Abstract
Background:
A new protocol for human papillomavirus (HPV) testing within the UK cervical screening programme commenced in April 2011, creating new patient experiences. This is the first review to synthesise a substantial body of international evidence of women’s information needs, views and preferences regarding HPV testing. We aimed to inform the development of educational materials to promote informed choice, reduce anxiety and improve disease control.
Methods:
We searched 12 bibliographic databases. Two reviewers independently screened papers and assessed study quality; disagreements were resolved by discussion. Results were extracted verbatim and authors’ findings treated as primary data. Studies were synthesised collaboratively using framework methods.
Results:
We synthesised findings from 17 studies. Women had overwhelmingly negative concerns; an HPV diagnosis was daunting, had associated problems of disclosure of a sexually transmitted infection (STI), impacted on relationships and provoked fear of stigmatisation. Nevertheless, many thought HPV testing could be a preferable alternative to repeat cytology. Knowledge was poor; women struggled to interpret limited information in the context of existing knowledge about STIs and cervical cancer.
Conclusion:
Women are likely to be poorly informed, have limited understanding and many unanswered questions. This could increase anxiety and reduce ability to make informed choices, presenting a substantial challenge for those who design and provide information.
Keywords: human papillomavirus, cervical screening, cervical cancer, systematic review
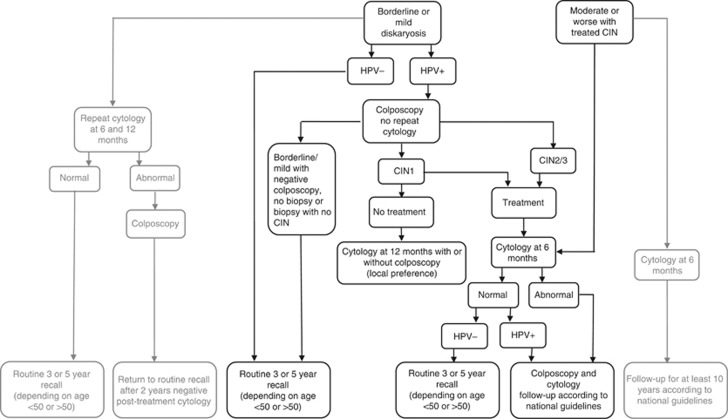
High-risk human papillomavirus (HPV) types 16 and 18 account for 70% of cervical cancers. England’s NHS Cervical Screening Programme was the first in the United Kingdom to launch a new protocol of HPV triage in April 2011 (Department of Health, 2011). Women with borderline or mild dyskaryosis will be routinely tested for HPV, and triaged according to the results (Figure 1; NHS Cancer Screening Programmes, 2010). High-risk human papillomavirus test-positive women will be fast-tracked to colposcopy, replacing usual practice of cytological surveillance at six monthly intervals. HPV test-negative women, deemed low risk for cervical cancer, will return to routine age-sensitive screening rather than cytological surveillance (Figure 1; NHS Cancer Screening Programmes, 2010; NHSCSP, 2010). These new clinical pathways generate new patient experiences. Acceptability to women is likely to be closely related to knowledge and understanding; poor understanding of test results is associated with anxiety (Maissi et al, 2004).
Figure 1.
Cervical screening protocols before and after the introduction of HPV testing.
Both the natural history of HPV and this new protocol are complex. To achieve good uptake in cervical cancer prevention while adequately informing women, HPV information should be evidence-based, sensitive to UK culture and practice, with accurate risk/benefit portrayal and estimation of uncertainty and consequences (Barratt et al, 2004; Bekker, 2010). This systematic review aimed to synthesise qualitative and quantitative evidence of people’s information needs, views and preferences regarding HPV testing, to inform the development of HPV educational materials to promote the key outcomes of informed choice, minimal anxiety and adequate uptake needed for disease control.
Materials and Methods
The review was conducted using methodology reported in the NHS Centre for Reviews and Dissemination report 4 (NHS Centre for Reviews and Dissemination, 2001), supplemented by Harden’s recommendations for systematic reviews of qualitative studies (Harden et al, 2004). We also adhered to guidance on methods for conducting and reporting systematic reviews in the PRISMA statement, where it could be applied to reviews of qualitative studies (Moher et al, 2009).
We searched 12 electronic databases using thesaurus terms and keywords relating to HPV and vaccination or testing (Appendix 1). Bibliographies of included studies were hand-searched. Searches were conducted in June 2009, updated in July 2010, and limited to 1980 onwards, when relevant papers began to appear. Two (of three) reviewers (MH, RL and DP) independently screened titles and abstracts for relevance, assessed relevant papers against inclusion criteria and considered study quality. Disagreements were resolved by discussion. Inclusion and exclusion criteria are detailed in Table 1.
Table 1. Inclusion and exclusion criteria for studies of HPV testing.
| Inclusion | Exclusion | |
|---|---|---|
| Population | Any participants who are asked about HPV testing in the context of either hypothetical scenarios or personal experience of testing | |
| Intervention | HPV testing in the context of cervical screening | Studies about HPV infection, or cervical screening, not HPV testing Studies about the testing process, for example, self-sampling versus conventional methods |
| Outcomes | People’s views on HPV testing, such as their understanding, attitude, perception, acceptability, concerns and information needs | Studies that assess participants’ knowledge and/or behaviour, not their views |
| Study design | Any study design used to elicit qualitative or quantitative data relating to participants’ views about HPV testing | |
| Reporting | Studies must be reported in sufficient detail for meaningful data extraction | Studies with insufficient detail, for example, available only as abstracts |
Abbreviation: HPV=human papillomavirus.
Qualitative studies were appraised using a quality checklist (National Institute for Health and Clinical Excellence, 2009). We excluded quotations from the original data and treated authors’ findings as primary data. Synthesists differ on what counts as data from primary studies (Major and Savin-Baden, 2010). We considered authors’ findings to be syntheses of entire primary data-sets, whereas quotations were illustrative examples of specific points. Studies were synthesised collaboratively by two reviewers (MH and DP) using the framework approach (Ritchie and Spencer, 1994). Data were repeatedly read to achieve familiarity, themes were identified and organised into categories, reviewed and refined until both reviewers agreed on the validity of the thematic framework. Data were then coded, the framework applied and again reviewed and refined until consensus was reached (Swallow et al, 2003).
Surveys were assessed using a quality checklist adapted from Pettigrew and Roberts (2006), and summarised using narrative synthesis methods (Popay et al, 2006).
