Abstract
Introduction
Cutaneous or umbilical endometriosis is a rare entity that is often overlooked because of chronic abdominal pain. We present a case of umbilical hernia that presented to the general surgeons due to chronic abdominal pain and nodule in the umbilicus, which was clinically diagnosed as umbilical papilloma.
Case presentation
A 48-year old multiparous Caucasian woman presented with painful nodule in the umbilicus for two and half years. The nodule was excised and the histopathological diagnosis was umbilicus endometriosis.
Conclusion
Umbilical endometriosis is a very rare disease but should be considered as a differential diagnosis in women presenting with umbilical swelling.
Keywords: Endometriosis, Umbilical endometriosis, Papilloma
Background
Endometriosis is the presence of functional endometrial (glands and/ or stroma) tissue outside the uterine cavity. It is a very common gynaecological disease. Endometriosis usually occurs in the pelvic cavity: on the ovaries, fallopian tubes, ligaments that support the uterus, the area between vagina and rectum, the outer surface of uterus, and lining of pelvic cavity; giving rise to the common presenting symptoms of pelvic pain, dysmenorrhoea, dyspareunia, cyclical bowel or bladder symptoms, and infertility. Extragenital or extrapelvic endometriosis is even more difficult to diagnose due to the extreme variability in presentation. Cutaneous or umbilical endometriosis is a rare entity that is often overlooked because of chronic abdominal pain.1 Rarely, it presents to the general surgeons because of clinical presentation that suggests as incisional hernia or other conditions related to general surgery.2
Case details
A 48-year old multiparous Caucasian woman presented with painful nodule in the umbilicus for two and half years in the surgical outpatient door. The nodule was 3 cm x 2cm, soft, domed-shaped, pigmented with papillary projections on the surface. The patient had cyclic pain in the nodule. However, there was no history of umbilical bleeding or discharge, any menstrual disturbances, alteration in bowel and bladder habit or infertility to suggest pelvic endometriosis.
She had past history of laparoscopic cholecystectomy two years previous. The preliminary clinical diagnosis was umbilical papilloma, hence surgical excision was performed and no further evaluation was done.
Normal results were reported from baseline investigations, which included a complete blood count, random blood sugar, serum creatinine, serum electrolytes, serum thyroid stimulating hormone and chest x-ray. Muscle conduction studies indicated myotonia of left abductor pollicis brevis elicited spontaneously and percussively. MRI of the cranium revealed a mega cisterna magna. The patient was diagnosed with dystrophia myotonica type 1 in association with mega cistern magna. Phenytoin 300mg/day was given to the patient. With treatment, the patient showed partial improvement in myotonia.
Gross examination
Single, gray-brown fungating nodule, measuring 2 cm in diameter on the surface of the skin fragment.
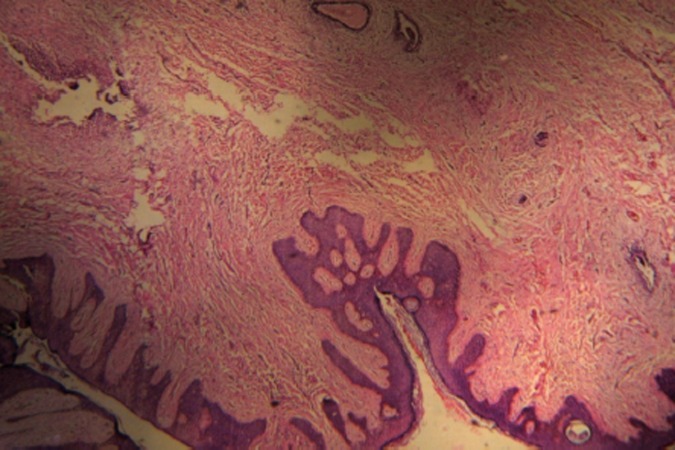
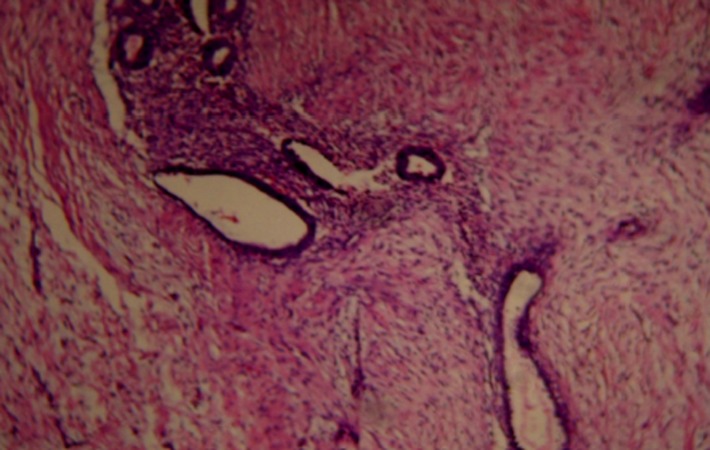
Histopathological examination
The lesion revealed glandular structures lined by bland cuboidal cells surrounded by stroma of spindle cells in the reticular dermis.
