Abstract
Background:
Most solid tumours contain regions of sub-optimal oxygen concentration (hypoxia). Hypoxic cancer cells are more resistant to radiotherapy and represent the most aggressive fraction of a tumour. It is therefore essential that strategies continue to be developed to target hypoxic cancer cells. Inhibition of the DNA damage response (DDR) might be an effective way of sensitising hypoxic tumour cells to radiotherapy.
Methods:
Here, we describe the cellular effects of pharmacological inhibition of the apical DDR kinase ATR (Ataxia Telangiectasia and Rad 3 related) with a highly selective inhibitor, VE-821, in hypoxic conditions and its potential as a radiosensitiser.
Results:
VE-821 was shown to inhibit ATR-mediated signalling in response to replication arrest induced by severe hypoxia. In these same conditions, VE-821 induced DNA damage and consequently increased Ataxia Telangiectasia Mutated-mediated phosphorylation of H2AX and KAP1. Consistently, ATR inhibition sensitised tumour cell lines to a range of oxygen tensions. Most importantly, VE-821 increased radiation-induced loss of viability in hypoxic conditions. Using this inhibitor we have also demonstrated for the first time a link between ATR and the key regulator of the hypoxic response, HIF-1. HIF-1 stabilisation and transcriptional activity were both decreased in response to ATR inhibition.
Conclusion:
These findings suggest that ATR inhibition represents a novel strategy to target tumour cells in conditions relevant to pathophysiology and enhance the efficacy of radiotherapy.
Keywords: ATR, hypoxia, replication, radiation, VE-821
The induction of DNA damage by either chemo or radiotherapy has proved to be an effective strategy for cancer therapy, particularly for certain cancers such as testicular and ovarian (Einhorn, 2002; Agarwal and Kaye, 2003). Despite this, many tumours show little or poor response and this has been attributed to the presence of efficient and overlapping DNA repair pathways. A key component of the cellular defence against the cytotoxic effects of DNA damage is a detection and repair network known as the DNA damage response (DDR) (Jackson and Bartek, 2009). Upstream signalling components of the DDR are recruited to sites of DNA damage where they act to trigger checkpoints that transiently arrest the cell cycle and directly stimulate repair. Two key regulatory proteins are the phosphoinositol 3-kinase-like serine/threonine protein kinases (PIKK) ATM (Ataxia Telangiectasia Mutated) and ATR (Ataxia Telangiectasia and Rad 3 related) (Kastan and Bartek, 2004; Cimprich and Cortez, 2008). Ataxia Telangiectasia Mutated is recruited to sites of double-strand breaks induced, for example, by ionising radiation, while ATR is recruited to single-stranded DNA coated with replication protein A. This single-stranded DNA structure arises when DNA replication forks stall. This occurs during normal replication (for example at fragile sites) or during replication arrest induced by severe hypoxia as well as in response to certain DNA-damaging drugs, such as cross-linkers, antimetabolites and topoisomerase inhibitors (Hammond et al, 2002; Sogo et al, 2002; Zou and Elledge, 2003; Glover et al, 2005). In response to hypoxia, the replication arrest has been attributed to a rapid decrease in nucleotide levels, which may in turn be a result of reduced ribonucleotide reductase activity in the absence of oxygen (Pires et al, 2010).
Substantial research effort has been directed at therapeutically targeting the DDR. Disruption of ATR through depletion, expression of kinase-dead protein or inhibition with weak or partially selective inhibitors has demonstrated a pivotal role for ATR in the repair of DNA damage and in subsequent cell survival (Cliby et al, 1998; Nghiem et al, 2001; Hurley et al, 2007; Wilsker and Bunz, 2007; Nishida et al, 2009). Additional studies using the genetic or chemical inhibition of ATR function have hinted at the therapeutic benefit of ATR inhibitors in increasing the effect of conventional cancer therapies. For example, S. pombe lacking the ATR homologue rad3 were identified as being sensitive to both ionising radiation and UV (Nasim and Smith, 1975). More recent studies have demonstrated that functional inhibition of ATR leads to increased sensitisation of cancer cells to oncogenic stress (Gilad et al, 2010; Schoppy et al, 2012). In addition, it has been shown that cells expressing a kinase-dead mutant ATR are radiosensitive when compared with wild-type cells due to compromised homologous recombination repair (Wang et al, 2004). Similar effects were observed in ATR-Seckel cancer cells (Hurley et al, 2007). Furthermore, NU6027, a compound originally developed as a CDK2 inhibitor but also identified as a potent ATR inhibitor, was shown to sensitise the breast cancer cell line MCF7 to ionising radiation (Peasland et al, 2011).
Regions of hypoxia develop in solid tumours essentially because the cellular demand for oxygen exceeds the available supply. The principle causes of this are the limited diffusion distance of oxygen in tumours and the inefficient tumour vasculature (Chitneni et al, 2011). Rapid and frequent variations in red blood cell flux lead to cycling hypoxia, that is, periods of hypoxia followed by reoxygenation (Yasui et al, 2010). The degree of tumour hypoxia is extremely relevant to patient outcome as regions of tumour hypoxia present a significant barrier to cancer therapy (Hockel et al, 1993). Hypoxic cells are more resistant to both chemo and radiotherapy and have a more aggressive phenotype (Graeber et al, 1996; Bristow and Hill, 2008). Therefore, it is important that targeted agents be developed for eradicating cancer cells in hypoxic conditions. Current approaches to achieve this include the development of novel agents, such as HIF-1 inhibitors, or the strategies to increase the sensitivity of hypoxic cancer cells to existing therapy modalities (Melillo, 2007; Onnis et al, 2009; Begg et al, 2011). One of the consequences of hypoxia is the repression of DNA repair pathways, which has been associated with increased chemo/radioresistance and genomic instability (Bristow and Hill, 2008; Olcina et al, 2010).
Inhibition of the DDR is likely to be an effective way of sensitising hypoxic cells to cancer therapy (Olcina et al, 2010). For example, we have previously shown that depletion of ATR using siRNA promotes cancer cell death under hypoxic conditions (Hammond et al, 2004). The absence of selective inhibitors has made it difficult to investigate the value of targeting ATR as a therapeutic strategy. However, the selective ATR inhibitor VE-821 (3-amino-6- (4-(methylsulfonyl) phenyl)-N-phenylpyrazine-2-carboxamide) was recently described (Charrier et al, 2011; Reaper et al, 2011). Inhibition of ATR using VE-821, either alone or in combination with DNA-damaging agents promotes cytotoxicity in cancer cells but only a reversible growth arrest in normal cells, thus demonstrating a therapeutic window for treatment. In this study we have determined that the ATR inhibitor VE-821 significantly reduces hypoxia-induced ATR signalling and that this leads to a loss of cancer cell viability. In addition a decrease in HIF–1-mediated signalling was observed when ATR was inhibited in hypoxic conditions. Most importantly, VE-821 increased radiation-induced loss of viability in both normal and hypoxic conditions. These data suggest that inhibition of ATR in combination with standard therapies will be an important approach in the future to target the hypoxic fraction of tumours.
