Abstract
Quality improvement (QI) interventions in health care organizations have produced mixed results with significant questions remaining about how QI interventions are implemented. Team-based reflection may be an important element for understanding QI implementation. Extensive research has focused on individual benefits of reflection including links between reflection, learning, and change. There are currently no published studies that explore how team-based reflection impact QI interventions. We selected 4 primary care practices participating in a QI trial that used a facilitated, team-based approach to improve colorectal cancer screening rates. Trained facilitators met with a team of practice members for up to eleven 1-hour meetings. Data include audio-recorded team meetings and associated fieldnotes. We used a template approach to code transcribed data and an immersion/crystallization technique to identify patterns and themes. Three types of team-based reflection and how each mattered for QI implementation were identified: organizational reflection promoted buy-in, motivation, and feelings of inspiration; process reflection enhanced team problem solving and change management; and relational reflection enhanced discussions of relational dynamics necessary to implement desired QI changes. If QI interventions seek to make changes where collaboration and coordination of care is required, then deliberately integrating team-based reflection into interventions can provide opportunities to facilitate change processes.
Keywords: health care, primary care, quality improvement, reflection, teams
Quality improvement (QI) interventions in clinical settings seek to enhance the extent to which health care is safe, timely, effective, efficient, equitable, and patient centered, while resulting in the best-possible patient outcomes.1 Despite the variety of QI approaches that have been tested, the dominant conclusion is that QI effectiveness is “consistently inconsistent,”2 with some interventions being “successful” and some with limited to no improvements.3–9 This has prompted calls for research to focus on understanding how and why QI interventions work rather than simply measuring whether they work.2,10
Extensive research has already shown various benefits of reflection,11,12 and a dynamic link among reflection, learning, and change.13–17 However, such reflection is frequently considered as a solitary activity, which is unlikely to affect a larger care team or organization. Although this work is important for individual professional development, the same level of attention has not been devoted to team-based reflection and how larger entities can harness the benefits of reflection.18
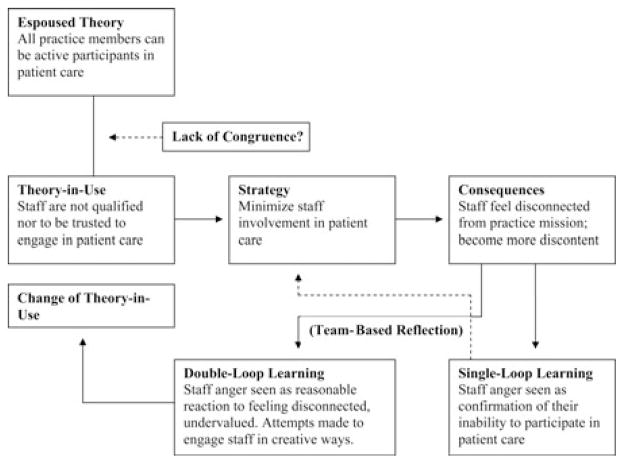
The Figure illustrates how team-based reflection might affect learning and change in a primary care practice. In this example, staff feel disconnected from patient care leading to staff discontent (adapted from Redmond19).
Figure.
Links between reflection, learning, and change. Adapted by permission from Gould N, Baldwin M. Farnham Social Work, Critical Reflection and the Learning Organization. Farnham, England: Ashgate; 2004:134. Copyright 2004 Ashgate.
When faced with a poor outcome, such as staff discontentment, one possibility is “single-loop learning” in which individuals repeat actions, learning in an uncritical fashion from previous experience. Such learning tends to maintain the status quo,20 and can lead to defensive routines and taboos on discussing key issues.14 In contrast, through team-based reflection, “double-loop learning” is enabled such that certain beliefs and behaviors are changed and the organization arguably becomes better suited to deal with changing professional environments.21
In this article, we present 3 types of team-based reflection that emerged from an in-depth qualitative analysis of primary care teams undergoing a QI intervention: organizational reflection, process reflection, and relational reflection. A review of the literature revealed connections between our findings and concepts commonly used when examining individual-level reflection. These concepts suggest that reflection is not a monolithic concept; rather, there are multiple dimensions of team-based reflection that may be useful to reflection scholars as well as QI researchers and participants.
