolates the sak gene was detected in over 60% (22/36), mainly those belonging to ST5 (n = 4), ST22 (n = 7) and CC30 (n = 8). The hl-III haemolysin gene was found in all isolates belonging to ST5, ST8, ST15, CC30 and ST398 as well as majority of CC97 (n = 6). Finally edinB was identified among all CC130 isolates but was absent in all other analysed lineages. All isolates were negative for etA, etB, etD, edinA and edinC.
Figure 3. Leukocidin, haemolysin and other virulence gene profiles.
UPGMA dendrogram displaying clustering and genetic similarity (using Jaccard’s coefficient) of leukocidin, haemolysin and other virulence gene profiles of analysed strains. Black box – positive; grey – ambiguous; white/blank – negative.
Adhesion Genes
The carriage of adhesion genes is presented in Figure 4. The genes: clfB, ebpS, fnbA, icaA and icaD were identified in all isolates. Other highly prevalent adhesion genes were: clfA (not detected in CC130), eno (not detected in ST398), fib (not detected in ST22), sdrC (not detected in ST5 and ST22) and sdrE (not detected in CC30 and CC151). Less common but also detected among analysed lineages were: bbp (detected in CC30 and CC151), cna (detected in ST22, CC30 and ST398), fnbB (detected in ST8, ST15, CC97 and ST398), sasG (detected in ST5, ST8 and CC97) and sdrD (detected in ST5, ST8, ST15, ST22 and CC97). The PCR detection of adhesion genes was specific and single bands only of expected size were observed.
Figure 4. Adhesion gene profiles.
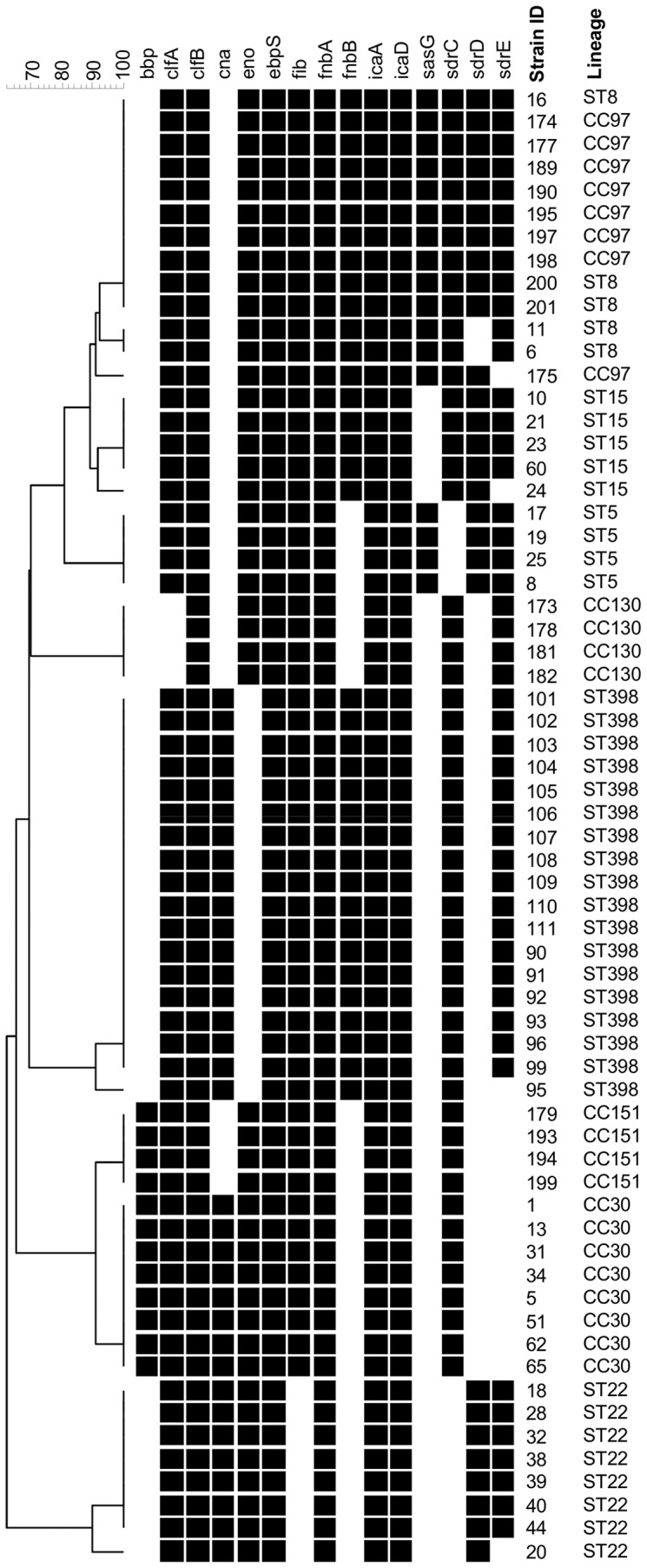
UPGMA dendrogram displaying clustering and genetic similarity (using Jaccard’s coefficient) of adhesion gene profiles of analysed strains. Black box – positive; grey – ambiguous; white/blank – negative.
