Abstract
Objectives
Health utility combines health related quality of life and mortality to produce a generic outcome measure reflecting both morbidity and mortality. It has not been widely used as an outcome measure in evaluations of emergency care and little is known about the feasibility of measurement, typical values obtained or baseline factors that predict health utility. We aimed to measure health utility after emergency medical admission, to compare health utility to age, gender and regional population norms, and identify independent predictors of health utility.
Methods
We selected 5760 patients across three hospitals who were admitted to hospital by ambulance as a medical emergency. The EQ-5D questionnaire was mailed to all who were still alive 30 days after admission. Health utility was estimated by applying tariff values to the EQ-5D responses or imputing a value of zero for those who had died. Multivariable analysis was used to identify independent predictors of health utility at 30 days.
Results
Responses were received from 2488 (47.7%) patients, while 541 (9.4%) had died. Most respondents reported some or severe problems with each aspect of health. Mean health utility was 0.49 (standard deviation 0.35) in survivors and 0.45 (0.36) including non-survivors. Some 75% had health utility below their expected value (mean loss 0.32, 95% confidence interval 0.31 to 0.33) and 11% had health utility below zero (worse than death). On multivariable modelling, reduced health utility was associated with increased age and lower GCS, varied according to ICD10 code and was lower among females, patients with recent hospital admission, steroid therapy, or history of chronic respiratory disease, malignancy, diabetes or epilepsy.
Conclusions
Health utility can be measured after emergency medical admission, although responder bias may be significant. Health utility after emergency medical admission is poor compared to population norms. We have identified independent predictors or health utility that need to be measured and taken into account in non-randomized evaluations of emergency care.
Keywords: health utility, emergency medicine, hospital admission
Background
Patient outcomes need to be measured after emergency medical care for research, quality improvement and benchmarking of performance [1]. Mortality is widely used as an outcome measure in research, and risk-adjusted mortality can be used to compare systems of emergency care and drive quality improvement [2,3]. Health related quality of life, by contrast, is less commonly used as an outcome measure in emergency medicine research and has rarely been used in quality improvement [4-7]. However, some important emergency interventions, such as thrombolysis for stroke [8], affect health related quality of life rather than mortality. The impact of these interventions will only be identified if we measure health related quality of life.
Health related quality of life has been measured after hospital admission for major trauma [9-11] and specific illnesses, such as myocardial infarction [12] and stroke [13]. Major trauma is only responsible for a small proportion of emergency hospital admissions. Most admissions are for medical conditions, with patients increasingly presenting with mixed pathologies and multiple co-morbidities. We need to measure health related quality of life in the general emergency medical population if we are to estimate the effect of interventions and changes in service delivery upon the whole relevant population.
If both mortality and health related quality of life are measured then these can be combined to provide an overall measure of health, known as health utility. This measure allows comparison of outcomes between a wide range of different conditions and interventions affecting both mortality and morbidity. Combining mortality and health related quality of life in a single measure also overcomes a problem inherent in measuring quality of life alone, the "healthy survivor effect", whereby an apparent improvement in health related quality of life may be caused by an increase in mortality among patients with lower quality of life. However, health utility has not been widely used as an outcome measure in evaluations of emergency care and little is known about the feasibility of measurement, typical values obtained or baseline factors that predict health utility.
Health utility among emergency medical patients will clearly be influenced by many factors, especially pre-existing co-morbidities, and emergency treatment will be only one factor influencing outcome. Baseline measurement of health related quality of life (i.e. prior to emergency care) is subject to substantial logistical barriers and likely to be unfeasible or impractical for most evaluations, so any non-randomized evaluation of emergency care using health utility as an outcome needs to measure and take into account factors that predict health utility after emergency care. We therefore need to know which covariates predict health utility after emergency medical care, as well as knowing whether measurement is feasible, before health utility can become a widely-used outcome measure for emergency care.
This study was undertaken as part of the DAVROS study (Development And Validation of Risk-adjusted Outcomes for Systems of emergency care) and aimed to evaluate the use of health utility as an outcome measure in emergency care. Our specific objectives were to compare health utility of the population to region, age and gender adjusted normal values and to identify independent predictors of health utility. We did not aim to compare services in this evaluation or draw inferences about the effect of emergency health care upon health utility.
Methods
We undertook a cross-sectional survey to measure health utility among patients recently admitted to hospital with a medical emergency using the EQ-5D self-complete questionnaire. We valued health utility using the EQ-5D for survivors and attributed a value of zero to those who had died by 30 days. The EQ-5D was developed following a review of existing generic health measures and consists of 5 questions relating to health status over the previous day [14,15]. The responses to the 5 questions allow patients to be classified into one of 243 possible health states. These health states were valued using preferences derived from the piloting of the questionnaire to produce a tariff for each state [15-17]. The tariff values overall health on a scale in which zero equates to death and one equates to perfect health. Negative values (health states worse than death) are possible.