Materials and methods
Cell lines and spheroid growth
RKO, HCT116 and DLD1 (colorectal), U2OS (osteosarcoma), MG-U87 (glioblastoma), MDA-MB-231 and MDA-MB-468 (breast), VmCub1 (bladder), HeLa (cervical), SKmel28 and IGR39 (melanoma), RCC4 (renal carcinoma) and SQ20B (head and neck) human cancer cell lines were maintained in DMEM with 10% FBS. Spheroids were grown using MG-U87 cells and were formed using the liquid overlay method. In brief, exponentially growing monolayers were trypsinised and 104 cells were seeded in regular growth medium onto a 1% agar-coated well of a 24-well plate. In all, 12–24 spheroids were grown per condition. Spheroids were grown for 7–10 days until the average diameter was approximately 400 μm. Media was replaced every 2 days. Spheroids were imaged using a Nikon Eclipse TE2000-E microscope (Nikon UK Limited, Kingston Upon Thames, UK) and measured using the ImageJ software (NIH). All cell lines were routinely mycoplasma tested and found to be negative.
Drug treatments
VE-821 (3-amino-6- (4-(methylsulfonyl) phenyl)-N-phenylpyrazine-2-carboxamide) provided by Vertex Pharmaceuticals (Europe) Ltd (Oxfordshire, UK). ATMi KU55933 (2-morpholin-4-yl-6-thianthren-1-yl-pyran-4-one) was obtained from Calbiochem (Darmstadt, Germany).
Clonogenic survival assay
After treatment colonies (>50 cells) were allowed to form for 10–14 days. Colonies were then stained with methylene blue and counted.
Hypoxia treatment
Hypoxia treatments were carried out in a Bactron II anaerobic chamber (Shell labs) or an In vivo2 400 (Ruskinn). For experiments at ⩽0.02% O2 cells were plated on glass dishes. Where no period of reoxygenation is indicated, cells were harvested inside the chamber with equilibrated solutions. Oxygen concentrations were verified in the cell culture dish using an Oxylite probe (Oxford Optronix, Oxford, UK).
Irradiation
Cells were irradiated using a Cs-137 irradiator (GSM:GSR D1; dose rate 1.938 Gy min−1). For irradiation in hypoxic conditions cells were sealed in equilibrated air-tight boxes and transported to the source. To validate this methodology, the HIF-1α levels of cells incubated in the hypoxic boxes were determined (Supplementary Figure S1).
Immunoblotting
Cell monolayers or spheroids were lysed in UTB (9 ℳ urea, 75 mℳ Tris-HCl pH 7.5 and 0.15 ℳ β-mercaptoethanol) and sonicated briefly. Antibodies used were Chk2-T68, p53-S15, Chk1-S296, Chk1-S317 and Chk1-S345 (Cell Signaling Technologies, Danvers, MA, USA), KAP1-S824, (Bethyl Laboratories, Inc., Montgomery, AL, USA), ATM-S1981 (Epitomics, Inc., Burlingame, CA, USA), p53 and β-actin (Santa Cruz Biotechnology, Santa Cruz, CA, USA), γH2AX (Upstate-Millipore, Billerica, MA, USA), HIF-1α (BD Biosciences, Oxford, UK) and GLUT-1 (Abcam, Cambridge, UK). The Odyssey infrared imaging technology was used (LI-COR Biosciences, Lincoln, NE, USA).
Immunofluorescence
53BP1 (Novus Biologicals, Ltd, Cambridge, UK) staining was carried out as previously described (Bencokova et al, 2009). Because of the presence of 1–2 53BP1 foci in the nuclei of unstressed cells induction of DNA damage was quantified by counting cells with more than 6 foci. Cells were visualised using a Nikon 90i microscope (Nikon). For imaging of hypoxic regions, spheroids were incubated with EF5 (final concentration 200 μℳ) for 6 h prior to fixation. Spheroids were soaked in 4% PFA overnight, washed in PBS and then soaked with 1% Sucrose-PBS. Spheroids were embedded in OCT and stored at −20 °C. Serial sections of 8–10 μm were cut and mounted onto poly-ℒ-lysine-coated slides. EF5 binding was detected with Cy-3 conjugated ELK3-A8 monoclonal antibody, as previously described (Woods et al, 1996; Qayum et al, 2009). ELK5-A8 antibody and EF5-competed stain (ELK5-A8+EF5) were obtained from the Department of Radiation Oncology, University of Pennsylvania.
Single-molecule DNA fibre analysis
DNA fibres were generated as previously described (Wilsker et al, 2008; Pires et al, 2010). Fibre spreads were imaged using a Bio-Rad Radiance confocal microscope and analysed using ImageJ software (NIH). At least 200 replication structures were counted and at least 100 replication tracks were measured per experiment.
Scratch wound assay
Scratch wound assays were carried out as described previously (Coutts et al, 2011). Wounds were imaged with a Nikon Eclipse TE2000-E microscope (Nikon) using × 4 objective at the wound mark just prior to being placed in hypoxia (⩽0.02% O2) after which they were imaged again.
Reporter assay
Cells were transfected with 5 × -HRE-luc or pSV-βgal (80 ng per well) using Lipofectamine 2000 (Invitrogen Life Technologies, Grand Island, NY, USA), alongside pCMV-Renilla (0.2 ng per well) for normalisation. Media was replaced with media containing DMSO or VE-821 and placed in hypoxia for the times indicated. Firefly and Renilla luciferase activities were measured using the Dual Glo Luciferase assay (Promega, Madison, WI, USA).
Quantitative real-time PCR
Quantitative real-time PCR was performed as previously (Hammond et al, 2006) using the Thermo Scientific Verso QRT–PCR following manufacturers recommendations (Thermo Scientific, Erembodegem, Belgium). Reactions were carried out in a 7500 Fast real-time PCR detection system (Applied Biosystems, Carlsbad, CA, USA). GLUT-1 expression levels were normalised to 18S rRNA.
siRNA transfection
HIF-1 siRNA (sense 5′-CUGAUGACCAGCAACUUGAdTdT-3′) or Stealth RNAi negative control (Invitrogen Life Technologies) at a final concentration of 50 nℳ were transfected into MDA-MB-231 cells using DharmaFECT (Thermo Scientific) according to the manufacturers’ instructions.
Statistical analysis
Statistical significance of differences between means of at least n=3 experiments was determined using Student’s t-test (P-values indicated accordingly in figure legend or main text). Error bars represent +/− s.e.m.