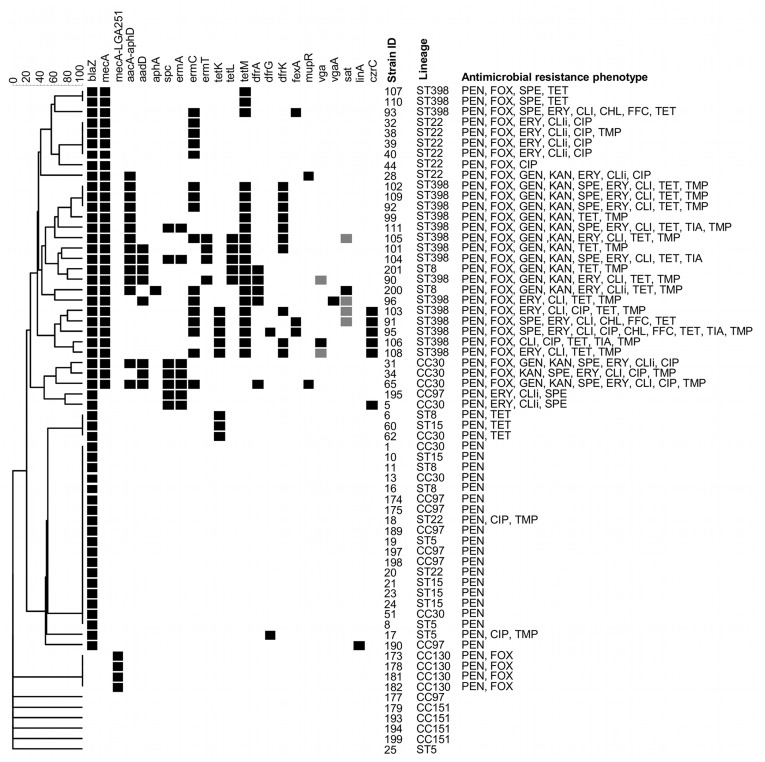
Antimicrobial Resistance Phenotypes and Genotypes
The results are presented in Figure 5 and Table 3. The majority of analysed isolates displayed penicillin resistance (n = 58). Methicillin resistance was detected for all isolates belonging to ST398 and CC130 as well as among equine ST8 (n = 2), ST22 (n = 6) and CC30 (n = 3) isolates. All ST398 isolates also displayed resistance to tetracycline, which was also detected among ST8 (n = 3), ST15 (n = 1) and CC30 (n = 1). Gentamicin-kanamycin resistant isolates included ST398 (n = 9), equine ST8 (n = 2), ST22 (n = 1) and CC30 (n = 2). A single isolate belonging to CC30 was kanamycin-resistant but gentamicin susceptible. Spectinomycin resistance was detected among ST398 (n = 10), CC30 (n = 4) and CC97 (n = 1). Erythromycin-clindamycin resistant isolates consisted of ST398 (n = 13), equine ST8 (n = 1), ST22 (n = 5), CC30 (n = 4) and CC97 (n = 1). One other isolate belonging to ST398 was clindamycin-resistant but susceptible to erythromycin. Resistance to trimethoprim was identified among ST398 (n = 13), ST5 (n = 1), equine ST8 (n = 2), ST22 (n = 2) and CC30 (n = 2). Chloramphenicol-florfenicol as well as tiamulin resistance was detected among ST398 isolates only (n = 3, n = 4, respectively). Resistance to ciprofloxacin was detected among ST398 (n = 3), ST5 (n = 1), ST22 (n = 7) and CC30 (n = 3). All isolates were susceptible to apramycin, vancomycin and teicoplanin.
Figure 5. Antimicrobial resistance genotypes and phenotypes.
UPGMA dendrogram displaying clustering and genetic similarity (using Jaccard’s coefficient) of antimicrobial resistance gene profiles of analysed strains. Black box – positive; grey – ambiguous; white/blank – negative. The far right column shows antimicrobial resistance phenotype. PEN, penicillin; FOX, cefoxitin; GEN, gentamicin; KAN, kanamycin; SPE, spectinomycin; CLI, clindamycin; ERY, erythromycin; CIP, ciprofloxacin; CHL, chloramphenicol; FFC, florfenicol; TET, tetracycline; TIA, tiamulin; TMP, trimethoprim; i, inducible.
Table 3. Comparison of the distribution of selected resistance genes among MRSA strains analysed in this study.