The study took place in three emergency departments in Sheffield, Barnsley and Rotherham in South Yorkshire in the United Kingdom and in the Yorkshire Ambulance Service. These three emergency departments provide adult emergency services to a largely urban population of around 1 million. Patients were identified by review of hospital computer systems and selected if they were (a) alive and not in cardiac arrest when attended by an emergency ambulance, and (b) were then either admitted to hospital or died in the ambulance or emergency department. We excluded children (aged < 18 years), women with obstetric emergencies, adults with primarily mental health emergencies and injured adults aged under 65. We felt that these patients would have markedly different health utility from the majority of emergency medical admissions and/or would present particular difficulties in measurement. The threshold of 65 years for injuries was chosen as a crude means of including those with injuries likely to be secondary to or associated with medical complaints, while excluding those with primarily traumatic reasons for admission.
Hospital computer records and local Coroner's Office lists of deaths were checked 30 days after patient admission and any patient not recorded as being dead was sent a letter from the emergency department inviting them to take part in the research, along with an information sheet, consent form and copy of the EQ-5D questionnaire. If they were willing to participate they signed the consent form, completed the EQ-5D and mailed both to the University of Sheffield in a postage-paid envelope. They were asked to return the uncompleted questionnaire if they did not wish to participate. A single reminder was mailed two weeks after the initial mailing to non-responders.
Emergency department data, including patient age, gender, physiology (heart rate, respiratory rate, blood pressure, peripheral oxygen saturation and Glasgow Coma Score (GCS)), recorded co-morbidities and hospital admission within the previous 30 days, were abstracted from computer and paper hospital records by a researcher. Ambulance physiology data were recorded by paramedics on the standard patient report forms and then scanned onto an electronic database. Ambulance data were then matched to emergency department data using the ambulance dispatch code. Wherever possible the first physiological recording (i.e. the ambulance recording) was used. Where no physiology was recorded in the ambulance or the cases could not be matched to the patient report form the emergency department physiology data were used. Each patient had an International Classification of Diseases version 10 (ICD-10) code attributed by hospital clerical staff as part of routine management. All data were entered onto a secure online database managed by the University of Sheffield Clinical Trials Unit.
Chi-square tests were used to test the association between baseline patient characteristics (age group, gender, ICD-10 code, hospital admission within the previous 30 days, recorded co-morbidities and hospital attended) and questionnaire response rate. Patients who had died by 30 days were attributed health utility of zero. Patients who had died effectively had a response rate of 100% whereas those who survived had a lower response rate. To account for this differential rate of missing data we upweighted the EQ-5D scores of questionnaire respondents by the inverse of the age- and sex- specific response rate. All analyses used the weighted scores. Health utility data for the normal United Kingdom population were used to calculate a regional, age and gender adjusted expected normal value for each patient [17]. Analysis of variance was used to test the association between baseline patient characteristics and health utility, and also between physiological variables and health utility. Finally multivariable linear regression was used to determine independent predictors of health utility. Continuous covariates were categorised for the purpose of displaying univariate associations and assessing linearity, but were included as continuous in the multivariable model. Functional form was assessed using fractional polynomials [18]. Missing data was handled by performing multiple imputation in which the candidate explanatory factors previously described were imputed on the basis of each other using chained imputation [19]. Reported results are based on multiple imputation results and the presented model is the averaged results from 50 imputations. All analyses were undertaken using Stat version 11 (Stata Statistical Software: Release 11. College Station, TX: StataCorp LP. 2009).
The study protocol was approved by the Leeds East Research Ethics Committee (reference 07/Q1206/24).
Results
We identified 2427 eligible cases between 11 February 2008 and 5 May 2008 in Sheffield, 1673 cases between 19 November 2007 and 24 February 2008 in Barnsley and 1660 cases between 19 November 2007 and 25 February 2008 in Rotherham. Out of the total of 5760 cases, 541 (9.4%) were identified as having died by 30 days after attendance: 519 were identified from the hospital computer system with no additional cases from local Coroner's records, while 22 were identified after relatives returned the questionnaire or contacted us following inadvertent mailing of someone who had died. Completed questionnaires were received from 2488 patients (47.7% of those alive at 30 days), while 71 patients declined to participate by returning an empty questionnaire and the remainder did not respond.