Results
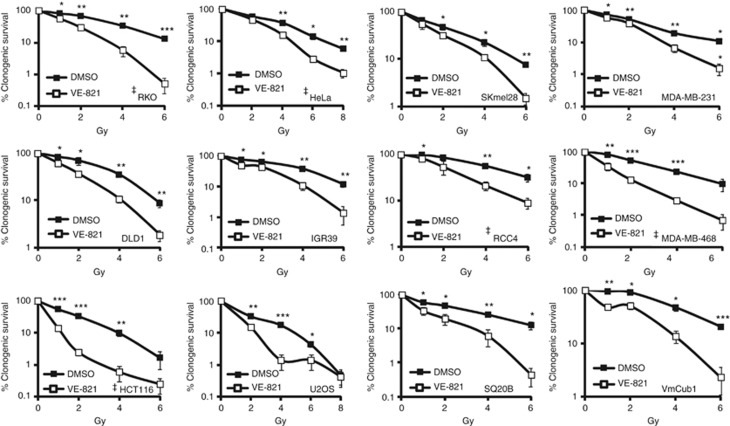
VE-821 radiosensitises cancer cells
Inhibition of ATR is predicted to increase sensitivity to radiation (Wang et al, 2004; Hurley et al, 2007; Gilad et al, 2010; Peasland et al, 2011; Schoppy et al, 2012). We have determined whether the combination of VE-821 and radiation significantly increased cancer cell killing compared with radiation alone. We exposed a variety of cell lines from a number of tumour types to a range of radiation doses in the presence or absence of VE-821 (1 μℳ) (Figure 1). As loss of p53 has been demonstrated to be synthetic lethal with loss of ATR, we considered which of the cell lines used expressed wild-type vs mutant p53 (Ruzankina et al, 2009; Reaper et al, 2011). However, it should be noted that the presence of wild-type p53 does not guarantee functionality of the p53 response and we have not investigated this here. We observed that the presence of VE-821 induced a significant enhancement of radiation-induced clonogenic cell death in all the cancer cell lines shown. These results clearly show that VE-821 can increase sensitivity to radiation and that this effect is independent of tumour type.
Figure 1.
VE-821 radiosensitises various cell lines. RKO, HCT116, DLD1, SKmel28, IGR39, RCC4, HeLa, U2OS, SQ20B, MDA-MB-231, MDA-MB-468 and VmCub1 cells were treated with DMSO or 1 μℳ VE-821 for 6 h and then exposed to a range of radiation doses. Colonies were counted after 8–12 days. Cells with reported WT TP53 are indicated with ‡. Significance values: *P<0.05; **P<0.005; ***P<0.0005.
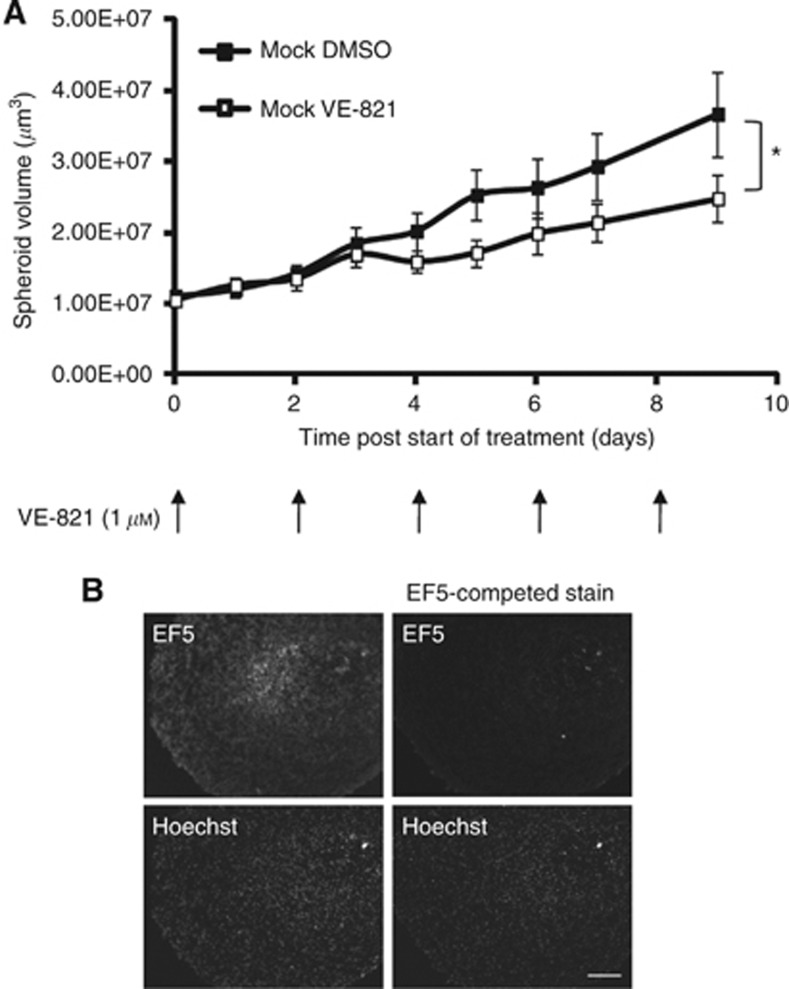
VE-821 inhibits the growth of cancer cells in 3D spheroid models
We have used 3D spheroid models to determine if VE-821 had a growth inhibitory effect in tumour models. The glioblastoma cell line, MG-U87 was chosen as it can be grown to form large spheroids. Media containing fresh VE-821 (1 μℳ) was replaced every other day and the average spheroid size measured over several days (Figure 2A). Treatment with VE-821 resulted in a significant decrease (P=0.0196) in the growth rate of the spheroids. Using EF5 as a hypoxia marker, we determined that the spheroids used in these experiments (Figure 2B) contained hypoxic regions (Koch, 2002). These data indicate that VE-821 can decrease the growth of tumour models and that potentially VE-821 affects the growth/viability of hypoxic cells. Because of the relevance of the presence of hypoxic regions for the treatment of most solid tumours, we investigated the effect of VE-821 treatment on cells exposed to a range of hypoxic conditions.
Figure 2.
VE-821 inhibits the growth of a 3D tumour model. Spheroids were grown from MG-U87 cells to average size of 400 μm and grown for further 9 days. (A) Spheroids were treated with either DMSO or 1 μℳ VE-821 and were replaced every 2 days for 9 days. The graph represents the average volume of at least 12 spheroids throughout treatment. (B) Before fixing, spheroids were treated with EF5. Spheroids were then fixed, sectioned and stained for EF5, demonstrating the presence of hypoxic regions within the spheroids. EF5 regular stain – ELK5-A8 antibody, EF5-competed stain – ELK5-A8+EF5. Significance values: *P<0.05.