| Number of positive isolates | ||||
| ST398 | ST8 | ST22 | CC30 | |
| (n = 18) | (n = 2) | (n = 6) | (n = 3) | |
| aacA-aphD | 9 | 2 | 1 | 2 |
| aadD | 4 | 1 | 0 | 3 |
| aphA | 0 | 1 | 0 | 0 |
| spc | 2 | 0 | 0 | 3 |
| ermA | 2 | 0 | 0 | 3 |
| ermC | 10 | 1 | 4 | 1 |
| ermT | 4 | 0 | 0 | 0 |
| tetK | 5 | 0 | 0 | 0 |
| tetL | 4 | 1 | 0 | 0 |
| tetM | 18 | 2 | 0 | 0 |
| dfrA | 2 | 2 | 0 | 1 |
| dfrG | 1 | 0 | 0 | 0 |
| dfrK | 10 | 0 | 0 | 0 |
The blaZ gene was detected in 84% of analysed isolates. The blaZ-negative isolates included all CC130 and CC151 strains. The mecA gene was identified in all ST398 strains as well as among isolates belonging to ST8 (n = 2), ST22 (n = 6) and CC30 (n = 3). All CC130 strains carried the mecA homologue - mecA LGA251. The aacA-aphD was the most common aminoglycoside resistance gene and it was detected in various lineages: ST398 (n = 9), ST8 (n = 2), ST22 (n = 1) and CC30 (n = 2). The aadD gene was found in ST398 (n = 4), ST8 (n = 1) and CC30 (n = 3) with all but two of these isolates also carrying the aacA-aphD. Single isolate belonging to ST8 carried the aphA gene (also aacA-aphD positive). The erythromycin resistance gene ermA was mainly detected in isolates belonging to CC30 (n = 4) but was also found among ST398 (n = 2) and CC97 (n = 1). All ermA-positive isolates carried also the spectinomycin resistance gene spc. More common among ST398 isolates was the ermC gene (n = 10), also detected in ST8 (n = 1) and ST22 (n = 4). The ermT gene was detected among ST398 isolates only (n = 4). All ST398 strains were positive for the tetM gene, which was also detected in equine ST8 (n = 2) isolates. The tetK gene was detected among ST398 (n = 5), ST8 (n = 1), ST15 (n = 1) and CC30 (n = 1). Furthermore, the tetL gene was found in ST398 (n = 4) as well as ST8 (n = 1). The trimethoprim resistance genes were prevalent mainly among ST398 with 55% of isolates carrying the dfrK gene (n = 10), which was not detected in any other lineage. The dfrA was identified in ST398 (n = 2), ST8 (n = 2) and CC30 (n = 1). The dfrG gene was detected in two isolates, one belonging to ST398 and other to ST5. The chloramphenicol-florfenicol resistance gene fexA was detected among ST398 isolates only (n = 3). The czrC, cadmium and zinc resistance gene, recently found to be associated with the SCCmec element from MRSA ST398, was identified in all but one ST398 isolates carrying the SCCmec type V as well as in a single MSSA isolate belonging to CC30. The detection of resistance genes by PCR was specific and single bands only of expected size were observed. Ambiguous DNA microarray results were obtained for vga and sat genes among some ST398 strains.
In summary, the MRSA ST398 isolates displayed a considerable antimicrobial resistance genotype heterogeneity as well as diversity. This feature was not, however, strictly restricted to the ST398 lineage. High content of antimicrobial resistance genes could also be observed in MRSA strains belonging to ST8 and CC30, with MRSA ST22 displaying a comparatively lower prevalence of resistance determinants.
Discussion
The DNA microarray-based analysis revealed a limited content of virulence determinants among MRSA ST398 isolates in comparison to the representatives of other ST/CC included in this study. The absence of significant virulence factors among isolates belonging to ST398 has been previously observed and later confirmed by the whole genome analysis of a MRSA ST398 strain [12], [30], [31]. The majority of virulence genes that were detected among ST398 strains were common among all ST/CC and represent the core virulence genes of S. aureus. We identified several genes that, although not unique to the ST398 lineage, were not prevalent among all analysed lineages and thus might mediate the ST398 ability for enhanced animal colonisation.
An intact hlb, which encodes a beta-haemolysin, was detected in 50% of ST398 isolates as well as in all or majority of cattle-associated isolates belonging to CC97, CC130 and CC151. The gene is chromosomally located but might become inactivated by insertion of hlb-converting phages that carry immune evasion genes such as sak, chp and scn [32]–[35]. Although these elements can provide the strain with a selective advantage, they encode human-specific molecules [35]. As such, the carriage of staphylokinase gene sak is prevalent among human strains whereas the presence of an intact hlb is common among cattle isolates [36], [37]. In this study all isolates carrying an intact hlb were negative for sak, confirming that the presence of an intact hlb gene and carriage of sak is commonly antagonistic. Some of the isolates belonging to ST15, CC97 and ST398 carried a disrupted hlb but were sak-negative, which might indicate an insertion of a different phage. Nevertheless the failure to detect sak among any of the ST398 isolates and presence of an intact hlb gene could suggest a lack of adaptation for the human host and/or mechanism for animal-specific colonisation.
Two of the adhesion genes detected among ST398 isolates displayed limited prevalence among other ST/CC: fnbB and cna. The fnbB gene is a homologue of fnbA and both genes encode fibronectin-binding protein. Although fnbA is highly prevalent and was identified in all analysed isolates, the fnbB gene was only detected in ST8, ST15, CC97 and ST398. It has been shown that the presence of both fnbA and fnbB can significantly enhance biofilm formation in MRSA isolates [38]. The importance of fnbA+fnbB carriage among ST398 isolates is unclear in the context of animal-specific colonisation as the cooperative function of fnbA- and fnbB-expressed molecules was shown to be significant for the development of systemic infection [39]. Of higher significance might be the carriage of collagen adhesion gene cna by all ST398 isolates. It was detected in only two other lineages, namely ST22 and CC30. The cna gene was previously reported as prevalent among pandemic CA-MRSA isolates belonging to ST30 [40]. It was also suggested that the gene might play role in facilitating stable colonisation [41].
