Abstract
Background
Self-medication results in wastage of resources, increases resistance of pathogens and generally causes serious health hazards such as adverse drug reactions, prolonged suffering and drug dependence. This study was undertaken to determine the reasons for self-medication and the pattern of self-medication among medical students.
Method
This cross-sectional descriptive study was conducted at the K.S. Hegde Medical Academy, Mangalore. The participants were medical students from first to final year. Medical students were selected through convenience sampling. The data was collected using a pre-tested semi-structured questionnaire. The data was analysed using SPSS version 16 and the results expressed as proportions.
Results
A total of 200 students, 121 (60.5%) female and 79 (39.5%) male, were included in the study. Of the medical students surveyed, self-medication was reported among 92%. The respondents who used self-medication found it to be time- saving in providing relief from minor ailments. The most common ailments for which self-medication were used were: the common cold (69%), fever (63%) and headache (60%). The students consulted their textbooks (39%) and seniors or classmates (38%) for the medications. Antipyretics (71%), analgesics (65%), antihistamines (37%) and antibiotics (34%) were the most common self- medicated drugs. Of the respondents, 33% were unaware of the adverse effects of the medication and 5% had experienced adverse reactions. The majority (64%) of students advised medications to others, more often to family and friends.
Conclusion
The prevalence of self-medication among medical students is high, facilitated by the easy availability of drugs and information from textbooks or seniors. A significant number of students are unaware of the adverse effects of the medication that they themselves take and suggest to others. Therefore, potential problems of self-medication should be emphasised to the students.
Keywords: Self-medication, Medical students
What this study adds:
The pattern of self-medication among medical students.
Factors influencing self-medication.
Potential adverse effects of self-medication.
Background
Self-medication can be defined as obtaining and consuming drugs without the advice of a physician for diagnosis, prescription or surveillance of treatment.1,2 Self-medication differs from self-care in that it involves drugs that may do good or cause harm.3 In several studies it has been found that inappropriate self-medication causes wastage of resources, increases resistance of pathogens and generally causes serious health hazards such as adverse drug reactions, prolonged suffering and drug dependence.3–6
There are many reasons for the increased likelihood of self- medication among medical students.3 These students have easy access to information from drug indices, literature, and other medical students to self-diagnose and self-medicate.
In addition, they have easy access to the medication itself through physician samples provided by pharmaceutical representatives, and “The White Coat” guarantees trouble-free access to drugs available in pharmacies.
There is a paucity of studies on self-medication among medical students.3 The present study was undertaken to identify the reasons for, and the patterns of, self-medication among medical students.
Method
This cross-sectional study was undertaken in K.S. Hegde Medical Academy, Mangalore, India, with approval from the Institutional Ethics Committee. The study population consisted of medical students from first to final year, within the age group of 18–25 years. Students were selected for the study by a convenient sampling method. The participants were briefed about the nature of the study, consent was given and a pre-tested semi-structured questionnaire administered to them. The information pertaining to the pattern of self-medication, indications for self-medication and drugs used for self-medication were included in the questionnaire. The investigators were present in case the respondents required assistance. For the purpose of the study, certain medical terms were explained to the first-year students, including dysmenorrhea, antipyretics and analgesics.
The data was analysed using SPSS version 16.00 and summarised as proportions.
Results
A total of 200 students participated in the study, of whom 121 (60.5%) were female and 79 (39.5%) were male. Among these 200 students, 45 (22.5%), 49 (24.5%) and 106 (53.0%) were studying in their first year, second year and final year respectively (Table 1). A total of 110 (90.9%) female participants and 74 (94.7%) male participants said they practiced self-medication. All the variables were denoted in multiple response questions.
Table 1: Socio-demographic characteristics of study population.