VE-821 inhibits hypoxia-induced ATR signalling and induces DNA damage
The range of oxygen tensions within a tumour can vary from normal (8% O2) to moderate hypoxia (1–2% O2) to severe hypoxia/anoxia (⩽0.02%O2) (Brown, 2007). We have previously demonstrated that conditions of severe hypoxia induce replicative stress and an ATR/ATM-mediated DDR (Hammond et al, 2002). Therefore, we first investigated the effect of VE-821 in these conditions. Hypoxia-induced phosphorylation of Chk1, a known target of ATR, was significantly decreased in response to VE-821 (over 15-fold) (Figure 3A, quantification shown in Supplementary Figure S2). As described previously, the total levels of Chk1 decreased with exposure time to hypoxia (⩽0.02% O2) (Pires et al, 2010). Hypoxia-induced p53 phosphorylation at serine 15 was also decreased in response to VE-821, although to a lesser degree (two-fold). These observations confirm the inhibition of hypoxia-induced ATR activity by VE-821. In contrast, neither phosphorylation of Chk2 nor of ATM was affected by VE-821 supporting the previous findings that this compound does not inhibit ATM-mediated signalling. In fact, some phosphorylation events associated with ATM activity in hypoxia were increased (Bencokova et al, 2009; Pires et al, 2010). The levels of both KAP1-S824 and γH2AX were increased two-fold (Figure 3A, Supplementary Figure S2). The levels of DNA damage, measured by the appearance of 53BP1 foci, were determined in response to VE-821 treatment in hypoxic conditions (⩽0.02% O2) (Figure 3B). As previously reported, hypoxia alone did not induce an accumulation of nuclear 53BP1 foci (Bencokova et al, 2009). However, in the presence of VE-821, a significant level of DNA damage was detected in hypoxia. This is consistent with ATR protecting stalled replication forks in hypoxia (⩽0.02% O2). These data suggest that while ATR activity was inhibited by VE-821 in hypoxia, DNA damage was induced and potentially ATM activity was increased.
Figure 3.
VE-821 inhibits hypoxia-induced ATR-mediated signaling, while inducing DNA damage and affecting replication kinetics. (A) RKO cells were exposed to ⩽0.02% O2 for the times indicated in the presence of DMSO or 1 μℳ VE-821. Western blotting was carried out as indicated. Representative blots of n=3 experiments are shown. The levels of β-actin were determined to ensure equal loading. Quantification is shown in Supplementary Figure S2. (B) RKO cells were treated with DMSO or 1 μℳ VE-821 as shown. Norm-6 h; Hyp-6 h ⩽0.02% O2. The percentage of cells with more than six nuclear 53BP1 foci is shown. (C–F) VE-821 decreases replication fork progression and increases origin firing. RKO cells were treated with DMSO or 1 μℳ VE-821 and were treated as indicated, either in normoxia or ⩽0.02% O2 for 6 h and subsequently reoxygenated for 1 h. DNA fibres were then produced and scored. (C, D) The percentage of different replication structures is shown. (E, F) The distribution of the fork rates for the second label (IdU) for the on-going forks (average speeds are indicated). Significance values: *P<0.01, **P<0.001, ***P<0.0001.
VE-821 affects replication kinetics in normoxia and after reoxygenation
Depletion of ATR has been shown to affect replication rates and origin firing in normal unstressed conditions (Syljuasen et al, 2005). We have shown previously that inhibition of Chk1 during periods of severe hypoxia affects reoxygenation-induced replication restart (Pires et al, 2010). To investigate the role of ATR in normal replication and after reoxygenation-induced restart, RKO cells were treated with VE-821 and single-molecule DNA fibre analysis was carried out. In both normoxia and reoxygenation, the number of new origins fired was significantly increased in the presence of VE-821 (Figures 3C and D). This is in accordance with recent reports in which hypoxia-activated ATR represses unscheduled origin firing (Martin et al, 2011). In addition, ATR inhibition led to an overall decrease in the average speed of on-going forks in both normoxia and reoxygenation (Figure 3E and F). The effect of VE-821 on origin firing and fork speed in normoxia confirms the role of ATR in mediating unstressed replication. Importantly, the availability of a specific ATR inhibitor has allowed us to verify that these changes are likely a result of ATR signalling to Chk1 in these conditions (Pires et al, 2010).
Hypoxic tumour cells show increased sensitivity to VE-821
We have shown previously that impaired ATR expression sensitises cells to severe hypoxia and reoxygenation (Hammond et al, 2004). To expand on this finding, we have used VE-821 in a range of oxygen tensions and determined its effect on viability by colony survival assay. As expected, RKO cells exposed to ⩽0.02% O2 in the presence of VE-821 (1 μℳ) were significantly more sensitive to hypoxia/reoxygenation than DMSO-treated cells (Figure 4A). These effects were anticipated because these conditions are known to induce a replication arrest and are therefore supportive of a role for ATR in maintaining fork stability. DNA replication is however unaffected by exposure to the milder levels of hypoxia (Pires et al, 2010). Surprisingly, VE-821 also sensitised cells to moderate hypoxia (2% O2) and subsequent reoxygenation (Figure 4B). Moreover, cells exposed to hypoxia were more sensitive to VE-821 than those in normoxic (20% O2) conditions (Figure 4C, Supplementary Figure S3). In support of this finding, we observed that treatment of cells with VE-821 under moderate hypoxia increased the sub G1 population after reoxygenation suggesting that apoptosis had been induced (data not shown). We have demonstrated that loss of ATR activity through VE-821 treatment impacts replication in the absence of additional stress (Figure 3C and E). However, as replication rates are unaffected by exposure to moderate hypoxia (Pires and Hammond, unpublished), this affect of VE-821 is predicted to be the same in normoxic and hypoxic conditions. We hypothesised that the increased sensitivity to VE-821 seen in cells exposed to hypoxia/reoxygenation compared with normoxia might be a result of differences in DNA damage accumulation and repair. Therefore, we investigated the accumulation of DNA damage in response to VE-821 over the time periods used for the clonogenic survival assay. Prolonged exposure (24 h) to VE-821 in either normoxia or hypoxia (1% O2) led to an increase in DNA damage, as measured by the accumulation of 53BP1 foci (Figure 4D). These data indicate that prolonged exposure to VE-821 induces DNA damage in both normoxic and hypoxic conditions. However, there was a significant increase in reoxygenation-induced DNA damage in the cells exposed to VE-821 (Figure 4D). Moreover, we observed that addition of VE-821 immediately prior to reoxygenation decreased colony survival suggesting that the failure to repair reoxygenation-induced damage is significant (Supplementary Figure S4). Furthermore, we and others have shown that DNA repair pathways are repressed in a range of hypoxic conditions, leading to lower repair efficiencies (Bristow and Hill, 2008; Yoo et al, 2009; Chan et al, 2010). We propose that the repression of DNA repair by both hypoxia and ATR inhibition renders hypoxic cells more sensitive to DNA-damaging events, such as reoxygenation or cancer therapy.