For example, when researchers recommend creating opportunities for QI participants to reflect on the larger organization—its purpose and mission,5 its interdependent resources,22 and the nature of its problems23—the reflection literature speaks to this through the concept of “helicopter vision” in which individuals (1) rise above a situation to get an overview of how the component parts fit together and how they create the overall situation and (2) descend back into it to be able to deal with it in an informed way.24
This provides a more holistic view of the organization and each person’s role within it. Lacking “helicopter vision” means individuals may be working on the basis of a partial, and perhaps distorted, picture and thus missing out on key information and insights.24
Focusing on change processes, QI researchers have noted the importance of having clear objectives and making time for “learning and planning for sustained improvements.”5 In the reflection literature, the concepts reflection-in-, -on-, and -for-action25,26 are useful for understanding how different kinds of reflection could enhance QI efforts. Reflection-in-action is observing one’s thoughts and actions as they are occurring to make adjustments. Reflection-on-action is looking back on previous actions to learn from them and affect future action. Reflection-for-action is pausing to contemplate the effects of changes and consider unanticipated consequences.
Furthermore, relational dynamics often underlie the success or failure of QI efforts. For example, Sobo et al8 emphasize communication problems that can arise when members of an organization work in “silos.” Throughout QI implementation, the notion of critical reflection can help unmask how power differences shape interactions and change processes,27 call into question taken-for-granted assumptions, evaluate effectiveness of the changes, and ensure that new changes do not replicate existing, ineffective processes.24,28
Although this scholarly work provides important insights relevant for QI implementation, there has been relatively little empirically driven work on team-based reflection to understand how reflection may affect team processes and QI implementation. If QI interventions seek to make changes that extend beyond the individual level, that is, where collaboration and coordination of care is required, then integrating team-based reflection into interventions may provide opportunities to facilitate change processes. In this analysis, our primary question was: How does reflection affect team processes and QI implementation? To answer this question, we conducted a qualitative analysis of 4 primary care practices as they participated in a 6-month QI intervention aimed at improving colorectal cancer (CRC) screening rates.
METHODS
Project SCOPE
Beginning in 2005, 25 New Jersey primary care practices participated in a federally funded QI trial called SCOPE (Supporting Colorectal Cancer Outcomes through Participatory Enhancements). Practices were randomized into either an intervention (n = 13) or control arm (n = 12). The primary aim of the trial was to test the effectiveness of a facilitated, team-based approach to improve CRC screening rates in primary care practices. The current analysis provides an in-depth look at team-based reflection to better understand QI implementation and does not provide results on the clinical outcomes of the study.
SCOPE used an organizational change model that views primary care practices as complex adaptive systems.29 The model used a process called reflective adaptive process (RAP)29,30 and 2-day-long learning collaboratives.31 Trained RAP facilitators met with a team of practice members representing multiple functional areas for up to eleven 1-hour RAP meetings. Facilitators followed a loosely structured QI plan designed to help teams better understand their current processes for cancer screening, brainstorm improvement ideas, reach consensus on a plan, and then implement and monitor this plan. As the name RAP suggests, time for reflection was intended to be a central element of these meetings.
The University of Medicine and Dentistry of New Jersey–Robert Wood Johnson Medical School Institutional Review Board approved this study. Medical directors and/or lead physicians of each practice as well as staff members who participated in the study gave informed consent. All names of practices and individuals have been changed to protect confidentiality.
Selection of practices for analysis
This analysis used a purposefully selected number of practice sites.32 Of the 25 SCOPE practices, 10 were excluded from this analysis because of not completing the entire intervention. Among the 15 eligible practices remaining, we selected 4 practices for analysis to reflect maximum variation among study facilitators (see Table 1) because external facilitators can impact the QI process in various ways such as how team conflict is managed.33
Table 1.
SCOPE PRACTICES AND RAP TEAMS
| Size of Practice | Type of Practice | Ownership of Practice | Size of RAP Team | Facilitator (Gender, Education) | |
|---|---|---|---|---|---|
| P1 | 27 | Single specialty (FM) | Physician owned | 7 | Female, Masters-Labor Relations |
| P2 | 15 | Single specialty (FM) | Physician owned | 5 | Female, PhD-Sociologya |
| P3 | 20 | Single specialty (IM) | Physician owned | 6 | Female, PhD-Sociologya |
| P4 | 66 | Single specialty with residency (FM) | Hospital owned | 9 | Male, MD |
Abbreviations: FM, family medicine; IM, internal medicine; RAP, reflective adaptive process; SCOPE, Supporting Colorectal Cancer Outcomes through Participatory Enhancements.
