Abstract
Purpose
To compare drivers and non-drivers, and describe the specific concerns of drivers, among individuals with glaucoma.
Methods
607 newly-diagnosed glaucoma patients from 14 clinical centers of the Collaborative Initial Glaucoma Treatment Study were randomly assigned to initial medicine or surgery and followed every six months for < 5 years. Driving status (drivers vs. non-drivers) as well as patient-reported visual function was determined by the Visual Activities Questionnaire and the National Eye Institute Visual Function Questionnaire. Clinical evaluation included visual field mean deviation (MD) and visual acuity. Statistical comparisons were made using t, Chi-square, and exact tests, regression, and Rasch analyses.
Results
Drivers were more likely than non-drivers to be male, white, married, employed, and have more education, higher income, and fewer co-morbidities. Over 50% of drivers reported at least “some” difficulty performing tasks involving glare, whereas 22% reported at least “some” difficulty with tasks requiring peripheral vision. At 54 months, drivers with moderate/severe bilateral visual field loss (VFL) reported greater difficulty with night driving and tasks involving visual search and visual processing speed than drivers with less bilateral VFL (all p-values <0.05). While those who remained drivers over follow-up had better MD in both eyes than those who became non-drivers due to eyesight, a number of drivers had marked VFL.
Conclusion
Inquiring about specific difficulties with tasks related to glare, visual processing speed, visual search and peripheral vision in driving, especially among patients with substantial bilateral VF damage, will enable physicians to more effectively counsel patients regarding driving.
Introduction
Individuals with glaucoma rate driving as very important in preserving independence. The two most important concerns identified by glaucoma patients in a recent study were the risks of visual field (VF) loss leading to an inability to drive, and the fear of long-term blindness.1 Ang and Eke2 found that while most glaucoma patients in their study retained useful vision, almost half (47%) eventually lost vision resulting in driving ineligibility.
Several previous studies found that glaucoma is an important risk factor for motor vehicle accidents,3–6 particularly among the elderly.3–5 While visual acuity is only weakly related to crash involvement, peripheral vision may play a more critical role.7 The combination of impaired visual processing and glaucoma may play a role in the etiology of older driver crashes that result in injuries.5 Finally, Szlyk et al.8 found a higher incidence of real-world and simulator accidents among individuals with glaucoma compared to controls.
Less well studied among glaucoma patients is the difficulty performing specific tasks related to safe driving. Bowers et al.9 in a small sample of 28 drivers found that those with worse VFs showed significantly poorer scores for changing lanes, driving around curves, and anticipatory skills. In a study of on-road driving performance, those with glaucoma were six times as likely to have difficulty detecting peripheral hazards and reacting to unexpected eventsas those with normal vision.6 Glaucoma patients also report more difficulty driving at night than during the day,10 and more difficulty driving at any time than a normally-sighted control group.11
Current research has considered the impact of bilateral VF status on quality of life (QOL), including driving concerns.12–15 McKean-Cowdin et al.14 found that bilateral VF loss had the greatest impact on QOL, with driving difficulties among the subscales that showed the greatest differences dependent on degree of unilateral and bilateral VF loss. In a separate paper that employed a binocular VF summation score, the same authors reported that individuals with glaucomatous VF loss had greater difficulties with driving activities; the majority of these persons were unaware of their glaucoma diagnosis.15 Finally, Freeman et al.13 found that individuals with bilateral glaucoma were more likely to report difficulties with night driving than those with unilateral and/or no glaucoma.
This study investigated four questions using data from the Collaborative Initial Glaucoma Treatment Study (CIGTS): (1) How do drivers differ from non-drivers? (2) How much difficulty do drivers report for specific visual tasks related to driving? (3) How does reported difficulty with driving tasks differ depending on bilateral clinical visual status? and, (4) Are drivers who become non-drivers over time different from those who remain drivers?
Methods
Sample and Procedures
The study protocol, eligibility criteria, and recruitment procedures have been described.16 In brief, 607 subjects were enrolled in the CIGTS between October, 1993 and April, 1997. Participants were newly diagnosed, open-angle glaucoma patients from 14 clinical centers across the United States. Eligible participants were between 25 and 75 years of age and agreed to be followed for a minimum of five years, with re-consent obtained for additional follow-up. The CIGTS protocol and informed consent were approved by Institutional Review Boards at the University of Michigan and at all clinical sites. Upon giving written informed consent, patients were randomized to initial trabeculectomy (n=300) or initial medical therapy (n=307). For more specifics on the treatment course see Lichter et al.17
Enrollment, Evaluation, and Follow-up
Prior to randomization, subjects received a comprehensive ophthalmologic examination and baseline telephone QOL interview. Information on participants’ age, race, and gender was obtained at the clinic site, while education and income level, marital status, employment status, and number of non-ocular co-morbidities (0–13) were collected during the QOL interview. Standardized follow-up ophthalmologic examinations and QOL interviews were conducted every 6 months following initial treatment. The CIGTS QOL interviews were administered from a centralized interviewing facility by trained telephone interviewers.
QOL Measures
The QOL protocol included both generic and condition-specific measures, and has been described in detail.18 The CIGTS utilized the Visual Activities Questionnaire (VAQ)19 and National Eye Institute Visual Function Questionnaire (NEI-VFQ)20 to assess patients’ perceptions of their visual functioning and the impact of visual problems on their daily activities, including driving. Both measures have established reliability and validity. 19,20 When the trial began, the 33-item VAQ was deemed to be the most relevant condition-specific measure of functional status available. Five years later, the NEI developed and released a measure of functional status, the 51-item VFQ 21 and, later, a 25-item version.20 The latter was added to the CIGTS QOL protocol in 1998.