Figure 1. Microscopic picture of skin with endometrial tissue (H & E Stain at 10x X 10x magnification).
Figure 2. Microscopic picture showing endometrial glands and stroma. (H & E Stain at 10x X 10x magnification).
Discussion
Extra-gonadal site of endometriosis is a rare pathologic condition.1,3 In extra-gonadal endometriosis, involvement of almost every organ has been described in the literature. Endometriosis involving the abdominal wall is termed as cutaneous endometriosis, and it is mostly associated with surgical scars1,3 after abdominal or pelvic operations, or may occur spontaneously4,5. These operations include hysterectomy, tubal ligation, Caesarean section, episiotomy and laparoscopy.6 Umbilical endometriosis is uncommon with an estimated incidence of 0.5 to 1%.6
In this case, most likely; umbilical endometriosis is due to surgical scar followed by previous laparoscopic surgery. Agarwal et al reported 60% of all cutaneous endometriosis being in an abdominal scar; and the most common antecedent surgery was Caesarean section.1
Cyclical pain in umbilicus with a palpable mass was most the presenting symptom in our case. Similarly, Agarwal et al observed classical cyclical symptoms during menstruation in all 10 review cases of cutaneous endometriosis.1 In the case report of scar endometriosis developing after an umbilical hernia repair with mess published by Majeski et al, the patient presented with similar symptom of cyclic pain in the umbilical mass with menstruation.6
Lee et al,5 and Techapongsatorn et al,3 each reported a rare case of umbilical endometriosis in which the patients had cyclical bleeding from the umbilical mass during menstrual period.
There are several doubts concerning the etiopathogenesis of this condition during the last decades.7 Multiple theories have been proposed to explain the development of endometriosis: metaplasia, retrograde menstruation, venous or lymphatic metastasis, and mechanical transplantation.6 In this case, umbilical endometriosis may be due to surgical scar with the possibilities of implantation of shredded endometrial cells or metaplasia of celomic epithelium into endometrial tissue.
The possibility of co-existing genital-pelvic endometriosis should be excluded8,9 by ultrasonogram and or exploratory laparoscopy of abdominal cavity. Since, evaluation of genital-pelvic endometriosis was not done in this case as the nodule clinically resembled papilloma, but the patient had symptoms of abdominal pain even before she underwent laparoscopic cholecystectomy; hence, it should be ruled out to exclude the other possible etiopathogenesis. If it co-exists with pelvic endometriosis, transplantation by lymphatic or hematogenous spread is favoured.8
The differential diagnosis of umbilical nodules includes: pyogenic granuloma, embryological rests, irreducible hernia, endometriosis, inclusion cysts, primary tumours or secondary metastatic tumours from intra-abdominal malignancy.3 Hence, umbilical endometriosis should be included in diagnosis of women presenting with umbilical swelling,3 and it is important for surgeons to be aware of pathologies that may be encountered in this region as laparoscopic surgery is becoming the main modality of surgical management for conditions in the field of general surgery as well as gynaecology where umbilicus has been used as the main trocar incision site in most laparoscopic procedures.2,4 Surgical excision is necessary for proper histopathological diagnosis as well as for therapeutic purpose.4,10 In perimenopausal we can wait and watch. The use of combined contraceptive may suppress the endometrial growth. Danazole (steroid androgen), Gonadotropin releasing hormone (GnRH) agonist (Zoladex) can be used preoperatively to reduce the size of endometrial implant size. The anti-inflammatory drugs and acetaminophen can be used to prevent the pain. Ablation by lazer vaporisation may also be done in older patients.4,10,11
Conclusion
Umbilical endometriosis is a rare condition but possible pathology of the umbilicus; and should be considered as a differential diagnosis in a women presenting with umbilical swelling. The diagnosis is difficult clinically, therefore, surgical excision with removal and histopathology is recommended for both diagnostic and therapeutic purposes. Simultaneous laparoscopy should be performed to the patient with suspicion of pelvic endometriosis.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
Nil
FUNDING
Nil
PATIENT CONSENT
Taken
- They have obtained written, informed consent for the publication of the details relating to the patient(s) in this report.