Different facilitators in P2 and P3.
Given the lack of empirical work on team-based reflection, we felt it was best to focus on generating a rich, descriptive analysis focused on a small number of cases. This facilitated our ability to develop new understandings of team-based reflection and to identify potential hypotheses that could be tested with a larger sample of practices in future work, consistent with qualitative sampling standards.32
Data collection
Two types of data informed this analysis: recorded RAP meetings and associated fieldnotes. Reflective adaptive process meetings were audio-recorded and digitally stored on a computer. Facilitators wrote descriptive fieldnotes of each RAP meeting to capture elements (eg, body language) that would not be available from audio-recordings. Fieldnotes were de-identified and stored as text documents.
Data analysis
Two authors (EKS and JH) performed the primary data analyses. Because the audio-recordings were not transcribed, we listened to each meeting from a single practice and transcribed salient segments. EKS then listened to and transcribed segments from the remaining 3 practices. In total, there were just over 26 hours of audio-recordings. Transcriptions generated approximately 100 pages of text that were imported into ATLAS.ti for coding purposes.
We used a template approach for analysis that involved coding our data set to create segments of text that were identifiable by topic and easily assembled for interpretation.34,35 The analytic steps (described in greater detail below) included (a) creating a coding scheme, (b) computer coding the text, (c) sorting segments by category, and (d) reading segments and making connections that were corroborated.34
Our analysis began with several a priori codes identified from the reflection literature such as reflection-in-, -on-, and -for-action, and critical reflection. Using these codes as a template, we read through all data of a single practice. When data segments did not correspond to codes in our template, we created new codes and added them to our template. Emergent codes included facilitator promptings for reflection, reflection on current and past processes, reflection on work relationships, reflection on organizational issues/problems, and identification of certain team member qualities. (see Table 2 for operational definitions of our key concepts used in this article).
Table 2.
OPERATIONAL DEFINITIONS OF KEY CONCEPTS
| Concept | Operational Definition |
|---|---|
| Reflection | “Replaying” an event to critically contemplate it, make sense of it, learn from it |
| Team-based reflection | Verbalizing one’s personal introspections in a group/team context; responding to others’ reflections |
| Organizational reflection | Conversations about the organization’s purpose/mission, its interdependent resources, and the nature of organizational problems |
| Process reflection | Conversations about how the team is doing their work/QI |
| Relational reflection | Conversations about relational dynamics within the organization, how relationships impact QI |
Abbreviation: QI, quality improvement.
By the third practice, no new codes were added to the template, thus indicating that we had reached saturation with our conceptual codes. A consensus approach, involving re-reading data or relistening to audio-files for segments in question, was used to resolve any discrepancies between coders. EKS then coded all practices using the complete template, with the co-authors reviewing the codes and segments of text to ensure accuracy and validity.
Next, the authors used an immersion/ crystallization technique that entailed re-reading the coded text segments to identify general themes or patterns.36 Through an inductive process during data analysis, we identified 3 types of team-based reflection: organizational reflection, process reflection, and relational reflection.
RESULTS
Each practice held at least 9 QI meetings with the study facilitator. In the 3 physician-owned practices, the owner/lead physician was present for the majority of the meetings. Practice 1 (P1) and practice 2 (P2) each had 2 physicians on the team. P4 was a residency practice and had 3 physicians including 1 resident on the team. The office manager of each practice was also on the team. Other members included employees from various functional areas including billing, front office/reception, file clerks, registered nurses, and medical assistants.
How does reflection affect team processes and QI implementation?
Using our 3 types of reflections as an analytic framework, we found that (1) organizational reflection promoted team member buy-in, motivation, and feelings of inspiration, (2) process reflection enhanced problem solving and change management, and (3) relational reflection enhanced discussions of relational dynamics and taken-for-granted assumptions.
Organizational reflection
Organizational reflection spurred new conversations among practice members37 that often pointed to the need for “helicopter vision,” that is, a more holistic view of the organization, its mission, and members’ roles within it. This created opportunities for practice members to develop common understandings and to feel inspired by knowing how all parts of the practice can fit into the mission.
An extended example of organizational reflection from P2 illustrates this point. P2 had been experiencing tension among practice personnel and poor communication. What was reported as tension between staff and the lead physician (Dr L) was evidenced, in part, by the turnover of 14 employees over the previous several years. Moreover, physicians and staff were critical of Dr L’s reportedly autocratic decision-making style.