Results
Summary of included studies
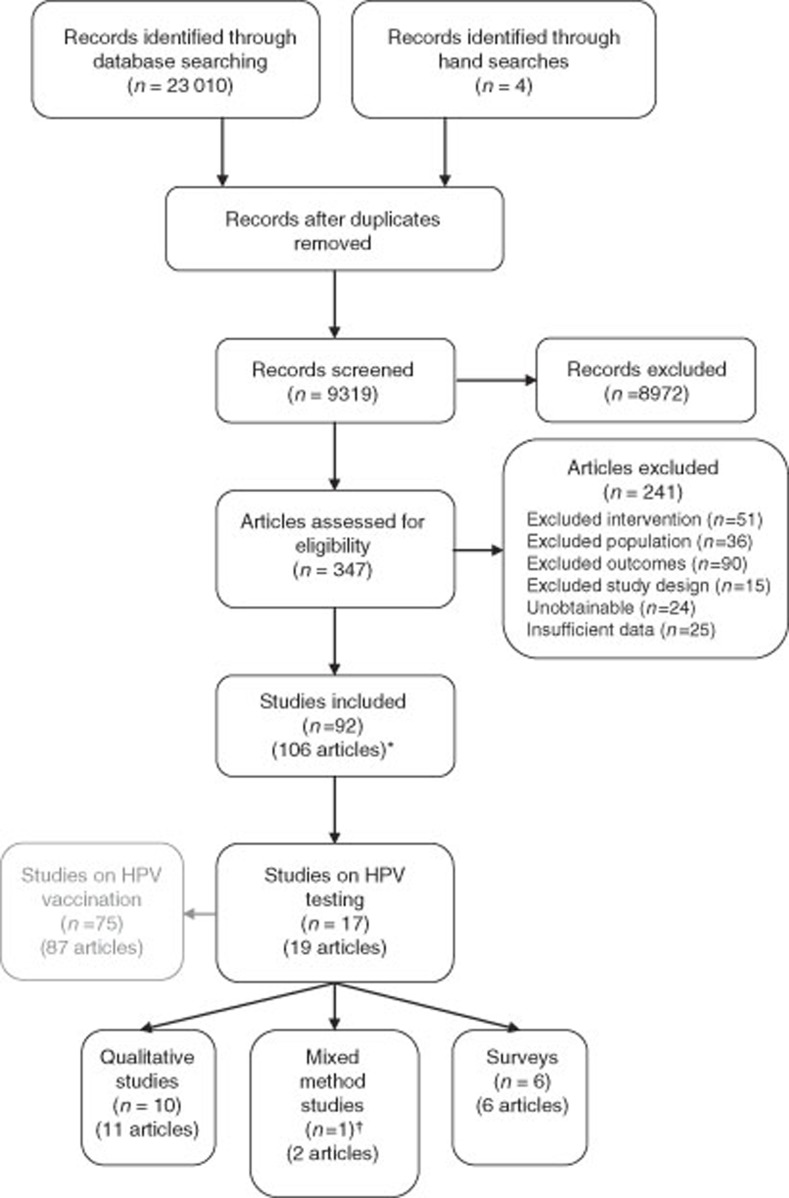
Sixteen surveys or qualitative studies and one mixed method (qualitative and quantitative) study (data from this study are reported with qualitative and quantitative results, therefore it may appear to be counted twice) met our inclusion criteria (Figure 2). Publication dates ranged between 1997 and 2010; most recent data collection reported in May 2007; thus most studies reflect findings that predate HPV vaccination and associated public information.
Figure 2.
PRISMA flowchart. *Some studies were reported in more than one publication. †Data from this study are reported with qualitative and quantitative results as appropriate.
Qualitative studies
Eleven qualitative studies were included (Table 2). Studies reporting results in more than one publication (Kahn et al, 2007; Daley et al, 2010) were consolidated. Included studies were from United States, United Kingdom, Australia and Canada and all used either focus groups or face-to-face interviews. Methods of analysis were grounded theory, thematic analysis or framework. Most recruited adult women; the majority of participants reflected UK cervical screening age. Study details are fully described in Table 2.
Table 2. Included qualitative studies.
| Study, Location | Data collection method and date | Participant details a | Analysis | Type of data collected or relevant questions asked |
|---|---|---|---|---|
| Anhang, 2004 Massachusetts, USA | Focus groups based on brief description of HPV August/September 2002 | 48 women aged 18–55+ (years) from low-income and minority populations; 44% Hispanic, 40% white; 73% educated to high school level or less | Grounded theory | Topics included current level of HPV knowledge, what information they would like to receive, how they imagined it would feel to receive a positive HPV test result, and whether they would like to be tested |
| Brown, 2007 Ontario, Canada | Face-to-face interviews based on HPV information and case scenario Date not reported | 20 women aged 25–83– a random sample of adult females in Ontario 65% Had college or university education | Thematic analysis | Women were asked views on four different treatment options for a case scenario of abnormal cytology: colposcopy; repeat Pap test; HPV test; discuss with primary care physician |
| Daley, 2010 Urban and rural South East, USA | Face-to-face interviews based on experience of HPV testing October 2001–September 2005 | 52 women recruited in gynaecological clinics, aged 18–44 years, who had abnormal cytology and were HPV positive 75% White, 11% Hispanic | Thematic analysis | Topic guide included knowledge of HPV, emotional responses to diagnosis, disclosure of test results and changes in health behaviour |
| Fernandez, 2009 Brownsville, TX, USA | Focus groups based on case scenario 2005 | 41 Hispanic adults aged 19–76 years (30 female) recruited in a poor area with high rates of cervical cancer | Thematic analysis | Topic guide included HPV awareness, knowledge and attitudes Reactions to learning about an HPV diagnosis were based on scenarios of a woman hearing her Pap test result, HPV+ status and disclosing her status to her partner |
| Kahn, 2007 Cincinnati, OH, USA | Baseline questionnaire followed by face-to-face interview 2 weeks later on receipt of test results July 2002/January 2003 | Sexually active females aged 14–21, recruited in an urban teen health centre 51% HPV positive, 23% abnormal cytology 82% non-Hispanic Black | Framework | Two topic guides used: one emphasised personal meaning of test results (perception of risk, personal liability etc), a second was modified to focus on cognitive understanding of test results and personal experience of STIs and cancer |
| Marlow, 2009 London, UK | Face-to-face interviews based on brief information about HPV Date not reported | 21 women aged 18–53 years recruited in a University setting by ‘snowballing’. 95% White British 76% had university education. | Framework | Women were asked what information they would need to be sufficiently informed to make a decision about HPV testing |
| McCaffery, 2003 Greater Manchester, UK | Eight focus groups based on brief information about HPV and HPV testing July/September 2000 | 71 women aged 20–59 years; 28% Pakistani, 27% Indian, 22% African-Caribbean, 22% White British; 35% had some tertiary education; 76% of these were Indian or Pakistani | Framework | Topic guide focused on reactions to HPV as an STI linked to cervical cancer; anticipated reactions to testing positive for HPV; partner, family and community attitudes to HPV testing, and religious and cultural influences |
| McCaffery, 2005 Sydney & surrounds, Australia | Face-to-face interviews based on experience of testing June/December 2002 | 20 women of screening age who were HPV positive and had abnormal cytology. 68% Anglo-Australian. 47% Had tertiary education. | Framework | Topic guide covered issues relating to the diagnosis of HPV and cervical screening, women’s psychological response to their HPV infection, their understanding of HPV and their information needs and preferences |
| McCaffery, 2006 Manchester & London, UK | Face-to-face interviews based on experience of testing June 2001/December 2003 | 74 women aged 20–64 years recruited in clinical trials of HPV testing or colposcopy clinics 54% Abnormal cytology, 77% HPV positive 55% White, 23% South Asian, 22% African-Caribbean. 61% had tertiary education | Framework | Topic guide included screening history, understanding of HPV test, experience of smear test results and HPV diagnosis, understanding and disclosure of results, emotional impact, and experience of treatment or follow-up |
| Vanslyke, 2009 Albuquerque, NM, USA | Focus groups based on brief information about HPV and HPV testing ‘before vaccine publically available’ | 54 low-income Hispanic women aged 18–60 years recruited in community locations; 43% had only primary education; 63% had household income <$20 000 | Thematic analysis | Topic guide included questions about cervical cancer and HPV, how participants would feel about being tested for HPV, and which of the three HPV prevention options they preferred and why: (1) fewer sexual partners; (2) condoms; and (3) vaccines |
| Waller, 2007b Manchester, UK | Face-to-face interviews following a second (12 month follow-up) HPV test Date not reported | 30 women aged 20–50+ (years), HPV positive with normal cytology at baseline; some HPV positive and some negative at 12 month follow-up; 47% had tertiary education | Framework | Topic guide focused on emotional responses to the tests, differences between the impact of the two tests, disclosure of results, decisions about follow-up and feeling about future screening |
Abbreviations: HPV=human papillomavirus; STI=sexually transmitted infection.
Age range, ethnicity, educational level and indicators of socio-economic status are given where data are available.
In five studies smear and HPV tests were conducted and results were known at the time of interview (McCaffery and Irwig, 2005; McCaffery et al, 2006; Kahn et al, 2007; Waller et al, 2007b; Daley et al, 2010). In two of these, participants had mixed results: HPV positive and negative; cytology normal and abnormal (McCaffery et al, 2006; Kahn et al, 2007). In two studies all were HPV positive and had abnormal cytology (McCaffery and Irwig, 2005; Daley et al, 2010). In one, all were HPV positive but had normal cytology (Waller et al, 2007b), in this study participants were retested after 12 months and, if still HPV positive, offered the choice of retest after a further 12 months or immediate colposcopy. Six studies gave untested women information about HPV then sought views about HPV testing (McCaffery et al, 2003; Anhang et al, 2004; Brown et al, 2007; Vanslyke et al, 2008; Fernandez et al, 2009; Marlow et al, 2009).