Table 1 shows the proportion of patients who had died by 30 days after hospital attendance and the proportion of those mailed who responded, according to baseline patient characteristics. The response rate was lowest among the youngest and oldest, and highest in the 60-69 year group. Patients diagnosed with diseases of the circulatory system, musculoskeletal system or nervous system had higher response rates while those diagnosed with diseases of the skin and subcutaneous tissue, endocrine, nutritional and metabolic diseases, mental and behavioural disorders or neoplasms had lower response rates. Patients with a history of chronic respiratory disease or heart disease, and those on long-term steroid or warfarin therapy had higher response rates than those without these co-morbidities.
Table 1.
Death and response rate in relation to patient characteristics
| N | Death rate n (%) | Response rate* n (%) | P-value for response rate* | |
|---|---|---|---|---|
| Overall | 5760 | 541 (9.4%) | 2487 (47.7%) | |
| Gender | 0.400 | |||
| Females | 2995 | 279 (9.3%) | 1273 (46.9%) | |
| Males | 2710 | 255 (9.4%) | 1193 (48.6%) | |
| Age | < 0.001 | |||
| Under 30 | 355 | 2 (0.6%) | 108 (30.6%) | |
| 30-39 | 368 | 4 (1.1%) | 117 (32.1%) | |
| 40-49 | 504 | 4 (0.8%) | 200 (40.0%) | |
| 50-59 | 516 | 19 (3.7%) | 258 (51.9%) | |
| 60-69 | 823 | 69 (8.4%) | 440 (58.4%) | |
| 70-79 | 1301 | 137 (10.5%) | 636 (54.6%) | |
| 80-89 | 1441 | 219 (15.2%) | 594 (48.6%) | |
| 90 or above | 422 | 82 (19.4%) | 122 (35.9%) | |
| Centre | < 0.001 | |||
| Barnsley | 1673 | 127 (7.6%) | 779 (50.4%) | |
| Rotherham | 1660 | 188 (11.3%) | 733 (49.8%) | |
| Sheffield | 2427 | 226 (9.3%) | 975 (44.3%) | |
| Hospital admission within the last 30 days | 0.007 | |||
| Yes | 879 | 93 (10.6%) | 361 (45.9%) | |
| No | 2734 | 259 (9.5%) | 1138 (46.0%) | |
| Unknown | 2147 | 189 (8.8%) | 988 (50.5%) | |
| ICD-10 code** | < 0.001 | |||
| Certain infectious and parasitic diseases | 118 | 24 (20.3%) | 47 (50.0%) | |
| Diseases of the circulatory system | 1074 | 148 (13.8%) | 506 (54.6%) | |
| Diseases of the digestive system | 530 | 29 (5.5%) | 228 (45.5%) | |
| Diseases of the genitourinary system | 296 | 22 (7.4%) | 114 (41.6%) | |
| Diseases of the musculoskeletal system and connective tissue | 114 | 1 (0.9%) | 59 (52.2%) | |
| Diseases of the nervous system | 180 | 6 (3.3%) | 94 (54.0%) | |
| Diseases of the respiratory system | 1060 | 174 (16.4%) | 451 (50.9%) | |
| Diseases of the skin and subcutaneous tissue | 50 | 4 (8.0%) | 12 (26.1%) | |
| Endocrine, nutritional and metabolic diseases | 96 | 4 (4.2%) | 32 (34.8%) | |
| Injury, poisoning and certain other consequences of external causes | 845 | 47 (5.6%) | 339 (42.5%) | |
| Mental and behavioural disorders | 120 | 4 (3.3%) | 42 (36.2%) | |
| Neoplasms | 110 | 46 (41.8%) | 23 (35.9%) | |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 1088 | 24 (2.2%) | 508 (47.7%) | |
| Other | 60 | 2 (3.3%) | 29 (50.0%) | |
| Unknown | 19 | 6 (31.6%) | 3 (23.1%) | |
| History of chronic respiratory disease | 746 | 96 (12.9%) | 359 (55.2%) | < 0.001 |
| History of heart disease | 1902 | 211 (11.1%) | 898 (53.1%) | < 0.001 |
| History of active malignancy | 266 | 84 (31.6%) | 86 (47.3%) | 0.91 |
| History of asthma | 661 | 44 (6.7%) | 291 (47.2%) | 0.792 |
| History of diabetes | 896 | 79 (8.8%) | 399 (48.8%) | 0.464 |
| History of epilepsy | 235 | 18 (7.7%) | 94 (43.3%) | 0.192 |
| On warfarin therapy | 319 | 33 (10.3%) | 180 (62.9%) | < 0.001 |
| On steroid therapy | 296 | 44 (14.9%) | 146 (57.9%) | < 0.001 |
* excluding deaths within 30 days
**primary discharge diagnosis
Table 2 shows the responses to each EQ-5D question. Most respondents reported at least some problems with each aspect of health and only about one in four were able to perform their usual activities or free from pain or discomfort.