The VAQ asks about problems individuals may have performing everyday tasks that involve visual function. Each item describes a vision problem and asks how often this problem occurs on a five-point scale from 1 (never) to 5 (always), or “not applicable.” The VAQ includes eight subscales: color discrimination, glare disability, light-dark adaptation, acuity/spatial vision, depth perception, peripheral vision, visual search, and visual processing speed. The VAQ total score and subscale scores were calculated as a mean of all items, or the items in that subscale, respectively. Higher scores indicate worse visual functioning. Five items across four different subscales (glare disability, peripheral vision, visual search, and visual processing speed) specifically refer to problems when driving. Three of the items relate to driving in general, and two are particular to night driving. The VAQ was administered at every interviewing time-point.
The NEI-VFQ was first administered at the 54-month follow-up and annually thereafter. The measure includes three questions focused on: current driving status, degree of difficulty driving during the day and at night, and among non-drivers, reasons for stopping.
Defining drivers and non-drivers
Current driving status was assessed every 6 months over the course of the CIGTS study. From 6 months to 48 months, drivers were defined as individuals who endorsed any of the five driving-related items of the VAQ. Beginning at 54 months, with the availability of the NEI-VFQ, we were able to: (1) define drivers by their response to a specific item about current driving status, and, (2) determine among those who became non-drivers, whether the reason was due to their eyesight or other causes.
Clinical measures
Every six months patients received a comprehensive ophthalmologic examination including automated perimetry with the Humphrey 24-2 full threshold VF testing protocol. The VF test’s mean deviation (MD) provides an overall measure of VF loss in each eye. Best corrected visual acuity (VA) was measured bilaterally using a modification of the Early Treatment Diabetic Retinopathy Study protocol, with scores at baseline ranging between 70 and 100 (i.e., 20/40 or better).16
Data Analyses
In brief, we examined patient reported vision function and clinical characteristics in a large group of patients with newly diagnosed glaucoma. Cross sectional analyses were conducted at 6 months post diagnosis and longitudinal analysis over 54 months in relation to driving status.
The first QOL questionnaire was completed just after the glaucoma diagnosis was made. To avoid the influence of recency of diagnosis or anticipation of treatment, we used six month clinical and QOL findings as a reference for comparison with subsequent values over follow-up. By six months almost all CIGTS patients had completed their initial treatment course.
Demographic comparisons of drivers to non-drivers were made using chi-square tests. Comparisons of clinical variables and patient-reported visual function (VAQ measure) at 6 and 54 months between drivers and non-drivers were made with two sample t-tests. Linear regression was used to compare drivers and non-drivers on these same outcomes while adjusting for sex, race, education, employment, income and number of co-morbidities. Next, Rasch analyses were performed on the five VAQ driving items using WINSTEPS software v3.66.0 (Winsteps, Chicago, IL).
Comparisons between 6 month and follow-up measures of MD in better and worse eyes were made using paired t-tests among subjects who were drivers at 6 months. VF change from 6 to 54 months was compared using two-sample t-tests in patients who remained drivers versus those who became non-drivers during this time.
The MD at the 54 month follow-up was used to characterize patients into three categories similar to those used by McKean-Cowdin et al.14
No bilateral VF damage and/or mild unilateral damage (No Bi) = either (a) both eyes with MD > −2 dB or (b) better eye MD > −2 dB and [−6 dB ≤ worse eye MD ≤ −2 dB]
Mild bilateral VF damage and/or moderate/severe unilateral damage (Mild Bi) = either (a) worse eye MD < −6 dB and better eye MD > −2 dB, or (b) both eyes with −6 dB ≤ MD ≤ −2 dB, or (c) worse eye MD < −6 dB and [−6 dB ≤ better eye MD ≤ −2 dB]
Moderate/severe bilateral damage (ModSev Bi) = both eyes MD < −6 dB.
Comparisons among these categories of VF damage were made using chi-square tests and extended Fisher’s exact tests for categorical variables. These analyses were performed using SAS® statistical software version 9.1 (SAS Institute Inc., Carey, NC).
Results
Table 1 displays sociodemographic differences between 471 drivers and 84 non-drivers who completed the 6 month follow-up. Significant differences (p <0.001) between drivers and non-drivers were found for sex, race, education, employment, income and marital status. Specifically, 60% of drivers were male compared to 27% of non-drivers. Most drivers were White (65%), whereas most non-drivers were Black (62%). Education past high school was reported by 57% of drivers but only 26% of non-drivers. More drivers vs. non-drivers were employed full time (53% vs. 23%), or had income in excess of $40,000 (44% vs. 6%). Most drivers (66%) but only 30% of non-drivers were married. Drivers reported significantly fewer co-morbidities (p<0.001). No significant association was found between driving status and age (p=0.087) or living alone (p=0.130). At six months, the distribution of initial treatment (medicine or surgery) did not differ significantly between drivers and non-drivers (p = 0.409). At 54 months, those who dropped out of the study compared to those who remained did not differ by age, sex, race, education, employment status, marital status, number of co-morbidities or baseline VF mean deviation, but drop-outs were significantly more likely to have less income and worse visual acuity. There were no significant differences between study participants and dropouts based on driving status at baseline.
Table 1.