Surveys
Seven surveys, from the United States, Australia and Canada, met our inclusion criteria (Table 3). Sample sizes ranged from 50 to 968. Four studies included participants with abnormal cytology. In one of these, participants were HPV positive (Daley et al, 2010), in three their HPV status was unknown (Le et al, 2004; McCaffery et al, 2008; Patel et al, 2008). In the remaining three studies, convenience samples of women were surveyed and selection criteria, if any, related to age, gender or ethnicity (Ferris et al, 1997; Huang et al, 2008; Papa et al, 2009).
Table 3. Included surveys.
| Study, location | Setting | Data collection method, date and response rate | Participant details a | Summary of relevant questions | Summary of results | |||
|---|---|---|---|---|---|---|---|---|
| Daley, 2010 South East, USA | Routine annual gynaecological examinations in local clinics | Paper and pencil questionnaire administered in clinic October 2001/September 2005 RR 31% | 154 women aged >18 years with abnormal cytology and HPV+69% White, 16% Hispanic | HPV knowledge, disclosure of HPV test results, emotional impact of HPV diagnosis | Only 39% correctly understood their own HPV diagnosis. 93% had disclosed their HPV status, 39% to a partner; 66% would disclose it to a future partner. 82% sought information from the internet, 70% from other sources. Negative responses included stigma (71%), anxiety (94%), stress (95%), anger (70%), confusion (71%), shock (70%) and self-blame (68%) but 95% agreed it could be worse. 26% thought HPV test results could change their future pregnancy plans |
|||
| Ferris, 1997 Augusta, GA, USA | Waiting rooms in one civilian and one military family practice clinic and one obs and gynae clinic | Questionnaire self-completed in clinic Date not reported RR 99% | 968 women aged >16 years; 55% black; 29% family income <$25K, 10% >$50K; 11% did not complete high school; 19% had tertiary education | Management preferences for case scenarios of ASCUS or LSIL based on test accuracy, potential discomfort and cost | Case scenario | Management preference |
||
| Repeat smear test (%) | Cervicography or colposcopy (%) | HPV DNA test (%) | ||||||
| ASCUS | 68 | 35 | 7 | |||||
| LSIL | 14 | 78 | 8 | |||||
| Test accuracy was the primary reason for women’s choice. | ||||||||
| Huang, 2008 San Francisco, USA | University based and community based primary care practices and community health clinics | Telephone and face-to-face interviews October 2002/January 2006 RR 85% | 865 women aged 50–80 years; 43% Asian, 30% White, 17% Latina; 39% did not complete high school; 31% income <$15 000 | Awareness of HPV and previous HPV testing; desire for HPV test; desired frequency of smear tests if HPV test was positive | 30% had heard of HPV and 7% had had an HPV test; 64% wanted to be tested for HPV. However, 78% would want frequent smear tests (>1 annually) if tested positive. 55% of women aged <65 years thought three yearly smear tests acceptable if HPV negative with normal cytology and 33% of women aged ⩾65 years would stop getting smear tests if HPV negative (+19% if physician recommended) | |||
| Le, 2004 Ottawa, Canada | University colposcopy clinic | Face-to-face interviews Date not reported RR 75% | 100 women aged 18–75 years, 42% with minor abnormal cytology; 66% office workers with tertiary education; 20% manual workers | Knowledge of the role of HPV in CIN and the rationale behind HPV testing; preferences between six monthly colposcopy (standard practice) or HPV test and annual colposcopy if HPV negative | 75% had little or no knowledge about the role of HPV in CIN; 84% had never heard of the HPV test, or had minimal knowledge. After explanation, 64% chose an HPV test with less frequent colposcopy follow-up if negative rather than six monthly colposopic surveillance until two consecutive clear results were obtained | |||
| McCaffery, 2008 Throughout Australia | Cervical screening in urban and rural family planning clinics across Australia | Postal questionnaires Date not reported RR 89% | 106 women aged 16–70 years with minor abnormal cytology; 42% university graduates | After using a decision aid, women chose their preferred management for mildly abnormal cytology: (1) HPV test; (2) usual care (a repeat smear test) | Of the 94 women who made a management choice 65% chose to have HPV testing. Having children, having a previous abnormal smear and having higher distress scores were significantly associated with choosing HPV triage | |||
| Papa, 2009 MA, USA | Routine annual examinations in one university hospital based obs and gynae clinic | Questionnaire self-completed in clinic January–March 2007 RR not reported | 50 women aged 30–69 years, 50% with history of abnormal cytology; 14% HPV; 88% white; 72% had tertiary education | Questions asked pre- and post-educational intervention: knowledge of HPV, pap smears and cervical cancer; feelings about being tested for HPV; concerns if tested positive; acceptability of HPV testing | 10 of the 16 knowledge questions were answered correctly significantly more often after the education intervention. Concern about testing positive to HPV decreased from 60% to 27% after education but the most common concern, a future diagnosis of cervical cancer, increased slightly. Women did not feel particularly anxious about getting tested for HPV and were very likely to agree to it | |||
| Patel, 2008 Pittsburgh, PA, USA | Hospital colposcopy clinic serving mainly low-income women | Questionnaire distributed in clinic January–May 2007 RR not reported | 202 women aged >18 years, 58% had >1 colposcopy visit; 58% white; 38% black; 41% high school education or less | Knowledge of HPV; preferred follow-up strategy after a diagnosis of CIN1: (1) smear test at 6 and 12 months (2) HPV test at 12 months | 75% knew what HPV or the HPV test was; 40% knew HPV is associated with warts, abnormal smears, cervical cancer, and 65% that it is sexually transmitted. 87% felt knowing their HPV status made them feel less nervous and 67% would feel less nervous if they could have less frequent smears. However, 64% preferred follow-up to be a smear test at 6 and 12 months, rather than an HPV test in 1 year | |||
Abbreviations: ASCUS=atypical squamous cells of undetermined significance; CIN=cervical intraepithelial neoplasia; HPV=human papillomavirus; LSIL=low-grade squamous intraepithelial lesion; RR=response rate.
Age range, ethnicity, educational level and indicators of socio-economic status are given where data are available.
Study quality
All included qualitative studies were considered by two reviewers to be of good to moderately good standard (Table 4). Only one survey was deemed to be good quality, that is, well conducted with a large sample size (>500) and high response rate (>80% Huang et al, 2008; Table 5).
Table 4. Quality assessment of qualitative studies.
| Anhang, 2004 | Brown, 2007 | Daley, 2010 | Fernandez, 2009 | Kahn, 2007 | Marlow, 2003 | McCaffery, 2003 | McCaffery, 2005 | McCaffery, 2006 | Vanslyke, 2009 | Waller, 2007b | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Theoretical approach | |||||||||||
| 1.1 Is a qualitative approach appropriate? | |||||||||||
| Appropriate | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Inappropriate | |||||||||||
| Unsure | |||||||||||
| 1.2 Is the study clear in what it seeks to do? | |||||||||||
| Clear | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Unclear | |||||||||||
| Mixed | |||||||||||
| Study design | |||||||||||
| 2.1 How defensible/ rigorous is study design/ methodology? | |||||||||||
| Defensible | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Not defensible | |||||||||||
| Unsure | ✓ | ||||||||||
| Data collection | |||||||||||
| 3.1 How well was data collection carried out? | |||||||||||
| Appropriate | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Inappropriate | |||||||||||
| Unsure/ unclear | ✓ | ||||||||||
| Validity | |||||||||||
| 4.1 Is researcher’s role clearly described? | |||||||||||
| Clear | ✓ | ||||||||||
| Unclear | |||||||||||
| Not described | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 4.2 Is context clearly described? | |||||||||||
| Clear | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Unclear | ✓ | ✓ | |||||||||
| Unsure | |||||||||||
| 4.3 Were methods reliable? | |||||||||||
| Reliable | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Unreliable | |||||||||||
| Unsure | ✓ | ✓ | |||||||||
| Analysis | |||||||||||
| 5.1 Is data analysis sufficiently rigorous? | |||||||||||
| Rigorous | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Not rigorous | |||||||||||
| Unsure/unreported | |||||||||||
| 5.2 Are the data ‘rich’? | |||||||||||
| Rich | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Poor | |||||||||||
| Poorly reported | ✓ | ✓ | |||||||||
| 5.3 Is the analysis reliable? | |||||||||||
| Reliable | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Unreliable | |||||||||||
| Unsure/unreported | ✓ | ✓ | ✓ | ||||||||
| 5.4 Are findings convincing? | |||||||||||
| Convincing | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Not convincing | |||||||||||
| Unsure | |||||||||||
| 5.5 Are findings relevant to aims of the study? | |||||||||||
| Relevant | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Irrelevant | |||||||||||
| Part relevant | ✓ | ||||||||||
| Ethics | |||||||||||
| 6.1 Clear and coherent reporting of ethical considerations? | |||||||||||
| Clear | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Unclear | |||||||||||
| Unsure/unreported | ✓ | ||||||||||
| Overall quality: G=good; M=moderately good | G | M | G | G | G | M | G | G | G | G | G |
Table 5. Quality assessment of surveys.