Table 2.
Responses to individual EQ-5D questions
| No problems | Some problems | Severe problems | |
|---|---|---|---|
| Mobility | 701 (28%) | 1682 (68%) | 104 (4%) |
| Self care | 1256 (50%) | 1041 (42%) | 190 (8%) |
| Usual activities | 604 (24%) | 1290 (52%) | 593 (24%) |
| Pain/discomfort | 552 (22%) | 1517 (61%) | 418 (17%) |
| Anxiety/depression | 1147 (46%) | 1116 (45%) | 224 (9%) |
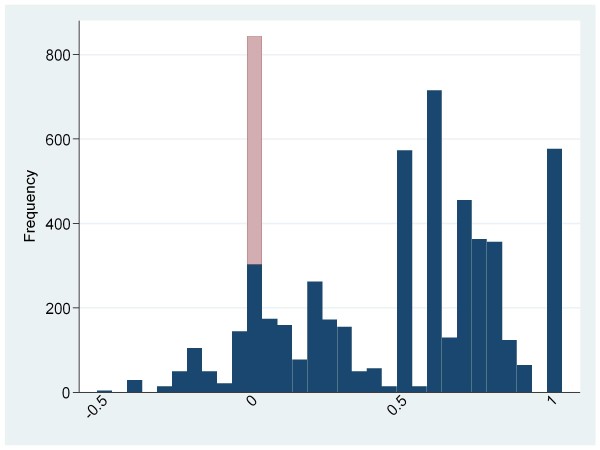
Figure 1 shows health utility for the population and Figure 2 shows health utility compared to regional age and gender adjusted norms. Dead patients are included in these figures with a health utility of zero while values derived from the survey are weighted to allow for non-response. In both figures the dead patients are shaded in pale gray while the survivors are dark gray. Health utility was generally poor compared to age and gender adjusted regional norms. A substantial proportion of patients had health utility well below normal values (75% of patients had health utility below their normal value; mean loss 0.32, 95% CI 0.31 to 0.33) and a significant proportion (11%) had health utility below zero.
Figure 1.
Health utility of the study population. Survivors are shaded in dark gray, dead patients in pale gray.
Figure 2.
Health utility loss compared to age and gender adjusted regional norms. Survivors are shaded in dark gray, dead patients in pale gray.
Mean health utility among survivors was 0.49 (standard deviation 0.35) while mean health utility in the whole cohort (i.e. including non-survivors) was 0.45 (0.36). Table 3 shows the association between patient characteristics and health utility. Mean health utility was lower in women, older patients and those with a recent hospital admission, recorded co-morbidities, neoplasms, diseases of the musculoskeletal system and connective tissue, diseases of the skin and subcutaneous tissue, diseases of the respiratory system, on steroid therapy and with abnormal physiological values or systolic blood pressure < 120 mmHg at presentation. On multivariable modelling (Table 4) health utility was reduced with increased age and lower GCS, varied according to ICD-10 and was lower among females, patients with recent hospital admission, on steroid therapy, or history of any of chronic respiratory disease, malignancy, diabetes and epilepsy. Other variables, most notably the physiological variables heart rate, respiratory rate, peripheral oxygen saturation and blood pressure, were not significant predictors of health utility in multivariate analysis.
Table 3.