Figure 4.
VE-821 sensitises cells to hypoxia. Clonogenic assays were carried out using RKO cells in the presence of DMSO or 1 μℳ VE-821. Cells were exposed to ⩽0.02% O2 (A) and 2% O2 (B) for the indicated time points and grown for 10 days. (C) Sensitisation of cells to 1 μℳ VE-821 vs DMSO after 24 h of exposure to various oxygen levels. (D) RKO cells were treated with DMSO or 1 μℳ VE-82 and exposed to 24 h normoxia (Norm), 24 h 1% O2 (Hyp) or 24 h 1% O2 and reoxygenated for 4 or 24 h (Reox 4 h) (Reox 24 h). Graph represents the percentage of cells with more than six 53BP1 foci. Significance values: *P<0.05; **P<0.005; ***P<0.0005.
VE-821 increases radiation-induced cell killing in physiologically relevant hypoxic conditions
As the efficacy of radiotherapy is compromised by tumour hypoxia and this is a major barrier to successful treatment, we evaluated the combination of radiation and VE-821 in a range of hypoxic conditions (Begg et al, 2011). RKO cells were exposed to a range of oxygen concentrations (0.5–2.0% O2) for 24 h in the presence of 1 μℳ VE-821 or DMSO before being irradiated at the doses indicated while still in hypoxic conditions. At 1 h after irradiation, the cells were returned to normal culture conditions to allow colonies to form. Significant increases in radiation-induced loss of viability was seen in response to VE-821 at 2% O2 (Figure 5A), 1% O2 (Figure 5B) and 0.5% O2 (Figure 5C). To gain some insight into the clinical benefits of ATR inhibition during radiotherapy, we again used the 3D spheroid model. Spheroids were grown as previously from the MG-U87 cell line and once grown irradiated (1 Gy) every day for 5 days. Media containing DMSO or 1 μℳ VE-821 was refreshed every 2 days through the duration of the experiment. The growth curves of the spheroids during and post treatments are shown (Figure 5D). The effect of VE-821 as a single agent was observed as noted previously (Figure 2A). Spheroids treated with radiation grew significantly slower (P=0.0089) than the mock treated. However, most importantly there was a significant decrease (P=0.0022) in growth in those irradiated in the presence of VE-821 compared with the DMSO control. These results indicate that VE-821 is an effective radiosensitiser in hypoxic conditions, as well as in in vitro tumour models. As shown previously, the spheroids contained hypoxic regions, demonstrated here by the presence of stabilised HIF-1α and increased GLUT-1 levels (Figure 5E). Interestingly, treatment with VE-821 reduced GLUT-1 levels suggesting the possibility that treatment with VE-821 had decreased HIF-1 activity.
Figure 5.
VE-821 is also a radiosensitiser in hypoxic conditions. RKO cells were treated with DMSO or 1 μℳ VE-821 and irradiated as indicated in the following oxygen tensions, 2% O2 (A), 1% O2 (B) or 0.5% O2 (C). Colony survival assays were carried out. The radiation response of RKO cells in normal O2 conditions (20% O2) is shown in Figure 1. (D) Spheroids were grown from MG-U87 cells as before and treated with combinations of DMSO or 1 μℳ VE-821 and mock per 1 Gy irradiation (RT) at the indicated times for 12 days. Average spheroid size is shown. Significance values: *P<0.05; **P<0.005; ***P<0.0005. (E) Western blots were carried out for HIF-1α, GLUT-1 and β-actin (loading control) on samples generated from spheroids at day 12 (lanes 3–6). Lanes 1–2 correspond to MG-U87 monolayer samples exposed to normoxia (Con) or 2% O2 for 30 min (Hyp).
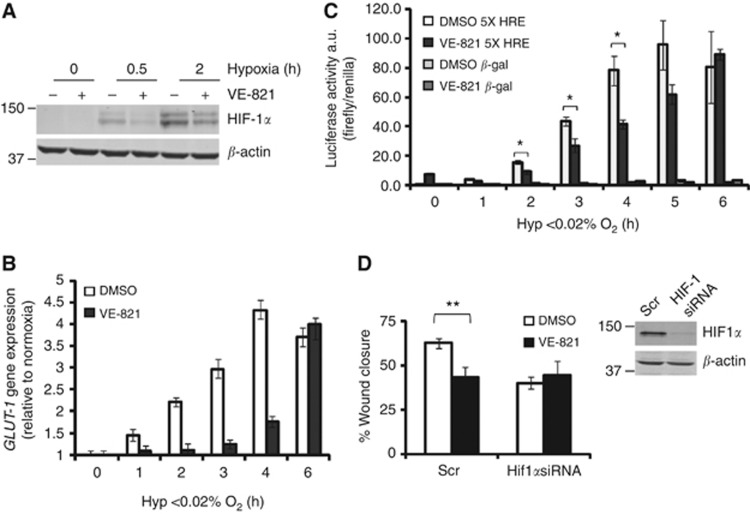
VE-821 transiently inhibits HIF-1 stabilisation and activity
It was demonstrated recently that in hypoxic conditions ATM phosphorylates HIF-1α (Cam et al, 2010). In agreement with this finding, we found that a specific ATM inhibitor reduced HIF-1α accumulation in hypoxia (2% O2) as well as induction of a well-characterised HIF-1 target, GLUT-1 (Supplementary Figure S5). As ATM and ATR share substrates, we hypothesised that ATR might also phosphorylate HIF-1α. RKO cells were exposed to ⩽0.02% O2 for up to 2 h with VE-821. Western blotting demonstrated that the levels of HIF-1α were significantly reduced in the presence of VE-821 (1.5 to 2-fold) (Figure 6A, Supplementary Figure S6A and B). The reduction of HIF-1α stabilisation in response to treatment with VE-821 was also noted during more prolonged periods of hypoxia up to 18 h (Supplementary Figure S6C). We hypothesised that the decreased HIF-1α levels in response to VE-821 would decrease transcriptional transactivation of target genes such as GLUT-1 (Cam et al, 2010). To address this, we measured GLUT-1 mRNA levels by qRT–PCR (Figure 6B) and also used a HIF-1 reporter system (Figure 6C). In both cases, the data indicate a decrease in HIF-1-mediated transcription in response to VE-821. Interestingly, the effects seen were most significant at early time points (up to 6 h). After longer exposures, there was no significant difference in HIF-1 activity with VE-821 (Supplementary Figure S6D). However, decreased levels of both GLUT-1 and LDH-A protein were observed in response to VE-821 in cells exposed up to 18 h of hypoxia (Supplementary Figure S6C). Next, we investigated whether HIF-1 inhibition by VE-821 had any significant effect on a hypoxia-mediated biological process. We used the scratch assay as a means of measuring wound closure in hypoxia. The highly motile cell line MDA-MB-231 was grown to near confluence, wounded and placed in hypoxic conditions (⩽0.02% O2). The degree of wound closure was significantly decreased in the presence of VE-821 (Figure 6D). Importantly, this effect was restricted to the hypoxic cells, as the inhibitor had no effect on the motility of cells in normoxia (Supplementary Figure S7). To clarify the role of HIF-1 in the mechanism by which VE-821 decreases cellular motility of hypoxic cells, we used siRNA to knock down HIF-1. As expected, HIF-1 knockdown alone lead to decreased motility in hypoxia (Figure 6D). However, this decrease was not affected by the presence of VE-821. These observations indicate that the inhibitory effect of VE-821 on hypoxic cell motility is dependent on HIF-1.