Characteristics between drivers and non-drivers at 6 month follow-up
| 6 months | |||
|---|---|---|---|
|
| |||
| Categorical variable* | Driver (n=471) | Non-driver (n=84) | P-value† |
| Freq (%) | Freq (%) | ||
| Age | |||
| 25–49 years | 119 (25.3) | 12 (14.3) | |
| 50–64 years | 198 (42.0) | 42 (50.0) | 0.087 |
| 65–74 years | 149 (31.6) | 28 (33.3) | |
| Sex | |||
| Male | 283 (60.1) | 23 (27.4) | |
| Female | 188 (39.9) | 61 (72.6) | <0.001 |
| Race | |||
| White | 307 (65.2) | 21 (25.0) | |
| Black | 144 (30.6) | 52 (61.9) | <0.001 |
| Asian & Other | 20 (4.3) | 11 (13.1) | |
| Education | |||
| <High School | 71 (15.1) | 44 (52.4) | |
| High School | 134 (28.5) | 18 (21.4) | <0.001 |
| >High School | 266 (56.5) | 22 (26.2) | |
| Employment | |||
| Employed (Full/Part time) | 246 (52.9) | 19 (22.9) | |
| Unemployed | 74 (15.9) | 34 (41.0) | <0.001 |
| Retired | 145 (31.2) | 30 (36.1) | |
| Income | |||
| <$10,000 | 49 (11.1) | 29 (39.7) | |
| $10,000–40,000 | 199 (45.2) | 40 (54.8) | <0.001 |
| >$40,000 | 192 (43.6) | 4 (5.5) | |
| Marital Status | |||
| Never married | 47 (10.0) | 18 (21.4) | |
| Married | 309 (65.6) | 25 (29.8) | <0.001 |
| Separated/widowed/divorced | 115 (24.4) | 41 (48.8) | |
| Live Alone | |||
| No | 400 (84.9) | 65 (78.3) | |
| Yes | 71 (15.1) | 18 (21.7) | 0.130 |
|
| |||
| Continuous Variable | Mean (SD) | Mean (SD) | P-value‡ |
|
| |||
| Non-Ocular Comorbidities | |||
| Number (Range 0–13) | 1.2 (1.4) | 2.2 (1.7) | <0.001 |
<1.5% missing for all variables except for income, 7.6% missing.
chi-square test
t-test
Differences in clinical outcomes and self-reported difficulties with visual function tasks between drivers and non-drivers are displayed in Table 2. On average, drivers had better MD and VA than non-drivers in both the better eye and worse eye at 6 months and 54 months. These differences were significant (all p-values < 0.014) in every case except MD in the worse eye at six months (p=0.613). Non-drivers reported significantly more difficulties with general visual function tasks at 6 month and 54 month follow-up in their total VAQ score, and all subscale scores (all p-values ≤0.05) except glare disability and light/dark adaptation. When the analyses comparing drivers and non-drivers were repeated adjusting for factors found significant in Table 1 (i.e., sex, race, education, employment, income, marital status, and number of non-ocular co-morbidities) most clinical differences remained significant at 54 months, while the observed differences between drivers and non-drivers regarding general visual function tasks were no longer significant.
Table 2.
Comparison of drivers and non-drivers by clinical and self-reported visual function variables at baseline (6 months) and 54 month follow-up
| 6 Month | 54 Month | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Continuous Variables | Driver (n=471) | Non-Driver (n=84) | Unadjusted P-value* | Adjusted P-value† | Driver (n=429) | Non-Driver (n=81) | Unadjusted P-value* | Adjusted P-value† |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Mean Deviation | ||||||||
| Better Eye | −2.1 (2.7) | −2.9 (3.0) | 0.014 | 0.966 | −1.9 (3.1) | −3.5 (3.7) | <0.001 | 0.007 |
| Worse Eye | −5.7 (4.9) | −5.9 (4.0) | 0.613 | 0.429 | −5.4 (5.2) | −7.0 (4.9) | 0.012 | 0.080 |
| Visual Acuity | ||||||||
| Better Eye | 87.7 (4.9) | 85.1 (5.4) | <0.001 | 0.012 | 86.9 (5.7) | 83.2 (6.9) | <0.001 | 0.003 |
| Worse Eye | 83.2 (7.5) | 79.7 (11.0) | 0.007 | 0.095 | 81.5 (10.6) | 75.3 (14.4) | 0.001 | 0.003 |
| Visual Activities Questionnaire | ||||||||
| Total Score | 1.9 (0.7) | 2.2 (0.8) | 0.003 | 0.647 | 1.9 (0.7) | 2.1 (0.9) | 0.025 | 0.458 |
| Color Discrimination | 1.5 (0.8) | 1.7 (0.9) | 0.047 | 0.368 | 1.5 (0.8) | 1.8 (1.0) | 0.008 | 0.134 |
| Glare Disability | 2.4 (1.0) | 2.4 (1.1) | 0.660 | 0.228 | 2.3 (1.1) | 2.2 (1.2) | 0.186 | 0.073 |
| Light/Dark Adaptation | 2.3 (1.0) | 2.5 (1.1) | 0.074 | 0.940 | 2.3 (1.1) | 2.5 (1.2) | 0.254 | 0.640 |
| Acuity/Spatial Vision | 2.4 (1.0) | 2.8 (1.2) | 0.008 | 0.374 | 2.2 (1.0) | 2.6 (1.1) | 0.008 | 0.458 |
| Depth Perception | 1.5 (0.7) | 1.8 (0.9) | 0.001 | 0.124 | 1.5 (0.7) | 1.8 (0.9) | 0.005 | 0.170 |
| Peripheral Vision | 1.7 (0.8) | 1.9 (0.9) | 0.014 | 0.902 | 1.7 (0.8) | 1.9 (0.9) | 0.019 | 0.471 |
| Visual Search | 2.0 (0.9) | 2.2 (0.9) | 0.040 | 0.903 | 1.9 (0.9) | 2.2 (1.1) | 0.052 | 0.467 |
| Visual Processing Speed | 1.8 (0.7) | 2.2 (0.9) | 0.001 | 0.164 | 1.7 (0.8) | 2.1 (1.0) | 0.008 | 0.521 |
t-test for unequal variance was used where applicable
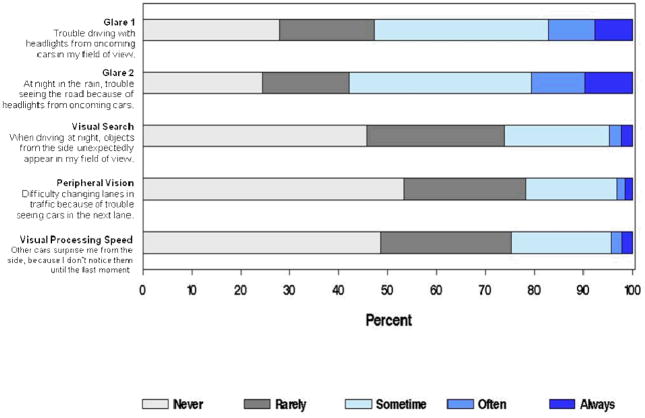
Figure 1 displays responses to the five VAQ items specifically related to driving at 6 months. Drivers more often reported difficulties with glare than with visual search, peripheral vision or visual processing speed. For both glare-related tasks, over 50% of drivers reported at least “some” difficulty. Over 20% of drivers reported “often” or “always” having difficulty seeing the road at night in the rain because of headlights. About 22% reported at least “some” difficulty with driving tasks requiring peripheral vision.