Health utility estimates stratified by patient characteristics
| Factor | N | N dead | Mean | SD | Median | p |
|---|---|---|---|---|---|---|
| Overall | 3028 | 541 | 0.45 | 0.36 | 0.52 | |
| Gender | < 0.001 | |||||
| Females | 1552 | 279 | 0.43 | 0.36 | 0.52 | |
| Males | 1448 | 255 | 0.48 | 0.37 | 0.59 | |
| Age | < 0.001 | |||||
| Under 30 | 110 | 2 | 0.65 | 0.38 | 0.76 | |
| 30-39 | 121 | 4 | 0.58 | 0.37 | 0.69 | |
| 40-49 | 204 | 4 | 0.53 | 0.40 | 0.69 | |
| 50-59 | 277 | 19 | 0.47 | 0.36 | 0.59 | |
| 60-69 | 509 | 69 | 0.45 | 0.37 | 0.52 | |
| 70-79 | 773 | 137 | 0.43 | 0.35 | 0.52 | |
| 80-89 | 813 | 219 | 0.40 | 0.34 | 0.52 | |
| 90 or above | 204 | 82 | 0.29 | 0.30 | 0.25 | |
| Centre | 0.071 | |||||
| Barnsley | 906 | 127 | 0.47 | 0.36 | 0.59 | |
| Rotherham | 921 | 188 | 0.44 | 0.36 | 0.52 | |
| Sheffield | 1201 | 226 | 0.44 | 0.37 | 0.52 | |
| Previous hospital admission | < 0.001 | |||||
| Yes | 454 | 93 | 0.35 | 0.36 | 0.29 | |
| No | 1397 | 259 | 0.46 | 0.37 | 0.52 | |
| Unknown | 1177 | 189 | 0.48 | 0.36 | 0.59 | |
| ICD-10 code | < 0.001 | |||||
| Certain infectious and parasitic diseases | 71 | 24 | 0.43 | 0.41 | 0.52 | |
| Diseases of the circulatory system | 654 | 148 | 0.46 | 0.36 | 0.56 | |
| Diseases of the digestive system | 257 | 29 | 0.53 | 0.36 | 0.62 | |
| Diseases of the genitourinary system | 136 | 22 | 0.43 | 0.39 | 0.52 | |
| Diseases of the musculoskeletal system and connective tissue | 60 | 1 | 0.33 | 0.34 | 0.52 | |
| Diseases of the nervous system | 100 | 6 | 0.51 | 0.36 | 0.59 | |
| Diseases of the respiratory system | 625 | 174 | 0.39 | 0.37 | 0.38 | |
| Diseases of the skin and subcutaneous tissue | 16 | 4 | 0.36 | 0.38 | 0.52 | |
| Endocrine, nutritional and metabolic diseases | 36 | 4 | 0.63 | 0.34 | 0.69 | |
| Injury, poisoning and certain other consequences of external causes | 386 | 47 | 0.43 | 0.34 | 0.52 | |
| Mental and behavioural disorders | 46 | 4 | 0.46 | 0.36 | 0.52 | |
| Neoplasms | 69 | 46 | 0.18 | 0.33 | 0.00 | |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 532 | 24 | 0.50 | 0.35 | 0.59 | |
| Other | 31 | 2 | 0.55 | 0.35 | 0.59 | |
| Unknown | 9 | 6 | 0.41 | 0.47 | 0.19 | |
| History of chronic respiratory disease | 455 | 96 | 0.32 | 0.32 | 0.29 | < 0.001 |
| History of heart disease | 1109 | 211 | 0.41 | 0.34 | 0.52 | < 0.001 |
| History of active malignancy | 170 | 84 | 0.29 | 0.35 | 0.19 | < 0.001 |
| History of asthma | 335 | 44 | 0.41 | 0.36 | 0.52 | 0.048 |
| History of diabetes | 478 | 79 | 0.40 | 0.35 | 0.52 | 0.003 |
| History of epilepsy | 112 | 18 | 0.39 | 0.38 | 0.52 | 0.074 |
| On warfarin therapy | 213 | 33 | 0.41 | 0.34 | 0.52 | 0.126 |
| On steroid therapy | 190 | 44 | 0.30 | 0.33 | 0.26 | < 0.001 |
| Glasgow coma scale | < 0.001 | |||||
| < = 8 | 111 | 67 | 0.24 | 0.36 | 0.03 | |
| 9-12 | 126 | 61 | 0.34 | 0.37 | 0.25 | |
| 13-15 | 2706 | 384 | 0.47 | 0.36 | 0.58 | |
| Missing | 85 | 29 | 0.32 | 0.33 | 0.36 | |
| Oxygen saturation (%) | < 0.001 | |||||
| > 93(air)/> 98(O2) | 1913 | 206 | 0.48 | 0.36 | 0.59 | |
| 90-93(air)/94-98(O2) | 541 | 120 | 0.42 | 0.36 | 0.52 | |
| < 90(air)/< 94(O2) | 472 | 175 | 0.36 | 0.36 | 0.29 | |
| Missing | 102 | 40 | 0.35 | 0.37 | 0.36 | |
| Systolic blood pressure (mmHg) | 0.002 | |||||
| 120-180 | 1967 | 274 | 0.46 | 0.36 | 0.58 | |
| > 180 | 364 | 48 | 0.46 | 0.35 | 0.59 | |
| 100-119 | 365 | 104 | 0.42 | 0.37 | 0.52 | |
| < 100 | 274 | 95 | 0.40 | 0.38 | 0.52 | |
| Missing | 58 | 20 | 0.31 | 0.36 | 0.36 | |
| Heart rate (per minute) | 0.003 | |||||
| 60-100 | 1874 | 287 | 0.46 | 0.36 | 0.55 | |
| 101-130 | 745 | 153 | 0.42 | 0.37 | 0.52 | |
| > 130 | 168 | 51 | 0.43 | 0.38 | 0.52 | |
| < 60 | 188 | 33 | 0.51 | 0.37 | 0.62 | |
| Missing | 53 | 17 | 0.33 | 0.36 | 0.36 | |
| Respiratory rate (per minute) | < 0.001 | |||||
| 10-25 | 2359 | 329 | 0.48 | 0.36 | 0.59 | |
| > 25 | 525 | 170 | 0.37 | 0.37 | 0.29 | |
| < 10 | 13 | 5 | 0.25 | 0.38 | 0.08 | |
| Missing | 131 | 37 | 0.34 | 0.35 | 0.36 |
Note: responders alive at 30 days are upweighted by the inverse of the age & gender specific response rate
Table 4.