| Socio-demographic factors | No. of students N=200 | % | |
|---|---|---|---|
| Gender | Male | 79 | 39.5 |
| Female | 121 | 60.5 | |
| Age group (years) | 18-21 | 153 | 76.5 |
| 22-25 | 47 | 23.5 | |
| Year of study | First year | 45 | 22.5 |
| Second year | 49 | 24.5 | |
| Final year | 106 | 53.0 | |
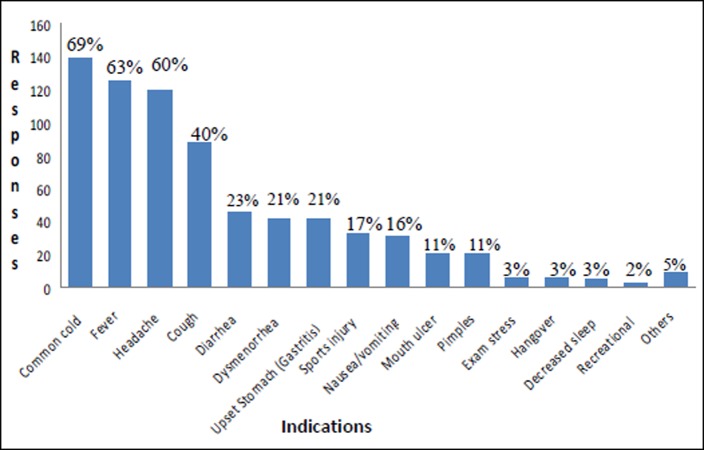
The study found that the conditions prompting self- medication (Figure 1) were the common cold (69%), fever (63%) and headache (60%), followed by gastrointestinal ailments, i.e. diarrhoea (23%), gastritis (21%) and nausea/vomiting (16%).
Figure 1: Indications for self-medication.
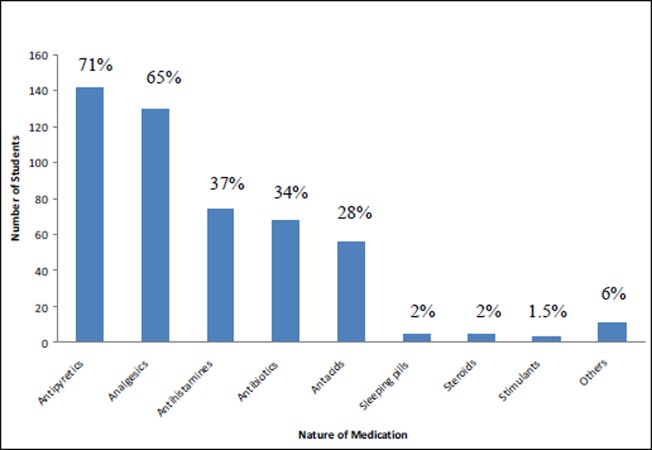
The classes of drugs that were commonly used (Figure 2) were antipyretics (71%), analgesics (65%), antihistamines (37%) and antibiotics (34%). Some potentially harmful drugs were also used, such as sleeping pills (2%), steroids (2%) and stimulants (1.5%).
Figure 2: Drugs used for self-medication.
A significant number, 32.6% of the study group, was unaware of the adverse effects of the drugs they took (Table 2). The study found that 10 students (5.4%) had experienced adverse reactions while on self-medication (Table 2). Of those who experienced adverse reactions, 50% consulted a doctor and the remaining 50% changed the medication on their own.
Table 2: Pattern of self-medication among medical students.
| Characteristics | Responses | |
|---|---|---|
| Reasons for self-medication (N=200) | No. of students | % |
| Lack of time to consult doctor | 22 | 11 |
| Minor ailment | 164 | 82 |
| Did not want to consult faculty/peers | 12 | 6 |
| Finished pharmacology, have confidence | 17 | 8.5 |
| Awareness of adverse effects (N=184) | ||
| Yes | 124 | 67.4 |
| No | 60 | 32.6 |
| Adverse reactions (N=184) | ||
| Experienced | 10 | 5.4 |
| Not experienced | 174 | 94.6 |
| Source (N=200) | ||
| Textbook | 78 | 39 |
| Senior/classmate | 76 | 38 |
| Pharmacist | 65 | 32.5 |
The most common sources of information for self- medication (Table 2), which were denoted in multiple choice questions, were textbooks (39%) and seniors or classmates (38%).
It was found that of 184 students who practiced self- medication, 117 (63.6%) suggested medication to others, most commonly to family/friends (51.8%) and to classmates or juniors (48.2%).
