Abstract
Objective
The aim of this study was to examine the difference of early maladaptive schemas and parenting origins in opioid abusers and non-opioid abusers.
Method
The early maladaptive schemas and parenting origins were compared in 56 opioid abusers and 56 non-opioids abusers. Schemas were assessed by the Young Schema Questionnaire 3rd (short form); and parenting origins were assessed by the Young Parenting Inventory.
Results
Data were analyzed by multivariate analysis of variance (MANOVA). The analysis showed that the means for schemas between opioid abusers and non-opioid abusers were different. Chi square test showed that parenting origins were significantly associated with their related schemas.
Conclusion
The early maladaptive schemas and parenting origins in opioid abusers were more than non-opioid abusers; and parenting origins were related to their Corresponding schemas.
Keywords: Cognitive aspects, opioid, parenting, Substance related disorders
Drug abuse, including opioids, is a global problem of significant proportions. Problematic drug use is now reported by several countries, including those within the developing world, particularly those countries close to or involved in the main trafficking routes (1). The most recent studies of drug abuse prevalence in Iran have indicated a serious and growing problem (2). Opioid dependence is diagnosed by the signs and symptoms associated with compulsive and prolonged self-administration of opioids. Persons with opioid dependence typically demonstrate continued use in spite of adverse physical, behavioral and psychological consequences (3, 4). Mokri reported that the Iranian addict is most likely to be “male, married and employed” (5). Considering the studies conducted in Iran, it seems that males constitute 95 percent of the population of clinical abusers; and male-female ratio is even 10 to 1 (5–7).
In the recent approaches, Young (8), and Beck, freeman and Davies (9) pied more attention to the importance of schemas-more pervasive and enduring psychological factors- in psychological disorders, including substance dependence. Young developed schema based on the concept of schema. Schema therapy provides a new system of psychotherapy that is especially well suited to patients with entrenched, chronic psychological disorders who have heretofore been considered difficult to treat.
Young hypothesized that some of these schemas-especially schemas that develop primarily as a result of toxic childhood experiences-might be at the core of many chronic disorders. To explore this idea, he defined a subset of schemas that he labeled Early Maladaptive Schemas. An Early Maladaptive Schema is a broad, pervasive theme or a pattern that comprised of memories, emotions, cognitions, and bodily sensations regarding oneself and one's relationships with others developed during childhood or adolescence, and elaborated throughout one's lifetime, and dysfunctional to a significant degree (8, 10).
Schema therapy can be useful and effective for patients with substance dependence. Therefore, Dual Focused Schema Therapy (DFST) is adapted for substance related disorders by Young, Ball, and Rounsaville. DFST model hypothesized that early maladaptive schemas form the core pathology in substance dependence. For example, substance abuse can occur as a direct behavioral expression if the activation of impaired limits schemas (entitlement, insufficient self-control) or when other-directness schema is triggered. Schemas of disconnection and rejection or impaired autonomy and performance are important as well (11, 12). Toxic childhood experiences are the primary origin of Early Maladaptive Schemas. To a large extent, the dynamics of a child's family are the dynamics of that child's entire early world. When patients find themselves in situations that activates their Early Maladaptive Schemas during adulthood; what they usually are experiencing is a drama from their childhood, usually with a parent (10). Parenting origins of schemas are important because they indicate that family Schemas have developed. Kaufman explored family interactions of heroin addicts and classified them according to dysfunctions described by Minuchin as following:
Enmeshed interaction: the family interacts through over-involvement and ineffective closeness, at the expense of the autonomy of different members.
Disengaged interaction: the interaction is distant and lacks emotion; closeness and a sense of belonging between family members are absent, allowing each family member to be a single unit. In addition, studies identified that most of the family relatives of heroin addicts interacted dysfunctionally. Of the mother–child relationships, 88% were enmeshed, and 3% were disengaged. On the other hand, 41% of father– child relationships were enmeshed, and 42% disengaged (13).