Figure 6.
VE-821 inhibits HIF-1 signalling. (A) RKO cells were exposed to ⩽0.02% O2 for the times indicated in the presence of DMSO or 1 μℳ VE-821. Western blotting was carried out for HIF-1α and β-actin (loading control). Representative blots of n=3 experiments are shown. (B) The levels of GLUT-1 mRNA were determined by qRT–PCR. 18S was used as the control. (C) RKO cells were transiently transfected with a HIF-1 reporter construct and exposed to hypoxia as indicated. The levels of luciferase relative to the renilla control are shown. (D) MDA-MB-231 cells were transfected with either Scr (scramble) or HIF-1 siRNA and scratch wound assays were carried out in the presence of DMSO or 1 μℳ VE-821. Western blot showing efficiency of knockdown is shown in inset. The graph represents the percentage of wound closure after 18 h exposure to hypoxia (⩽0.02% O2). Significance values: *P<0.05, **P<0.01.
Discussion
Our in vitro studies demonstrate that cancer cells are sensitised to hypoxia/reoxygenation by the highly specific ATR inhibitor, VE-821. As part of this study, we have also shown for the first time that inhibition of ATR leads to a decrease in HIF-1-mediated signalling. We propose that this is a result of decreased phosphorylation of HIF-1 by ATR, potentially on residue serine 696, although this remains to be formally proven (Cam et al, 2010). Our findings support recent studies demonstrating a clear overlap between the DDR and HIF signalling pathways (Cam et al, 2010; Bouquet et al, 2011). In addition to this link between the DDR and hypoxia-mediated signalling, ATR has recently been shown to have a role in hypoxia-induced angiogenesis. Economopoulou et al (2009) demonstrated that endothelial cells require ATR signalling to H2AX for efficient angiogenesis and that this is independent of HIF-1. We have restricted out studies to date to tumour cells rather than endothelial cells but hypothesise that VE-821 might have anti-angiogenic properties (Rankin et al, 2009). Here our own findings show that ATR inhibition had a transient effect on HIF-1 in vitro. The finding that both ATM and DNA-PK can phosphorylate HIF-1 likely explains this, especially as our data suggests that VE-821 increases hypoxia-induced ATM activation. Despite this, ATR inhibition by VE-821 did decrease cell motility in hypoxic conditions and that this effect was dependent on HIF-1. Inhibition of HIF-1 activity is an attractive therapeutic aspect to VE-821 activity, particularly as the compensation by ATM may be less relevant in tumours as ATM expression is frequently lost (Yu et al, 2004; Ye et al, 2007; Ding et al, 2008; Jiang et al, 2009; Cam et al, 2010). It is clear that the linking of two pathways so critical to tumour development and progression will have a significant impact on cancer therapy.
In general, radiotherapy is the most effective cancer therapy available. A caveat of this is the reduced efficacy of radiotherapy in hypoxic cancer cells (Sprong et al, 2006; Begg et al, 2011). This study clearly demonstrates the potential benefit of combining an ATR inhibitor with radiotherapy for effective targeting of cancer cells in physiological conditions. Significantly, we observed a positive effect of combining VE-821 and radiation over a range of oxygen concentrations, and not just under severe hypoxia (⩽0.02–2% O2). Given the previously described role of ATR in the response to hypoxia-induced replication arrest in severely hypoxic conditions, this was not surprising (Hammond et al, 2002; Hammond et al, 2004). However, we also found that cells exposed to moderate levels of hypoxia (0.5–2% O2) were more sensitive to VE-821 than those maintained in normal tissue culture conditions. Our data is consistent with the hypothesis that this is due to the induction of DNA damage by prolonged VE-821 treatment in a background of hypoxia-repressed DNA repair. This finding is highly significant as due to the challenges of delivering chemotherapeutics to the hypoxic regions of tumours an agent, which is effective against moderately hypoxic regions as well as the more severe areas, is optimal.
It is likely that ATR inhibitors will also be effective in combination with a number of other cancer therapies currently in development. Recently NU6027, a compound originally developed as a CDK2 inhibitor, was found to be a more potent inhibitor of ATR and was shown to sensitise cells to commonly used anticancer chemotherapeutics including temozolomide (Peasland et al, 2011). Using this inhibitor, Peasland et al (2011) were also able to demonstrate synthetic lethality when NU6027 was used in combination with a PARP inhibitor. This work further underscores the potential of ATR inhibitors as novel anticancer agents and suggests they will have particular value in targeting hypoxia-associated radioresistance.
Acknowledgments
A Cancer Research UK grant awarded to EMH (C6515/A9321) supported this work.
Footnotes
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
John R Pollard, Philip M Reaper and Peter A Charlton are full-time employees of Vertex Pharmaceuticals (Europe), Ltd and hold equity in Vertex Pharmaceuticals, Inc. W. Gillies McKenna is on the advisory board of Vertex Pharmaceuticals (Europe), Ltd.