The analysis of lineages other than ST398 revealed a probable association between certain virulence genes and specific ST/CC. The lukF-PV-P83/lukM locus, which encodes a bi-component leukotoxin that is highly active against bovine neutrophils, was previously reported to be common among cattle isolates related to the RF122 strain [42]. Similarly, in this study the lukF-PV-P83/lukM locus was detected only among CC151 isolates. The enterotoxin gene cluster egc was found among all ST5, ST22, CC30 and CC151 strains. This cluster has been previously reported to be more common in carriage strains than invasive isolates and to be prevalent among nasal isolates [41], [43]. In this study such association could not be determined; instead the egc cluster appears to be prevalent among specific S. aureus lineages. Our data also shows that the allelic variant of staphylococcal genomic island vSaβ carrying splA, splB and lukD/lukE genes might be prevalent in isolates belonging to ST5, ST8, ST15, CC97, CC130 and CC151.
We found a varying level of similarity in virulence genotypes between the ST398 lineage and other ST/CC. The comparison of superantigen genotypes revealed that the lack of enterotoxin genes is not a unique feature of ST398 as the same profile was identified for all isolates belonging to ST15 and CC130. Comparing genes associated with leukocidins, haemolysins and serine proteases shows that ST398 isolates most closely resemble the ST22 and CC30 groups as all lack lukD/lukE, splA and splB genes. These three lineages also displayed similar set gene profiles. Interestingly, both ST22 and ST398 lineages were found to carry CC30-specific allelic variants of some of the set genes. The exact function of set-encoded exotoxin-like proteins remains to be determined but it has been demonstrated that the set products exhibit immunostimulatory properties [44]. Identification of set markers that are shared between ST398 and other successful MRSA lineages such as ST22 and CC30 can provide candidate genes for further investigation of individual set genes and their role in host colonisation and infection.
The clustering of antimicrobial resistance genotypes was highly heterogeneous and profile similarity was observed for strains belonging to different ST/CC. It has been previously observed by Monecke et al [42] that the carriage of antibiotic resistance determinants is largely non-lineage specific due to the promiscuous nature of mobile genetic elements carrying them. Interestingly, the resistance profile of ST398 was most comparable to the two equine MRSA ST8 strains. They shared the aacA-aphD, aadD, ermC, tetL and dfrA genes with the ST398 isolates and most importantly both ST8 isolates carried tetM. This suggests that the animal-associated isolates share a common resistance gene pool amongst each other to a greater degree than with the human strains. Evaluation of a larger collection of animal S. aureus strains, both MSSA and MRSA would be necessary to further investigate this finding. Moreover, the diversity and high prevalence of tet genes might not be a unique feature of MRSA ST398 but rather a common characteristic of animal-associated MRSA.
In conclusion, to date it is unclear what factors mediate the rapid dissemination of MRSA ST398 among livestock. The failure to identify any significant virulence factors in MRSA ST398 strains might suggest that the lineage harbours novel virulence determinants, particularly those that might enhance colonisation. Although the ST398 resistance gene pool is likely to have played a significant role in the selection of MRSA ST398 as livestock-coloniser, we have demonstrated in this study that similar antimicrobial resistance gene profiles can be detected among other animal-associated MRSA strains such as ST8. Further investigations into MSSA and MRSA isolates from different animal species are necessary to confirm the relative contribution the resistance genes and virulence determinants encoding colonisation factors have played in the spread of successful clones, as well as the relative importance of such factors in comparison with animal husbandry and movement factors.
Materials and Methods
Bacterial Strains
A total of sixty four S. aureus isolates of human and animal origin were investigated (Table 1). Each isolate analysed in this study was selected on the basis of representing a unique fingerprint as determined by pulsed-field gel electrophoresis (Figures S1, S2) following an analysis of a panel of 134 isolates and using a cut-off value of 100% for differentiation of pulsotypes. The PFGE was conducted as described by the Harmony protocol [45]. All ST398 isolates were non-typeable with SmaI and the genomic DNA was successfully digested with Cfr9I.
All isolates belonging to ST398 (n = 18) were isolated in Belgium from various host species: human (pig farmers, n = 2), pig (surveillance, n = 4), cattle (mastitis, n = 3), horse (infection, n = 2) chicken (surveillance, n = 4) and rat (surveillance, n = 3) between 2008 and 2010. The non-ST398 comparator panel consisted of human and animal isolates. Cattle isolates (n = 16) were isolated from cases of clinical mastitis in the UK from April 2006 to September 2007. Equine clinical isolates (n = 2) were isolated in Northern Ireland in 2010. Human isolates (n = 47) were isolated in the UK in the London area from Kingston Hospital, The Royal Brompton Hospital, and from The Royal Marsden Hospital, between 2007 and 2009.
