Abstract
Background:
The understanding of metastatic patterns after metachronous contralateral breast cancer (CBC) may help determine the biological nature of CBC.
Methods:
A cohort of 8478 women with breast cancer treated at Guy’s and St Thomas’ NHS Foundation Trust between 1975 and 2006 were studied. Organ-specific 5-year cumulative incidence and incidence rate ratios were assessed for women diagnosed with unilateral breast cancer (UBC), CBC within 5 years and CBC more than 5 years of the initial diagnosis.
Results:
Women diagnosed with CBC within 5 years had a higher incidence of metastases in all organs compared with UBC. Women with a short interval time to CBC developed metastasis more rapidly and were more likely to develop visceral and distant cutaneous metastases compared with bone metastasis.
Conclusion:
These findings explain poor prognosis of women with early occurring CBC and suggest that some of these CBCs are indicators of aggressive and/or systemic disease.
Keywords: metachronous cancer, contralateral breast cancer, patterns of metastasis
Women with visceral metastases following breast cancer have a poorer prognosis than those with bony lesions (Solomayer et al, 2000; Howell et al, 2003). Although bone is the most frequently affected site after a primary breast cancer (DeVita et al, 2008), little is known regarding the organ-preferential metastasis after metachronous contralateral breast cancer (CBC).
Recently, we found that women who develop CBC within 5 years are at an increased risk of dying from breast cancer (Vichapat et al, 2011a). We therefore hypothesised that some CBCs, occurring early, indicate the presence of systemic disease and potentially a preference for visceral metastatic pathways. To elucidate these findings, we compared the patterns of metastasis in women diagnosed with CBC within and after 5 years with those in women with unilateral breast cancer (UBC).
Patients and Methods
Patients
We identified 8478 women treated for an invasive primary breast cancer at Guy’s and St Thomas’ NHS Foundation Trust between 1975 and 2006. We used a 6-month interval to distinguish metachronous from synchronous CBC (Schwentner et al, 2012).
We excluded: 5 women who underwent contralateral prophylactic mastectomy, 20 with synchronous CBC, 205 who contributed less than 6 months of follow-up, 22 with metastasis at the time of CBC diagnosis and 400 with metastasis at the time of initial diagnosis. To allow for equal time at risk of developing metastasis, we excluded 127 women lost to follow-up and 105 who developed distant metastasis within 6 months of the initial breast cancer, leaving 7594 eligible women, of whom 305 developed metachronous CBC.
Our outcome of interest was distant metastasis. Distant metastases were defined as any lesion located outside the breast tissue, mastectomy scar, ipsilateral axillary lymph nodes or ipsilateral supraclavicular lymph nodes. Sites of metastasis were grouped as: bone; visceral (lesions in thoracic or abdominal viscera); central nervous system; distant cutaneous; distant lymph nodes; multiple organs (metastases diagnosed at two or more sites within 6 months after the first distant metastasis); and unknown site. The study has the approval of the Guy's NHS Research Ethics Committee.
Statistical analysis
Five-year cumulative incidence was calculated for each metastatic site. P-values were estimated using Gray’s test. Incidence rate ratios (IRR) were computed via percentile bootstrap estimates. The probability curves for visceral or distant cutaneous metastases were estimated using competing risk regression using interval time to CBC as an explanatory variable in a linear model and in a nonlinear model.
Results
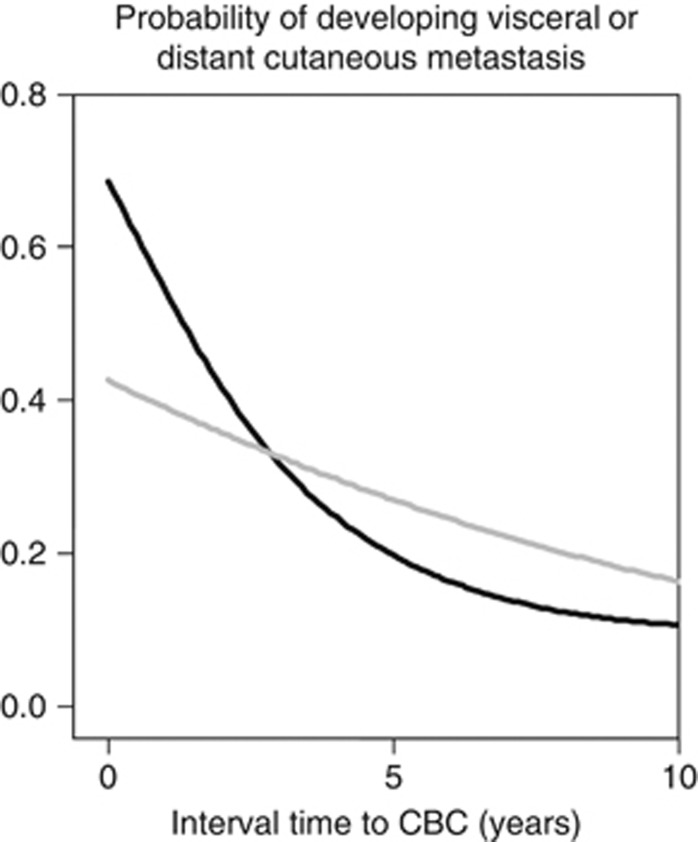
Figure 1 shows the 5-year cumulative incidence curves for each metastatic site. Lymph node involvement at the contralateral axilla was considered as a distant lymph node metastasis for women with UBC and a local recurrence for women with CBC, therefore no women with CBC were classified in this category.