During early RAP meetings, the team discussed their desire to enhance the practice’s prevention mission. Dr W (a second physician on the RAP team) was instrumental in helping the team to reflect on how they could “develop a renewed mindset in the whole practice about health maintenance and screening” as a way to not only improve their patient care but also help staff feel connected to the practice’s prevention mission. She commented to the team:
We need to empower them (staff) to feel like they understand the whole prevention issue and why that’s important for us …. When somebody says “when was my last physical?” they can say “Oh! We need to find that out for you and let’s see when you need to come back.
Dr L questioned what the staff needed to know about prevention. The office manager responded:
Well, just some of the basic things … which types of cancers are most prevalent for which gender and which age …. I don’t know if all the medical assistants would know something like that because I wouldn’t and I don’t think the front (staff) would know.
Dr L skeptically asked: “Is that really useful?” The office manager responded: “It is … we can’t just be completely blind about it ….” Dr W added:
We are the ones to help prevent people from getting to the point of being acute … our whole premise as family practitioners are to keep people healthy, to keep families healthy …. We (should) start by teaching our staff that … to help them understand where we’re coming from, and why it’s important to have patients come in before they get sick.
Later in this discussion, Dr L said: “You know, this is very inspiring because I had no idea that the front desk would care about this ….” At subsequent RAP meetings, team members shared poignant reflections that helped shape their QI efforts including a lengthy conversation about the possibility of creating what Dr L called an “office culture change,” where people “feel part of the office ….” Having reflective conversations on the practice’s mission and finding value in including all practice members into that mission was important, particularly for the lead physician, for gaining buy-in and motivation to implement changes and for creating feelings of inspiration to change the office culture.
Process reflection
Engaging in process reflection as a team provided benefits to QI implementation particularly through enhanced change management and problem solving. Process reflection was spurred by questions such as: How will we generate ideas? How will we communicate with each other? What could we improve on?
Process reflection was built into the SCOPE intervention design. For example, facilitators encouraged teams to establish “ground rules” that would serve as a code of conduct for the team.38 Ground rules typically included such things as commitments to share RAP team discussions with other practice members, being truthful and open, and promises from practice leaders that “jobs will not be lost” as a result of being critical or candid. These conversations prompted teams to reflect on how they wanted to work together based on desired values (eg, respect all opinions), group process (eg, how to communicate with others), and team/meeting logistics (eg, how to handle team member absences).
Process reflection also often entailed reflection-inaction that helped team members better understand how others felt during the change process and reduced the potential for misinterpretations. For example, as the facilitator at P1 was talking to the team about their QI plans, she stopped herself—apparently noticing the lead physician’s facial expression—and said, “Are you looking cynical or am I just reading … ?” The physician interrupted her saying, “No, I’m just exhausted (chuckling).” Similarly, while sharing some positive impressions at P2, the facilitator stopped herself to say to Dr L, “You look troubled … ” Dr L interjected, “I appreciate your enthusiasm but I just don’t get it, but that’s just me, I guess.” Other team members then added encouraging words about their progress and helped Dr L see the value in their QI efforts.
In another example, the facilitator at P4 stopped the team’s discussion and said,
I apologize—I forgot something that you mentioned (at a previous meeting). You actually wanted to split this group up (into subcommittees). Is that still the case or do you want to remain as one team and discuss as one whole process?
Many team members responded and they reached consensus to stay as one group. These examples point to the benefits of openly reflecting on how the change process is being perceived and managed by reducing potential misinterpretations or misunderstandings.
Whereas the previous examples speak to how reflection enhanced change management, the following example highlights the use of reflection for enhanced team problem solving. At P4, a physician researched the practice’s CRC screening rate prior to a RAP meeting. She reported with great disappointment that in the past year only 12% of patients had been appropriately screened for colon cancer. A nonclinical team member asked: “What is the percentage that we would be looking for?” To which the office manager responded, “100%!” This prompted a team discussion of what a realistic screening rate goal should be given their largely underinsured patient population. These conversations created the opportunity for the team to have a shared understanding of what the problem was (ie, a very low screening rate) and then move into discussions that would enable them to—as the physician emphasized—“watch this number … grow.”
