Abstract
Rational
An increasing number of fatal road-accidents have been reported in which ecstasy was found in the blood of drivers. Although, ecstasy is frequently found to have been used in combination with alcohol, studies on the acute effects of ecstasy co-administered with alcohol on driving performance are relatively rare.
Objective
The present study was designed to establish the extent of driver impairment as a consequence of ecstasy or combined ecstasy and alcohol use as compared to driving under the influence of 0.3‰, 0.5‰ and 0.8‰ alcohol. Furthermore, subjective performance was also assessed.
Results
Alcohol and ecstasy mainly influenced automated driving performance such as lateral and speed control. However, small to no effects of the substances were found on more complex driving behaviour. Overall, variance within the different driving measures was high especially when participants were treated with 3.4-methylenedioxy-methamphetamine (MDMA) and alcohol. Furthermore, equivalence testing showed that combined use may lead to impaired driving for some, but not all, drivers. Participants rated their own performance to be slightly worse than normal in both studies. Since driving was actually seriously deteriorated, this was a falsely positive assessment of their condition.
Conclusions
The dissociation between subjective perceptions and objective performance decrements are important notions for traffic safety since this may affect a driver’s judgement of whether or not it is safe to drive. For example, an intoxicated individual might decide to drive because the feelings of alertness caused by MDMA cloud the impairing effects of other drugs such as alcohol, thereby creating a potentially serious risk for traffic safety.
Keywords: Driving simulator, Driving performance, Alcohol, Ecstasy
Introduction
Driving under the influence of drugs is an important public health and road traffic safety related problem (Christophersen and Morland 1997; Drummer et al. 2003; Movig et al. 2004; Mura et al. 2006; Ojaniemi et al. 2009; Schwilke et al. 2006). Several fatal and non-fatal injurious road accidents have been reported in which ecstasy was found in the blood of drivers (Henry 1992; Verschraagen et al. 2007). This is not surprising considering that ecstasy is the second most popular drug in Europe after cannabis (EMCDDA 2010). In fact, the EMCDDA estimates that the life time prevalence (ever used) of ecstasy use for adults (16–64 years) in Europe ranges between 0.3% and 9.6% with current ecstasy use (used last year) estimated to range between 0.1% and 3.7%.
Ecstasy refers to a synthetic substance that is chemically related to amphetamines but differs to some extent in its effects. Whereas amphetamines are mainly known for their energising effects, ecstasy is commonly appreciated for its entactogenic properties. Concretely this means that besides increased feelings of energy after the ingestion of ecstasy, there is also a feeling of euphoria and an intensification of impressions in contact with other people, music and light (Baylen and Rosenberg 2006). The best-known member of the ecstasy group of drugs is 3.4-methylenedioxy-methamphetamine (MDMA), but other analogues are also sometimes found in ecstasy tablets (3,4-Methylenedioxyamphetamine (MDA), MDEA). The drug is commonly used in social scenes such as dance events and is frequently combined with other drugs such as cannabis and amphetamines and (most frequently) alcohol (Brookhuis et al. 2004; Nabben et al. 2007; Mora et al. 2009).
Only, a small number of experimental studies have assessed the acute effects of MDMA on skills related to driving. These studies generally showed that MDMA acted as a psychomotor stimulant that increases arousal and psychomotor function. As such, it was demonstrated that MDMA improved tracking performance (Lamers et al. 2003), psychomotor speed (Dumont et al. 2008, 2010; Lamers et al. 2003) and impulse control (Ramaekers and Kuypers 2006). However, MDMA has also been shown to have a negative effect on skills that are important for driving, for example the impairment of spatial memory performance (Kuypers and Ramaekers 2005; Kuypers et al. 2006, 2007), movement perception (Kuypers and Ramaekers 2005; Ramaekers et al. 2009) and divided attention (Lamers et al. 2003; Kuypers et al. 2007). Furthermore, when combined with alcohol, MDMA’s stimulant effects are generally not strong enough to fully overcome alcohol-induced impairment of psychomotor function (Dumont et al. 2008, 2010; Hernandez-Lopez et al. 2002)
Reports on the acute effects of MDMA co-administered with alcohol on driving performance are also relatively rare (Brookhuis et al. 2004; Kuypers et al. 2006). Kuypers et al. (2006) assessed the influence of 75 and 100 mg MDMA alone and combined with alcohol (average BAC around 0.4‰) on actual driving performance in a within-subjects design. They found that automated driving performance, as measured with the road tracking test (O’Hanlon et al. 1982), was impaired by alcohol (i.e. increased standard deviation of the lateral position; SDLP) but decreased after use of MDMA (both dosages). Moreover, the standard deviation of speed (SDSP) also decreased under the influence of MDMA (both dosages) although it was unaffected by alcohol. Co-administration of 100 mg but not 75 mg MDMA was also found to moderate the alcohol-induced impairment in SDLP. Furthermore, there was no effect of co-administration on SDSP. The responses of drivers to speed changes of a lead vehicle as measured by the car following test (Brookhuis et al. 1994) were unaffected by MDMA (both dosages) alone or when co-administered with alcohol. However, because of the obvious reason that high-risk situations in an experiment on the road cannot be (ethically) acceptable, other more complex interactions with traffic participants and risk taking in traffic could not be investigated in this study. Brookhuis et al. (2004) on the other hand used a driving simulator to test MDMA effects and could therefore safely assess the more high-risk aspects of driving.
In this latter study, recreational ecstasy users who were going to a dance party drove in the simulator before going to the party, 1 hour after the use of their own, self-bought and self-administered ecstasy (average MDMA, 59 mg). After the party, they were tested again while they were under the influence of MDMA and various other substances such as (in 80% of the cases) marihuana and (in 90% of the cases) alcohol (an average BAC of 0.39‰ once back in the lab approximately 1 h after the party). The participants were also tested in a sober condition on a different day at a comparable time. The results indicated that SDLP was unaffected by MDMA alone but was impaired by multidrug use. From non drug to MDMA and from MDMA to multi drug both speed and SDSP increased. As found in the on-road study, performance on the car following test was unaffected in both drug conditions. However, measures of risk taking and situation awareness in complex traffic situations were affected by multidrug use (increased gap time and an increased number of crashes). Because of the quasi-experimental design, i.e. no control over the active substances, however, it is hard to draw straightforward conclusions from this experiment on the influence of combined alcohol and MDMA use on critical aspects of driving performance.
Therefore, the aim of the present study was to investigate the risks involved in driving under the influence of MDMA (100 mg) alone and when co-administered with alcohol (0.5‰) in a controlled environment, i.e. in driving simulator, with in controlled design. What is more to determine the implications of the results for traffic safety? To this end a double blind ‘alcohol reference’ study was initially performed. In this study (study 1) the influence of three levels of alcohol (0.3‰, 0.5‰ and 0.8‰) were tested against a placebo condition on a set of measures within specifically developed scenarios, similar to the ones later used in the study on MDMA and driving (study 2).
According to Dumont et al. (2010), MDMA may provide a sense of adequate performance that is not in accordance with actual performance. This is an important notion for traffic safety and therefore subjective effects are also assessed.
Study 1: alcohol reference study
Methods and materials
Participants
Nineteen participants started the study; however, two dropped out during the experiment due to physical problems not related to the experiment. Therefore, data of 17 participants (nine males, eight females) with an average age of 23.6 (SD = 3.8) years were analysed. The participants were all experienced drivers who had held their driving licence for at least 3 years (mean (SD), 4.52 (1.98)) and drove at least 5,000 km per year. All participants were in good health and reported no prior problems with drug or alcohol abuse. Participation was voluntary and participants received a monetary bonus.
Study design
The study was conducted according to a double-blind, placebo-controlled, four-way cross-over design with treatment orders counterbalanced. Participants were presented with alcoholic drinks leading up to a BAC of 0.3‰, 0.5‰ or 0.8‰ and a placebo which looked and smelled like an alcoholic beverage but contained no alcohol.
Procedure
The participants were instructed to abstain from alcohol in the 24 h prior to the experiment and to refrain from caffeinated beverages on the morning of the experiment. They were then tested during five separate testing days. Each test day started between 1 p.m. and 3 p.m. The first testing day started with a screening of the participants by questioning them about their lifestyle in relation to alcohol and drugs using the Drug Abuse Screening Test-10 (Skinner 1982). After this screening the participants were trained in the simulator for 30 min. In this training the participants practised all of the driving scenarios in a full dress rehearsal and were screened for simulator sickness.