Figure 1.
Visual Activities Questionnaire Driving Items by percent reporting specific visual function concerns among drivers at 6 months
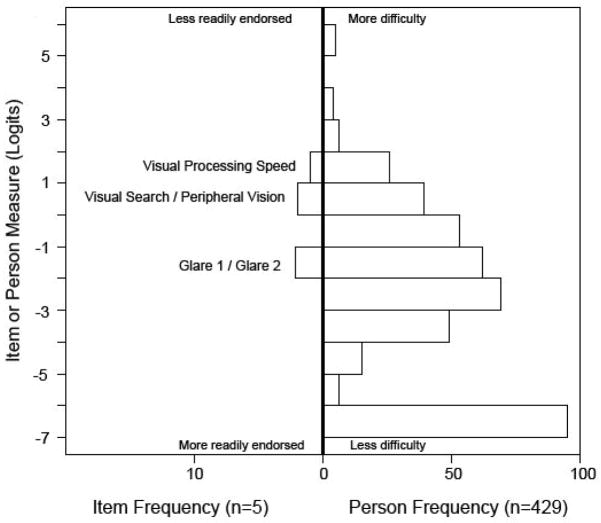
We then used Rasch Analysis to score the 5 driving items of the VAQ.22,23 Figure 2 shows the resulting person and item frequencies. Referring to person measures, the most negative logit score (lowest bar) reflects those drivers who did not endorse any difficulty with the five driving tasks (XX%). The items appear to be well targeted for people who indicate some degree of difficulty with visual function tasks related to safe driving.23 The item measures suggest that the two glare items were endorsed almost universally before the other three VAQ driving items. Of the remaining three items, visual search was endorsed next followed by peripheral vision and then visual processing speed. The infit mean squares are all within the recommended range (0.7 to 1.3), indicating all five items are useful.23
Figure 2.
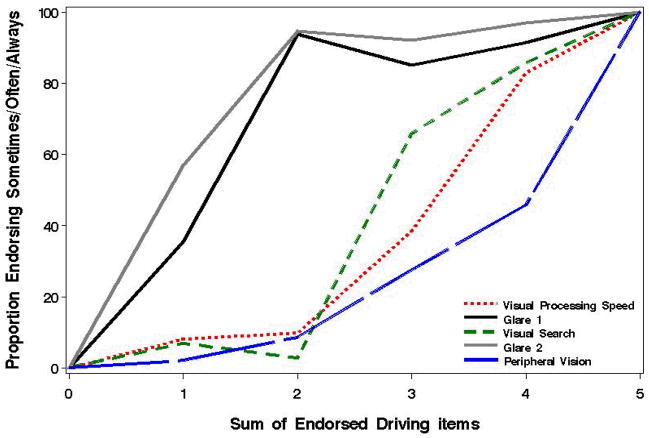
Visual Activities Questionnaire, the proportion endorsed for each question, by the number of endorsed driving items. We dichotomized each of the five responses as “sometimes” or more often (i.e., endorsed as a concern) versus “rarely” or “never”.
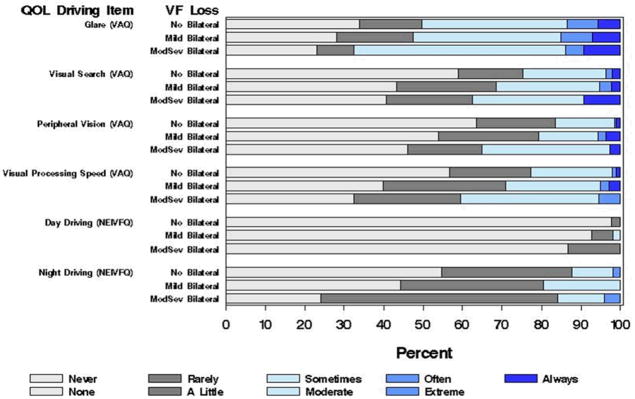
The association between bilateral visual field loss (VFL) and the frequency of difficulty with specific driving tasks at the 54 month follow-up (Figure 3) was next considered. We averaged the responses for the two glare questions, as justified in Figure 2 by their similar response pattern. Drivers with ModSev Bi VFL were more likely to report at least “some” difficulty with all five driving tasks compared to those with Mild or No Bi VFL. In terms of visual search, 38% of drivers with ModSev Bi VFL reported at least “sometimes” having difficulty with objects from the side unexpectedly appearing in their field of view while driving at night versus 31% of those with Mild Bi VFL, and 25% of those with No Bi VFL. Regarding peripheral vision, 35% of drivers with ModSev Bi VFL reported at least “sometimes” having difficulty changing lanes due to trouble seeing other cars compared to 17% of those with No Bi VFL. About 41% of subjects with ModSev Bi VFL (versus 29% with Mild Bi VFL and 23% with No Bi VFL) reported at least “sometimes” having difficulty driving using visual processing speed. For tasks involving visual search and visual processing speed, the differences noted between the three categories of bilateral VFL are significant (p=0.009 and p=0.001, respectively). The association with peripheral vision was marginally significant (p=0.060).