Molecular Typing
Isolates were spa-typed [46], [47] and sequence type was determined by multilocus sequence typing (MLST) for one representative of each spa type identified [48]. Spa type, MLST and clonal complexes were assigned using BioNumerics software (Version 5.10; Applied Maths, Belgium). SCCmec typing was conducted according to the method of Boye et al [49]. When SCCmec type IV was identified the strains were sub-typed using the method developed by Milheirico et al [50] whereas strains harbouring SCCmec type V were sub-typed according to method by Higuchi et al [51].
DNA Microarray Analysis
DNA microarray analysis was performed using Identibac MRSA Array-Tube (AT, STAU-PM5_5, production year: 2008; Identibac, Surrey, UK). Genomic DNA was isolated using Clondiag StaphyType Kit lysis reagents and Qiagen DNeasy kit, following the StaphyType protocol (StaphyType; Alere Technologies GmbH, Germany). Amplification, labelling and array hybridisation of target DNA was performed according to the manufacturer’s instructions (Identibac, Surrey, UK). In short, around 1.5 µg of the DNA was amplified using primers provided by the manufacturer and labelled by incorporation of biotin-16-dUTP (Roche Diagnostics, Germany). The labelled PCR product was hybridised to the probes, after which the AT was washed successively with 2×SSC 0.01% Triton, 2×SSC and 0.2×SSC buffers, followed by treatment with 2% blocking solution and addition of poly-HRP streptavidin (Thermo Fisher Scientific Inc, USA). The AT was washed again and peroxidise substrate was added (Seramun green; Seramun, Germany). The chip images were captured using ATR03 reader (AlereTechnologies GmbH, Germany). Visualisation and analysis of hybridized probes was conducted using IconoClust software package (CLONDGIAG; Germany). The analysis of raw data (probe signal values, Table S1) was performed in accordance with previously published methods [36], [42]. The results were converted into numerical format (2– present, 1– ambiguous, 0– absent) and further analysed using BioNumerics (Version 5.10; Applied Maths, Belgium).
PCR Analysis of Adhesion and Resistance Genes not Present on the Array
Isolates were also screened by PCR for the presence of adhesion and additional resistance genes using previously described primers and thermal cycling conditions (Table S2). The selected adhesion genes tested were: bbp, cna, eno, ebpS, fnbB, fib, clfA, clfB, fnbA, sdrC, sdrD, sdrE, icaA, icaD and sasG. The additional resistance genes tested were: tetL, dfrK, spc, ermT, czrC and mecA LGA251. Gene was considered as present if the PCR product was a single and specific band of the expected length. The PCR results were converted into numerical format (2– present, 0– absent) and analysed using BioNumerics (Version 5.10; Applied Maths, Belgium). The adhesion gene profiles were based on PCR results only whereas the antimicrobial resistance genotypes consisted of collated DNA microarray and PCR data.
Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was performed by the broth microdilution method, using in-house prepared microtitre plates following CLSI recommendations [52]. The following antimicrobials were evaluated: penicillin G, cefoxitin, gentamicin, kanamycin, spectinomycin, apramycin, erythromycin, vancomycin, teicoplanin, clindamycin, ciprofloxacin, tetracycline, chloramphenicol, florfenicol, trimethoprim and tiamulin. Interpretation of MICs was according to the CLSI guidelines. S. aureus ATCC 29123 was used as a control strain.
Supporting Information
UPGMA cluster analysis of PFGE patterns (after SmaI digestion) using Dice similarity coefficient and position tolerance of 1.2%.
(DOC)
UPGMA cluster analysis of PFGE patterns (after Cfr9I digestion) using Dice similarity coefficient and position tolerance of 1.2%.
(DOC)
Raw DNA microarray data showing signal intensity values for all array tube probes.
(XLS)
Primers used in this study.
(DOC)
Acknowledgments
We are grateful to Meenaxi Sharma for technical support. We also thank the Kingston Hospital, the Royal Brompton Hospital and the Royal Marsden Hospital for providing the human isolates, AHVLA regional laboratories for providing the bovine mastitis isolates and the Agri-Food and Biosciences Institute (AFBI) for providing the equine isolates.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported by a PhD project grant SC1004 from the Department for Environment, Food and Rural Affairs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Feil EJ, Cooper JE, Grundmann H, Robinson DA, Enright MC, et al. How clonal is Staphylococcus aureus? J Bacteriol. 2003;185(11):3307–3316. doi: 10.1128/JB.185.11.3307-3316.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herron-Olson L, Fitzgerald JR, Musser JM, Kapur V. Molecular correlates of host specialization in Staphylococcus aureus. PLoS One. 2007;2(10):e1120. doi: 10.1371/journal.pone.0001120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guinane CM, Ben Zakour NL, Tormo-Mas MA, Weinert LA, Lowder BV, et al. Evolutionary genomics of Staphylococcus aureus reveals insights into the origin and molecular basis of ruminant host adaptation. Genome Biol Evol. 2010;2:454–466. doi: 10.1093/gbe/evq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lowder BV, Guinane CM, Ben Zakour NL, Weinert LA, Conway-Morris A, et al. Recent human-to-poultry host jump, adaptation, and pandemic spread of Staphylococcus aureus. Proc Natl Acad Sci U S A. 2009;106(46):19545–19550. doi: 10.1073/pnas.0909285106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walther B, Monecke S, Ruscher C, Friedrich AW, Ehricht R, et al. Comparative molecular analysis substantiates zoonotic potential of equine methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2009;47(3):704–710. doi: 10.1128/JCM.01626-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Neeling AJ, van den Broek MJ, Spalburg EC, van Santen-Verheuvel MG, Dam-Deisz WD, et al. High prevalence of methicillin resistant Staphylococcus aureus in pigs. Vet Microbiol. 2007;122(3–4):366–372. doi: 10.1016/j.vetmic.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 7.Khanna T, Friendship R, Dewey C, Weese JS. Methicillin-resistant Staphylococcus aureus colonization in pigs and pig farmers. Vet Microbiol. 2008;128(3–4):298–303. doi: 10.1016/j.vetmic.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Harlizius J, Kock R, Lambrecht C, Schulze-Horset T, Hendrix MGR, et al. Prevalence of MRSA in pig-production units in North-Rhine Westphalia, Germany. 2008.