| Daley, 2010 | Ferris, 1997 | Huang, 2008 | Le, 2004 | McCaffery, 2008 | Papa, 2009 | Patel, 2008 | |
|---|---|---|---|---|---|---|---|
| Overall clarity of aims and method: | |||||||
| Is the study reported in sufficient detail and clarity for the reader to understand and make sense of it? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Selection of the sample: | |||||||
| Could responders be different from non-responders, or from the population the sample was taken from? | L | ✓ | ✓ | ✓ | ✓ | R | R |
| Measurement issues: | |||||||
| Are the measures reported objective and reliable? | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ |
| Survey methods: | |||||||
| Was the survey carried out in a trustworthy way? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Data and statistical issues: | |||||||
| Was the analysis appropriately conducted? | S | ✓ | ✓ | S | S | S | ✓ |
| Bias | |||||||
| Is there evidence of any other biases (e.g., funding bias)? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Abbreviations: L=low response rate (⩽60%); R=response rate not reported; S=small sample (⩽200); ?=scenarios were complex and questions ambiguous, representing a potential source of bias.
Evidence synthesis
Three main categories (and themes within them) emerged from the included studies.
The psychosocial burden of HPV infection
Emotional responses to diagnosis
Nine qualitative studies described participants’ emotional reactions to receiving an HPV diagnosis, either in reality (McCaffery and Irwig, 2005; McCaffery et al, 2006; Kahn et al, 2007; Waller et al, 2007b; Daley et al, 2010) or in response to hypothetical questions (McCaffery et al, 2003; Anhang et al, 2004; Vanslyke et al, 2008; Fernandez et al, 2009). All reported emotions such as worry, fear, anger, distress, anxiety, upset, shock and confusion. In one study a negative test result, following a previous positive result, was associated with feelings of relief or happiness (Waller et al, 2007b). Some participants found awareness of their HPV status reassuring or empowering (McCaffery et al, 2003; Anhang et al, 2004; Kahn et al, 2007; Vanslyke et al, 2008), because, if positive, they felt they could do something about it.
Women… characterised the HPV test result as a three-part negative diagnosis…they find out that (1) they have an abnormal result, (2) a sexually transmitted disease that is not curable and (3) a condition that may progress to cancer. (Daley et al, 2010) (USA, abnormal cytology, all HPV+)
A number of participants, particularly those with abnormal result, believed that early discovery of an abnormal test result enabled them to take action to prevent later disease. (Kahn et al, 2007) (USA, all tested, 23% abnormal cytology, 51% HPV+)
Three USA surveys reported emotional reactions to HPV test results; two of these had small samples and all three had a low or unreported response rate. In one all participants had abnormal cytology and were HPV positive (Daley et al, 2010). Negative responses included stigma (71%), anxiety (94%), stress (95%), anger (70%), confusion (71%), shock (70%) and self-blame (68%); 26% thought their HPV test results could change their future pregnancy plans. However, there were also positive responses: 95% agreed that ‘it could be worse’, 63% were ‘hopeful’, 68% felt ‘in control’ and 20% ‘empowered’. For women attending a primary care clinic for their annual smear test, concern about testing positive for HPV decreased from 60 to 27% following an educational intervention but concern about a future diagnosis of cervical cancer increased slightly (Papa et al, 2009). Of 202 women surveyed in a colposcopy clinic, 87% felt that knowing their HPV status made them feel less nervous (Patel et al, 2008).
Anxiety associated with HPV-positive status
In four qualitative studies, specific worries for those who had received a positive HPV test result included possible transmission to a partner, risk of cervical cancer, impact on sexual relationships and fertility, and fear of stigma and blame (McCaffery and Irwig, 2005; McCaffery et al, 2006; Waller et al, 2007b; Daley et al, 2010).
These (feelings) included fear and anxiety about cancer and becoming ill, concerns about fertility, feelings of being unclean because of the sexually transmitted nature of HPV, concerns about transmission and sexual relationships, a negative impact on feelings about sex, and relationship issues including blaming a partner for the infection. (Waller et al, 2007b) (UK, normal cytology, all HPV+ at baseline)
Six qualitative studies described worry about the definition of HPV as an sexually transmitted infection (STI; Anhang et al, 2004; McCaffery and Irwig, 2005; McCaffery et al, 2006; Brown et al, 2007; Kahn et al, 2007; Daley et al, 2010). For many participants, especially in specific ethnic and religious groups (South Asian, Hispanic, Roman Catholic), associations with promiscuity and immoral behaviour led to feelings of stigma, shame and embarrassment, and potentially grave consequences.
They associated stigma with sexual transmission, linking HPV transmission to infidelity, immorality and degenerate behaviour. They clearly anticipated extreme [psychological] discomfort if informed of having positive test results. (Brown et al, 2007) (Canada, hypothetical)
There were also similarities between the South Asian group and the white British and African Caribbean women with strong religious beliefs. Among these women there was some existing stigma around an abnormal smear, and a direct link with sexual activity and promiscuity.(McCaffery et al, 2006) (UK, all tested, 54% abnormal cytology, 77% HPV+)
However, one small US survey of a mainly white population tests reported that, following an educational intervention, participants did not feel particularly anxious about getting tested for HPV and were very likely to agree to it (Papa et al, 2009).
The effect of HPV diagnosis on relationships
The effect of an HPV diagnosis on relationships was explored in seven qualitative studies, four relating to real situations (McCaffery et al, 2006; Kahn et al, 2007; Waller et al, 2007b; Daley et al, 2010) and three to hypothetical questions (McCaffery et al, 2003; Vanslyke et al, 2008; Fernandez et al, 2009). In response to hypothetical situations, both men and women would worry that their partner had been unfaithful or that they themselves would be accused of infidelity. They were concerned about the effect this would have on their relationship, particularly if there were already relationship problems. For women who had received HPV positive test results, similar concerns were expressed and appeared to be connected with participants’ assumptions that the infection must have come from a current or recent partner.
… in relationships where there had been recent discord, infidelity, or had ended unhappily, the HPV test result led to questions about trust and fidelity and accusations of blame for the infection. (McCaffery et al, 2006) (UK, all tested, 54% abnormal cytology, 77% HPV+)
Most women said that their partner would be angry, doubt their fidelity, and possibly abandon them... While some men understood that their own infidelity could be the cause of their partner’s infection, most stated that their first reaction would be to question the woman’s faithfulness. (Fernandez et al, 2009) (USA, hypothetical)
In two qualitative studies, where participants realised that HPV infection could lie dormant for a considerable period and therefore could have been acquired from their own or their partners’ previous relationships, less anxiety was expressed (McCaffery et al, 2006; Waller et al, 2007b). Failure to understand this led participants to believe that the test was a reliable method of establishing fidelity (McCaffery et al, 2003; Kahn et al, 2007). None of the included surveys addressed this theme.