Figure 3.
Visual Activities Questionnaire and National Eye Institute-Visual Function Questionnaire Driving Items by level of bilateral visual field loss at 54 months. Findings reported for Glare (VAQ) are the average of drivers’ responses to the two VAQ items on glare
The same bilateral VFL categories were used to evaluate two NEI-VFQ items at 54 months (difficulty with daytime and night-time driving). In both cases, drivers with ModSev Bi VFL reported more difficulty than those with No Bi VFL (p=0.018 and p=0.009, respectively). Among drivers who did not drive at night (n=24), 16 responded it was due (at least in part) to their eyesight, and 8 responded “for other reasons.” Overall, far fewer individuals reported difficulty with daytime driving, although those with ModSev Bi VFL were more likely to report “a little” difficulty. For those who drove at night, 76% with ModSev Bi VFL (compared to 56% with Mild Bi VFL and 45% with No Bi VFL) rated night driving at least “a little” difficult.
Clinical change over time between those who remained drivers and those who became non-drivers by 54 months of follow-up is shown in Table 3. Subjects whose driving and non-driving status shifted more than three times in the four-year period (n = 100) were excluded from this analysis. There were no significant differences in the average MD change in the worse or better eye over time among those who remained drivers or those who became non-drivers. However, mean VA in both the worse and better eye significantly worsened over time among those who remained drivers and those who became non-drivers. The mean VA of the better eye showed decreases of 1.0 and 4.2 letters from 6 to 54 months for drivers and non-drivers (p<0.001 and p=0.006, respectively). The difference between these two mean decreases was significant (p=0.033). When the analyses included adjustment for significant sociodemographic factors and number of co-morbidities (see Table 1), the 6 to 54 month clinical change (MD and VA) in drivers compared to those who became non-drivers is significant and became even stronger.
Table 3.
Clinical comparison of drivers at 6 months who remained drivers vs. those who became non-drivers through 54 month follow-up, excluding those patients who were never drivers
| Visual Field Measure | N§ | 6 Months | 54 Months|| | Difference | Adjusted Difference | P-value* |
|---|---|---|---|---|---|---|
| Mean Deviation | Mean (SD) | LSMean (SE) | ||||
| Better Eye | ||||||
| Remain Driver | 337 | −2.0 (2.7) | −1.8 (3.1) | 0.2 (2.1) | 0.3 (0.3) | 0.143 |
| Became Non-Driver | 29 | −2.5 (2.1) | −3.3 (2.8) | −0.7 (2.7) | −0.9 (0.5) | 0.158 |
| (p-value) | 0.091† | 0.008‡ | ||||
| Worse Eye | ||||||
| Remain Driver | 337 | −5.5 (4.8) | −5.4 (5.3) | 0.1 (3.0) | 0.3 (0.4) | 0.606 |
| Became Non-Driver | 29 | −6.8 (5.4) | −8.3 (5.1) | −1.5 (4.8) | −1.3 (0.7) | 0.106 |
| (p-value) | 0.093† | 0.013‡ | ||||
| Visual Acuity | ||||||
| Better Eye | ||||||
| Remain Driver | 340 | 87.9 (4.6) | 86.9 (5.3) | −1.0 (4.6) | −0.4 (0.6) | <0.0001 |
| Became Non-Driver | 30 | 87.1 (6.4) | 82.9 (9.4) | −4.2 (7.7) | −3.9 (1.0) | 0.006 |
| (p-value) | 0.033† | 0.001‡ | ||||
| Worse Eye | ||||||
| Remain Driver | 340 | 83.5 (7.3) | 81.6 (10.4) | −1.9 (9.8) | −1.4 (1.3) | <0.0001 |
| Became Non-Driver | 30 | 82.0 (9.0) | 75.8 (14.9) | −6.2 (13.7) | −5.5 (2.1) | 0.020 |
| (p-value) | 0.105† | 0.054‡ |
paired t-test comparing 6 vs 54 months for each subject
p-value from 2-sample t-test
p-value from regression analysis with adjustments for sex, race, education, employment, income, marital status, and number of non-ocular comorbidities
missing data
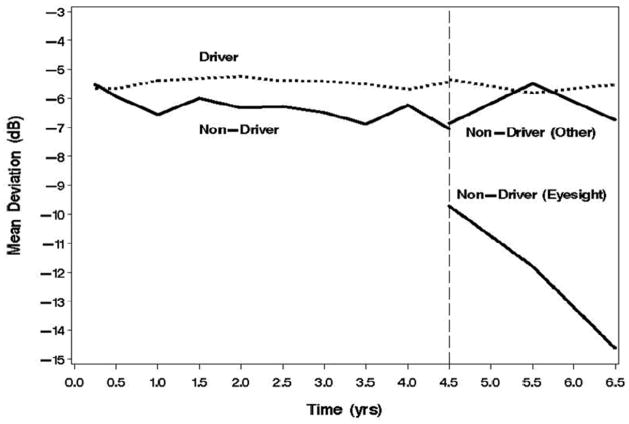
Figure 4 displays the average MD scores in the worse eye over the first 6.5 years of follow-up by driving status at each QOL interview. Drivers had consistently better MD values than non-drivers. At 4.5 years, when responses from the NEI-VFQ became available, the plot shows average MD scores among three groups (drivers, non-drivers due to eyesight and, non-drivers for other reasons). Both drivers and non-drivers who stopped for reasons other than eyesight show similar MD scores roughly between −5 and −6 dB. At 54 months, those who became non-drivers due to eyesight compared to those who became non-drivers for other causes were more likely to have significant worsening of their MD and VA over time. In addition, drivers at baseline who became non-drivers by 54 months compared to those who remained drivers were more likely to be black, have less education, and more co-morbidities.