Multivariable analysis of factors associated with health utility (EQ-5D score)
| Beta | 95% CI | p | |
|---|---|---|---|
| Factor | |||
| Gender (male v female) | 0.049 | 0.016, 0.082 | 0.003 |
| Previous hospital admission within 30 days (yes v no) | -0.101 | -0.138, -0.064 | < 0.001 |
| ICD-10 code | |||
| Certain infectious and parasitic diseases | (reference) | < 0.001 | |
| Diseases of the circulatory system | 0.043 | -0.066, 0.151 | |
| Diseases of the digestive system | 0.119 | 0.003, 0.235 | |
| Diseases of the genitourinary system | -0.007 | -0.133, 0.120 | |
| Diseases of the musculoskeletal system and connective tissue | -0.091 | -0.238, 0.057 | |
| Diseases of the nervous system | 0.127 | -0.009, 0.263 | |
| Diseases of the respiratory system | 0.053 | -0.056, 0.163 | |
| Diseases of the skin and subcutaneous tissue | -0.275 | -0.526, -0.023 | |
| Endocrine, nutritional and metabolic diseases | 0.180 | 0.011, 0.348 | |
| Injury, poisoning and certain other consequences of external causes | -0.012 | -0.123, 0.100 | |
| Mental and behavioural disorders | -0.014 | -0.165, 0.137 | |
| Neoplasms | -0.091 | -0.253, 0.072 | |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 0.085 | -0.024, 0.194 | |
| Other | 0.128 | -0.042, 0.298 | |
| Unknown | |||
| History of chronic respiratory disease | -0.094 | -0.144, -0.043 | < 0.001 |
| History of active malignancy | -0.111 | -0.190, -0.032 | 0.006 |
| History of diabetes | -0.072 | -0.118, -0.026 | 0.002 |
| History of epilepsy | -0.101 | -0.186, -0.016 | 0.021 |
| On steroid therapy | -0.105 | -0.169, -0.041 | 0.001 |
| Age * | < 0.001 | ||
| Glasgow coma scale * | < 0.001 |
* EQ5D was reduced with increased age and lower GCS; both were monotonic but non-linear decreases for which a quadratic model produced an adequate fit, Age: Fitted line is -0.0015*Age-0.000018*Age2, GCS: Fitted line is 0.0043*GCS +0.000852*GCS2
R-squared statistic for the model = 12.6%.
Discussion
To our knowledge, this is the first study to measure health utility in an unselected cohort of patients after emergency medical admission. We found that health utility was markedly below regional age and gender adjusted norms and 11% of the population had health utility below zero. Measurement of mortality alone is inadequate in evaluating emergency medical treatments and services. If survivors have severely impaired health related quality of life then the value of interventions that improve survival alone may be open to question.
We identified patient characteristics that independently predicted health utility. Older patients, women, those with a low presenting GCS and those with recent hospital admission, on steroid therapy, or history of any of chronic respiratory disease, malignancy, diabetes or epilepsy had lower health utility. Non-randomized research and performance indicators measuring health utility should, if possible, measure and adjust for these covariates in analysis. Other baseline measures (heart rate, respiratory rate and blood pressure) were associated with health utility but were not independent predictors on multivariate analysis. These are potentially helpful findings because they indicate that the main independent predictors of health utility, with the exception of GCS, are likely to be routinely available and relatively easy to record for observational research. Additional efforts to record baseline physiology, with the exception of GCS, are unlikely to represent a worthwhile use of resources. However, it should be recognised that some of the factors were also associated with response rate. The estimated association between patient characteristics and health utility may therefore be influenced by responder bias. Furthermore, the R-squared statistic for the model (12.6%), whilst not especially low in the biomedical setting, suggests that the variables we identified only explain a modest proportion of variability. Examination of other co-morbidities, particularly those affecting mobility and mental health, could help to explain variability in health utility.
We deliberately selected a diverse sample. Emergency medical admissions include a substantial proportion of patients with ill-defined complaints or multiple morbidities, as reflected by the large group in our cohort with unclassified diagnoses. Including these patients is important to ensure a truly representative sample and attention is not focussed upon those with clearly defined single pathologies, but this can make it more difficult to draw inferences about the effects of intervention, if health utility data are used for this purpose.