Particularly reassuring was the knowledge that the virus could lie dormant for a long time so exposure was not necessarily recent and did not mean that a partner had been unfaithful. (Waller et al, 2007b) (UK, normal cytology, all HPV+ at baseline)
An unexpected finding was the frequency with which participants noted that testing was an effective way to monitor one’s sexual partners. (Kahn et al, 2007) (USA, all tested, 23% abnormal cytology, 51% HPV+)
Participants were divided about feelings of guilt relating to a positive HPV diagnosis. Some women considered themselves at least partially to blame (McCaffery et al, 2006; Kahn et al, 2007; Daley et al, 2010). However, some felt that guilt was not necessary because STIs, such as HPV, are so common (McCaffery et al, 2006; Kahn et al, 2007), or that there is no guilt attached to HPV if it is perceived as cancer rather than an STI (Kahn et al, 2007). None of the included surveys addressed this theme.
Reasons given for feeling guilty focused on not taking care of oneself, not practising safe sexual behaviours, and not monitoring one’s sexual partner…they would share responsibility because they stayed with him despite knowing he was unfaithful, did not insist that he use a condom, or did not monitor him carefully enough. (Kahn et al, 2007) (USA, all tested, 23% abnormal cytology, 51% HPV+)
Among this group of women, common STIs such as HPV were seen as an inevitable part of sexual activity. (McCaffery et al, 2006) (UK, all tested, 54% abnormal cytology, 77% HPV+)
Concerns about disclosure of HPV status
Another issue that added to the burden of anxiety was disclosure (McCaffery and Irwig, 2005; McCaffery et al, 2006; Kahn et al, 2007; Waller et al, 2007b; Marlow et al, 2009; Daley et al, 2010); it was noted that the majority of women told, or intended to tell, someone that they had received a positive HPV test result (Kahn et al, 2007; Daley et al, 2010). The reason some participants gave was a sense of responsibility to past, current and future sexual partners. Others wanted support from the people they disclosed their test results to, but this was not always possible. Where participants had disclosed their HPV-positive status, some reported limited supportive response because of a general lack of knowledge about the virus (McCaffery et al, 2006; Waller et al, 2007b). Reasons women mentioned for not disclosing their positive HPV test result included feelings of stigma and shame, as well as feeling unable to explain their result or not thinking it was necessary (McCaffery et al, 2006; Kahn et al, 2007; Waller et al, 2007b). In one study, some participants avoided talking to their partners about their positive HPV test result by focussing instead on their smear test result (McCaffery et al, 2006). However, it was also acknowledged that, among couples who were open with each other about their sexual history, disclosure did not pose problems (McCaffery et al, 2006).
For women entering new relationships testing positive led to worries about transmitting the infection to their new partner and anxieties about disclosing their infection to someone they had only recently met. (McCaffery et al, 2006) (UK, all tested, 54% abnormal cytology, 77% HPV+)
For some women feeling anxious led them to disclose their result and this helped lessen their concerns when friends and family were reassuring and supportive. For others disclosure was unhelpful because friends and family had not heard of HPV and so were not able to provide the support that had been hoped for. (Waller et al, 2007b) (UK, normal cytology, all HPV+ at baseline)
One US survey of women, who had tested HPV positive and who had abnormal smear test results (Daley et al, 2010), explored intentions to disclose their HPV status to others and found that 93% had, most commonly to a partner (39%), female friend (28%) or their mother (18%), and 66% said they would disclose it to a future partner. This was a small survey with a risk of response bias.
The acceptability of HPV testing and triage
Acceptability of HPV testing
Questions about the acceptability of HPV testing for women were mainly asked in hypothetical scenarios in the qualitative studies. In five out of six of these, participants were asked how they would feel about HPV testing if it were available (McCaffery et al, 2003; Anhang et al, 2004; Brown et al, 2007; Vanslyke et al, 2008; Fernandez et al, 2009). Although most found the idea of testing acceptable, some participants worried that the test would be embarrassing or uncomfortable, feared the consequences of a positive outcome or, being in a monogamous relationship, saw no need for it. There was also more resistance to HPV testing among South Asian and Roman Catholic groups.
For the Indian and Pakistani women, testing was perceived to reflect non-traditional cultural or religious practices concerning sex and monogamy… Among the White British women taboos surrounding sex within Catholic families were also raised as potentially restrictive to women participating in HPV testing. (McCaffery et al, 2003) (UK, hypothetical)
The stigma associated with testing HPV positive did not discourage them from recognising value of HPV testing…The desire to gain knowledge from test results and to act responsibly outweighed the stigma attached to carrying the virus. (Brown et al, 2007) (Canada, hypothetical)
In one hypothetical study (Brown et al, 2007), women thought HPV testing was preferable to repeat smear tests but in another study where HPV-positive participants had a second HPV test after 12 months (Waller et al, 2007b), most preferred the reassurance of colposcopy to a further 12 month wait and a third HPV test.
The primary reasons for supporting this choice (HPV test) were the convenience of a single testing visit and the reduced anxiety involved with not having to undergo repeat cytology in 6 months. The key argument in favour of HPV testing, overall, was a faster, more definitive result that guided them to appropriate options. (Brown et al, 2007) (Canada, hypothetical)
Anxiety was one reason for choosing to have a colposcopy immediately… There was a sense among some women that waiting another year they might allow something to develop which could otherwise be dealt with now. This was associated with the belief that cancer is a disease that can progress rapidly and therefore early detection and treatment must be important. (Waller et al, 2007b) (UK, normal cytology, all HPV+ at baseline)
The triage process
Six included surveys sought views on HPV triage. In one study, 968 women in US primary care were given two case scenarios for mildly abnormal cytology. After reading information, they were asked to choose their follow-up preferences for each from repeat smear test, HPV test, colposcopy or cervicography (Ferris et al, 1997). Only 7 and 8% preferred an HPV test, but the information was complex and choices only based on discomfort, accuracy and cost. The low risk of mild abnormalities progressing to cervical cancer following a negative HPV test was not explained.
In a well-conducted survey in US primary care, 865 older women (aged 50–80 years) were asked about the acceptability of HPV testing and its impact on their preferences for cervical screening (Huang et al, 2008). Acceptability was high; 64% wanted to be tested, but 78% wanted more frequent smear tests (>1 annually) if they tested positive. However, 55% of those under 65 years would accept three yearly smear tests if they tested HPV negative and had normal cytology, and 33% of those over 65 would be happy to stop cervical screening altogether if they had negative results.
Two surveys recruited women in colposcopy clinics. One was a Canadian study in which 100 women chose between two follow-up options, either six monthly colposcopy until two consecutive normal examinations and cytology results (standard practice) or HPV test and one annual colposcopy visit if HPV negative (Le et al, 2004), 64% chose the HPV test to triage the need for frequent colposcopy follow-up. The other sought the preferences of 202 US women after a diagnosis of grade one cervical intraepithelial neoplasia (CIN1) between a smear test at 6 and 12 months or an HPV test at 12 months (Patel et al, 2008). In this study, 67% said they would feel less nervous if they could have less frequent smears, yet 64% preferred follow-up to be a smear test at 6 and 12 months rather than an HPV test in 1 year, and 13% wanted both.
Finally, in one Australian survey, 94 women with mildly abnormal smear test results were given a decision aid and asked to choose between a repeat smear test (usual care) and an HPV test; 65% chose the HPV test (McCaffery et al, 2008).
The importance of informed consent
In two hypothetical qualitative studies, where there was overall support for HPV testing, participants mentioned the importance of informed consent (Brown et al, 2007; Vanslyke et al, 2008). Both women who were tested and those who were not wanted to know more about the testing procedure (Waller et al, 2007b; Vanslyke et al, 2008; Marlow et al, 2009).
Across groups, participants spoke emphatically about the importance of women giving express consent prior to being tested for HPV, and said they would feel violated, tricked or angry if they were tested without their knowledge. (Vanslyke et al, 2008) (USA, hypothetical)
Information needs
Content and quality of information
Among the qualitative studies, women emphasised that the content and quality of information was important and that unclear information could be misleading and unhelpful (McCaffery et al, 2003; McCaffery and Irwig, 2005; McCaffery et al, 2006). One study drew attention to the difficulty people had in interpreting new information about HPV in the context of their existing knowledge (Fernandez et al, 2009), and in three, participants had sought information from the media, the internet or other sources (McCaffery and Irwig, 2005; Waller et al, 2007b; Daley et al, 2010).