Figure 4.
Mean Deviation in worse eye over time by driving status based on the Visual Activities Questionnaire (0–4.5 years) and National Eye Institute-Visual Function Questionnaire (4.5 – 6.5 years)
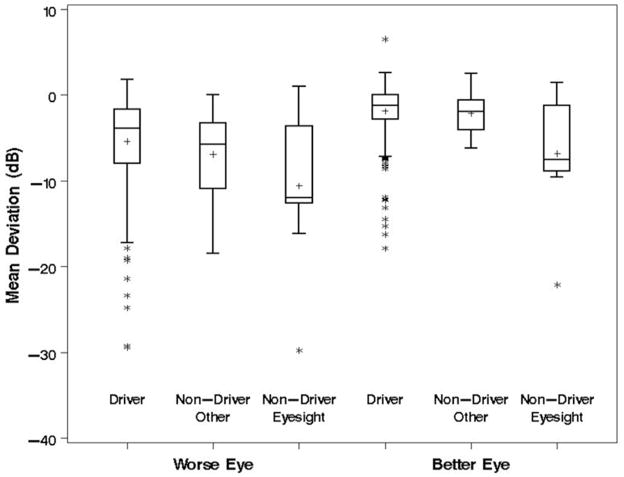
To further illustrate the clinical differences between these three groups, we present box plots comparing the MD of the worse and better eye between drivers, non-drivers for non-ocular reasons, and non-drivers due to eyesight at 54 months (Figure 5). The general trend is for drivers to have better MD values in both the worse and better eye than non-drivers who have stopped driving due to eyesight at 54 months. Nevertheless, the lower whiskers and outlier points on Figure 5 indicate that there are a number of drivers who have marked VF damage in both the worse and better eye.
Figure 5.
Boxplot showing the distribution of mean deviation values at 54 months by National Eye Institute- Visual Function Questionnaire driving status. Boxes extend from the 25th to 75th percentile. The crossbar is at the median, and the “+” sign indicates the mean. Whiskers extend to the nearest point within 1.5 times the interquartile range. Points beyond whiskers are indicated as outliers
Discussion
This study found that drivers and non-drivers with glaucoma differ on clinical measures of vision (VF and VA) but do not differ on patient reported difficulty across general tasks of daily living requiring vision. Patient reported difficulty on tasks specific to driving does, however, appear to be related to the degree of visual field loss among drivers. Drivers with moderate to severe bilateral VF damage consistently reported more difficulty with safe driving visual tasks than those with either mild or no bilateral damage. This finding is consistent with other recent studies suggesting that bilateral VF damage may place individuals at higher risk for safe driving.13–15, 24
While we found that difficulties with tasks involving glare were reported by the highest percentage of drivers, reported difficulty with tasks involving visual search and visual processing speed varied more depending on the degree of bilateral VF loss. Haymes et al.6 found an increase in accidents among individuals with glaucoma, with the strongest risk factor being impaired UFOV, a test of visual information processing speed. When drivers were asked a general question about “difficulty with day driving in familiar places,” we found only a small percentage of individuals reported even “a little” difficulty. When the questions addressed more specific visual tasks, such as “difficulty changing lanes” or “cars surprising them from the side,” substantially more drivers reported at least some difficulty, particularly ones with bilateral VF damage.
Not surprisingly, night driving was found to be more difficult than daytime driving. Three quarters of drivers reported at least a little difficulty with night driving, consistent with previous studies.11–13 In a two-year prospective study, Freeman et al.25 found that drivers with more limited peripheral VFs were more likely to stop night driving, even when controlling for demographic, health status, and co-morbidities factors. They also found a strong association between bilateral VF loss and difficulty with night driving.
Ophthalmologists are often asked to counsel patients on when or whether they should drive. Combining patients’ visual function as assessed by objective tests with more specific questions about difficulties when driving may help providers identify those patients at higher risk. Our preliminary Rasch findings22,23 suggest that beginning with items about glare might serve as good screening questions to separate glaucoma patients at greater risk for vision problems while driving. It appears that when glaucoma patients become aware of problems with driving and vision, glare problems are usually noticed first. Given the importance of driving, and the impact that visual disorders have on driving capabilities, future research should build on the driving items considered here to develop of a validated driving questionnaire to assist physicians in discussions with their patients.
It is also important to assess the amount of driving patients do and determine whether visual abilities can meet the demand. If not, the need to reduce or stop driving should be discussed with the patient and documented in the medical record. Including family members in discussions about driving may be beneficial; research has shown that, compared to individuals without glaucoma, glaucoma patients are more likely to report family concerns about their driving.26 In states with limited driver’s licenses, physicians can make appropriate referrals for patients so they don’t drive in circumstances that place themselves and others at a higher risk of an accident.14
In on-road driving performance, drivers with glaucoma compared to those with normal vision have been found to execute many driving maneuvers safely, but are far more likely to have difficulty with detection of peripheral obstacles and reaction to unexpected events.24 Along with developing a validated questionnaire, reliable functional tests are needed to assess driving deficits in the clinical area. Owsley et al.7 have suggested using tests of visual attention and processing speed that can identify high risk drivers. To preserve independence, it is necessary to understand which VF defects lead to visual disability and which can be compensated for by the remaining vision and/or cognitive factors.12 Drivers should also incorporate new technologies when available (e.g., designing new window positioning and mirror areas to assist drivers with particular visual concerns,12 and using new auto-navigation systems). Other possibilities include encouraging the use of more public transportation when available.