Figure 1.
Cumulative incidence curves, the corresponding 5-year cumulative incidence estimates and the IRRs of organ-specific metastasis including bone, visceral organs, central nervous system, distant cutaneous, distant lymph node, multiple organs, unknown sites, women with a record of breast cancer death without report on distant metastasis and women who died from other causes for women with UBC (A), women with metachronous CBC within 5 years (B) and women with metachronous CBC after 5 years of the initial breast cancer (C).
The cumulative incidence of metastases for women diagnosed with CBC within 5 years rose steeply after diagnosis (Figure 1, panel B). Compared with women with UBC, visceral and cutaneous metastases occurred more often in women with CBC within 5 years as shown in panels A and B (P<0.001 for both sites). The slope and the site-specific cumulative incidence curves were similar between women with UBC and women with CBC more than 5 years after the initial cancer (Figure 1, panels A and C).
Compared with women with UBC and women with CBC more than 5 years after the initial diagnosis, women with CBC within 5 years had higher IRRs for visceral and cutaneous metastasis than for bone metastasis (for example, IRR 2.1 and 1.5, respectively, compared with 1.3 and 0.16 for women with UBC; Figure 1, panels A, B and C).
Five-year cumulative incidence of metastases was lower in women with UBC who received tamoxifen for the initial tumour (24% vs 33%, P<0.001). In women with CBC, tamoxifen treatment for the initial tumour was not associated with metastasis after CBC (54% vs 58% for women with CBC within 5 years and 26% vs 23% for women with CBC after 5 years, who received and did not receive tamoxifen, respectively). Metastatic occurrence in women with CBC with an initial cancer diagnosis after 1990 was lower than that of those diagnosed before 1990 but not statistically significantly different (45% vs 61%, P=0.07 for women with CBC within 5 years). Period of initial diagnosis was not associated with metastatic occurrence in women with CBC after more than 5 years.
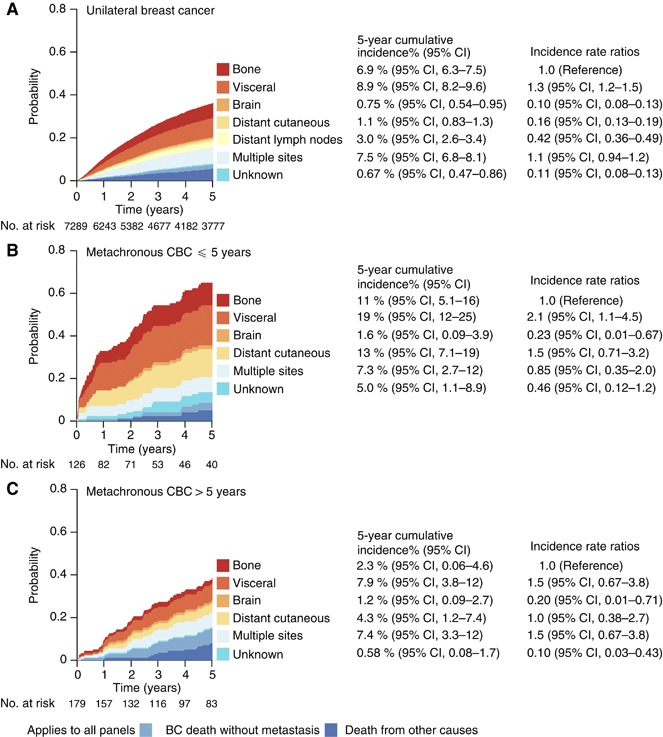
Figure 2 illustrates the probabilities of developing visceral or distant cutaneous metastasis after CBC against interval time to CBC. Under both assumptions of linearity and nonlinearity, the probability was high immediately after the CBC diagnosis and gradually decreased with a longer interval time.
Figure 2.
Five-year probabilities of developing visceral or distant cutaneous metastasis after the diagnosis of CBC are plotted against interval time to CBC. The gray curve shows the probability estimated from a competing risk regression, based on a linear relationship between the probability and the interval time. The black curve shows the probability using a cubic spline relationship with three knots.
Discussion
Women diagnosed with CBC within 5 years more commonly presented with metastasis to visceral organs and distant cutaneous sites, compared with women with UBC. A steep increase in cumulative incidence curves for women with CBC within 5 years indicates a rapid disease progression. Women diagnosed with CBC more than 5 years after the initial breast cancer had patterns of metastatic spread similar to women with UBC.