It was recognised in all groups that clear and accurate information was critical to everyone’s response to HPV and the potential impact of testing... ‘Ignorance causes many problems’. (McCaffery et al, 2003) (UK, hypothetical)
Throughout the discussions, participants continued to show confusion about the new information as they attempted to fit it into their current schemas for sexually transmitted diseases, infection, cancer and other illness. (Fernandez et al, 2009) (USA, hypothetical)
One US survey of 154 women who had tested HPV positive and had abnormal smear test results (Daley et al, 2010) found that 82% had sought information about HPV from the internet and 70% from other sources. However, only 31% responded.
Unanswered questions
Specific queries were raised in most of the studies including questions related to HPV transmission (McCaffery et al, 2003; Anhang et al, 2004; McCaffery and Irwig, 2005; Vanslyke et al, 2008; Fernandez et al, 2009; Marlow et al, 2009; Daley et al, 2010), prevention (Anhang et al, 2004; McCaffery and Irwig, 2005; McCaffery et al, 2006; Vanslyke et al, 2008; Marlow et al, 2009; Daley et al, 2010), symptoms (Anhang et al, 2004; Vanslyke et al, 2008; Fernandez et al, 2009; Marlow et al, 2009), risk factors for HPV infection and cervical cancer (Anhang et al, 2004; Marlow et al, 2009) and whether HPV could cause other cancers or genital warts (McCaffery et al, 2003; Anhang et al, 2004; McCaffery and Irwig, 2005; Marlow et al, 2009).
… many asked whether HPV could be transmitted to a baby during pregnancy or delivery. (Anhang et al, 2004) (USA, hypothetical)
Information concerning a possible cure was sought. Some women were curious about the preventive properties of condoms. (Daley et al, 2010) (USA, abnormal cytology, all HPV+)
All women wanted to know the cause of HPV and once told it was sexually transmitted, they asked if this was the only way to contract it… if lifestyle factors such as diet or alcohol increased risk of infection… the potential for the virus to clear spontaneously and how long this took…(Marlow et al, 2009) (UK, hypothetical)
Questions also arose about the natural history of HPV infection and its progression to cervical cancer including prevalence of HPV and cervical cancer (Marlow et al, 2009), the timeline (Marlow et al, 2009), and latency and regression (Anhang et al, 2004; McCaffery and Irwig, 2005; Waller et al, 2007b; Marlow et al, 2009). In three studies participants wanted information about the consequences of HPV infection for sexual partners (McCaffery and Irwig, 2005; Fernandez et al, 2009; Marlow et al, 2009), and in two of these there were also questions about the effect of HPV on pregnancy and fertility (McCaffery and Irwig, 2005; Marlow et al, 2009).
They asked about prevalence of HPV…and wanted to know why so many women become infected… Women were particularly interested in the time between contracting HPV and developing cervical cancer …Younger women (18–25) asked many questions about the prevalence of cervical cancer... (Marlow et al, 2009) (UK, hypothetical)
Women wanted to know how long the virus could lie dormant and whether it would ever completely clear. If women had had a previous abnormality in the past, they wanted to know whether this was a new infection or a recurrence of the previous infection… They also wanted to know what they could do about it themselves and whether HPV could impact on their fertility. (McCaffery and Irwig, 2005) (Australia, abnormal cytology, all HPV+)
Consequences for men were frequently mentioned, including whether men were just carriers or are likely to experience harmful effects. (Marlow et al, 2009) (UK, hypothetical)
None of the included surveys reported whether there were any unanswered questions.
Misunderstandings and misinterpretations
In several of the qualitative studies, there was considerable confusion, misunderstanding or misinterpretation. This was particularly apparent in the studies where participants had not been tested for HPV and had minimal prior knowledge (Anhang et al, 2004; McCaffery et al, 2006; Fernandez et al, 2009; Marlow et al, 2009; Daley et al, 2010).
A number of women tried to equate descriptions of HPV as low risk or high risk with risky behaviours or risky individuals, as opposed to strains of the virus. (Anhang et al, 2004) (USA, hypothetical)
After being told that HPV caused most cases of cervical cancer, many women interpreted the diagnosis of HPV as equivalent to a diagnosis of cancer. (Fernandez et al, 2009) (USA, hypothetical)
A particular source of anxiety and confusion for many participants was the association between HPV and warts (McCaffery et al, 2003; Anhang et al, 2004; McCaffery and Irwig, 2005; McCaffery et al, 2006; Kahn et al, 2007). People were confused about different types of warts, where on the body they might occur and how they were associated with different HPV types. This was compounded by doctors’ use of the term ‘wart virus’ when referring to high-risk HPV. Genital warts were thought to be disgusting and highly stigmatizing, and the possibility of developing them was a source of great distress (McCaffery et al, 2003; McCaffery and Irwig, 2005; McCaffery et al, 2006; Kahn et al, 2007). None of the included surveys addressed this theme.
All the women interviewed were aware of genital warts and some thought there was an association with genital warts and cervical cancer. Because of the greater familiarity with genital warts and because clinicians often referred to HPV as the ‘wart virus’, many of the women interviewed thought they had genital warts on their cervix or elsewhere internally and were concerned they might spread to other visible genital areas or cause warts on their partner. (McCaffery and Irwig, 2005) (Australia, abnormal cytology, all HPV+)
(Some women) highlighted the negative connotations of the term ‘wart’, which seemed to have a long-standing stigma as an STI... ‘Warts’ in any form were viewed as unpleasant and unwanted and these perceptions were described as being rooted in early childhood experience. (McCaffery et al, 2003) (UK, hypothetical)
Information that helped to reassure
Some of the information given to study participants helped to alleviate their anxiety (McCaffery and Irwig, 2005; McCaffery et al, 2006; Waller et al, 2007b). This included that HPV is common (McCaffery and Irwig, 2005; McCaffery et al, 2006), does not have symptoms (McCaffery et al, 2006; Waller et al, 2007b) and can be cleared by the immune system (McCaffery and Irwig, 2005; McCaffery et al, 2006; Waller et al, 2007b). Reassurance also came from being informed that the transition from HPV infection to cervical cancer was slow (McCaffery and Irwig, 2005), that there is effective treatment for CIN (McCaffery et al, 2006; Waller et al, 2007b), and that men rarely experience adverse effects (McCaffery et al, 2006). Women’s distress associated with genital warts was allayed by the information that warts were unlikely to develop (McCaffery and Irwig, 2005; McCaffery et al, 2006). Counter-intuitively the information that condoms are only partially effective in preventing transmission of HPV was also reassuring for two reasons: it relieved women’s sense of guilt for not using them and it removed the need to suggest their use, which could be interpreted by a partner as mistrust or suspicion (McCaffery et al, 2003; McCaffery et al, 2006).
Understanding that the impact of HPV on men was negligible…appeared to alleviate considerable anxiety. Importantly it meant that there was no necessity to inform sexual partners about the infection, which allowed women to avoid the challenges of disclosure. (McCaffery et al, 2006) (UK, all tested, 54% abnormal cytology, 77% HPV+)
Information that the transition from HPV infection to cervical cancer is slow was an important factor which reduced some women’s anxiety about their infection. This appeared particularly useful for women following observational management. (McCaffery and Irwig, 2005) (Australia, abnormal cytology, all HPV+)
None of the included surveys addressed what information would offer reassurance.
Discussion
Summary of main findings
This is the first systematic review and qualitative synthesis of an emerging international literature on people’s views about HPV testing in the context of cervical screening. Three thematic categories emerged: the psychosocial burden of HPV infection, the acceptability of HPV testing and triage and information needs. Notably, the first was much more prominent in ‘real’ situations where participants expressed overwhelmingly negative concerns, suggesting that facing an HPV diagnosis in real life, with the associated problems of disclosure and fear of stigmatisation, was more daunting than women imagined in hypothetical scenarios. Many women in the studies of HPV testing as a hypothetical proposal thought it a preferable alternative to repeat smear tests, but did not want to be tested without their knowledge or without informed consent. Our review reveals an overwhelming lack of understanding about HPV with participants struggling to interpret limited information in the context of existing knowledge, impacting on the ability to make informed choices.