- 9.Smith TC, Male MJ, Harper AL, Kroeger JS, Tinkler GP, et al. Methicillin-resistant Staphylococcus aureus (MRSA) strain ST398 is present in Midwestern U.S. swine and swine workers. PLoS One. 2009;4(1):e4258. doi: 10.1371/journal.pone.0004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van den Eede A, Martens A, Lipinska U, Struelens M, Deplano A, et al. High occurrence of methicillin-resistant Staphylococcus aureus ST398 in equine nasal samples. Vet Microbiol. 2009;133(1–2):138–144. doi: 10.1016/j.vetmic.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 11.Persoons D, Van Hoorebeke S, Hermans K, Butaye P, de Kruif A, et al. Methicillin-resistant Staphylococcus aureus in poultry. Emerg Infect Dis. 2009;15(3):452–453. doi: 10.3201/eid1503.080696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fessler A, Scott C, Kadlec K, Ehricht R, Monecke S, et al. Characterization of methicillin-resistant Staphylococcus aureus ST398 from cases of bovine mastitis. J Antimicrob Chemother. 2010;65(4):619–625. doi: 10.1093/jac/dkq021. [DOI] [PubMed] [Google Scholar]
- 13.Huijsdens XW, van Dijke BJ, Spalburg E, van Santen-Verheuvel MG, Heck ME, et al. Community-acquired MRSA and pig-farming. Ann Clin Microbiol Antimicrob. 2006;5:26. doi: 10.1186/1476-0711-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis HC, Molbak K, Reese C, Aarestrup FM, Selchau M, et al. Pigs as source of methicillin-resistant Staphylococcus aureus CC398 infections in humans, Denmark. Emerg Infect Dis. 2008;14(9):1383–1389. doi: 10.3201/eid1409.071576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fanoy E, Helmhout LC, van der Vaart WL, Weijdema K, van Santen-Verheuvel MG, et al. An outbreak of non-typeable MRSA within a residential care facility. Euro Surveill. 2009;14(1):19080. [PubMed] [Google Scholar]
- 16.van Duijkeren E, Ikawaty R, Broekhuizen-Stins MJ, Jansen MD, Spalburg EC, et al. Transmission of methicillin-resistant Staphylococcus aureus strains between different kinds of pig farms. Vet Microbiol. 2008;126(4):383–389. doi: 10.1016/j.vetmic.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Fitzgerald JR, Sturdevant DE, Mackie SM, Gill SR, Musser JM. Evolutionary genomics of Staphylococcus aureus: Insights into the origin of methicillin-resistant strains and the toxic shock syndrome epidemic. Proc Natl Acad Sci U S A. 2001;98(15):8821–8826. doi: 10.1073/pnas.161098098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larsen AR, Skov RL, Jarlier V, Henriksen AS. Epidemiological differences between the UK and Ireland versus France in Staphylococcus aureus isolates resistant to fusidic acid from community-acquired skin and soft tissue infections. J Antimicrob Chemother. 2008;61(3):589–594. doi: 10.1093/jac/dkm532. [DOI] [PubMed] [Google Scholar]
- 19.Nulens E, Stobberingh EE, van Dessel H, Sebastian S, van Tiel FH, et al. Molecular characterization of Staphylococcus aureus bloodstream isolates collected in a dutch university hospital between 1999 and 2006. J Clin Microbiol. 2008;46(7):2438–2441. doi: 10.1128/JCM.00808-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donker GA, Deurenberg RH, Driessen C, Sebastian S, Nys S, et al. The population structure of Staphylococcus aureus among general practice patients from the Netherlands. Clin Microbiol Infect. 2009;15(2):137–143. doi: 10.1111/j.1469-0691.2008.02662.x. [DOI] [PubMed] [Google Scholar]
- 21.Argudin MA, Mendoza MC, Mendez FJ, Martin MC, Guerra B, et al. Clonal complexes and diversity of exotoxin gene profiles in methicillin-resistant and methicillin-susceptible Staphylococcus aureus isolates from patients in a Spanish hospital. J Clin Microbiol. 2009;47(7):2097–2105. doi: 10.1128/JCM.01486-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson AP, Aucken HM, Cavendish S, Ganner M, Wale MC, et al. Dominance of EMRSA-15 and -16 among MRSA causing nosocomial bacteraemia in the UK: Analysis of isolates from the European antimicrobial resistance surveillance system (EARSS). J Antimicrob Chemother. 2001;48(1):143–144. doi: 10.1093/jac/48.1.143. [DOI] [PubMed] [Google Scholar]
