Abstract
Background
Medical education is associated with various pressures and stresses which can lead to depression. This study was undertaken to discover the prevalence of depression in medical students and various factors contributing to depression.
Method
This is a cross-sectional, questionnaire-based study. Using stratified random sampling, 237 students were selected according to year of study. Patient Health Questionnaire (PHQ-9), based on PRIME-MD Today, was used to make a provisional diagnosis of depression.
Results
The overall prevalence of provisionally diagnosed depressive and major depressive disorder using PHQ-9 was 21.5% and 7.6%, respectively. Year of study and academic performance of students had a statistically significant association with depression. Other factors, including gender, self-reported past history of depression, family history of psychiatric disorders, type of social support, family structure, number of siblings and education of parents were not found to have any significant association with prevalence of depression in the study. It was also observed that students were reluctant to seek help for depressive symptoms.
Keywords: Medical students, depression, academic performance
Background
Medical students are confronted with significant academic, psychological and existential stressors.1 Consequently, prevalence of depression is higher in medical students compared to the general population.2,3 It has been observed that mental health worsens after students begin medical school and remains poor throughout training. On a personal level, this distress can contribute to substance abuse, broken relationships, suicide, and attrition from the profession. On a professional level, studies suggest that student distress contributes to cynicism and subsequently may affect students' care of patients, relationship with faculty, and ultimately the culture of the medical profession.4
According to the Diagnostic and Statistic Manual, Fourth Edition (DSM- IV), individuals must exhibit five of the following symptoms to meet the criteria for a major depressive disorder: depressed mood, diminished interest or pleasure, significant weight loss, insomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished ability to concentrate, and recurrent thoughts of death; and at least one symptom should be either depressed mood or loss of interest or pleasure.
Methods
Using stratified random sampling, 237 medical students were selected according to year of study. Students participating in the study were undertaking a baccalaureate course in medicine from Maulana Azad Medical College, New Delhi. Sample size was arrived at on the basis of 39% prevalence of depression in medical students, observed in a previous Indian study,1 with 95% confidence interval and considering 30% as worst prevalence.
Patient Health Questionnaire (PHQ-9), based on PRIME MD Today (Primary Care Evaluation of Mental Disorders), was used to provisionally diagnose depression. This is a self-administered questionnaire which assists in screening, evaluating and provisionally diagnosing depression. It has been field tested and validated in large primary care patient samples.5 The nine items of the PHQ- 9 are based directly on the nine diagnostic criteria for major depressive disorder in DSM-IV. Information regarding various personal and academic factors was also collected.
Results
The response rate of the study was 79%; 53.3% of students showed a positive response to questions one or two or both of the PHQ-9. These questions are used as screening questions and are based on symptoms which must be present for the diagnosis of major depressive disorder.
Overall prevalence of provisionally diagnosed depressive and major depressive disorder in medical students was found to be 21.5% and 7.6%, respectively.
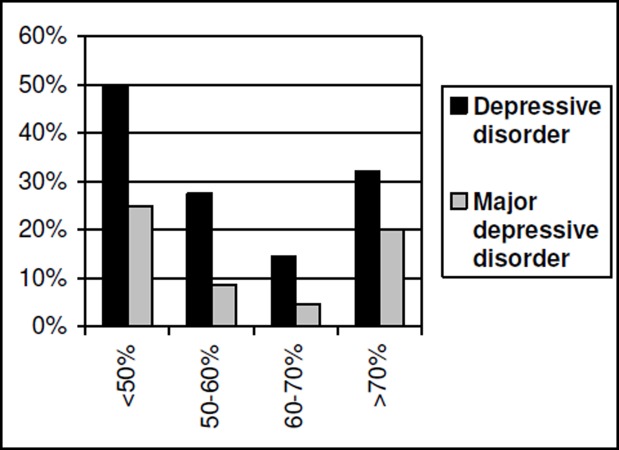
Our results revealed that year of study and academic performance of medical students have a significant association with the prevalence of depression. First year students had the highest prevalence of depression followed by second year students (P value < 0.001). It was also observed that students with poor or excellent academic performance (based on the scores obtained in recent terminal or annual examinations) had higher rates of depression (P value < 0.05). Figure 1,2
Figure 1. Prevalence of depressive and major depressive disorder according to year of study (x axis).