On the other four testing days, participants were given beverages containing vodka (40%) filled up with orange juice until the intended BAC was reached (as measured by a Dräger Alcotest® 7410 Plus breathalyzer) or only orange juice with a spray of alcohol on top as a placebo. The amount of administered alcohol was dependent on the weight, height and gender of the participant and was calculated using the Widmark formula (Widmark 1932). The driving test was then conducted 20 min post-alcohol intake and took approximately 50 min.
In order to keep the participant at a constant alcohol level, the test was paused every 20 min to do a breath analysis and administer extra alcohol when necessary. The tests differed in the order of occurrence in different sessions to prevent the participants from anticipating the critical moments during the scenarios. After the driving task, the participants were asked to fill in questionnaires and had to wait in waiting room until they were able to return home safely. The participants were only allowed to leave when their BAC was below 0.1‰. The study was approved by the ethical committee of the Department of Psychology at the University of Groningen.
Apparatus
Participants were required to complete test rides in a (fixed-base) driving simulator consisting of a mock-up car with original controls (three pedals, clutch, steering wheel, safety belt, indicator and hand brake) linked to a dedicated graphics computer, registering driver behaviour while the road environment and dynamic traffic are computed at 30 Hz+. Participants had a 180º view of the road environment (see Fig. 1. for an illustration). Other vehicles in the simulated world interact with each other and the simulator car autonomously, and behave according to hierarchically structured decision rules that are based on human driving behaviour (Van Wolffelaar and Van Winsum 1992).
Fig. 1.

Illustration of the driving simulator
A virtual world, including relevant scenarios for testing, the effects of alcohol and drugs was developed for these studies; see Veldstra et al. (2009), for a detailed overview. The virtual environment consisted of several road types: urban (6.5 km), rural (22.6 km) and motorway (9.8 km). Average traffic densities were used on all of these road types.
Driving tasks assessing automated driving performance
Speed management
Speed was assessed on all road types. Participants under the influence of alcohol might lower their speed to compensate for sedating effects. On the other hand, stimulating drugs such as MDMA might make the participant want to speed up because hazard perception is decreased (see also Brookhuis et al. 2004). Another compensating mechanism in speed management is (deliberately) varying speed. In the case of severe sedation, a participant might temporarily increase speed to increase feelings of arousal, indicated by an increase in the standard deviation of speed (Brookhuis 1998). Therefore, besides average speed, the SDSP was assessed as well.
Road tracking task
On two rural roads of approximately 10 km (posted speed 100 km/h) road tracking was monitored. The road tracking task is designed to measure involuntary (unconscious) response errors, or tracking errors, calculated as the SDLP (O’Hanlon et al. 1982).
Driving tasks assessing complex driving performance
Car following
Response to other traffic participants was assessed using a car following test on a rural road (Brookhuis et al. 1994). In this scenario the participant was instructed to follow a lead car at a short but safe distance. The lead car was programmed to change speed between 60 and 80 km/h and to accelerate and decelerate within a randomly varied frequency of between 0.025 and 0.05 Hz (20 and 40 s.). The participants’ reactions to these speed changes were measured by assessing the coherence, the gain and most importantly, the delay in their responses. The coherence is the extent to which the patterns of speed changes of the lead- and following car correspond. So, if the participant is not following speed changes of the lead car properly, the coherence would be low. However, if the participant is following as instructed coherence would be high. After coherence is established, the style of following can also be analysed. This is done by assessing the gain and the delay. The gain is a measurement of the type of speed reaction the participants had to the speed changes of the lead car and is returned as an amplification factor between the speed signals of the lead- and follow car. When there is an overreaction, the gain is larger than one, while at an underreaction, the gain is smaller than one. The delay (technically, phase shift between the two speed signals) is the response time of the participant to the speed changes of the lead car (see Brookhuis et al. 1994; De Waard and Brookhuis 2000).
Gap acceptance
The gap acceptance task was used to asses risk taking in traffic (Adams 1995). In this task, participants drove on a two lane urban road with a posted speed limit of 50 km/h and had to turn left at a y-junction through a stream of oncoming traffic that had the right of way. The time between each of the cars in this stream increased every 1 s, ranging from 1 to 12 s. In this task the driver had to weigh the waiting time versus the risk of causing an accident and come to a decision to either choose a small risky gap, with a short waiting time or a larger, safer gap with a longer waiting time. The parameters included to assess the drivers risk taking were: the size of the chosen gap in seconds and the distance to the car approaching the driver while traversing the crossing. Accordingly, lower gap time (in seconds) and a smaller distance to the approaching car entails riskier behaviour.
Running red lights
Analyses of driver records of patients that admitted substance abuse showed that drug users had significantly more traffic violations than a non-drug control group (MacDonald et al. 2004). Therefore, the violation of traffic regulations was assessed by a traffic light scenario developed by De Waard et al. (1999). In this scenario the participant approached a green traffic light that turned amber just 2 s before the participant would be passing the light (posted speed 50 km/h). If participants kept the same speed they would drive through red, if they sped up they would most likely drive through amber and if they wanted to stop they had to brake firmly. The choice of the participant was determined by assessing the colour of the traffic light at the moment of crossing.
Car pulling out of a car park
Alcohol intoxication and sedation by (medicinal) drugs has been associated with significant deterioration in attention and reaction time (Kelly et al. 2004). A scenario used to measure the driver’s reaction to unexpected events was a scenario in which a car pulled out of a car park while driving in an urban area (posted speed 50 km/h). The dependent measure was the minimal time to collision.
Crashes
Even though crashes tend to occur more frequently in a driving simulator than in real traffic, it is still an important indicator of driving safely. Having a crash is the ultimate outcome of an unsafe act (Brookhuis et al. 2004). Therefore, the total number of crashes during the entire ride was assessed.
Subjective measures
Karolinska sleepiness scale
A modified version of the Karolinska Sleeping Scale (KSS; Reyner and Horne 1998) was used to assess the participants’ own feeling of alertness before and after driving. Scores ranged from 1 (‘extremely alert’) to 9 (‘Sleepy, I have to fight not to fall asleep’).
Rating scale mental effort
The Rating Scale Mental Effort (RSME; Zijlstra 1993) was used to assess whether there was a difference in the mental effort participants had to invest during the driving session for the different alcohol conditions.
Driving quality scale
Using the Driving Quality Scale developed by Brookhuis et al. (1985), the participant had to judge his or/her own performance. Driving quality was rated by driver on a 10-cm visual analogue scale (0 = poor; 10 = excellent).
Data analysis
All statistical analyses were conducted by means of SPSS 16 for Windows. Normally distributed data were subjected to a general linear model univariate repeated measures analysis with alcohol level (four levels) as main within-subjects factor. If the Mauchly’s test indicated that the assumption of sphericity was violated, the degrees of freedom were corrected using the Greenhouse–Geisser correction. On the non-normally distributed data, Friedman’s tests were performed and contrasts were explored with the Wilcoxon exact test. Dichotomous data were subjected to a Cochran’s test. Missing values were corrected by replacing them with the mean of the participant over all conditions (i.e. ipsative mean imputation; Shafer and Graham 2002). This technique was chosen to preserve the data. Replacement of missing values with individual means was chosen over replacement with overall mean values to prevent the downward attenuation of variance.
Results
Pharmacokinetic assessments
The average alcohol levels in the three alcohol administration conditions as measured by breath analyses were: 0.28‰ (SD = 0.05), 0.49‰ (SD = 0.08) and 0.80‰ (SD = 0.10).
Automated driving performance
Speed management
Average (+SE) performance scores and p values for all driving tasks are displayed in Table 1. A main within-subjects effect of alcohol level on speed was revealed in the urban driving setting (F (2.29) = 3.44, p < 0.05). The average speed was not above the posted speed but participants tended to drive faster when their alcohol level was above 0.5‰ as compared to placebo (on average 1.3 km/h (SE = 0.58) faster (F (1) = 5.37, p < 0.05) when BAC was 0.5‰ and on average 1.47 km/h (SE = 0.76) faster (F (1) = 3.8, p = 0.068) when BAC was 0.8‰). There was no effect of alcohol level on speed when driving on the rural road and motorway. Also, there was no effect of alcohol on SDSP for any of the road types.
Table 1.