Relational reflection
Relational reflection involves critically reflecting on relational dynamics within the organization and having open, honest conversations about how relationships may be impacting QI efforts. To illustrate, we compare P2 and P3 as both experienced relational office dynamics that were negatively affecting working relationships and progress in QI efforts.
P2 wanted to create a practice-wide prevention mission where all practice members could be involved and feel valued. Their rationale was that if practice members felt empowered to promote prevention, they would be more invested in their work, leading to improved office dynamics, reduced staff turnover, and improved delivery of preventive care. However, tensions, between the lead physician (Dr L) and other practice members, hampered their ability to work on QI projects. Over the course of the intervention, the team confronted these issues head on. During one team discussion, the office manager said to Dr L, “I ask you all the time—what do you want from the office as a whole? What are you trying to accomplish? I think if they (staff) hear from you, it will make a difference.” Dr L asked: “Do I ever give you an answer?” The office manager replied: “No, you give me pieces …. I don’t know when they (staff) hear from you unless it’s things that are wrong, truthfully ….”
Here, the office manager’s straightforward critical reflection on how Dr L related to staff served as an important turning point in Dr L’s perspective on her role as the leader in the practice. At the very next meeting Dr L said to the team: “I wanted to give a little speech since (the office manager) told me people really don’t know where I’m coming from ….” She then talked about how her personal history in family medicine had shaped her practice philosophy and leadership style. As a team, they made plans for Dr L to share this with the rest of the practice and to have an open dialogue with staff on their roles in the practice mission.
In contrast, the RAP team at P3 struggled to generate ideas and develop QI plans. At the end of one RAP meeting, team members continued talking with the facilitator after the lead physician left the room, commenting on why nobody would speak up in the meetings. One person said: “I think they’re afraid of what reaction they’re going to get … is it going to put something in the back of the doctor’s head that eventually they’ll be punished ….” A long-term employee added: “And there’s a lot of stuff that goes on …. I feel like I can’t really say anything.” Team members’ uneasiness with reflecting on relational issues in the presence of the physicians inhibited their ability to raise critical or dissenting perspectives throughout the QI process, and the team ultimately did not implement any new changes targeting better clinical care and, more specifically, CRC screening.
DISCUSSION
Many innovations being introduced into primary care require health care professionals and practice staff to work differently than in the past. Yet, little attention has been paid to communication, relationships, teamwork, leadership, and other human factor needs as practices adopt new ideas.39,40 This was a major issue for practices in the American Academy of Family Physicians National Demonstration Project,41 as practices had the most difficulty when changes affected multiple roles, required coordination across work units, and challenged the traditional physician-centered model of primary care.42
On the basis of our findings, we suggest that QI efforts in health care organizations would benefit from ongoing team-based reflection. Our findings suggest that organizational reflection, process reflection, and relational reflection can aid such organizations by creating opportunities to enhance stakeholders’ motivation to undergo changes; by helping teams in the actual work of problem solving and using a team to implement changes; and by dealing with power dynamics and relational issues that may impede the ability to implement desired QI changes.
Rather than studying reflection as a solitary, introspective activity, we have explored 3 types of team-based reflection as evidenced during QI discussions in primary care settings. Although addressed separately for analytic purposes, they are actually interdependent. More specifically, our findings suggest that organizational reflection and process reflection can be dependent on adequate relational reflection. For example, at P2, the team’s organizational reflection on their practice-wide prevention mission was clearly interrelated with their relational reflection on tensions among practice personnel. Our contrasting example of P3 where the QI team struggled to establish a climate of reflection, suggests that an absence of relational reflection may impede QI implementation when team members do not feel safe to share critical or dissenting opinions.
Our analysis has several limitations. First, the small sample limits our ability to generalize to other primary care practices or health care organizations. However, because of the dearth of empirical research on team-based reflection, an important strength of this study is that the qualitative data cover the span of the QI intervention. Such data are not typically available in larger survey studies. Therefore, the richness of these data facilitated a more detailed look at the effects of team-based reflection on QI implementation. Second, we cannot report on whether or not reflection mattered for improving clinical outcomes (ie, cancer screening rates). Our analysis is limited to how reflection impacted the process of the QI intervention. Finally, we are mindful of issues of researcher bias, and the validity and reliability of our themes and findings. We took steps to minimize such bias primarily through ongoing discussions among the authors to verify our coding scheme, interpretations, and conclusions.