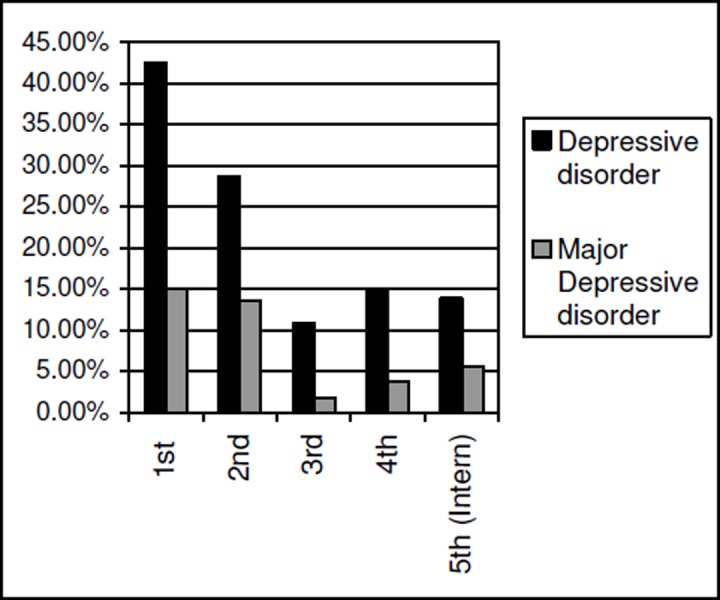
Figure 2. Prevalence of depressive and major depressive disorder according to academic performance (x axis) (as determined by aggregate marks).
Other factors such as gender, family history of psychiatric disorders, past history of depression, type of social support and family structure, number of siblings and education of parents were not found to have a statistically significant impact on prevalence of depression in the study.
14.7% of medical students reported having previous episodes in which they experienced various symptoms suggestive of depression. However, only 4.7% had sought counselling for the same.
Discussion
Medical education can be quite stressful and studies all over the world have consistently shown a high prevalence of depression in medical students. A study based in the United States found 24% of medical students to be depressed.6 In another study in the United States, 12% of medical students were diagnosed with probable major depression using DSM III criteria.3 In India, the prevalence of depression was around 39%.1 These alarming statistics have been corroborated by this study. It was observed that the prevalence of provisionally diagnosed depressive disorder and major depressive disorder in medical students was 21.5% and 7.6%, respectively.
Academic performance had a significant association with depression in medical students. This is similar to results seen in another study based in India.7 The stigma associated with poor academic performance may be a contributing factor. On the other hand, students with excellent academic performance maybe facing pressures due to the competitive nature of medical education.
Upon entering medical school, students are faced with a new environment and experience high academic stress. This could be contributing to the higher prevalence of depression seen in first year medical students in this study. Similar trends have been observed in Sweden.2
Gender did not have any significant association with prevalence of depression in this study. This is comparable to findings of a prior Indian study.7
Medical students are reluctant to seek help from mental health services. Although 14.7% students admitted to have experienced depressive symptoms, only 4.7% had ever consulted a counsellor. In a prior study to find prevalence of depression and use of mental health services amongst medical students, it was seen that only 22% of depressed students were using mental health counselling services.6 The most frequently cited barriers to using these services were lack of time, lack of confidentiality, stigma associated with using mental health services, cost, fear of documentation on academic record, and fear of unwanted intervention.6
Table 1: Percentage of students with probable depressive disorder and associated factors.