Average (SE) of the driving tasks for all treatment conditions in study 1
| Driving task | Placebo | Alcohol 0.3‰ | Alcohol 0.5‰ | Alcohol 0.8‰ | Main within subjects effect |
|---|---|---|---|---|---|
| Road tracking | |||||
| SDLP (cm) | 15.77 (0.01) | 17.71 (0.01) | 17.88 (0.01) | 19.88 (0.01) | F (2.29) = 3.44, p < 0.05 |
| Speed (km/h) | 100.5 (2.6) | 95.5 (2.4) | 100.3 (1.8) | 99.4 (2.2) | χ 2 (3) = 5.26, n.s |
| SD speed (km/h) | 1.6 (0.3) | 1.8 (0.3) | 1.6 (0.3) | 2.4 (0.5) | χ 2 (3) = 6.0, n.s |
| Car following | |||||
| Coherence | 0.89 (0.02) | 0.90 (0.01) | 0.88 (0.02) | 0.87 (0.03) | χ 2 (3) = 1.0, n.s |
| Gain | 0.84 (0.3) | 0.87 (0.3) | 0.82 (0.3) | 0.78 (0.2) | χ 2 (3) = 2.87, n.s |
| Delay | 3.49 (0.3) | 3.35 (0.3) | 3.67 (0.3) | 3.31 (0.2) | χ 2 (3) = 2.2, n.s |
| Motorway driving | |||||
| Speed (km/h) | 105.96 (3.9) | 108.7 (3.7) | 111.9 (3.9) | 107.3 (5.4) | χ 2 (3) = 1.87, n.s |
| Sd speed (km/h) | 2.7 (0.2) | 2.7 (0.3) | 2.5 (0.2) | 2.8 (0.3) | F (2.56) = 0.46, n.s |
| Urban Driving | |||||
| Speed (km/h) | 35.9 (0.6) | 35.9 (0.6) | 37.3 (0.7) | 37.4 (0.6) | F (2.29) = 3.44, p < 0.05 |
| Sd speed (km/h) | 17.5 (0.3) | 17.5 (0.3) | 17.6 (0.4) | 17.5 (0.5) | F (2.84) = 0.09, n.s |
| Gap acceptance | |||||
| Gap time (s) | 5.7 (0.3) | 5.7 (0.3) | 5.4 (0.3) | 5.5 (0.3) | χ 2 (3) = 0,913, n.s |
| Distance to car (m) | 53.3 (5.1) | 48.5 (5.1) | 46.7 (4.11) | 41.0 (6.7) | F (2.81) = 0.36, n.s |
| Car pulling out of parking | |||||
| TTC | 1.61 (0.15) | 1.26 (0.18) | 1.58 (0.33) | 1.42 (0.11) | χ 2 (3) = 1.255, n.s |
| Running red light | χ 2 (3) = 5.53, n.s | ||||
| (% running red) | 23.5 | 11.8 | 29.4 | 35.3 | |
| (% running amber) | 0 | 0 | 0 | 0 | – |
| No. of crashes | 3 | 0 | 2 | 1 | – |
Significance indicated by p value
Road tracking
As expected, there was a main within-subjects effect of alcohol level on SDLP (F (2.08) = 5.68, p < 0.05). As compared to the placebo, SDLP was decreased for 0.3‰ (−2.0 cm (F (1) = 12.07, p < 0.05)), 0.5‰ (−2.1 cm (F (1) = 4.15, p < 0.05)) and 0.8‰ alcohol (4.1 cm (F (1) = 10.12, p < 0.05)).
When comparing the different alcohol levels to each other, contrast analyses revealed that the difference between the SDLP with alcohol levels 0.3‰ and 0.5‰ was not significant (F (1.0) = 0.190, n.s.). However, the SDLP difference between a 0.5‰ and 0.8‰ alcohol level was significant (F (1.0) = 5.165, p < 0.05).
Complex driving performance
There was no within-subjects effect of alcohol level on running red lights, reaction to the car pulling out of a car park or the number of crashes (see Table 1).
Car following
There was no main within-subject’s effect of alcohol level on any of the car following measures. Overall the coherence was high (average, 0.88 (SE, 0.014)), indicating that participants were accurate in their speed adaptations as reaction to the speed changes of the lead car; this means that they were following the lead car as instructed.
Gap acceptance
There was no significant main effect of alcohol level on gap times. When looking at the participants distance to the approaching car, at the moment of crossing the junction, it seems that participants generally accepted a smaller distance when alcohol level was higher; however, this effect was non-significant (F (2.81) = 0.36, p < 0.094) at the p = 0.05 level.
Subjective measures
Karolinska sleeping scale
There was an overall effect for time on task on the KSS (pre vs. post driving; F (1) = 19.39, p = 0.001), with participants rating themselves as more sleepy post driving. There was, however, no alcohol effect. Although the time on task effect appeared to increased with alcohol level, the interaction effect of alcohol and time was not significant (F (2.78) = 2.56, p = 0.07) at the p = 0.05 level.
Rating scale mental effort
There was an overall effect of alcohol on ratings of mental effort (F (2.35) = 4.07, p < 0.05). Participants rated their invested effort as higher in the alcohol conditions as compared to the placebo condition. Contrast tests revealed that this difference was significant for the 0.5‰ alcohol condition (F (1) = 12.04, p < 0.05) and the 0.8‰ alcohol condition (F (1) = 4.76, p < 0.05).
Driving quality scale
There was no effect of alcohol on the subjective assessment of driving performance. Participants rated their performance to be slightly worse than normal in all conditions.
Treatment evaluation
More than half of the participants guessed the amount of alcohol they had received correctly (between 56% and 71%). The highest rate of correct guesses was in the 0.8‰ alcohol condition (71%). Binomial tests were applied to measure whether the proportion of participants guessing the condition they were in correct significantly differed from chance level (25%). However, tests revealed no significant difference for any of the alcohol conditions.
Discussion and conclusions
The results of the alcohol study indicate that alcohol mainly influenced automated driving performance such as speed control and weaving (SDLP). Speed on urban roads increased when BAC was above 0.5‰. However, this increase was small and did not exceed the posted speed. SDLP increased as a function of BAC, indicating that participants were weaving increasingly more as they were under the influence of higher alcohol levels, comparable to the well-known Borkenstein curve (Borkenstein et al. 1964) and as also reported by Louwerens et al. (1987).
Car following was performed adequately as reflected in a high coherence values; however, we found no effects of alcohol on any of the car following measures. Previous research on the influence of alcohol on car following measures has been ambiguous. For example, De Waard and Brookhuis (1991) reported a 19% increase in delay under the influence of an alcohol level of 0.46‰, but no effect on gain, whereas Kuypers et al. (2006) reported no significant effect of alcohol (at 0.37‰) on delay or gain.
The aim of study 1 was to serve as a reference for driving under the influence of MDMA and combined MDMA and alcohol in automated but also in more complex driving tasks. However, the majority of the scenarios in which more complex driving performance was assessed showed no significant differences from the placebo and could therefore not be used as references for the second study. For only one scenario, an effect of alcohol on performance was found, namely the gap acceptance scenario.
Since drug-affected drivers have demonstrated reduced perceptions of risk (Brookhuis et al. 2004), one might have expected to find a smaller gap time when BAC was higher. However, participants selected approximately the same gap irrespective of their BAC. Only the average distance of the participants to the approaching car at the moment of crossing was affected by alcohol, in that the average distance was smaller when BAC was higher. Since the perceptual motor capacities necessary for crossing the junction tend to be affected by alcohol, both in speed and coordination (Tarter et al. 1971), it probably took the participants a bit longer to initiate a reaction. One could argue that the participants were taking a greater risk by accepting the same gap while ignoring initiation capabilities. It would have been safer to wait for a larger gap, since it would take more time to cross.
As stated, the effects of alcohol were mainly found on automated driving performance and were not found in the scenarios where more complex driving behaviour was measured. This might be due to the dynamic nature of these kinds of tasks. Since the scenarios measuring complex driving performance are so dynamic, they allow for different strategies to compensate for intoxicating effects. For example, where one participant might have reduced speed to have an increased reaction time to unexpected events, another might have adopted an alternative strategy in which altering speed was not necessary. For automated driving tasks, these compensatory strategies are limited and may therefore be more sensitive to drug-induced effects. Fairclough and Graham (1999) hypothesised that compensatory responses are triggered by the awareness and subjective discomfort of reduced performance efficacy. Although the current study was double blind, the majority of the participants still guessed the alcohol condition they were in correctly and may perhaps have responded by compensating for the impairing effects. One way in which they did this was by investing more mental effort, since scores on the RSME increased for the higher alcohol levels. This might also explain why participants felt they had not driven any worse under the influence of any of the alcohol conditions as compared to the placebo when asked to rate their own driving performance.