Discussion
Self-medication is becoming an increasingly important area within healthcare, 4 and this study has shown that it is even more prevalent among medical students. This study has found a prevalence of self-medication of 92% in medical students in contrast to 59% in a non-medical population in a previous study.1 It is also noted that a high level of education and professional status are predictive factors for self-medication.3 This is similar to the findings in a study conducted by Erlend Hem and colleagues5 (90%) but is higher than the findings (60%) in the study conducted by Henry James and colleagues.3
In our study it was found that more male students (94%) practice self-medication than female students (91%). This differs from a previous study conducted among medical students, which showed a greater prevalence among female students (45%) than male students (44%).3
Our study denoted that the most common reasons for self- medication were minor ailments (82%) and lack of time to consult a doctor (11%), which is in concordance with other studies that reported the reasons as mild illness (40%) and shortage of time to consult a doctor (32%).3 The next common reason for self-medication in our study among medical students was their confidence in self-diagnosis (8.5%), which is unique to this study group. Misplaced confidence can lead to inappropriate self-medication and can expose the participants to all the risks associated with inappropriate use of medications.3
With respect to indications, results were similar to those found in a previous study.3 We also found medical students self-medicate for unusual reasons, i.e. sports injuries, hangovers, exam stress and recreational drug use, which may not be common in the general public. In the study it was noticed that the classes of drugs that were commonly used were antipyretics (71%), analgesics (65%), antihistamines (37%) and antibiotics (34%). This is similar to studies done earlier, which showed antipyretics (43%), analgesics (81%), antibiotics (6%) and antihistamines (13%) were commonly used.3 In other studies it was found that medical students (N=68) used more types of antibiotics compared to the non-medical students (N=69), which may be because of their knowledge about antibiotics.7 We have found, however, that 11 (5.5%) of the medical students are not afraid of using drugs with potentially harmful adverse effects and potential for addiction and abuse, i.e. sleeping pills (2%), steroids (2%) and stimulants (1.5%). These drugs may not be as easily available to the general population as they are to medical students, who can obtain them by virtue of their profession, and previous studies have reported higher use of antimicrobials when the study participant was a healthcare professional.3
Despite studying in detail about all these drug reactions, 32.6% of the students were unaware of the adverse effects of the drugs they used for self-medication. In addition to this, 5.4% of the study group reported experiencing adverse effects, for which they either consulted a doctor or stopped the medication.
The study group cited their source of information for self- medication in most cases as textbooks (39%) and seniors or classmates (38%); this is similar to other studies, which showed medical students use their academic medical knowledge 50% of the time to self-medicate.7
Conclusion
This descriptive study has found that self-medication is very common among medical students, facilitated by the easy availability of drugs, and information from textbooks/seniors. A significant number of students are unaware of the adverse effects of the medication that they themselves take and suggest to others. Since inappropriate self-medication has the potential to cause serious harm, not only to the students themselves but also to those whom they suggest medication, potential problems of self- medication should be emphasised to the students to minimise this risk. Restriction of sale of drugs with potentially harmful effects should be implemented effectively with monitoring systems between the physicians and pharmacists. Steps can also be taken to educate pharmacists on the need to cross-check with the prescribing physician while dispensing such drugs.
The limitations of this study included the absence of a comparative group, such as students from another field; the small sample size; and the absence of interventions, like providing information regarding hazards of self-medication.
ACKNOWLEDGEMENTS
The authors would like to thank the medical students for participating in this study.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed
CONFLICTS OF INTEREST
The authors declare that they have no competing interests
FUNDING
Not applicable.
ETHICS COMMITTEE APPROVAL
Institutional Ethics Committee, K.S. Hegde Medical Academy, Nitte University, Mangalore
Please cite this paper as : Badiger S, Kundapur R, Jain A, Kumar A, Patanashetty S, Thakolkaran N, Bhat, Ullal N. Selfmedication patterns among medical students in South India. AMJ 2012, 5, 4, 217 – 220.http//dx.doi.org/10.4066/AMJ.2012.1007.
References
- 1.Shankar PR, Partha P, Shenoy N.. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montastruc JL, Bagheri H, Geraud T, Lapeyre Mestre M.. Pharmacovigilance of self-medication. Therapie. 1997;52:105–110. [PubMed] [Google Scholar]
- 3.James H, Handu SS, Khalid AJ, Khaja A, Otoom S, Sequeira RP.. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15:270–275. doi: 10.1159/000092989. [DOI] [PubMed] [Google Scholar]
- 4.Hughes CM, McElnay JC, Fleming GF.. Benefits and risks of self medication. Drug Saf. 2001;24:1027–1037. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hem E, Stokke G, Reidar Tyssen R, Gronvold NT, Vaglum P, Ekeberg O.. Self-prescribing among young Norwegian doctors: a nine-year follow-up study of a nationwide sample. BMC Med. 2005;3:16. doi: 10.1186/1741-7015-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiyingi KS, Lauwo JAK.. Drugs in home: danger and waste. World Health Forum. 1993;14:381–384. [PubMed] [Google Scholar]
- 7.Sarahroodi S, Arzi A, Sawalha A.F., Ashtarinezhad A.. Antibiotic Self-Medication among South Iranian University Students. International Journal of Pharmacology. 2010;6((1)):48–52. [Google Scholar]