- All possible steps have been taken to safeguard the identity of the patient(s).
- This submission is compliant with the requirements of local research ethics committees.
Please cite this paper as: Singh A. Umbilical endometriosis mimicking as papilloma to general surgeons: A case report AMJ 2012, 5, 5, 272-274. http//dx.doi.org/10.4066/AMJ.2012.1198
References
- 1.Agarwal A, Fong YF.. Cutaneous endometriosis. Singapore Med J. 2008;49(9):704–709. [PubMed] [Google Scholar]
- 2.Aydin O. Scar endometriosis-a gynaecologic pathology often presented to the general surgeon rather than the gynaecologist: report of two cases. Langenbecks Arch Surg. 2007;392(1):105–109. doi: 10.1007/s00423-006-0107-8. [DOI] [PubMed] [Google Scholar]
- 3.Techapongsatorn S, Techapongsatorn S. Primary umbilical endometriosis. J Med Assoc Thai. 2006;89(10):1753–1755. [PubMed] [Google Scholar]
- 4.Teh WT, Vollenhoven B, Harris PI. Umbilical endometriosis, a pathology that a gynecologist may encounter when inserting the Veres needle. Fertil Steril. 2006;86(6):1764.e1-2. doi: 10.1016/j.fertnstert.2006.03.070. [DOI] [PubMed] [Google Scholar]
- 5.Lee A, Tran HT, Walters RF, Yee H, Rosenman K, Sanchez MR. Cutaneous umbilical endometriosis. Dermatol Online J. 2008;14(10):23. [PubMed] [Google Scholar]
- 6.Majeski J, Craggie J. Scar endometriosis developing after an umbilical hernia repair with mesh. South Med J. 2004;97(5):532–534. doi: 10.1097/00007611-200405000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Frischknecht F, Raio L, Fleischmann A, Dreher E, Luscher KP, Mueller MD. Umbilical endometriosis. Surg Endosc. 2004;18(2):347. doi: 10.1007/s00464-003-4245-6. [DOI] [PubMed] [Google Scholar]
- 8.Friedman PM, Rico MJ. Cutaneous endometriosis. Dermatol Online J. 2000;6(1):8. [PubMed] [Google Scholar]
- 9.Krumbholz A, Frank U, Norgauer J, Ziemer M.. Umbilical endometriosis. J Dtsch Dermatol Ges. 2006;4(3):239–241. doi: 10.1111/j.1610-0387.2006.05927.x. [DOI] [PubMed] [Google Scholar]
- 10.Ideyi SC, Schein M, Niazi M. Spontaneous endometriosis of the abdominal wall. Dig Surg. 2003;20(3):246–248. doi: 10.1159/000070392. [DOI] [PubMed] [Google Scholar]
- 11.Purvis RS, Tyring SK. Cutaneous and subcutaneous endometriosis:surgical and hormonal therapy. J Dermatol Surg Oncol. 1994;20:693–695. doi: 10.1111/j.1524-4725.1994.tb00456.x. [DOI] [PubMed] [Google Scholar]