In conclusion, the effects of alcohol were mainly found on automated driving performance such as weaving and speed control. Therefore, these are the main parameters that will serve as references for the second study on the influence of MDMA and alcohol on driving performance.
Study 2: the effects of MDMA and alcohol
Methods and materials
Participants
Participants were recruited by flyers distributed at the University of Groningen. In the beginning 20 volunteers participated in this study. However, one participant did not comply with the rules of participation and was therefore discarded from further analyses. This participant tested positive for MDMA in the placebo condition even though he had tested negative in the urine drug screen as was conducted at the start of every testing day. This became apparent during the post hoc pharmacological analyses. Therefore, 19 healthy volunteers (ten males, nine females) aged between 21 and 40 years (mean (SD), 30.8 (5.65)) were used for further analyses. They were all experienced drivers who had held their driving licence between 3 to 20 years (mean (SD), 8.8 (5.7)) and had all used MDMA before participating in the study (lifetime use varied between 10 and 100 pills). Moreover, they had experience with alcohol use but were not abusers (participants on average drank 7.8 (SD = 5.8) alcoholic beverages per week).
Participants were medically examined by a medical supervisor. Vital signs were checked and standard blood chemistry was examined. Inclusion criteria were: experience with the use of MDMA (at least five times in the past 12 months); experience with the use of alcohol (2–20 consumptions a week); free from psychotropic medication; good physical health as determined by examination and laboratory analysis; good medical, endocrine and neurological condition; normal weight, body mass index between 18 and 28 kg/m2; a valid driving licence (minimum 3 years); driving experience with a minimum of 5,000 km per year and written informed consent. Exclusion criteria were: a history of drug abuse or addiction as determined by examination; excessive drinking (>20 alcoholic consumptions a week); current or history of psychiatric disorder; history of malignant hyperthermia/serotonin syndrome; cardiovascular abnormalities as assessed by standard ECG; hypertension (diastolic >100; systolic >170); pregnancy, lactation or wishing to become pregnant during the period of the study; participation in any clinical trial including blood sampling and/or administration of substances up to 6 weeks before the study and susceptibility to simulator sickness (participants were pre-tested).
This study was conducted according to the code of ethics on human experimentation established by the declaration of Helsinki (latest revision, Seoul 2008) and in accordance with the Medical Research Involving Human Subjects Act (WMO). Approval for the studies was obtained from the Medical Ethics Committee of the University Medical Centre of Groningen and the Dutch Central Committee on Research Human Subjects (CCMO). A permit for obtaining, storing and administering MDMA was obtained from the Dutch drug enforcement administration.
Design and treatment
The study design was a double-blind, placebo-controlled, four-way crossover design with treatment orders counterbalanced according to a Latin square. On the testing days, the participants randomly received a single dose of 100 mg MDMA, or placebo, and a single dose of alcohol (aiming at BAC 0.5‰) or placebo. The placebos, alcohol and MDMA where administered orally. Alcohol was administered according to the same procedure as in the alcohol reference study (study 1) and MDMA and placebo–MDMA were administered in a capsule. MDMA (or placebo) was obtained from Duchefa Pharma B.V. Haarlem, Nl, the Netherlands and encapsulated according to EU Good Manufacturing Practice by Basic Pharma Geleen, N1, the Netherlands.
Procedure
After there was no medical objection for participation, participants were invited to come in for a training day to check for simulator sickness and to practise all of the driving scenarios in a full dress rehearsal. After the training day, participants visited the facilities four additional times (1 day for each condition), with a washout period of 1 week in between. Participants were asked to refrain from any drugs starting 1 week before the screening and during the whole study period. Drug screens in urine and alcohol screened in breath were conducted before the start of every testing day. Female participants were also screened for pregnancy. Participants were allowed to take part on the testing day only if they had passed these screenings. Furthermore, participants were asked to refrain from alcohol and on the day prior to the testing day and from caffeinated beverages on the testing day itself. Participants were compensated for their participation by means of a monetary reward.
Pharmacokinetic assessment
Two blood samples (10 ml) were taken 1.5 h post-drug. One sample was centrifuged after collection for 15 min at ca. 2,000 rpm at ca. 4°C for the extraction of serum. Saliva was collected every hour until 7 h post-drug-intake with a StatSure’s Saliva Sampler (®). After collection all samples were stored at −20°C until further analyses. Furthermore, dried bloodspots were collected by finger prick for a special drug assessment kit provided by the University of Heidelberg in order to investigate a new less invasive way of testing for drugs in blood (Jantos et al. 2011).
Driving tasks
Driving tests were conducted between 1.5 and 3.5 h post MDMA (30 min after the first alcohol administration 10 min after subsequent administrations). Alcohol level was kept constant during all parts of the drive. The same measures employed in study 1 were also used in study 2.
Subjective measures
The same subjective measures employed in study 1 were also used in study 2. In addition, we asked participants in the introduction session how they thought the different drug conditions would influence their driving performance on a scale ranging from 0 (worse) to 12 (better). We then asked them again after every driving session, to see whether they thought that the drug they had had may have influenced their driving performance.
Data analysis
Treatment effects were handled in the same way as in study 1. After the assessment of treatment effects, a so called equivalence test was conducted on measures in which the treatment effect in the alcohol reference study was significant. In this test the equivalence of drug effects based on the difference to the placebo were compared to the criterion levels as established in the alcohol reference study. Equivalence was tested by assessing if the pre-established criterion levels fell within the 95% confidence interval of the drug effects. If this was so, then the drug effect was considered to be clinically relevant (Mascha and Sessler 2011). Furthermore, concentration-effect relations were determined by regressing concentrations of MDMA in blood and saliva for both the MDMA- and MDMA co-administered with alcohol condition to behavioural measures.
Results
Pharmacokinetics
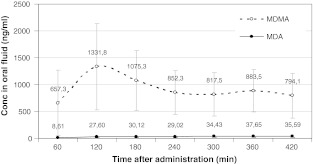
BAC levels were 0.48‰ (SD = 0.11) for the alcohol-alone condition and 0.50‰ (SD = 0.11) for the alcohol–MDMA condition. MDMA and MDA concentrations in blood (serum, whole blood and dry bloodspots) and oral fluid were comparable between treatments (see Table 2 and for further analyses see also Jantos et al. 2011). As can be seen in Fig. 2, MDMA in saliva peaked 2 h after intake and decreased in the 2 h following. Hereafter, the level was relatively stable for the remaining hours that were measured. Measures of MDMA concentration in dried blood and whole blood correlated weakly with peak concentrations in oral fluid (r = 0.324, p = 0.07 for both dried blood spots and whole blood). There was no correlation between serum and oral fluid MDMA concentrations. This is in line with Samyn et al. (2002).
Table 2.
Average (SD) concentration MDMA and MDA in blood (mg/ml) for both the MDMA and MDMA co-administered with alcohol condition
| MDMA | MDA | |||
|---|---|---|---|---|
| MDMA | MDMA and alcohol | MDA | MDA and alcohol | |
| Serum | 150.72 (144.95) | 135.45 (131.38) | 3.13 (3.66) | 3.21 (3.10) |
| Whole blood | 170.41 (160.22) | 159.25 (148.68) | 6.69 (7.79) | 5.67 (6.57) |
| DBS | 173.70 (164.22) | 162.50 (152.76) | 6.52 (7.74) | 6.28 (6.76) |
Fig. 2.
Average (95% CI) nanograms per millimeter MDA and MDMA in saliva per hour after intake
Automated driving performance
Mean (SE) performance scores for all driving tasks and p values for main treatment effects are displayed in Table 3
Table 3.