The similar incidence and patterns of metastasis in women with UBC and those with CBC diagnosed after more than 5 years, suggests that the tumour biology of these tumours is similar. In contrast, the rapid occurrence of metastases among women diagnosed with CBC within 5 years of their primary cancer and the predilection for visceral and distant cutaneous metastasis supports our previous findings of poor prognosis among women diagnosed with CBC soon after the initial breast cancer (Vichapat et al, 2011a, 2011b). We do not have access to detailed morphological data or molecular profiles of the two cancers, and therefore we cannot distinguish a new primary CBC from a metastatic lesion. Studies investigating the clonal relationship between primary breast cancer and CBC reported evidence of metastatic CBC, although this was rarer than a new primary CBC (Janschek et al, 2001; Teixeira et al, 2004).
We limited the study to the first metastatic occurrence because any subsequent metastases may be underreported when patients reach palliative care. During the period of this study, metastatic sites were diagnosed primarily using different types of imaging and very occasionally histopathology. Information on metastasis was available in more than 90% of women dying from breast cancer. Owing to the possible underreporting of metastases, we separately reported on women who died of breast cancer without a record of metastasis. Site of metastasis was not reported in 1% of all women and in 5% of women diagnosed with CBC within 5 years.
Tamoxifen treatment reduces the risk of developing CBC (Chen et al, 1999) but the treatment of the initial breast cancer was not associated with the incidence of metastasis after CBC. The trend for a lower incidence of metastases after 1990 may reflect the improvements in diagnosis and treatment.
Conclusion
Our data indicate that a significant proportion of CBCs occurring shortly after the initial cancer may represent or indicate active systemic disease. Further experimental studies are warranted for verifying CBC’s biological nature. The rapidly rising high incidence of visceral and cutaneous metastases in women with a short interval to CBC raises questions about clinical management of women in this situation.
Acknowledgments
We acknowledge the financial support from Cancer Research UK and the Royal Thai Government. The research was supported by the National Institute for Research (NIHR) Biomedical Research Centre based at Guy's and St Thomas' NHS Foundation Trust and King's College London.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
The authors declare no conflict of interest.
References
- Chen Y, Thompson W, Semenciw R, Mao Y (1999) Epidemiology of contralateral breast cancer. Cancer Epidem Biomar 8(10): 855–861 [PubMed] [Google Scholar]
- DeVita VT, Lawrence TS, Rosenberg SA (2008) DeVita, Hellman, and Rosenberg's Cancer: Principles & Practice of Oncology, 8th edn. Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia [Google Scholar]
- Howell A, Robertson JF, Vergote I (2003) A review of the efficacy of anastrozole in postmenopausal women with advanced breast cancer with visceral metastases. Breast Cancer Res Treat 82(3): 215–222 [DOI] [PubMed] [Google Scholar]
- Janschek E, Kandioler-Eckersberger D, Ludwig C, Kappel S, Wolf B, Taucher S, Rudas M, Gnant M, Jakesz R (2001) Contralateral breast cancer: molecular differentiation between metastasis and second primary cancer. Breast Cancer Res Treat 67(1): 1–8 [DOI] [PubMed] [Google Scholar]
- Schwentner L, Wolters R, Wischnewsky M, Kreienberg R, Wockel A (2012) Survival of patients with bilateral versus unilateral breast cancer and impact of guideline adherent adjuvant treatment: a multi-centre cohort study of 5292 patients. Breast 21(2): 171–177 [DOI] [PubMed] [Google Scholar]
- Solomayer EF, Diel IJ, Meyberg GC, Gollan C, Bastert G (2000) Metastatic breast cancer: clinical course, prognosis and therapy related to the first site of metastasis. Breast Cancer Res Treat 59(3): 271–278 [DOI] [PubMed] [Google Scholar]
- Teixeira MR, Ribeiro FR, Torres L, Pandis N, Andersen JA, Lothe RA, Heim S (2004) Assessment of clonal relationships in ipsilateral and bilateral multiple breast carcinomas by comparative genomic hybridisation and hierarchical clustering analysis. Br J Cancer 91(4): 775–782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vichapat V, Garmo H, Holmberg L, Fentiman IS, Tutt A, Gillett C, Luchtenborg M (2011a) Prognosis of metachronous contralateral breast cancer: importance of stage, age and interval time between the two diagnoses. Breast Cancer Res Treat 130(2): 609–618 [DOI] [PubMed] [Google Scholar]
- Vichapat V, Gillett C, Fentiman IS, Tutt A, Holmberg L, Luchtenborg M (2011b) Risk factors for metachronous contralateral breast cancer suggest two aetiological pathways. Eur J Cancer 47(13): 1919–1927 [DOI] [PubMed] [Google Scholar]