- 23.Smith EM, Green LE, Medley GF, Bird HE, Fox LK, et al. Multilocus sequence typing of intercontinental bovine Staphylococcus aureus isolates. J Clin Microbiol. 2005;43(9):4737–4743. doi: 10.1128/JCM.43.9.4737-4743.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jorgensen HJ, Mork T, Caugant DA, Kearns A, Rorvik LM. Genetic variation among Staphylococcus aureus strains from Norwegian bulk milk. Appl Environ Microbiol. 2005;71(12):8352–8361. doi: 10.1128/AEM.71.12.8352-8361.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rabello RF, Moreira BM, Lopes RM, Teixeira LM, Riley LW, et al. Multilocus sequence typing of Staphylococcus aureus isolates recovered from cows with mastitis in Brazilian dairy herds. J Med Microbiol 56(Pt. 2007;11):1505–1511. doi: 10.1099/jmm.0.47357-0. [DOI] [PubMed] [Google Scholar]
- 26.Ikawaty R, Brouwer EC, Jansen MD, van Duijkeren E, Mevius D, et al. Characterization of Dutch Staphylococcus aureus from bovine mastitis using a multiple locus variable number tandem repeat analysis. Vet Microbiol. 2009;136(3–4):277–284. doi: 10.1016/j.vetmic.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 27.Hasman H, Moodley A, Guardabassi L, Stegger M, Skov RL, et al. Spa type distribution in Staphylococcus aureus originating from pigs, cattle and poultry. Vet Microbiol. 2010;141(3–4):326–331. doi: 10.1016/j.vetmic.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 28.Hata E, Katsuda K, Kobayashi H, Uchida I, Tanaka K, et al. Genetic variation among Staphylococcus aureus strains from bovine milk and their relevance to methicillin-resistant isolates from humans. J Clin Microbiol. 2010;48(6):2130–2139. doi: 10.1128/JCM.01940-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, et al. The molecular evolution of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect. 2007;13(3):222–235. doi: 10.1111/j.1469-0691.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 30.Kadlec K, Ehricht R, Monecke S, Steinacker U, Kaspar H, et al. Diversity of antimicrobial resistance pheno- and genotypes of methicillin-resistant Staphylococcus aureus ST398 from diseased swine. J Antimicrob Chemother. 2009;64(6):1156–1164. doi: 10.1093/jac/dkp350. [DOI] [PubMed] [Google Scholar]
- 31.Schijffelen MJ, Boel CH, van Strijp JA, Fluit AC. Whole genome analysis of a livestock-associated methicillin-resistant Staphylococcus aureus ST398 isolate from a case of human endocarditis. BMC Genomics. 2010;11:376. doi: 10.1186/1471-2164-11-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coleman DC, Arbuthnott JP, Pomeroy HM, Birkbeck TH. Cloning and expression in Escherichia coli and Staphylococcus aureus of the beta-lysin determinant from Staphylococcus aureus: Evidence that bacteriophage conversion of beta-lysin activity is caused by insertional inactivation of the beta-lysin determinant. Microb Pathog. 1986;1(6):549–564. doi: 10.1016/0882-4010(86)90040-9. [DOI] [PubMed] [Google Scholar]
- 33.Coleman DC, Sullivan DJ, Russell RJ, Arbuthnott JP, Carey BF, et al. Staphylococcus aureus bacteriophages mediating the simultaneous lysogenic conversion of beta-lysin, staphylokinase and enterotoxin A: Molecular mechanism of triple conversion. J Gen Microbiol. 1989;135(6):1679–1697. doi: 10.1099/00221287-135-6-1679. [DOI] [PubMed] [Google Scholar]
- 34.Carroll JD, Cafferkey MT, Coleman DC. Serotype F double- and triple-converting phage insertionally inactivate the Staphylococcus aureus beta-toxin determinant by a common molecular mechanism. FEMS Microbiol Lett. 1993;106(2):147–155. doi: 10.1111/j.1574-6968.1993.tb05951.x. [DOI] [PubMed] [Google Scholar]
- 35.van Wamel WJ, Rooijakkers SH, Ruyken M, van Kessel KP, van Strijp JA. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J Bacteriol. 2006;188(4):1310–1315. doi: 10.1128/JB.188.4.1310-1315.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Monecke S, Kuhnert P, Hotzel H, Slickers P, Ehricht R. Microarray based study on virulence-associated genes and resistance determinants of Staphylococcus aureus isolates from cattle. Vet Microbiol. 2007;125(1–2):128–140. doi: 10.1016/j.vetmic.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 37.Delgado S, Garcia P, Fernandez L, Jimenez E, Rodriguez-Banos M, et al. Characterization of Staphylococcus aureus strains involved in human and bovine mastitis. FEMS Immunol Med Microbiol. 2011;62(2):225–235. doi: 10.1111/j.1574-695X.2011.00806.x. [DOI] [PubMed] [Google Scholar]