Supplementary Material
References
- Agarwal R, Kaye SB (2003) Ovarian cancer: strategies for overcoming resistance to chemotherapy. Nat Rev Cancer 3: 502–516 [DOI] [PubMed] [Google Scholar]
- Begg AC, Stewart FA, Vens C (2011) Strategies to improve radiotherapy with targeted drugs. Nat Rev Cancer 11: 239–253 [DOI] [PubMed] [Google Scholar]
- Bencokova Z, Kaufmann MR, Pires IM, Lecane PS, Giaccia AJ, Hammond EM (2009) ATM activation and signaling under hypoxic conditions. Mol Cell Biol 29: 526–537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouquet F, Ousset M, Biard D, Fallone F, Dauvillier S, Frit P, Salles B, Muller C (2011) A DNA-dependent stress response involving DNA-PK occurs in hypoxic cells and contributes to cellular adaptation to hypoxia. J Cell Sci 124: 1943–1951 [DOI] [PubMed] [Google Scholar]
- Bristow RG, Hill RP (2008) Hypoxia and metabolism. Hypoxia, DNA repair and genetic instability. Nat Rev Cancer 8: 180–192 [DOI] [PubMed] [Google Scholar]
- Brown JM (2007) Tumor hypoxia in cancer therapy. Methods Enzymol 435: 297–321 [DOI] [PubMed] [Google Scholar]
- Cam H, Easton JB, High A, Houghton PJ (2010) mTORC1 signaling under hypoxic conditions is controlled by ATM-dependent phosphorylation of HIF-1alpha. Mol Cell 40: 509–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan N, Pires IM, Bencokova Z, Coackley C, Luoto KR, Bhogal N, Lakshman M, Gottipati P, Oliver FJ, Helleday T, Hammond EM, Bristow RG (2010) Contextual synthetic lethality of cancer cell kill based on the tumor microenvironment. Cancer Res 70: 8045–8054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charrier JD, Durrant SJ, Golec JM, Kay DP, Knegtel RM, Maccormick S, Mortimore M, O'Donnell ME, Pinder JL, Reaper PM, Rutherford AP, Wang PS, Young SC, Pollard JR (2011) Discovery of potent and selective inhibitors of Ataxia Telangiectasia Mutated and Rad3 related (ATR) protein kinase as potential anticancer agents. J Med Chem 54: 2320–2330 [DOI] [PubMed] [Google Scholar]
- Chitneni SK, Palmer GM, Zalutsky MR, Dewhirst MW (2011) Molecular imaging of hypoxia. J Nucl Med 52: 165–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimprich KA, Cortez D (2008) ATR: an essential regulator of genome integrity. Nat Rev Mol Cell Biol 9: 616–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cliby WA, Roberts CJ, Cimprich KA, Stringer CM, Lamb JR, Schreiber SL, Friend SH (1998) Overexpression of a kinase-inactive ATR protein causes sensitivity to DNA-damaging agents and defects in cell cycle checkpoints. Embo J 17: 159–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutts AS, Pires IM, Weston L, Buffa FM, Milani M, Li JL, Harris AL, Hammond EM, La Thangue NB (2011) Hypoxia-driven cell motility reflects the interplay between JMY and HIF-1alpha. Oncogene 30: 4835–4842 [DOI] [PubMed] [Google Scholar]
- Ding L, Getz G, Wheeler DA, Mardis ER, McLellan MD, Cibulskis K, Sougnez C, Greulich H, Muzny DM, Morgan MB, Fulton L, Fulton RS, Zhang Q, Wendl MC, Lawrence MS, Larson DE, Chen K, Dooling DJ, Sabo A, Hawes AC, Shen H, Jhangiani SN, Lewis LR, Hall O, Zhu Y, Mathew T, Ren Y, Yao J, Scherer SE, Clerc K, Metcalf GA, Ng B, Milosavljevic A, Gonzalez-Garay ML, Osborne JR, Meyer R, Shi X, Tang Y, Koboldt DC, Lin L, Abbott R, Miner TL, Pohl C, Fewell G, Haipek C, Schmidt H, Dunford-Shore BH, Kraja A, Crosby SD, Sawyer CS, Vickery T, Sander S, Robinson J, Winckler W, Baldwin J, Chirieac LR, Dutt A, Fennell T, Hanna M, Johnson BE, Onofrio RC, Thomas RK, Tonon G, Weir BA, Zhao X, Ziaugra L, Zody MC, Giordano T, Orringer MB, Roth JA, Spitz MR, Wistuba II, Ozenberger B, Good PJ, Chang AC, Beer DG, Watson MA, Ladanyi M, Broderick S, Yoshizawa A, Travis WD, Pao W, Province MA, Weinstock GM, Varmus HE, Gabriel SB, Lander ES, Gibbs RA, Meyerson M, Wilson RK (2008) Somatic mutations affect key pathways in lung adenocarcinoma. Nature 455: 1069–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economopoulou M, Langer HF, Celeste A, Orlova VV, Choi EY, Ma M, Vassilopoulos A, Callen E, Deng C, Bassing CH, Boehm M, Nussenzweig A, Chavakis T (2009) Histone H2 AX is integral to hypoxia-driven neovascularization. Nat Med 15: 553–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einhorn LH (2002) Curing metastatic testicular cancer. Proc Natl Acad Sci USA 99: 4592–4595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilad O, Nabet BY, Ragland RL, Schoppy DW, Smith KD, Durham AC, Brown EJ (2010) Combining ATR suppression with oncogenic Ras synergistically increases genomic instability, causing synthetic lethality or tumorigenesis in a dosage-dependent manner. Cancer Res 70: 9693–9702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover TW, Arlt MF, Casper AM, Durkin SG (2005) Mechanisms of common fragile site instability. Hum Mol Genet 14 Spec No 2: R197–R205 [DOI] [PubMed] [Google Scholar]
- Graeber TG, Osmanian C, Jacks T, Housman DE, Koch CJ, Lowe SW, Giaccia AJ (1996) Hypoxia-mediated selection of cells with diminished apoptotic potential in solid tumours. Nature 379: 88–91 [DOI] [PubMed] [Google Scholar]
- Hammond EM, Denko NC, Dorie MJ, Abraham RT, Giaccia AJ (2002) Hypoxia links ATR and p53 through replication arrest. Mol Cell Biol 22: 1834–1843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond EM, Dorie MJ, Giaccia AJ (2004) Inhibition of ATR leads to increased sensitivity to hypoxia/reoxygenation. Cancer Res 64: 6556–6562 [DOI] [PubMed] [Google Scholar]
- Hammond EM, Mandell DJ, Salim A, Krieg AJ, Johnson TM, Shirazi HA, Attardi LD, Giaccia AJ (2006) Genome-wide analysis of p53 under hypoxic conditions. Mol Cell Biol 26: 3492–3504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hockel M, Knoop C, Schlenger K, Vorndran B, Baussmann E, Mitze M, Knapstein PG, Vaupel P (1993) Intratumoral pO2 predicts survival in advanced cancer of the uterine cervix. Radiother Oncol 26: 45–50 [DOI] [PubMed] [Google Scholar]
- Hurley PJ, Wilsker D, Bunz F (2007) Human cancer cells require ATR for cell cycle progression following exposure to ionizing radiation. Oncogene 26: 2535–2542 [DOI] [PubMed] [Google Scholar]
- Jackson SP, Bartek J (2009) The DNA-damage response in human biology and disease. Nature 461: 1071–1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H, Reinhardt HC, Bartkova J, Tommiska J, Blomqvist C, Nevanlinna H, Bartek J, Yaffe MB, Hemann MT (2009) The combined status of ATM and p53 link tumor development with therapeutic response. Genes Dev 23: 1895–1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastan MB, Bartek J (2004) Cell-cycle checkpoints and cancer. Nature 432: 316–323 [DOI] [PubMed] [Google Scholar]