How this study fits in
Our findings confirm those of a review revealing poor knowledge about HPV infection (Klug et al, 2008), inform the existing literature on patient education and HPV suggesting the need for simple, clear, targeted information (Waller et al, 2007a; Hall et al, 2008; Klug et al, 2008; McNair et al, 2009; Roland et al, 2009; Waller et al, 2009; McCaffery et al, 2010), and augment the literature on the psychological effects of testing HPV positive (McCaffery et al, 2004; Maissi et al, 2005; Wang et al, 2010).
Study strengths and limitations
Our review was comprehensive and rigorously conducted. In August 2011, we repeated the searches and found no new studies meeting our inclusion criteria. There are conflicting views on what counts as data from primary qualitative studies, and whether original data, authors’ interpretations or both should be included (Major and Savin-Baden, 2010). We chose to include authors’ words as they represented syntheses of complete sets of original data of which the quotations were illustrative examples.
The review was limited by the scope of the primary studies. There were no relevant studies exploring the views of health professionals. Only one qualitative study and none of the surveys recruited male participants. None of the studies developed the theme of the impact of HPV on men, nor were there any that investigated the views of lesbian and bisexual women. Therefore, our review cannot reflect the views of these groups, although more than half of the study populations included different ethnic groups. However, there were limited comparisons between the groups and little in-depth exploration of the related cultural influences. Nevertheless, the rich data in the qualitative studies vividly conveyed women’s views. However, the small number and relatively poor quality of surveys only supplemented the qualitative studies to a limited extent.
It is possible that the research itself, by raising issues for discussion, may exacerbate anxiety; a study of women with abnormal cervical cytology unaware of their HPV status suggested that anxiety may be explained by factors other than learning of test results and may vary by ethnicity and lifestyle factors (Johnson et al, 2011). Our findings should be placed in the context of the large number of tests having been carried out worldwide over the past 5 years.
None of the studies investigated views about HPV triage in the context of the UK model. Although some women may be relieved not to have repeat smear tests, others may find the idea of not acting on an abnormal test result difficult. None of the studies explored the introduction of HPV vaccination and how this would relate to cervical screening and HPV testing. Of the 17 included studies, only four qualitative studies and no surveys were conducted in the United Kingdom. Therefore, the extent to which their findings are applicable in UK settings is uncertain.
Implications for research, and UK policy and practice
More research may be needed to investigate the information needs of women at different stages of the cervical screening processes, and of specific groups including health professionals, HPV-vaccinated women, ethnic minority and other hard-to-reach groups. Women asked well-considered, thoughtfully-framed questions indicating real concern and desire to know more. Nevertheless, it is important for genuinely informed consent that people are not overwhelmed with information (O'Neill, 2003). Identification of the salient points allowing informed choice or uptake from this complex information remains a challenge to researchers. However, this review forms part of the ongoing, multi-method HPV Core Messages Study and our findings will be aggregated with the other study components (a systematic review of views on HPV vaccination, qualitative interviews with UK women and girls, and surveys of UK public and healthcare professionals) to inform the development of educational materials.
Some terminology, for example, ‘high-risk HPV’ and ‘wart virus’, was confusing or alarming and not clearly understood. Explanations about causation, risk of cervical abnormality or cancer, persistence/clearance of monogenic HPV and difference from genital wart viruses are needed. Valuable reassuring messages were: HPV is common, symptom free, usually clears without treatment and rarely has adverse effects on men. Although many women were strongly motivated to share their worries and concerns about an HPV-positive test, some could not, because of lack of understanding, inability to articulate their story, their confidantes’ inability to understand, or fear of stigma or blame. It may be helpful to emphasize the commonness of HPV so that it becomes normalized as an everyday infection. Familiarization with HPV through the vaccination programmed could help.
Conclusions
Faced with this new protocol, clear and consistent information and the avoidance of ambiguous or misleading terminology could alleviate women’s anxiety, relieve their burden of blame and allow them informed consent. This is a substantial challenge for those who design and provide information.
Acknowledgments
We acknowledge the contributions of Theresa Marteau, Kirsten McCaffery and the late Joan Austoker to study design, and thank Sally Warmington, Annie Hendry, Ellen Richards and the staff of John Spalding Library, Wrexham Medical Institute, for their help. This study is part of the multi-method HPV Core Messages project, funded by Cancer Research UK (ref C1273/A9479).
Appendix 1
Search strategy
Databases searched
MEDLINE
MEDLINE in process and other non-indexed citations
EMBASE
CINAHL (Cumulative Index to Nursing and Allied Health Literature)
PsycINFO
AMED (Allied and Complementary Medicine Database)
HMIC (Health Management Information Consortium)
BNI (British Nursing Index)
Cochrane library
BIOSIS
SCI (Science Citation Index)
SSCI (Social Science Citation Index)
ISI proceedings
ASSIA (Applied Social Sciences Index and Abstracts)
Search Strategy for Medline (adapted for other databases)
Papillomavirus Vaccines/
DNA Probes, HPV/
Human papillomavirus 16/
Human papillomavirus 18/
(HPV).ti,ab.
(Human papilloma viru$).ti,ab.
(Human papillomaviru$).ti,ab.
(vaccin$ or immunis$).ti,ab.
(prevent or prevention or preventing).ti,ab.
(test or testing).ti,ab.
1 or 2 or 3 or 4 or 5 or 6 or 7
8 or 9 or 10
11 and 12
13 limited to human
16 limited to 1980 onwards
(L1 or E2 or E5 or E6 or E7).ti,ab.
15 not 16
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
The authors declare no conflict of interest.