Next steps must push these lines of inquiry further to better understand when to reflect on organizational, process, and relational issues, and how much reflection is necessary for QI “success.” As with any research, new questions have emerged: Is it reasonable to expect QI teams to continue meeting and reflecting ad infinitum? Are there ever diminishing returns on ongoing reflective practices? Perhaps, most importantly, future research must systematically study a larger number of practices to see if/how variations in reflection impact clinical outcomes, which is at the heart of the call for fundamental health services change. Future research should consider hypotheses generated from this exploration, including whether enhanced QI team reflection improves intermediate process variables, such as communication and team decision making, and eventually improved clinical outcomes.
CONCLUSIONS
Team-based reflection can affect the QI change process. Although certainly not a panacea, building an environment of trust where members of the organization can openly and critically reflect while implementing changes can address many of the social and relational elements that so often hinder effective change. As health care researchers develop approaches to improve health care organizations and patient care, they should consider ways to intentionally integrate reflective practices into these efforts.
Acknowledgments
This study was supported by a grant from the National Cancer Institute (R01 CA112387-01). In addition, Dr Crabtree’s time was supported in part by a senior investigator grant from the National Cancer Institute (1K05CA140237).
Footnotes
The authors declare that they have no competing interests or commercial associations that might pose a conflict of interest in connection with this article.
References
- 1.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Walshe K, Freeman T. Effectiveness of quality improvement: learning from evaluations. Qual Saf Health Care. 2002;11:85–87. doi: 10.1136/qhc.11.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(suppl 2):112–145. [PubMed] [Google Scholar]
- 4.Chandra A, Frank Z. Utilization of performance appraisal systems in health care organizations and improvement strategies for supervisors. Health Care Manag. 2004;23(1):25–30. doi: 10.1097/00126450-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Ovretveit J, Bate P, Cleary P, et al. Quality collaboratives: lessons from research. Qual Saf Health Care. 2002;11(4):345–351. doi: 10.1136/qhc.11.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ovretveit J, Staines A. Sustained improvement? Findings from an independent case study of the Jonkoping Quality Program. Qual Manag Health Care. 2007;16(1):68–83. doi: 10.1097/00019514-200701000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Oxman A, Thomson M, Davis D, Haynes R. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. Can Med Assoc J. 1995;153(10):1423–1431. [PMC free article] [PubMed] [Google Scholar]
- 8.Sobo EJ, Bowman C, Aarons GA, Asch S, Gifford AL. Enhancing organizational change and improvement prospects: lessons from an HIV testing intervention for veterans. Hum Relat. 2008;67(4):443–453. [Google Scholar]
- 9.Solberg LI. If you’ve seen one quality improvement collaborative. Ann Fam Med. 2005;3:198–199. doi: 10.1370/afm.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney SE. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152. doi: 10.1136/bmj.a3152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein R. Mindful practice. J Am Med Assoc. 1999;282:833–839. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 12.Mamede S, Schmidt HG, Penaforte JC. Effects of reflective practice on the accuracy of medical diagnoses. Med Educ. 2008;42:468–475. doi: 10.1111/j.1365-2923.2008.03030.x. [DOI] [PubMed] [Google Scholar]
- 13.Antonacopoulou EP. The dynamics of reflexive practice: the relationship between learning and changing. In: Reynolds M, Vince R, editors. Organizing Reflection. Burlington, VT: Ashgate; 2004. pp. 47–64. [Google Scholar]
- 14.Argyris C. On Organisational Learning. 2. Oxford UK: Blackwell; 1999. [Google Scholar]
- 15.Dixon N. The Organizational Learning Cycle: How Can We Learn Collectively. London, England: McGraw-Hill; 1994. [Google Scholar]
- 16.Nevis EC, DiBella AJ, Gould JM. Organizations as learning systems. Sloan Manag Rev. 1995 Winter;:73–85. [Google Scholar]