- Koch CJ (2002) Measurement of absolute oxygen levels in cells and tissues using oxygen sensors and 2-nitroimidazole EF5. Methods Enzymol 352: 3–31 [DOI] [PubMed] [Google Scholar]
- Martin L, Rainey M, Santocanale C, Gardner LB (2011) Hypoxic activation of ATR and the suppression of the initiation of DNA replication through cdc6 degradation. Oncogene e-pub ahead of print 19 December 2011 doi: 10.1038/onc.2011.585 [DOI] [PMC free article] [PubMed]
- Melillo G (2007) Targeting hypoxia cell signaling for cancer therapy. Cancer Metastasis Rev 26: 341–352 [DOI] [PubMed] [Google Scholar]
- Nasim A, Smith BP (1975) Genetic control of radiation sensitivity in Schizosaccharomyces pombe. Genetics 79: 573–582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nghiem P, Park PK, Kim Y, Vaziri C, Schreiber SL (2001) ATR inhibition selectively sensitizes G1 checkpoint-deficient cells to lethal premature chromatin condensation. Proc Natl Acad Sci USA 98: 9092–9097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishida H, Tatewaki N, Nakajima Y, Magara T, Ko KM, Hamamori Y, Konishi T (2009) Inhibition of ATR protein kinase activity by schisandrin B in DNA damage response. Nucleic Acids Res 37: 5678–5689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olcina M, Lecane PS, Hammond EM (2010) Targeting hypoxic cells through the DNA damage response. Clin Cancer Res 16: 5624–5629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onnis B, Rapisarda A, Melillo G (2009) Development of HIF-1 inhibitors for cancer therapy. J Cell Mol Med 13: 2780–2786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peasland A, Wang LZ, Rowling E, Kyle S, Chen T, Hopkins A, Cliby WA, Sarkaria J, Beale G, Edmondson RJ, Curtin NJ (2011) Identification and evaluation of a potent novel ATR inhibitor, NU6027, in breast and ovarian cancer cell lines. Br J Cancer 105: 372–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pires IM, Bencokova Z, Milani M, Folkes LK, Li JL, Stratford MR, Harris AL, Hammond EM (2010) Effects of acute versus chronic hypoxia on DNA damage responses and genomic instability. Cancer Res 70: 925–935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qayum N, Muschel RJ, Im JH, Balathasan L, Koch CJ, Patel S, McKenna WG, Bernhard EJ (2009) Tumor vascular changes mediated by inhibition of oncogenic signaling. Cancer Res 69: 6347–6354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rankin EB, Giaccia AJ, Hammond EM (2009) Bringing H2AX into the angiogenesis family. Cancer Cell 15: 459–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaper PM, Griffiths MR, Long JM, Charrier JD, Maccormick S, Charlton PA, Golec JM, Pollard JR (2011) Selective killing of ATM- or p53-deficient cancer cells through inhibition of ATR. Nat Chem Biol 13: 428–430 [DOI] [PubMed] [Google Scholar]
- Ruzankina Y, Schoppy DW, Asare A, Clark CE, Vonderheide RH, Brown EJ (2009) Tissue regenerative delays and synthetic lethality in adult mice after combined deletion of Atr and Trp53. Nat Genet 41: 1144–1149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoppy DW, Ragland RL, Gilad O, Shastri N, Peters AA, Murga M, Fernandez-Capetillo O, Diehl JA, Brown EJ (2012) Oncogenic stress sensitizes murine cancers to hypomorphic suppression of ATR. J Clin Invest 122: 241–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sogo JM, Lopes M, Foiani M (2002) Fork reversal and ssDNA accumulation at stalled replication forks owing to checkpoint defects. Science 297: 599–602 [DOI] [PubMed] [Google Scholar]
- Sprong D, Janssen HL, Vens C, Begg AC (2006) Resistance of hypoxic cells to ionizing radiation is influenced by homologous recombination status. Int J Radiat Oncol Biol Phys 64: 562–572 [DOI] [PubMed] [Google Scholar]
- Syljuasen RG, Sorensen CS, Hansen LT, Fugger K, Lundin C, Johansson F, Helleday T, Sehested M, Lukas J, Bartek J (2005) Inhibition of human Chk1 causes increased initiation of DNA replication, phosphorylation of ATR targets, and DNA breakage. Mol Cell Biol 25: 3553–3562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Powell SN, Iliakis G, Wang Y (2004) ATR affecting cell radiosensitivity is dependent on homologous recombination repair but independent of nonhomologous end joining. Cancer Res 64: 7139–7143 [DOI] [PubMed] [Google Scholar]
- Wilsker D, Bunz F (2007) Loss of ataxia telangiectasia mutated- and Rad3-related function potentiates the effects of chemotherapeutic drugs on cancer cell survival. Mol Cancer Ther 6: 1406–1413 [DOI] [PubMed] [Google Scholar]
- Wilsker D, Petermann E, Helleday T, Bunz F (2008) Essential function of Chk1 can be uncoupled from DNA damage checkpoint and replication control. Proc Natl Acad Sci USA 105: 20752–20757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods ML, Koch CJ, Lord EM (1996) Detection of individual hypoxic cells in multicellular spheroids by flow cytometry using the 2-nitroimidazole, EF5, and monoclonal antibodies. Int J Radiat Oncol Biol Phys 34: 93–101 [DOI] [PubMed] [Google Scholar]
- Yasui H, Matsumoto S, Devasahayam N, Munasinghe JP, Choudhuri R, Saito K, Subramanian S, Mitchell JB, Krishna MC (2010) Low-field magnetic resonance imaging to visualize chronic and cycling hypoxia in tumor-bearing mice. Cancer Res 70: 6427–6436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye C, Cai Q, Dai Q, Shu XO, Shin A, Gao YT, Zheng W (2007) Expression patterns of the ATM gene in mammary tissues and their associations with breast cancer survival. Cancer 109: 1729–1735 [DOI] [PubMed] [Google Scholar]
- Yoo YG, Hayashi M, Christensen J, Huang LE (2009) An essential role of the HIF-1alpha-c-Myc axis in malignant progression. Ann N Y Acad Sci 1177: 198–204 [DOI] [PubMed] [Google Scholar]
- Yu G, Zhu MH, Zhu Z, Ni CR, Zheng JM, Li FM (2004) Expression of ATM protein and its relationship with p53 in pancreatic carcinoma with tissue array. Pancreas 28: 421–426 [DOI] [PubMed] [Google Scholar]
- Zou L, Elledge SJ (2003) Sensing DNA damage through ATRIP recognition of RPA-ssDNA complexes. Science 300: 1542–1548 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.