Comparison of our data to previous studies of specific patient groups is complicated by differences in the timing of measurement, with most studies measuring health utility later than 30 days after admission, and previous studies limiting analysis to survivors. Even allowing for these differences our study suggests that at 30 days unselected emergency medical admissions, with a mean EQ-5D score among survivors of 0.49 (median 0.59), have worse health utility than patients suffering major trauma (median EQ-5D 0.73 at one year [9], mean 0.69 at 12-18 months [10]), stroke (mean 0.62 at 6 months [13]) or myocardial infarction (median 0.73 at 2 to 25 months [12]).
Our findings suggest that measuring health utility after emergency admission is feasible and potentially worthwhile. The response rate of 48% is sufficient for meaningful analysis and relatively high for an unsolicited mailing to an unselected sample, but carries a significant risk of responder bias. We have identified a number of factors that predict questionnaire response and need to be considered when planning future research. Although most deaths were identified though hospital systems we inadvertently mailed questionnaires to 22 patients who had died within 30 days. This risk was discussed with the ethics committee before the study and accepted as inevitable. However, inadvertent mailing to a deceased person has the potential to cause distress and should be taken into account when measuring health status.
An important implication of our study is that evaluations of emergency care, whether research or audit, that measure mortality without attempting to measure health related quality of life may fail to measure the true value of emergency care. Health utility after emergency admission is typically lower than age, gender and regional norms, and severely reduced in a substantial proportion.
Our study has a number of limitations. Only about half of the population responded and completed the questionnaire. We identified a number of factors predicting response which suggested that response was more likely among those aged 60-69 and those with co-morbidities, perhaps because these patients are more likely to be engaged in ongoing medical care. However, it is not clear what effect this bias will have on estimates of overall health utility.
The EQ-5D is a validated and widely used measure of health status, but when using the questionnaire patients do not directly value their health utility. Instead it is calculated using tariff values applied to the ratings they indicate on five dimensions of health. This means that the estimate of health utility generated by the EQ-5D for an individual may not equate to that individual's perception of their health status. This means that when the EQ-5D generates an estimate of less than zero for health utility we cannot assume that the individual rates their health status as being worse than death, only that their health status has been rated during EQ-5D validation as being worse than death. Furthermore, a single measurement at 30 days after hospital admission may represent a temporary state, associated with pain or loss of mobility for example, and should not be interpreted as a life not worth saving. Our study does not provide data on health changes after emergency medical admission or allow comparison to a control group, so we cannot draw inferences regarding the effectiveness or otherwise of the care provided.
The data presented in Figure 2 showing deviation from population norms should be interpreted with caution. The data are presented in this way to allow us to take into account population norms and should not be used to draw inferences about the quality of local emergency care or the implications of our findings for specific individuals. The cases with extreme values, in particular, may simply represent random variation with some people rating their health as good despite a low age and gender predicted value (and vice versa).
Finally, identifying patient characteristics that predict questionnaire response and health utility involved multiple hypothesis testing with the associated risk of spurious chance findings. We did not adjust statistical significance to account for multiple testing so would urge caution in interpreting findings with p-values between 0.05 and 0.01.
Conclusion
Health utility can be measured after emergency medical admission, although responder bias may be significant. Health utility after emergency medical admission is poor compared to population norms. We have identified independent predictors or health utility that need to be measured and taken into account in non-randomized evaluations of emergency care. Further research is required to determine whether the findings of our study can be reproduced in other regions, countries and emergency care settings. Research is also required to identify reasons for non-response, to determine how responder bias may influence estimates of health utility and to explore methods to improve questionnaire response in this setting.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SG and JN conceived and designed the study. RW and MS collected the data. MB analysed the data. SG wrote the first draft and all authors contributed to revision and preparation of the final draft. All authors read and approved the final manuscript.
Contributor Information
Steve W Goodacre, Email: s.goodacre@sheffield.ac.uk.
Richard W Wilson, Email: r.w.wilson@sheffield.ac.uk.
Mike Bradburn, Email: m.bradburn@sheffield.ac.uk.
Martina Santarelli, Email: m.santarelli@sheffield.ac.uk.
Jon P Nicholl, Email: j.nicholl@sheffield.ac.uk.
Acknowledgements
The study was funded by the United Kingdom Medical Research Council. The study funders had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The researchers were independent of the study funders.
We thank Susan Proctor, Jim Wardrope, Alison Walker, Julian Humphrey, Simon McCormick, Mike Clancy, Anne-Maree Kelly, Zoe Lowe, Lauren Bowden, Jill Burns, Sheila Briggs, Zoe White and the DAVROS Steering Committee (Fiona Lecky, Mark Gilthorpe, Jane Shewan, Rosemary Harper, Enid Hirst) for their help with this project.