Average (SE) of the driving tasks for all treatment conditions in study 2
| Driving task | Placebo | Alcohol | MDMA | MDMA with alcohol | Main within- subjects effect |
|---|---|---|---|---|---|
| Road tracking | |||||
| SDLP (cm) | 21 (1.2) | 24 (1.3) | 19 (1.0) | 22 (1.3) | F (2.72) =6.16, p < 0.005 |
| Speed (km/h) | 105.8 (2.2) | 105.8 (2.8) | 102.24 (1.4) | 104.1 (2.0) | χ 2 (3) = 8.21, p <0.05 |
| SD speed (km/h) | 3.0 (0.6) | 4.5 (0.9) | 2.5 (0.3) | 3.7 (0.6) | χ 2 (3) = 10.33, p < 0.02 |
| Car following | |||||
| Coherence | 0.74 (0.06) | 0.81 (0.03) | 0.75 (0.05) | 0.79 (0.03) | χ 2 (3) = 1.80, n.s. |
| Gain | 5.2 (0.6) | 4.8 (0.5) | 5.5 (0.6) | 4.6 (0.4) | χ 2 (3) = 1.86, n.s. |
| Delay | 0.73 (0.05) | 0.77 (0.06) | 0.75 (0.05) | 0.79 (0.05) | F (2.52) = 0.59, n.s. |
| Motorway driving | |||||
| Speed (km/h) | 121.7 (3.2) | 119.8 (4.0) | 118.6 (2.5) | 121.5 (3.8) | χ 2 (3) = 4.45, n.s. |
| Sd speed (km/h) | 6.3 (0.8) | 6.6 (0.9) | 6.3 (1.0) | 7.2 (1.2) | F (2.16) = 0.23, n.s. |
| Urban driving | |||||
| Speed (km/h) | 46.7 (0.9) | 47.0 (1.0) | 48.2 (0.8) | 47.6 (1.3) | F (2.77) = 0.94, n.s. |
| Sd speed (km/h) | 5.6 (0.3) | 5.8 (0.2) | 5.1 (0.4) | 6.1 (0.4) | F (2.66) = 2.75, n.s. |
| Gap acceptance | |||||
| Gap time (s) | 4.0 (0.2) | 4.1 (0.2) | 4.1 (0.2) | 4.0 (0.2) | F (2.52) = 0.25, n.s. |
| Distance to car (m) | 30.6 (1.9) | 32.2 (2.1) | 32.3 (1.9) | 32.9 (2.3) | F (2.51) = 0.63, n.s. |
| Car pulling out of parking | |||||
| TTC | 1.39 (0.09) | 1.30 (0.09) | 1.27 (0.11) | 1.31 (0.09) | χ 2 (3) = 3.26, n.s. |
| Running red light | χ 2 (3) = 5.56, n.s. | ||||
| (% running red) | 63.2 | 52.6 | 68.4 | 68.4 | – |
| (% running amber) | 5.3 | 0 | 0 | 10.5 | – |
| No. of crashes | 1 | 2 | 2 | 3 | – |
Significance indicated by p value
Speed management
Participants kept to the posted speed on all road types. However, on the rural roads where they could drive more freely, the participants showed a main effect of treatment on speed (χ 2 (3) = 8.21, p <0.05). Simple contrasts analyses revealed that this difference stems mainly from a decrease in speed in the MDMA condition as compared to the placebo condition (average ∆ (SE), 0.95 km/h (0.36); Z = 2.66, p < 0.05). Moreover, there was a main effect of treatment on the SDSP when participants were driving on the rural road (χ 2 (3) = 10.33, p < 0.02). The SDSP was higher when participants were driving under the influence of alcohol 0.5‰ as compared to the placebo (average ∆ (SE), 0.41 km/h (0.30); Z = 2.05, p < 0.05). Furthermore, there was an interaction effect of alcohol (0.5‰ and placebo) and MDMA (100 mg and placebo) on SDSP. The SDSP was significantly lower when driving under the influence of MDMA than when under the influence of alcohol (average ∆ (SE), 0.55 km/h (0.24); Z = 2.61, p < 0.05).
Road tracking
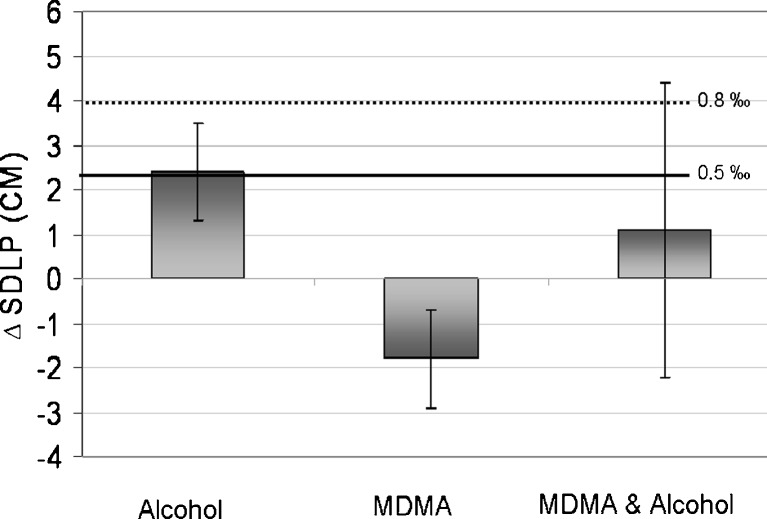
As expected, there was a main within-subjects effect of treatment on weaving, measured as the SDLP (F (2.72) = 6.16, p < 0.005). As can be seen in Fig. 3, compared to placebo, SDLP increased 1.11 cm under the influence of combined alcohol and MDMA administration. However, this difference was not significant (F (1) = 1.12, n.s). Moreover, SDLP increased 2.42 cm under the influence of alcohol (F (1) = 5.3, p < 0.05) and decreased 1.84 cm under the influence of MDMA (F (1) = 5.3, p < 0.05). This interaction effect of ∆ SDLP when treated with BAC 0.5‰ and ∆ SDLP when treated with MDMA was also significant (F (1) = 15.17, p < 0.001). Although ∆ SDLP when treated with MDMA alone was significantly lower than SDLP under the influence of BAC 0.5‰ for the combined treatment of MDMA and alcohol, it was not (F (1) = 1.61, n.s). When comparing average ∆ SDLP under the influence of BAC 0.5‰ in the current study with the first study, no significant difference was found (t (34) = 0.204, n.s.). Therefore, equivalence could be tested. Equivalence testing demonstrated that increments in SDLP when treated with combined alcohol 0.5‰ and MDMA were equivalent to the pre-established margin at BAC 0.5‰ and even 0.8‰. When looking at the 95% confidence interval for the ∆ SDLP under the influence of combined alcohol and MDMA (see Fig. 3), one can see that the upper bound clearly exceeds the pre-established margins of both BAC 0.5‰ (2.1 cm) and BAC 0.8‰ (4.1 cm). This indicates that within the range of possible means an average SDLP impairment that is larger than impairment under BAC 0.5‰ or even BAC 0.8‰ could be found. T tests comparing the two criterion levels to ∆ SDLP in the combined treatment condition confirm this assertion since they showed no significant difference when compared with BAC 0.5‰ (t (34) = 0.68, n.s) and BAC 0.8‰ (t (34) = −1.83, n.s.). However, the lower bound of the confidence interval spreads over the null line as well; indicating that a subset of individuals may show no impairment or even an average improvement (i.e. decrease) in SDLP as compared to the placebo.
Fig. 3.
