With an estimated two million new cases of tuberculosis (TB) annually diagnosed within its borders, even the notion of a “TB-free India” — the stated vision of the nation’s decades-old Revised National Tuberculosis Control Program — seems as remote as the Himalayas.
But government officials are hoping they’re on the right track to reducing that incidence, which represents 21% of the global tuberculosis burden, by imposing a requirement that all “clinical establishments run or managed by the Government (including local authorities), private or NGO [nongovernmental organizations] sectors and/or individual practitioners” report monthly on the cases they’ve diagnosed (www.tbcindia.nic.in/pdfs/TB%20Notification%20Govt%20%20Order%20dated%2007%2005%202012.pdf).
The mandatory reporting requirement does not appear to come with a carrot or stick, as the government made no mention of doctors either receiving a reward for filing a monthly report, or a punishment for failing to do so.
But at a minimum, it’s hoped it will help officials get a more accurate gauge of the true scope of India’s tuberculosis problem and reduce the mortality rate, which the World Health Organization projected to be 26 per 100 000 in 2010 (https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=IN&outtype=pdf), or about two deaths every three minutes, according to TBC India (www.tbcindia.nic.in/).
“Even in 1905, Dr. Robert Koch in his Nobel Lecture mentioned that there are two essential steps for controlling tuberculosis. Firstly, training of doctors for TB diagnosis and secondly, the need for doctors to inform a central authority (obligation to report) when diagnosis has been achieved. This order will help achieve both,” says Dr. Nevin Wilson, regional director of the South East Asia Office of the International Union Against Tuberculosis and Lung Disease.
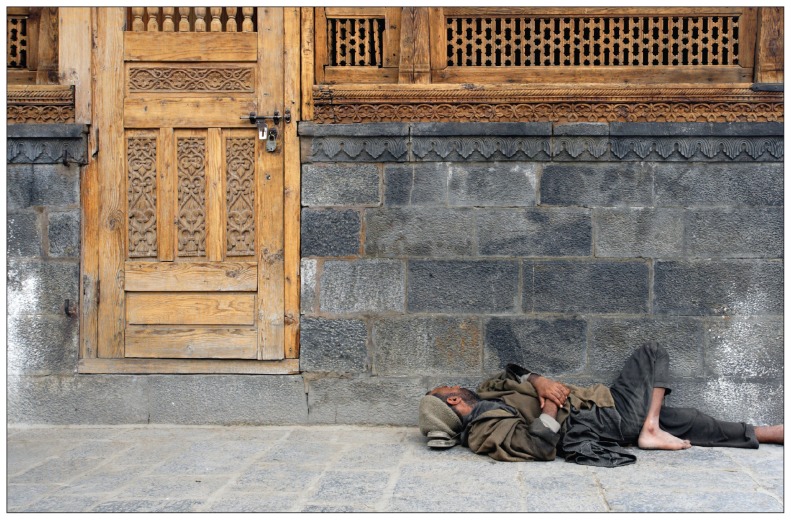
Tuberculosis is considered to be one of the principal diseases of poverty and the homeless are among those at high risk.
Image courtesy of © 2012 Thinkstock
The Indian Medical Association also endorsed the move. “It is a step in the right direction since every doctor should report TB,” says Dr. D.R. Rai, honorary secretary general of the association. “This will also help in more accurate estimation of the disease trends in the country. Thus, in the long run, proper allocation of resources and identification of priorities will be possible. The government has made provisions for extra funds for TB and this will help in tackling the extra number of cases that will be reported due to mandatory notification.”
The 2011 annual report of the Revised National Tuberculosis Control Program asserts that India has been achieving a 70% case detection rate and an 83% cure rate in new smear positive patients since 2007 (http://tbcindia.nic.in/pdfs/RNTCP%20TB%20India%202011.pdf).
The largest block of undetected and unreported cases are believed to fall within the rubric of the nation’s huge private health care sector. Multiple studies have raised concerns about the knowledge level of private practitioners in prescribing proper and uniform drug regimens to tuberculosis patients.
Mandatory reporting should help redress that problem, says Dr. G.K. Ramachandrappa, president of the Indian Medical Association. “Multi-drug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) have added to the potential challenges in the effective control of tuberculosis. With notification we go to the patient, instead of the patient coming to us and thus decreasing default or lost in follow-up cases,” Ramachandrappa says, adding that there should be a consequent decrease in the incidence of MDR-TB.
The government also hopes that more informed treatment will help to prevent cases of totally drug-resistant tuberculosis (which the WHO has not acknowledged as a separate form of TB), such as the four that surfaced in Mumbai in December 2011, three of which, the government said, were the consequence of “erratic, unsupervised second-line drugs, added individually and often in incorrect doses, from multiple private practitioners (on average from 4 physicians during an 18-month period) in an attempt to cure” MDR-TB (http://tbcindia.nic.in/pdfs/RNTCP%20Response%20DR%20TB%20in%20India%20-%20Jan%202012%20update.pdf).
Wilson is hopeful most doctors will comply with the notification order as it’s consistent with the Indian Medical Council’s code of professional conduct and India has a history of compliance, having “achieved good results for polio and other vector-borne diseases.”
But others have raised concerns that notification is a breach of patient confidentiality.
Confidentiality is “culture sensitive,” notes Dr. Supten Sarbadhikari, a member of the Ministry of Health and Family Welfare’s expert committee on electronic medical records standards. “It is very different in the Indian subcontinent from that in the West. Breach of confidentiality in cases where the disease is associated with stigma can be serious.”