References
- Cairns CB, Garrison HG, Hedges JR, Schriger DL, Valenzuela TD. Development of New Methods to Assess the Outcomes of Emergency Care. Ann Emerg Med. 1998;31:166–171. doi: 10.1016/S0196-0644(98)70324-5. [DOI] [PubMed] [Google Scholar]
- Spaite DW, Maio R, Garrison HG, Desmond JS, Gregor MA, Stiell IG, Cayten CG, Chew JL, MacKenzie EJ, Miller DR, O'Malley PJ. Emergency Medical Services Outcome Project (EMSOP) III: The role of risk adjustment in out-of-hospital outcomes research. Ann Emerg Med. 2002;40:79–88. doi: 10.1067/mem.2002.124758. [DOI] [PubMed] [Google Scholar]
- Jarman B, Bottle A, Aylin P, Browne M. Monitoring changes in hospital standardised mortality ratios. BMJ. 2005;330:329. doi: 10.1136/bmj.330.7487.329. doi: 10.1136/bmj.330.7487.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graff L, Stevens C, Spaite D, Foody J. Measuring and Improving Quality in Emergency Medicine. Acad Emerg Med. 2002;9:1091–1107. doi: 10.1111/j.1553-2712.2002.tb01563.x. [DOI] [PubMed] [Google Scholar]
- Welch SJ, Asplin BR, Stone-Griffith S, Davidson SJ, Augustine J, Schuur J. Emergency Department Operational Metrics, Measures and Definitions: Results of the Second Performance Measures and Benchmarking Summit. Ann Emerg Med. 2010. in press . [DOI] [PubMed]
- Lindsay P, Schull M, Bronskill S, Anderson G. The Development of Indicators to Measure the Quality of Clinical Care in Emergency Departments Following a Modified-Delphi Approach. Acad Emerg Med. 2002;9:1131–9. doi: 10.1111/j.1553-2712.2002.tb01567.x. [DOI] [PubMed] [Google Scholar]
- Beattie E, Mackway-Jones K. A Delphi study to identify performance indicators for emergency medicine. Emerg Med J. 2004;21:47–50. doi: 10.1136/emj.2003.001123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NINDS rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- Ringburg AN, Polinder S, van Ierland MC, Steyerberg EW, van Lieshout EM, Patka P, van Beeck EF, Schipper IB. Prevalence and Prognostic Factors of Disability After Major Trauma. J Trauma. 2011;70:916–22. doi: 10.1097/TA.0b013e3181f6bce8. [DOI] [PubMed] [Google Scholar]
- Holtslag HR, van Beeck EF, Lindeman E, Leenen LP. Determinants of long-term functional consequences after major trauma. J Trauma. 2007;62:919–27. doi: 10.1097/01.ta.0000224124.47646.62. [DOI] [PubMed] [Google Scholar]
- Polinder S, Haagsma JA, Bonsel G, Essink-Bot ML, Toet H, van Beeck EF. The measurement of long-term health-related quality of life after injury: comparison of EQ-5D and the health utilities index. Inj Prev. 2010;16:147–53. doi: 10.1136/ip.2009.022418. [DOI] [PubMed] [Google Scholar]
- Nowels D, McGloin J, Westfall JM, Holcomb S. Validation of the EQ-5D quality of life instrument in patients after myocardial infarction. Qual Life Res. 2005;14:95–105. doi: 10.1007/s11136-004-0614-4. [DOI] [PubMed] [Google Scholar]
- Pickard AS, Johnson JA, Feeny DH. Responsiveness of generic health-related quality of life measures in stroke. Qual Life Res. 2005;14:207–19. doi: 10.1007/s11136-004-3928-3. [DOI] [PubMed] [Google Scholar]
- The Euroqol Group. Euroqol: A new facility for the measurement of health related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- EQ-5D: A standardised instrument for use as a measure of health outcome. http://www.euroqol.org/ (accessed 25/11/11)
- Dolan P, Gudex C, Kind P, Williams A. Modelling valuations for the EuroQol health states. Medical care. 1997;35(11):1095–1108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- Kind P, Hardman G, Macran S. UK population norms for EQ5D. Centre for Health Economics, University of York; 1999. http://www.york.ac.uk/inst/che/pdf/DP172.pdf Discussion paper 172. [Google Scholar]
- Royston P, Altman DG. Regression using Fractional Polynomials of Continuous Covariates: Parsimonious Parametric Modelling. Journal of the Royal Statistical Society. Series C (Applied Statistics) 1994;43(3):429–467. [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: John Wiley; 1987. [Google Scholar]