- 38.O’Neill E, Humphreys H, O’Gara JP. Carriage of both the fnbA and fnbB genes and growth at 37 degrees C promote FnBP-mediated biofilm development in meticillin-resistant Staphylococcus aureus clinical isolates. J Med Microbiol 58(Pt. 2009;4):399–402. doi: 10.1099/jmm.0.005504-0. [DOI] [PubMed] [Google Scholar]
- 39.Shinji H, Yosizawa Y, Tajima A, Iwase T, Sugimoto S, et al. Role of fibronectin-binding proteins A and B in in vitro cellular infections and in vivo septic infections by Staphylococcus aureus. Infect Immun. 2011;79(6):2215–2223. doi: 10.1128/IAI.00133-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Otsuka T, Saito K, Dohmae S, Takano T, Higuchi W, et al. Key adhesin gene in community-acquired methicillin-resistant Staphylococcus aureus. Biochem Biophys Res Commun. 2006;346(4):1234–1244. doi: 10.1016/j.bbrc.2006.06.038. [DOI] [PubMed] [Google Scholar]
- 41.Nashev D, Toshkova K, Salasia SI, Hassan AA, Lammler C, et al. Distribution of virulence genes of Staphylococcus aureus isolated from stable nasal carriers. FEMS Microbiol Lett. 2004;233(1):45–52. doi: 10.1016/j.femsle.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 42.Monecke S, Slickers P, Ehricht R. Assignment of Staphylococcus aureus isolates to clonal complexes based on microarray analysis and pattern recognition. FEMS Immunol Med Microbiol. 2008;53(2):237–251. doi: 10.1111/j.1574-695X.2008.00426.x. [DOI] [PubMed] [Google Scholar]
- 43.van Belkum A, Melles DC, Snijders SV, van Leeuwen WB, Wertheim HF, et al. Clonal distribution and differential occurrence of the enterotoxin gene cluster, egc, in carriage- versus bacteremia-associated isolates of Staphylococcus aureus. J Clin Microbiol. 2006;44(4):1555–1557. doi: 10.1128/JCM.44.4.1555-1557.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams RJ, Ward JM, Henderson B, Poole S, O’Hara BP, et al. Identification of a novel gene cluster encoding staphylococcal exotoxin-like proteins: Characterization of the prototypic gene and its protein product, SET1. Infect Immun. 2000;68(8):4407–4415. doi: 10.1128/iai.68.8.4407-4415.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murchan S, Kaufmann ME, Deplano A, de Ryck R, Struelens M, et al. Harmonization of pulsed-field gel electrophoresis protocols for epidemiological typing of strains of methicillin-resistant Staphylococcus aureus: A single approach developed by consensus in 10 European laboratories and its application for tracing the spread of related strains. J Clin Microbiol. 2003;41(4):1574–1585. doi: 10.1128/JCM.41.4.1574-1585.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. www.ridom.de.
- 47.Shopsin B, Gomez M, Montgomery SO, Smith DH, Waddington M, et al. Evaluation of protein A gene polymorphic region DNA sequencing for typing of Staphylococcus aureus strains. J Clin Microbiol. 1999;37(11):3556–3563. doi: 10.1128/jcm.37.11.3556-3563.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000;38(3):1008–1015. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boye K, Bartels MD, Andersen IS, Moller JA, Westh H. A new multiplex PCR for easy screening of methicillin-resistant Staphylococcus aureus SCCmec types I-V. Clin Microbiol Infect. 2007;13(7):725–727. doi: 10.1111/j.1469-0691.2007.01720.x. [DOI] [PubMed] [Google Scholar]
- 50.Milheirico C, Oliveira DC, de Lencastre H. Multiplex PCR strategy for subtyping the staphylococcal cassette chromosome mec type IV in methicillin-resistant Staphylococcus aureus: ‘SCCmec IV multiplex’. J Antimicrob Chemother. 2007;60(1):42–48. doi: 10.1093/jac/dkm112. [DOI] [PubMed] [Google Scholar]
- 51.Higuchi W, Takano T, Teng LJ, Yamamoto T. Structure and specific detection of staphylococcal cassette chromosome mec type VII. Biochem Biophys Res Commun. 2008;377(3):752–756. doi: 10.1016/j.bbrc.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 52.Clinical and Laboratory Standards Institute, editor. (January 2006) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; Approved standard - seventh edition.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
UPGMA cluster analysis of PFGE patterns (after SmaI digestion) using Dice similarity coefficient and position tolerance of 1.2%.
(DOC)
UPGMA cluster analysis of PFGE patterns (after Cfr9I digestion) using Dice similarity coefficient and position tolerance of 1.2%.
(DOC)
Raw DNA microarray data showing signal intensity values for all array tube probes.
(XLS)
Primers used in this study.
(DOC)