SDLP, average difference to placebo and 95% CI per condition for road tracking and equivalence to alcohol–placebo difference at levels 0.5‰ and 0.8‰ as established in study 1
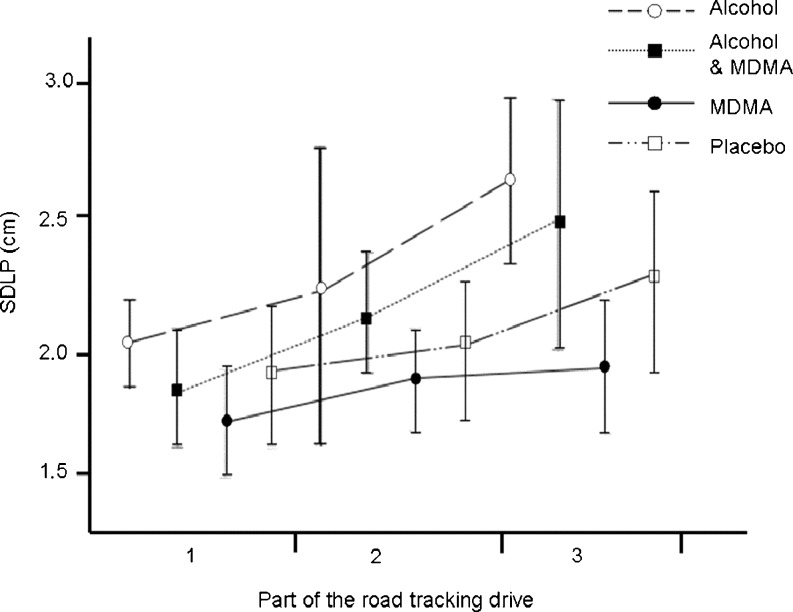
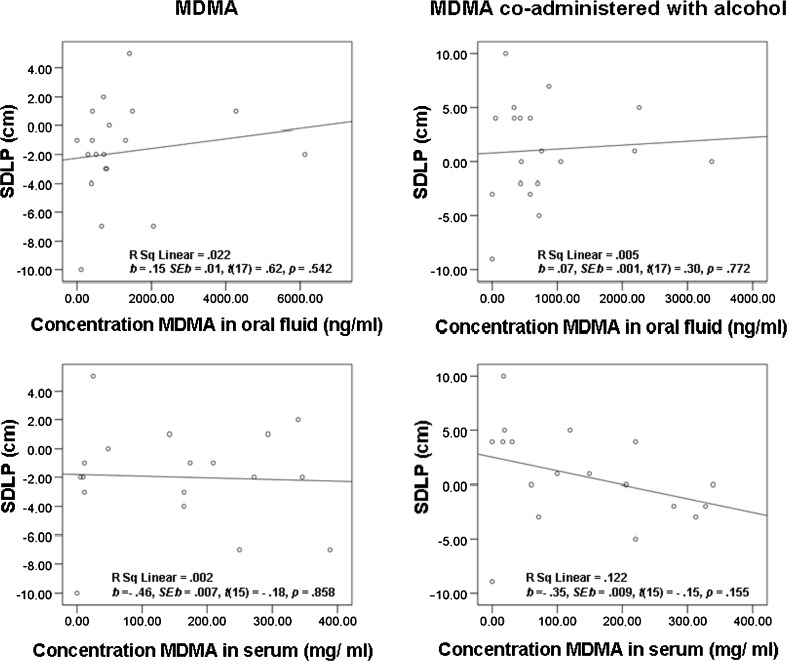
Analyses reveal that there was an effect of time on task for SDLP (F (1.93) = 12.05, p < 0.001). Overall SDLP increased over time (see Fig. 4). Furthermore, there was a slight effect for the treatment by time interaction (F (6) = 2.45, p = 0.088). As can be seen in Fig. 4, SDLP increases sturdily with time in all conditions except in the MDMA condition in which it only increase lightly. Regression of the SDLP differences to placebo in both the MDMA- and MDMA co-administered with alcohol condition on drug concentrations in saliva and serum showed a general lack of association (see Fig. 5).
Fig. 4.
Average SDLP and 95% CI per treatment condition as function of part of the road tracking drive
Fig. 5.
Regression lines for SDLP difference to placebo and MDMA concentrations in serum and saliva during driving tests when treated with MDMA and MDMA co-administered with alcohol
Complex driving performance
There was no within-subjects effect of alcohol level on gap acceptance, running red lights, the car pulling out of a car park scenario or the number of crashes.
Car following
There was no main within-subject’s effect of treatment on any of the car following measures. Overall the coherence was lower than in study 1 (average (SE), 0.77 (0.03)) but even when correcting for the low coherence by only analysing participants with a coherence of above 0.75; there was no main effect of drug conditions on any of the car following measures.
Subjective measures
Treatment evaluation
At the end of every session, participants were asked in which condition they thought they were in. The majority of participants guessed correctly (between 68% and 89%). Binomial tests were applied to measure whether the proportion of participants guessing the condition they were in correct significantly differed from chance level (25%). For all conditions except the MDMA co-administered with alcohol condition, this was the case.
Driving quality assessment
When asking participants in the introduction session how they thought the different drug treatments would influence their driving performance, participants predicted their performance to be worse than normal. Furthermore, participants thought their driving would deteriorate more when treated with combined alcohol and MDMA as compared when they were treated with alcohol only (Z = 2.60, p < 0.009) or only with MDMA (Z = 2.42, p < 0.05). After testing the participants were asked if the treatment they thought that they had had may have influenced their driving performance. Overall, participants thought that the drug treatment that they had received would still make them drive a little worse than normal. However, this time they expected that the influence on their driving performance did not differ between treatments. Furthermore, we compared the pre-driving test subjective ratings with post-driving test ratings of participants who had guessed the treatment they had received correctly. Participants rated the influence of the treatment on their performance worse in the pre- as compared to the post-driving test. This difference was significant for both the MDMA (Z = 2.6, p < 0.007) and the combined MDMA/alcohol condition (Z = 2.52, p < 0.008), but not for the alcohol condition (Z = 2.39, p = n.s). There was, however, no effect of treatment on self rated driving quality (χ 2 (4) = 1.68, n.s.).
Rating scale mental effort
There was no effect of treatment on the RSME (χ 2 (4) = 0.84, n.s).
Karolinska sleepiness scale
The average ratings of alertness as measured by the KSS pre-driving test were equal over all conditions. However, participants gave higher average ratings post- driving test as compared to pre-driving test (χ 2 (7) = 32.81. p < 0.001), indicating that they rated themselves as less alert after the driving tests. Analyses of contrasts reveal that this difference was significant for the placebo (Z = 2.48, p < 0.05), alcohol (Z = 3.02, p < 0.001) and combined alcohol–MDMA (Z = 2.16, p < 0.05) conditions but not for the MDMA only condition (Z = 1.04, n.s).
Discussion and conclusions
The effect of 0.5‰ alcohol on weaving in this study was very similar to the effect of alcohol 0.5‰ found in the alcohol reference study. Moreover, an increase in SDLP of about 2.4 cm is almost identical to findings in other simulator- (Thompson et al. 2010) and on-road-driving studies (Kuypers et al. 2006; Louwerens et al. 1987; Ramaekers et al. 2006). As reported before in other studies (Ramaekers and Kuypers 2006; Ramaekers et al. 2006), SDLP was positively affected by MDMA (alone). Although, the moderating effect of MDMA on alcohol as found by Kuypers et al. (2006) failed to reach significance in this study. Equivalence testing demonstrated, though, that combined use could lead to impairment that is equivalent to BAC 0.5‰ or even BAC 0.8‰ since the upper limit of 95% confidence interval associated with the mean SDLP change in the combined treatment condition clearly exceeded the pre-established margin of both alcohol levels. However, the lower bound of the confidence interval spreads over the null line as well, indicating that a subset of participants may not be impaired or even slightly improved with respect to SDLP performance as compared to the placebo condition. Furthermore, this illustrates the large variance found in performance. Apparently, participants were differentially influenced by the different drug conditions. The lack of association between drug concentrations and performance confirms this assertion.
When looking at the time on task effects of the tested substances on weaving (SDLP), it was apparent that SDLP increased sturdily over time for all treatment conditions but only slightly for the MDMA-only condition. This indicates that participants might keep up their vigilance for a longer period of time because of the stimulating effects of MDMA. However, this stimulation did not appear to be not large enough to uphold when MDMA was co-administered with alcohol since the pattern of weaving increase observed was the same in the co-administration condition as in the placebo and alcohol condition. This is in line with the alertness ratings of participants before and after driving, in that the participants indicated they felt less alert after driving as compared with before driving in all treatment conditions except in the MDMA condition.
A behavioural compensating mechanism to keep up vigilance is (deliberately) varying speed. In the case of sedation, as would be experienced in the alcohol condition, a participant might temporarily increase speed to increase feelings of arousal as can be seen in an increase in the standard deviation of speed (Brookhuis 1998). Although this was not a strategy chosen by the group of participants in the first alcohol reference study, in the second, MDMA study participants did tend to vary their speed more when treated with alcohol only as compared to the placebo, but only when driving on the rural road. This is the kind of road type where one would expect such a behavioural compensation, since it is a monotonous road with little other traffic participants to consider. Furthermore, SDSP decreased when under the influence of MDMA only which would be expected since MDMA increases feelings of alertness and vigilance (Kuypers et al. 2007) therefore diminishing the need for behavioural compensation.