Over the five year follow-up, few CIGTS participants reported they stopped driving due to vision. Consistent with our findings regarding co-morbidities, previous studies have reported the presence of chronic conditions (e.g., cardiovascular disease, stroke, and diabetes) as well as poorer self-reported health can contribute to a change in driving status.27–30 While others have found that older women were more likely to discontinue driving than their male counterparts,27–29,31–33 no gender differences were observed in those who stopped driving over the course of this study. Additional studies are needed to discern the association between cognitive processing and decisions about driving.27,32,33
The non-drivers in this study who stopped driving for vision reasons did have substantially lower MD values than those who remained drivers. A change in vision has been found by previous investigators to be a significant predictor of driving cessation.27–32 However, our results also indicate that some drivers with substantial VF loss continue to drive. Focus groups with drivers and persons who stopped driving may identify the factors most relevant to individuals when deciding whether to stop driving.
This study’s strengths include a large sample of well-characterized glaucoma patients. The longitudinal design allowed comparisons of changes in driving status, and assessment of QOL and bilateral clinical outcomes over time. The VAQ assessed difficulties with driving tasks across a number of important visual function areas. Limitations include a small number of drivers who became non-drivers over the study’s course, thereby restricting our ability to identify factors that were associated with driving cessation. Second, we cannot distinguish the impact of glaucoma on driving from that of other conditions or aging in the absence of a comparison group of individuals without glaucoma. Third, the study sample represents individuals who were willing to enroll in a randomized treatment trial, and these subjects may not be representative of glaucoma patients seeking initial treatment. Fourth, the clinical measures were eye specific and any combination of these measures may not reflect true binocular vision. Finally, duration and type of driving (i.e., driving exposure) were not factored into the associations we report. Previous studies have found that drivers with glaucoma compared to those without glaucoma were more likely to self-regulate their driving, thereby avoiding potentially difficult situations such as driving at night, in rush hour, on expressways, in unfamiliar areas, and during inclement weather.26,34
Conclusion
Individuals with glaucoma indicate greater difficulty in performing safe driving tasks with worsening VFs, particularly when bilateral damage is present. More targeted discussions about driving should be included as a part of regular clinical care. When clinical examination reveals glaucomatous visual deficits, physician inquiries about driving exposure and difficulties with specific driving tasks can be useful when counseling patients regarding safe driving.
Acknowledgments
Supported by grants from the National Eye Institute (EY015700 & EY09148) and an unrestricted grant from Allergan, Inc.
References
- 1.Bhargava JS, Patel B, Foss AJ, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Investigative Ophthalmology & Visual Science. 2006;47(7):2885–2888. doi: 10.1167/iovs.05-1244. [DOI] [PubMed] [Google Scholar]
- 2.Ang GS, Eke T. Lifetime visual prognosis for patients with primary open-angle glaucoma. Eye. 2007;21(5):604–608. doi: 10.1038/sj.eye.6702284. [DOI] [PubMed] [Google Scholar]
- 3.McGwin G, Jr, Owsley C, Ball K. Identifying crash involvement among older drivers: Agreement between self-report and state records. Accident Analysis and Prevention. 1998;30(6):781–791. doi: 10.1016/s0001-4575(98)00031-1. [DOI] [PubMed] [Google Scholar]
- 4.McGwin G, Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Investigative Ophthalmology & Visual Science. 2005;46(12):4437–4441. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 5.Owsley C, McGwin G, Jr, Ball K. Vision impairment, eye disease, and injurious motor vehicle crashes in the elderly. Ophthalmic Epidemiology. 1998;5(2):101–113. doi: 10.1076/opep.5.2.101.1574. [DOI] [PubMed] [Google Scholar]
- 6.Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Risk of falls and motor vehicle collisions in glaucoma. American Journal of Ophthalmology. 2007;48:1149–1155. doi: 10.1167/iovs.06-0886. [DOI] [PubMed] [Google Scholar]
- 7.Owsley C, McGwin G., Jr Vision impairment and driving. Survey of Ophthalmology. 1999;43(6):535–550. doi: 10.1016/s0039-6257(99)00035-1. [DOI] [PubMed] [Google Scholar]
- 8.Szlyk JP, Mahler CL, Seiple W, Edward DP, Wilensky JT. Driving performance of glaucoma patients correlates with peripheral visual field loss. Journal of Glaucoma. 2005;14(2):145–150. doi: 10.1097/01.ijg.0000151686.89162.28. [DOI] [PubMed] [Google Scholar]
- 9.Bowers A, Peli E, Elgin J, McGwin G, Jr, Owsley C. On-road driving with moderate visual field loss. Optometry and Vision Science. 2005;82(8):657–667. doi: 10.1097/01.opx.0000175558.33268.b5. [DOI] [PubMed] [Google Scholar]