- 17.Srivastva S, Bilimoria D, Cooperrider DC, Fry RE. Management and organizational learning for positive global change. Manag Learn. 1995;26(1):37–54. [Google Scholar]
- 18.Ghaye T. Building the Reflective Healthcare Organisation. Oxford UK: Blackwell Publishing; 2008. [Google Scholar]
- 19.Redmond B. Reflecting on practice: exploring individual and organizational learning through a reflective teaching model. In: Gould N, Baldwin M, editors. Social Work, Critical Reflection and the Learning Organization. Burlington, VT: Ashgate; 2004. pp. 129–142. [Google Scholar]
- 20.Argyris C, Schon D. Organisational Learning II: Theory, Method and Practice. Reading, MA: Addison-Wesley; 1996. [Google Scholar]
- 21.Gould N, Taylor I, editors. Reflective Learning for Social Work. Aldershot: Arena; 1996. [Google Scholar]
- 22.Plsek PE. Quality improvement methods in clinical medicine. Pediatrics. 1999;103(1):203–214. [PubMed] [Google Scholar]
- 23.Wilson T, Berwick D, Cleary P. What do collaborative improvement projects do? Experience from seven countries. Jt Comm J Qual Saf. 2003;29:85–93. doi: 10.1016/s1549-3741(03)29011-0. [DOI] [PubMed] [Google Scholar]
- 24.Thompson S, Thompson N. The Critically Reflective Practitioner. New York, NY: Palgrave Macmillan; 2008. [Google Scholar]
- 25.Killion J, Todnem G. A process for personal theory building. Educ Leadersh. 1991;43(6):14–16. [Google Scholar]
- 26.Schon D. The Reflective Practitioner: How Professionals Think in Action. London, England: Temple Smith; 1983. [Google Scholar]
- 27.Brookfield S. Developing Critical Thinkers. San Francisco, CA: Jossey-Bass; 1987. [Google Scholar]
- 28.Fook J. Critical reflection and organizational learning and change: a case study. In: Gould N, Baldwin M, editors. Social Work, Critical Reflection and the Learning Organization. Burlington, VT: Ashgate; 2004. pp. 41–55. [Google Scholar]
- 29.Stroebel C, McDaniel R, Crabtree B, Miller W, Nutting P, Stange K. How complexity science can inform a reflective process for improvement in primary care practices. Jt Comm J Qual Patient Saf. 2005;31(8):438–446. doi: 10.1016/s1553-7250(05)31057-9. [DOI] [PubMed] [Google Scholar]
- 30.Balasubramanian BA, Chase SM, Nutting PA, et al. Using Learning Teams for Reflective Adaptation (ULTRA): insights from a team-based change management strategy in primary care. Ann Fam Med. 2010;8(5):425–432. doi: 10.1370/afm.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaw EK, Chase SM, Howard J, et al. More black to explore: how quality improvement collaboratives shape practice change. J Am Board Fam Med. 2012;25:149–157. doi: 10.3122/jabfm.2012.02.110090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuzel AJ. Sampling in qualitative inquiry. In: Crabtree B, Miller W, editors. Doing Qualitative Research. 2. Thousand Oaks, CA: Sage Publications; 1999. pp. 33–45. [Google Scholar]
- 33.Shaw EK, Looney JA, Chase SM, et al. In the moment: the impact of intentional facilitators on group processes. Group Facil: A Res Appl J. 2010;23:523–533. [Google Scholar]
- 34.Crabtree B, Miller W. Using codes and code manuals: a template organizing style of interpretation. In: Crabtree B, Miller W, editors. Doing Qualitative Research. 2. Thousand Oaks, CA: Sage; 1999. pp. 163–177. [Google Scholar]
- 35.Miles M, Huberman A. Qualitative Data Analysis: A Source-book of New Methods. Beverly Hills, CA: Sage; 1984. [Google Scholar]
- 36.Borkan J. Doing Qualitative Research. Immersion/crystallization. 2. Thousand Oaks, CA: Sage Publications; 1999. pp. 179–194. [Google Scholar]
- 37.Jordan ME, Lanham HJ, Crabtree B, et al. The role of conversation in health care interventions: enabling sensemaking and learning. Implement Sci. 2009;4:15. doi: 10.1186/1748-5908-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lapointe-Lemaire S. IAF Canada Monograph Series. 5. 2009. Ground rules; pp. 1–5. [Google Scholar]
- 39.Bohmer RMJ. Designing Care: Aligning the Nature and Management of Health Care. Boston, MA: Harvard Business Press; 2009. [Google Scholar]
- 40.Christensen CM, Grossman JH, Hwang J. The Innovator’s Prescription: A Disruptive Solution for Health Care. New York, NY: McGraw-Hill; 2009. [Google Scholar]
- 41.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010;8 (Suppl 1):S45–56. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8(suppl 1):S33–S44. doi: 10.1370/afm.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]