Another compensation mechanism for driving under the influence of sedating drugs such as alcohol is lowering ones speed. Furthermore, Brookhuis et al. (2004) reported an increase in speed when participants were under the influence of MDMA in urban areas and on the motorway. In the current study, however, participants kept to the posted speed on all road types and in the MDMA condition even decreased speed a bit more when driving on the rural road.
Car following remained unaffected under all treatment conditions. Overall coherence was relatively low, indicating that participants were following the lead car less well, which may have disturbed the measurement of car following. This is in line with Brookhuis et al. (2004), who also reported no significant effects of drug conditions on car following.
As said, the aim of the study was to investigate more complex driving behaviour as well and compare it to driving under the influence of different levels of alcohol. In the alcohol reference study, we found little to no effects of alcohol on any of measures assessing complex driving behaviour. Similarly, in the MDMA study, there were no effects found of any of the treatment conditions on the performance measures in these more complex scenarios.
One factor that might have contributed to variance in performance was the variance of the MDMA concentrations, as detected in saliva and, especially, in blood. It has previously been postulated that individuals might genetically differ in their metabolism of the drug (e.i. slow metabolizers versus rapid metabolizers). Individuals may therefore have variable concentrations of the parent compound and metabolites in blood after the same dose was administered (De La Torre et al. 2004; Oesterheld et al. 2004). Although this might explain the high variance of the MDMA in bodily fluids, it does not explain the lack of association with behavioural results. In the alcohol study, it was proposed that this might be due to variance in compensation strategies which make it hard to come to one conclusion about the average effects of treatments on measures in the complex driving scenarios.
This idea is supported in this study when looking at the large variances, especially in the multidrug condition. This was coincidently also the condition in which most participants’ guessed the treatment they had received incorrectly. Anecdotally, some participants indicated not to have noticed that they were administered alcohol in addition to MDMA. If drivers are not aware of the intoxicating effects of alcohol when driving under the influence of MDMA, and therefore do not feel the subjective discomfort of reduced performance efficacy, they might not compensate accordingly.
Moreover, when comparing self assessment of driving performance with the automated driving results, we could conclude that in case of alcohol consumption the self evaluation led to the wrong conclusions. In this condition participants rated their performance before and after driving under the influence as the same: that is, slightly worse than normal. Since their driving was actually seriously deteriorated, this conclusion was a falsely positive assessment of the situation. In the case of MDMA, the opposite was the case. The driving performance of the MDMA users was better than their self-assessment. Moreover, participants predicted their driving behaviour to deteriorate most when driving under the influenced of combined substances, but after having driven under the influence of the combined treatment condition performance was rated as the same to all other treatment conditions. This dissociation between subjective perceptions and objective performance impacts is an additional important notion for traffic safety since it might affect a driver’s judgement of whether or not it is safe to drive. An intoxicated individual might decide to drive because the feelings of alertness caused by MDMA cloud the impairing effects of other drugs such as alcohol, thereby implying a serious risk for traffic safety.
Acknowledgements
The funding for this research was provided by the EU-project DRUID (TREN-05-FP6TR-S07.61320-518404-DRUID). We would like to thank the anonymous reviewers and Ben Lewis Evans for their helpful comments on earlier versions of this paper.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Adams J. Risk. London: London University, College London Press; 1995. [Google Scholar]
- Baylen CA, Rosenberg H. A review of the acute subjective effects of MDMA/ecstasy. Addiction. 2006;10(7):933–947. doi: 10.1111/j.1360-0443.2006.01423.x. [DOI] [PubMed] [Google Scholar]
- Borkenstein RF, Crowther RF, Shumate RP, Zeil WW, Zylman R. The role of the drinking driver in traffic accidents. Bloomington: Department of Police Administration, Indiana University; 1964. [Google Scholar]
- Brookhuis KA. How to measure driving ability under the influence of alcohol and drugs, and why. Hum Psychopharmacol Clin Exp. 1998;13:S64–S69. doi: 10.1002/(SICI)1099-1077(1998110)13:2+<S64::AID-HUP51>3.0.CO;2-N. [DOI] [Google Scholar]
- Brookhuis KA, De Vries G, Prins van Wijngaarden P, Veenstra G, Hommes M, Louwerens JW, O’Hanlon JF. The effects of increasing doses of meptazinol (100, 200, 400 mg) and glafenine (200 mg) on driving performance. Haren: Traffic Research Centre, University of Groningen; 1985. [Google Scholar]
- Brookhuis KA, De Waard D, Mulder LJM. Measuring driving performance by car-following in traffic. Ergonomics. 1994;37(3):427–434. doi: 10.1080/00140139408963661. [DOI] [Google Scholar]
- Brookhuis KA, De Waard D, Samyn N. Effects of MDMA (ecstasy) and multiple drug use on (simulated) driving performance and traffic safety. Psychopharmacology. 2004;173:440–445. doi: 10.1007/s00213-003-1714-5. [DOI] [PubMed] [Google Scholar]
- Christophersen AS, Morland J. Drugged driving, a review based on the experience in Norway. Drug Alcohol Depend. 1997;47(2):125–135. doi: 10.1016/S0376-8716(97)00081-1. [DOI] [PubMed] [Google Scholar]
- De La Torre R, Farre M, Roset PN, Pizarro N, Abanades S, Segura M, Segura J, Cami J. Human pharmacology of MDMA: pharmacokinetics, metabolism, and disposition. Ther Drug Monit. 2004;26(2):137–144. doi: 10.1097/00007691-200404000-00009. [DOI] [PubMed] [Google Scholar]
- De Waard D, Brookhuis KA (1991) Assessing driver status: a demonstration experiment on the road. Accident Anal Prev 23(4): 297–307 [DOI] [PubMed]
- De Waard D, Brookhuis KA. Drug effects on driving performance, letter to the editor. Ann Intern Med. 2000;133:656. doi: 10.7326/0003-4819-133-8-200010170-00021. [DOI] [PubMed] [Google Scholar]
- De Waard D, Van der Hulst M, Brookhuis KA. Elderly and young drivers’ reaction to an in-car enforcement and tutoring system. Appl Ergon. 1999;30:147–157. doi: 10.1016/S0003-6870(98)00002-7. [DOI] [PubMed] [Google Scholar]
- Drummer OH, Gerostamoulos J, Batziris H, Chu M, Caplehorn JRM, Robertson MD, Swann P. The incidence of drugs in drivers killed in Australian road traffic crashes. Forensic Sci Int. 2003;134:154–162. doi: 10.1016/S0379-0738(03)00134-8. [DOI] [PubMed] [Google Scholar]
- Dumont GJ, Wezenberg E, Valkenberg MM, de Jong CA, Buitelaar JK, van Gerven JM, Verkes RJ. Acute neuropsychological effects of MDMA and ethanol (co-)administration in healthy volunteers. Psychopharmacology (Berl) 2008;197:465–474. doi: 10.1007/s00213-007-1056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont GJH, Schoemaker RC, Touw DJ, Sweep FCGJ, Buitelaar JK, van Gerven JMA, Verkes RJ (2010) Acute psychomotor effects of MDMA and ethanol (co-) administration over time in healthy volunteers. J Psychopharmacol 24(2):155–164 [DOI] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) Selected issue—drugs and driving. Luxembourg: Office for Official Publications of the European Communities; 2010. [Google Scholar]
- Fairclough SH, Graham R. Impairment of driving performance caused by sleep deprivation or alcohol: a comparative study. Journal of the Human Factors and Ergonomics Society. 1999;41:118–128. doi: 10.1518/001872099779577336. [DOI] [PubMed] [Google Scholar]