References
- Anhang R, Wright TC, Smock L, Goldie SJ (2004) Women’s desired information about human papillomavirus. Cancer 100, pp 315–320 [DOI] [PubMed] [Google Scholar]
- Barratt A, Trevena L, Davey H, McCaffery K (2004) Use of decision aids to support informed choices about screening. BMJ 329(7464): 507–510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekker H (2010) Decision aids and uptake of screening: aids improve informed decision making, but not necessarily uptake. BMJ 341: c5407. [DOI] [PubMed] [Google Scholar]
- Brown L, Ritvo P, Howlett R, Cotterchio M, Matthew A, Rosen B, Murphy J, Mai V (2007) Attitudes toward HPV testing: interview findings from a random sample of women in Ontario, Canada. Health Care Women Int Vol. 28, pp 782–798 [DOI] [PubMed] [Google Scholar]
- Daley EM, Perrin KM, McDermott RJ, Vamos CA, Rayko HL, Packing-Ebuen JL, Webb C, McFarlane M (2010) The psychosocial burden of HPV: a mixed-method study of knowledge, attitudes and behaviors among HPV+ women. J Health Psychol 15(2): 279–290 [DOI] [PubMed] [Google Scholar]
- Department of Health (2011) Improving Outcomes: a Strategy for Cancer, http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_123394.pdf Accessed 12 July 2011
- Fernandez ME, McCurdy SA, Arvey SR, Tyson SK, Morales-Campos D, Flores B, Useche B, Mitchell-Bennett L, Sanderson M (2009) HPV knowledge, attitudes, and cultural beliefs among Hispanic men and women living on the Texas-Mexico border. Ethn Health 14(6): 607–624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris DG, Kriegel D, Cote L, Litaker M, Woodward L (1997) Women's triage and management preferences for cervical cytologic reports demonstrating atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesions. Arch Fam Med 6(4): 348–353 [DOI] [PubMed] [Google Scholar]
- Hall B, Howard K, McCaffery K (2008) Do cervical cancer screening patient information leaflets meet the HPV information needs of women? Patient Educ Couns 72(1): 78–87 [DOI] [PubMed] [Google Scholar]
- Harden A, Garcia J, Oliver S, Rees R, Shepherd J, Brunton G, Oakley A (2004) Applying systematic review methods to studies of people's views: an example from public health research. J Epidemiol Community Health 58(9): 794–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang AJ, Perez-Stable EJ, Kim SE, Wong ST, Kaplan CP, Walsh JME, Iwaoka-Scott AY, Sawaya GF (2008) Preferences for human papillomavirus testing with routine cervical cancer screening in diverse older women. J Gen Intern Med 23(9): 1324–1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson CY, Sharp L, Cotton SC, Harris CA, Gray NM, Little J (2011) Human papillomavirus infection and anxiety: Analyses in women with low-grade cervical cytological abnormalities unaware of their infection status. PLoS ONE 6(6): e21046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn JA, Slap GB, Bernstein DI, Tissot AM, Kollar LM, Hillard PA, Rosenthal SL (2007) Personal meaning of human papillomavirus and Pap test results in adolescent and young adult women. Health Psychol 26(2): 192–200, (37 ref) [DOI] [PubMed] [Google Scholar]
- Klug SJ, Hukelmann M, Blettner M (2008) Knowledge about infection with human papillomavirus: a systematic review. Prev Med 46(2): 87–98 [DOI] [PubMed] [Google Scholar]
- Le T, Hicks W, Menard C, Boyd D, Hewson T, Hopkins L, Kee Fung MF (2004) Human papilloma virus testing knowledge and attitudes among women attending colposcopy clinic with ASCUS/LGSIL pap smears. J Obstet Gynaecol Canada 26(9): 788–792 [DOI] [PubMed] [Google Scholar]
- Maissi E, Marteau TM, Hankins M, Moss S, Legood R, Gray A (2004) Psychological impact of human papillomavirus testing in women with borderline or mildly dyskaryotic cervical smear test results: cross sectional questionnaire study. BMJ 328(7451): 1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maissi E, Marteau TM, Hankins M, Moss S, Legood R, Gray A (2005) The psychological impact of human papillomavirus testing in women with borderline or mildly dyskaryotic cervical smear test results: 6-month follow-up. Br J Cancer 92(6): 990–994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major CH, Savin-Baden M (2010) An Introduction to Qualitative Research Synthesis: Managing the Information Explosion in Social Science Research. Routledge: London [Google Scholar]
- Marlow LAV, Wardle J, Grant N, Waller J (2009) Human papillomavirus (HPV) information needs: a theoretical framework. J Fam Plann Reprod Health Care 35(1): 29–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery K, Forrest S, Waller J, Desai M, Szarewski A, Wardle J (2003) Attitudes towards HPV testing: a qualitative study of beliefs among Indian, Pakistani, African-Caribbean and white British women in the UK. Br J Cancer 88: 42–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery K, Irwig L (2005) Australian women's needs and preferences for information about human papillomavirus in cervical screening. J Med Screen 12(3): 134–141 [DOI] [PubMed] [Google Scholar]
- McCaffery K, Waller J, Forrest S, Cadman L, Szarewski A, Wardle J (2004) Testing positive for human papillomavirus in routine cervical screening: examination of psychosocial impact. BJOG 111(12): 1437–1443 [DOI] [PubMed] [Google Scholar]
- McCaffery K, Waller J, Nazroo J, Wardle J (2006) Social and psychological impact of HPV testing in cervical screening: a qualitative study. Sex Transm Infect 82(2): 169–174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery KJ, Irwig L, Chan SF, Macaskill P, Barratt A, Lewicka M, Clarke J, Weisberg E (2008) HPV testing versus repeat Pap testing for the management of a minor abnormal Pap smear: evaluation of a decision aid to support informed choice. Patient Educ Couns 73(3): 473–481 [DOI] [PubMed] [Google Scholar]
- McCaffery KJ, Irwig L, Turner R, Chan SF, Macaskill P, Lewicka M, Clarke J, Weisberg E, Barratt A (2010) Psychosocial outcomes of three triage methods for the management of borderline abnormal cervical smears: an open randomised trial. BMJ 340: b4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNair R, Power J, Carr S (2009) Comparing knowledge and perceived risk related to the human papilloma virus among Australian women of diverse sexual orientations. ANZ J Public Health 33(1): 87–93 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group FTP (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339: 332–339 [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (2009) The Guidelines Manual 2009, Appendix I: Methodology checklist: qualitative studies, http://www.nice.org.uk/aboutnice/howwework/developingniceclinicalguidelines/clinicalguidelinedevelopmentmethods/GuidelinesManual2009.jsp (Accessed 5 January 2011)
- NHS Cancer Screening Programmes (2010) HPV Triage and Test of Cure Protocol for Women Aged 25 to 64 Years, http://www.cancerscreening.nhs.uk/cervical/hpv-triage-test-flowchart-v2.pdf (Accessed 14 June 2011)
- NHS Centre for Reviews and Dissemination (2001) Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for those Carrying Out or Commissioning Reviews 2nd edn NHS CRD, University of York: York [Google Scholar]
- NHSCSP (2010) Colposcopy and Programme Management Guidelines for the NHS Cervical Screening Programme (2nd edition) ISBN 978 1 84463 069 1 http://www.cancerscreening.nhs.uk/cervical/publications/nhscsp20.pdf (Accessed 4 August 2011)
- O'Neill O (2003) Some limits of informed consent. J Med Ethics 29: 4–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papa D, Simas TAM, Reynolds M, Melnitsky H (2009) Assessing the role of education in women's knowledge and acceptance of adjunct high-risk human papillomavirus testing for cervical cancer screening. J Low Genit Tract Dis 13(2): 66–71 [DOI] [PubMed] [Google Scholar]
- Patel M, Guido R, Chang JC, Meyn LA (2008) What are patient preferences for follow-up after low-grade cervical intraepithelial neoplasia? J Low Genit Tract Dis 12(2): 122–126 [DOI] [PubMed] [Google Scholar]
- Pettigrew M, Roberts H (2006) Systematic Reviews in the Social Sciences: a Practical Guide. Blackwell: Oxford [Google Scholar]
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews: a product of the ESRC methods programme (Version I) (available from n.simpson@lancaster.ac.uk). Lancaster: Institute of Health Research, 2006 [Google Scholar]
- Ritchie J, Spencer L (1994) Qualitative data analysis applied policy research. In Analysing Qualitative Data Bryman A, Burgess R (eds) pp 173–194. Routledge: London [Google Scholar]
- Roland KB, Benard VB, Saraiya M, Hawkins NA, Brandt H, Friedman AL (2009) Assessing cervical cancer screening guidelines in patient education materials. J Women’s Health 18(1): 5–12 [Google Scholar]
- Swallow V, Newton J, Lottum CV (2003) How to manage and display qualitative data using 'Framework' and Microsoft® Excel. J Clin Nurs 12: 610–612 [DOI] [PubMed] [Google Scholar]
- Vanslyke JG, Baum J, Plaza V, Otero M, Wheeler C, Helitzer DL (2008) HPV and cervical cancer testing and prevention: knowledge, beliefs, and attitudes among Hispanic women. Qual Health Res 18(5): 584–596 [DOI] [PubMed] [Google Scholar]
- Waller J, Marlow LAV, Wardle J (2007a) The association between knowledge of HPV and feelings of stigma, shame and anxiety. Sex Transm Infect 83(2): 155–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller J, Marlow LAV, Wardle J (2009) Anticipated shame and worry following an abnormal Pap test result: The impact of information about HPV. Prev Med 48(5): 415–419 [DOI] [PubMed] [Google Scholar]
- Waller J, McCaffery K, Kitchener H, Nazroo J, Wardle J (2007b) Women’s experiences of repeated HPV testing in the context of cervical cancer screening: a qualitative study. Psycho-Oncol 16: 196–204 [DOI] [PubMed] [Google Scholar]
- Wang K-L, Jeng C-J, Yang Y-C, Chen C-A, Cheng W-F, Chen T-C, Mast TC, Wang Y-C, Hsieh C-Y (2010) The psychological impact of illness among women experiencing human papillomavirus-related illness or screening interventions. J Psychosom Obstet Gynaecol 31(1): 16–23 [DOI] [PubMed] [Google Scholar]