- 10.Parrish RK, II, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Archives of Ophthalmology. 1997;115(11):1447–1455. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 11.Gutierrez P, Wilson R, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Archives of Ophthalmology. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 12.Nelson P, Aspinall P, Papasouliotis O, Worton B, O’Brien C. Quality of life in glaucoma and its relationship with visual function. Journal of Glaucoma. 2003;12(2):139–150. doi: 10.1097/00061198-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Freeman EE, Muñoz B, West SK, Jampel HD, Friedman DS. Glaucoma and quality of life: the Salisbury Eye Evaluation. Ophthamology. 2008;115(2):233–8. doi: 10.1016/j.ophtha.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 14.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP Los Angeles Latino Eye Study Group. Severity of visual field loss and health-related quality of life. American Journal of Ophthalmology. 2007;143(6):1013–1023. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R Los Angeles Latino Eye Study Group. Impact of visual field loss on health-related quality of life in glaucoma. Ophthalmology. 2008;115(6):941–948. doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Musch DC, Lichter PR, Guire KE, Standardi CL The CIGTS Study Group. The Collaborative Initial Glaucoma Treatment Study: Study design, methods, and baseline characteristics of enrolled patients. Ophthalmology. 1999;106(4):653–662. doi: 10.1016/s0161-6420(99)90147-1. [DOI] [PubMed] [Google Scholar]
- 17.Lichter PR, Musch DC, Gillespie BW, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943–1953. doi: 10.1016/s0161-6420(01)00873-9. [DOI] [PubMed] [Google Scholar]
- 18.Janz NK, Wren PA, Lichter PA, et al. Quality of life in newly diagnosed glaucoma patients: The Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2001;108(5):887–897. doi: 10.1016/s0161-6420(00)00624-2. [DOI] [PubMed] [Google Scholar]
- 19.Sloane ME, Ball K, Owsley C, Bruni JR, Roenker DL. The visual activities questionnaire: Developing an instrument for assessing problems in everyday visual tasks. Technical Digest: Noninvasive Assessment of the Visual System. 1992;1:26–29. [Google Scholar]
- 20.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Archives of Ophthalmology. 2001;119(7):1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 21.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Archives of Ophthalmology. 1998;116(11):1496–1504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 22.Massof RW. An interval-scaled scoring algorithm for visual function questionnaires. Optomotry and Visual Science. 2007;84(8):689–704. doi: 10.1097/OPX.0b013e31812f5f35. [DOI] [PubMed] [Google Scholar]
- 23.Pesudovs K, Burr JM, Harley C, Elliott DB. The development, assessment, and selection of questionnaires. Optomotry and Visual Science. 2007;84(8):663–674. doi: 10.1097/OPX.0b013e318141fe75. [DOI] [PubMed] [Google Scholar]
- 24.Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauban BC. Glaucoma and On-Road Driving Performance. Investigative Ophthalmology and Visual Science. 2008;49(7):3035–3041. doi: 10.1167/iovs.07-1609. [DOI] [PubMed] [Google Scholar]
- 25.Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and their association with driving modification in older adults. Investigative Ophthalmology & Visual Science. 2006;47(2):514–20. doi: 10.1167/iovs.05-0934. [DOI] [PubMed] [Google Scholar]
- 26.Adler G, Bauer M, Rottunda S, Kuskowski M. Driving habits and patterns in older men with glaucoma. Soc Work Health Care. 2005;40(3):75–87. doi: 10.1300/J010v40n03_05. [DOI] [PubMed] [Google Scholar]
- 27.Anstey KJ, Windsor TD, Luszcz, Andrews GR. Predicting driving cessation over 5 years in older adults: Psychological well-being and cognitive competence are stronger predictors than physical health. Journal of the American Geriatrics Society. 2006;54(1):121–6. doi: 10.1111/j.1532-5415.2005.00471.x. [DOI] [PubMed] [Google Scholar]
- 28.Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and time to driving cessation in older adults. Optometry and Vision Science. 2005;82(8):765–73. doi: 10.1097/01.opx.0000175008.88427.05. [DOI] [PubMed] [Google Scholar]
- 29.Gilhotra JS, Mitchell P, Ivers R, Cumming RG. Impaired vision and other factors associated with driving cessation in the elderly: the Blue Mountains Eye Study. Clinical and Experimental Ophthalmology. 2001;29(3):104–7. doi: 10.1046/j.1442-9071.2001.00411.x. [DOI] [PubMed] [Google Scholar]
- 30.Dellinger AM, Sehgal M, Sleet DA, Barrett-Connor E. Driving cessation: What older former drivers tell us. Journal of the American Geriatrics Society. 2001;49(4):431–5. doi: 10.1046/j.1532-5415.2001.49087.x. [DOI] [PubMed] [Google Scholar]
- 31.Ragland DR, Satariano WA, MacLeod KE. Reasons given by older people for limitation or avoidance of driving. The Gerontologist. 2004;44(2):234–44. doi: 10.1093/geront/44.2.237. [DOI] [PubMed] [Google Scholar]
- 32.Keay L, Munoz B, Turano KA, Hassan SE, Munro C, Duncan D, Baldwin KC, Jasti S, Gower EW, West SK. Visual and cognitive deficits predict stopping restricting driving: the Salisbury Eye Evaluation Driving Study (SEEDS) Investigative Ophthalmology and Visual Science. 2008 doi: 10.1167/iovs.08-2367. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edwards JD, Ross LA, Ackerman ML, Small BJ, Ball KK, Bradley S, Dodson JE. Longitudinal predictors of driving cessation among older adults from the ACTIVE clinical trial. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2008;63(1):6–12. doi: 10.1093/geronb/63.1.p6. [DOI] [PubMed] [Google Scholar]
- 34.McGwin G, Mays A, Joiner W, DeCarlo DK, McNeal A, Owsley C. Is glaucoma associated with motor vehicle collision involvement and driving avoidance. Investigative Ophthalmology and Visual Science. 2004;45(11):3934–9. doi: 10.1167/iovs.04-0524. [DOI] [PubMed] [Google Scholar]