- Henry JA. Ecstasy and the dance of death. BMJ. 1992;305(6844):5–6. doi: 10.1136/bmj.305.6844.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Lopez C, Farre M, Roset PN, Menoyo E, Pizarro N, Ortuno J, Torrens M, Cami J, De la Torre R. 3,4-Methylenedioxymethamphetamine (ecstasy) and alcohol interactions in humans: psychomotor performance, subjective effects, and pharmacokinetics. J Pharmacol Exp Ther. 2002;300:236–244. doi: 10.1124/jpet.300.1.236. [DOI] [PubMed] [Google Scholar]
- Jantos R, Veldstra JL, Mattern R, Brookhuis KA, Skopp G. Analysis of 3,4-methylenedioxymetamphetamine: whole blood versus dried blood spots. J Anal Toxicol. 2011;35(5):269–273. doi: 10.1093/anatox/35.5.269. [DOI] [PubMed] [Google Scholar]
- Kelly E, Darke S, Ross J. A review of drug use and driving: epidemiology, impairment, risk factors and risk perceptions. Drug Alcohol Rev. 2004;23:319–344. doi: 10.1080/09595230412331289482. [DOI] [PubMed] [Google Scholar]
- Kuypers KPC, Ramaekers JG. Transient memory impairment after acute dose of 75 mg 3.4-methylene-dioxymethamphetamine. J Psychopharmacol. 2005;19:633–639. doi: 10.1177/0269881105056670. [DOI] [PubMed] [Google Scholar]
- Kuypers KPC, Samyn N, Ramaekers JG. MDMA and alcohol effects, combined and alone, on objective and subjective measures of actual driving performance and psychomotor function. Psychopharmacology. 2006;187(4):467–475. doi: 10.1007/s00213-006-0434-z. [DOI] [PubMed] [Google Scholar]
- Kuypers KPC, Wingen M, Limbert N, Samyn N, Ramaekers JG. Acute effects of nocturnal doses of MDMA on measures of impulsivity and psychomotor performance throughout the night. Psychopharmacology (Berl) 2007;129(1):111–119. doi: 10.1007/s00213-006-0679-6. [DOI] [PubMed] [Google Scholar]
- Lamers CT, Ramaekers JG, Muntjewerff ND, Sikkema KL, Samyn N, Read NL, Brookhuis KA. Dissociable effects of a single dose of ecstasy (MDMA) on psychomotor skills and attentional performance. Journal of psychopharmacology (Oxford, England) 2003;17(4):379–387. doi: 10.1177/0269881103174015. [DOI] [PubMed] [Google Scholar]
- Louwerens JW, Gloerich ABM, de Vries G, Brookhuis KA, O’Hanlon JF. The relationship between drivers’ blood alcohol concentration (BAC) and actual driving performance during high speed travel. In: Noordzij PC, Roszbach R, editors. Alcohol, drugs and traffic safety—T86. Amsterdam: Elsevier; 1987. pp. 183–186. [Google Scholar]
- Macdonald S, Mann RE, Chipman M, Anglin-Bodrug K. Collisions and traffic violations of alcohol, cannabis and cocaine abuse clients before and after treatment. Accid Anal Prev. 2004;36:795–800. doi: 10.1016/j.aap.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Mascha EJ, Sessler DI. Equivalence and noninferiority testing in regression models and repeated-measures designs. Anesth Analg. 2011;112(3):678–687. doi: 10.1213/ANE.0b013e318206f872. [DOI] [PubMed] [Google Scholar]
- Mora A, Arroyo A, Barbal M, Palahí M, Barbería E, Sánchez M. Driving under the effects of drugs of abuse: studies of oral fluid. Ann Toxicol Anal. 2009;21(4):197–202. [Google Scholar]
- Movig KLL, Mathijssen MPM, Nagel PHA, Van Egmond T, De Gier JJ, Leufkens HGM, Egberts ACG. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev. 2004;36(4):631–636. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- Mura P, Chatelain C, Dumestre V, Gaulier JM, Ghysel MH, Lacroix C, Kergueris MF, Lhermitte M, Moulsma M, Pepin G, Vincent F, Kintz P. Use of drugs of abuse in less than 30-year-old drivers killed in a road crash in France: a spectacular increase for cannabis, cocaine and amphetamines. Forensic Sci Int. 2006;160:168–172. doi: 10.1016/j.forsciint.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Nabben T, Koet S, Korf DJ. NL trend watch; gebruikersmarkt Uitgaansdrugs in Nederland 2006–2007. Amsterdam: Rozenberg; 2007. [Google Scholar]
- O’Hanlon JF, Haak TW, Blaauw GJ, Riemersma JBJ. Diazepam impairs lateral position control in highway driving. Science. 1982;217:79–80. doi: 10.1126/science.7089544. [DOI] [PubMed] [Google Scholar]
- Oesterheld JR, Armstrong SC, Cozza KL. Ecstasy: pharmacodynamic and pharmacokinetic interactions. Psychosomatics. 2004;45:84–87. doi: 10.1176/appi.psy.45.1.84. [DOI] [PubMed] [Google Scholar]
- Ojaniemi KK, Lintonen TP, Impinen AO, Lillsunde PM, Ostamo AI. Trends in driving under the influence of drugs: a register-based study of DUID suspects during 1977–2007. Accid Anal Prev. 2009;41:191–196. doi: 10.1016/j.aap.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Kuypers KPC. Acute effects of 3,4-methylenedioxymethamphetamine (MDMA) on behavioral measures of impulsivity: alone and in combination with alcohol. Neuropsychopharmacology. 2006;31:1048–1055. doi: 10.1038/sj.npp.1300894. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Kuypers KPC, Samyn N. Stimulant effects of 3,4-methylenedioxymethamphetamine (MDMA) 75 mg and methylphenidate 20 mg on actual driving during intoxication and withdrawal. Addiction. 2006;101:1614–1621. doi: 10.1111/j.1360-0443.2006.01566.x. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Kuypers KPC, Wingen M, Heinecke A, Formisano E. Involvement of inferior parietal lobules in prospective memory impairment during acute MDMA (ecstasy) intoxication: an event-related fMRI study. Neuropsychopharmacology. 2009;34:1641–1648. doi: 10.1038/npp.2008.219. [DOI] [PubMed] [Google Scholar]
- Reyner LA, Horne JA. Falling asleep whilst driving: are drivers aware of prior sleepiness. Int J Legal Med. 1998;111:120–123. doi: 10.1007/s004140050131. [DOI] [PubMed] [Google Scholar]
- Samyn N, De Boeck G, Wood M, Lamers CTJ, De Waard D, Brookhuis KA, Verstraete AG, Riedel WJ. Plasma, oral fluid and sweat wipe ecstasy concentrations in controlled real life conditions. Forensic Sci Int. 2002;128:90–97. doi: 10.1016/S0379-0738(02)00157-3. [DOI] [PubMed] [Google Scholar]
- Schwilke EW, Sampaio dos Santos MI, Logan BK. Changing patterns of drug and alcohol use in fatally injured drivers in Washington State. J Forensic Sci. 2006;51:1191–1198. doi: 10.1111/j.1556-4029.2006.00239.x. [DOI] [PubMed] [Google Scholar]
- Shafer JL, Graham JW (2002) Missing data: our view of the state of the art. Psychol Method 7(2):147–177 [PubMed]
- Skinner H. The drug abuse screening test. Addict Behav. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Jones BM, Simpson CD, Vega A. Effects of task complexity and practice on performance during acute alcohol intoxication. Percept Mot Skills. 1971;33:307–318. doi: 10.2466/pms.1971.33.1.307. [DOI] [PubMed] [Google Scholar]
- Thompson I, Williams G, Caldwell B, Aldington S, Dickson S, Lucas N, McDowall J, Weatherall M, Robinson G, Beasley R. Randomised double-blind, placebo-controlled trial of the effects of the ‘party pills’ BZP/TFMPP alone and in combination with alcohol. J Psychopharmacol. 2010;24:1299–1308. doi: 10.1177/0269881109102608. [DOI] [PubMed] [Google Scholar]
- Van Wolffelaar PC, Van Winsum W (1992) A new driving simulator including an interactive intelligent traffic environment. Proceedings of the third international conference on vehicle navigation and information systems. pp. 499–506.
- Veldstra JL, Brookhuis KA, de Waard D. Developing a virtual driving environment to test dose related effects of alcohol and drugs on simulated driving performance. In: de Waard D, Godthelp J, Kooi FL, Brookhuis KA, editors. Human factors, security and safety. Maastricht: Shaker; 2009. pp. 239–249. [Google Scholar]
- Verschraagen M, Maes A, Ruiter B, Bosman IJ, Smink BE, Lusthof KJ. Post-mortem cases involving amphetamine-based drugs in The Netherlands. Comparison with driving under the influence cases. Forensic Sci Int. 2007;170:163–170. doi: 10.1016/j.forsciint.2007.03.030. [DOI] [PubMed] [Google Scholar]
- Widmark EMP. Die theoretischen Grundlagen und die praktische Verwendbarkeit der gerichtlich-medinizischen Alkoholbestimmung. Berlin: Urban und Schwarzenberg; 1932. [Google Scholar]
- Zijlstra FRH (1993) Efficiency in work behavior: a design approach for modern tools. Dissertation, Delft University of Technology, Delft