| Factor | Total N=237 100% |
Probable Depressive Disorder | Not having depression n =186 78.5% |
||
|---|---|---|---|---|---|
| Major Depressive Disorder n=18 7.6% |
Other depressive disorder n=33 13.9% |
Total n=51 21.5% |
|||
| Sex (p value- 0.33) | |||||
| Male | 53.2% | 6.3% | 13.5% | 19.8% | 80.2% |
| Female | 46.8% | 9% | 14.4% | 23.4% | 76.6% |
| Year (p value – 0.001) | |||||
| 1st | 16.9% | 15%** | 27.5% | 42.5% | 57.5% |
| 2nd | 21.9% | 13.5% | 15.3% | 28.8% | 71.2% |
| 3rd | 23.2% | 1.8% | 9.1% | 10.9% | 89.1% |
| 4th | 22.8% | 3.7% | 11.1% | 14.8% | 85.2% |
| Intern | 15.2% | 5.6% | 8.3% | 13.9% | 86.1% |
| Academic performance (on the basis of percentage of marks) (p value- 0.038) | |||||
| <50% | 3.4% | 25%** | 25% | 50% | 50% |
| 50-70% | 84.8% | 6% | 12.9% | 18.9% | 81.1% |
| >70% | 11.8% | 20% | 12.1% | 32.1% | 67.9% |
| Residence (p value- 0.43) | |||||
| Hostel | 24.9% | 10% | 6.9% | 16.9% | 83.1% |
| Hostel (workdays) | 35.4% | 7.1% | 13.1% | 20.2% | 79.8% |
| At home | 39.7% | 6.4% | 19.1% | 25.5% | 74.5% |
| Family structure (p value- 0.8) | |||||
| Joint | 15.2% | 3.7% | 18.5% | 22.2% | 77.8% |
| Nuclear | 84.8% | 7.9% | 16.6% | 24.5% | 75.5% |
| Siblings (p value- 0.49) | |||||
| None | 8.5% | 0 | 15% | 15% | 85% |
| One | 60.2% | 9.85% | 9.85% | 19.7% | 80.3% |
| Two | 25.4% | 3.3% | 25% | 28.3% | 71.7% |
| More than two | 5.9% | 13.3% | 6.7% | 20% | 80% |
| Parents education (p value- 0.76) | |||||
| High school and below | 4.2% | 10% | 10% | 20% | 80% |
| Graduate | 36.7% | 11.5% | 12.6% | 24.1% | 75.9% |
| Post graduate and above | 59.1% | 5% | 15% | 20% | 80% |
| Family history of depression and other psychiatric disorders (p value- 0.09) | |||||
| Yes | 3.8% | 11.1% | 33.3% | 44.4% | 55.6% |
| No | 96.2% | 7.45% | 13.15% | 20.6% | 79.4% |
| Previous history of depressive symptoms (p value- 0.27) | |||||
| Yes | 14.8% | 8.6% | 20% | 28.6% | 71.4% |
| No | 85.2% | 7.4% | 12.9% | 20.3% | 79.7% |
| Past consultation with counsellor (p value- 0.4) | |||||
| Yes | 4.7% | 0 | 9.1% | 9.1% | 90.9% |
| No | 95.3% | 8% | 14.1% | 22.1% | 77.9% |
Conclusion
In conclusion, this study has shown that the prevalence of depression in medical students is high and a similar trend has been seen in studies done around the globe. Academic performance and the year of study have an impact on the prevalence of depression. Medical students are reluctant to seek help for depressive symptoms. Initiatives need to be taken to decrease the prevalence of depression in medical students and improve their help-seeking behaviour.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests
FUNDING
STS Scheme of Indian Council of Medical Research
ETHICS COMMITTEE APPROVAL
This study was approved by the Institutional Ethical Committee at Maulana Azad Medical College, New Delhi. Informed consent was obtained from all study participants.
Please cite this paper as: Sidana S, Kishore J, Ghosh V, Gulati D, Jiloha RC, Anand T. Prevalence of depression in students of a medical college in New Delhi: A cross-sectional study. AMJ 2012, 5, 5, 247-250. http//dx.doi.org/10.4066/AMJ.2012.750.
References
- 1.Vaidya PM, Mulgaonkar KP. Prevalence of depression, anxiety and stress in undergraduate medical students and its correlation with their academic performance. Indian J of Occup Ther. 2007;39:7–10. [Google Scholar]
- 2.Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: A cross-sectional study. Med Educ. 2005;39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 3.Zoccolillo M, Murphy GE, Wetzel RD. Depression among medical students. J Affect Disord. 1986;11:91–96. doi: 10.1016/0165-0327(86)90065-0. [DOI] [PubMed] [Google Scholar]
- 4.Dyrbye LN, Matthew R, Thomas MR, Shanafelt TD. Medical Student Distress: Causes, Consequences, and Proposed Solutions. Mayo Clin Proc. 2005;80:1613–1622. doi: 10.4065/80.12.1613. [DOI] [PubMed] [Google Scholar]
- 5.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of Prime MD Today. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 6.Givens JL, Tjia J. Depressed medical students' use of mental health services and barriers to use. Acad Med. 2002;77:918–921. doi: 10.1097/00001888-200209000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Supe AN. A study of stress in medical students in GS Seth Medical College. J Postgrad Med. 1998;44:1–6. [PubMed] [Google Scholar]