Psychotherapy with addicted individuals often involves a shift in therapeutic techniques during the transition from early to later recovery treatment. A conceptual model based on attachment theory can provide a rationale and framework for this shift in the treatment of some addicted persons (14). However, as Riso (11) has suggested, research in this area needs to evaluate whether Axis I and II patients differ from one another, as well as from control groups in the schemas. Very little is currently known about existence of early maladaptive schemas in Axis I patients. The main purpose of the current research is to study the main components that are suggested by schema theory in substance dependent patients compared with non- dependent individuals. Note that an effective clinical intervention is essentially dependent on accurate, comprehensive and well-studied therapeutic planning and theories.
Materials and Method
Participants were 56 opioid-dependent patients (clinical group) and 56 non- dependent (non-clinical group). Clinical sample group consisted of 20- to 45-year-old males, with a mean age of 29.74 years, who received diagnosis of substance dependence, and were in treatment period at least for 2 months. They were selected randomly from two addiction recovery centers in Iran, Qazvin. General inclusion criteria were: 1) male gender; 2) age>20 and <45 years old; 3) receiving diagnosis of only opioid dependence, according to the criteria of DSM-IV-TR; 4) holding education level of higher than elementary; 5) being in early partial remission, and receiving Methadone maintenance treatment. Structured clinical interview for DSM-IV disorders were used for selecting the clinical sample group. The non- dependent sample comprised of 56 males with age range of 20 to 45 years. They were selected from 2 state factories. Stratified sampling method was used for selecting workers based on their job-field. The subjects were excluded if they mentioned having a history of substance use. Based on their official profiles, they did not have a history of substance dependence or any clinical disorder. All the participants were examined using the measures below:Structured clinical interview for DSM-IV Axis I disorders (SCID-I): Selection of clinical sample was based on their files in clinics. After selecting each individual, SCID-I was used to ensure their opioid dependence. SCID-I is a semi-structured interview used to assess Axis I disorders. To yield a possible diagnosis, the interviewer queried each of the “yes” responses of those diagnoses for which there were a sufficient number of endorsed items (15).
Early Maladaptive Schema Questionnaire: The Early Maladaptive Schema Questionnaire is made by Young (10) to measure 17 early maladaptive schemas. YSQ-3ed (short form) is a 90-item instrument utilizing a 6-point Likert-type format. There are supports for the reliability and validity of this instrument in several studies (16, 17, 18). In Iran, Ghiasi (19) demonstrated the scale's validity. Ghiasi reported coefficient alphas of 0.94 for this Questionnaire, and in the range of 0.6 – 0.90 for subscales. In addition, the YSQ also showed good discriminant and convergent validity with respect to measures of dysfunctional Attitudes. In the present study, internal consistency for the scale was adequate (α=0.94).Young Parenting Inventory: The Young Parenting Inventory (YPI) is designed to identify parental origins of maladaptive schemas. YPI has 72 items, each of which is scored on a rating scale from 1 to 6. On each item, the patients score their parents separately based on how they treated the patients during childhood. Thus, YPI reflects the family environment that probably results in developing schemas. Social Isolation/Alienation schema is not measured by the YPI (The origin of Social Isolation is usually in the peer group rather than in parenting). Salavati (20) reported consistency coefficient of 0.69 for the YPI-Mother form and 0.80 for the YPI-Father form. In the present study, this instrument presented an internal consistency value of .90 for the YPI-mother form and .88 for the YPI-father form.
Results
To evaluate predominant schemas in substance abusers, frequencies of EMSs in subjects, whose score was higher than the cut point, were calculated. The results are shown in Table 1.
Table 1.
Frequencies of Early Maladaptive Schemas in opioid abusers and non-abusers
| Schema | Clinical group (abusers) | Control group (non-abusers) | ||
|---|---|---|---|---|
| frequency | percentage | frequency | percentage | |
| Abandonment/Instability | 53 | 94.6 | 5 | 8.9 |
| Emotional Deprivation | 50 | 89.28 | 17 | 30.4 |
| Punishment | 48 | 85.7 | 15 | 26.7 |
| Social Isolation/Alienation | 47 | 83.9 | 10 | 17.9 |
| Unrelenting Standards/Hyper criticalness | 47 | 83.9 | 12 | 21.4 |
| Insufficient Self-Control/Self-Discipline | 46 | 82.1 | 12 | 21.4 |
| Self-Sacrifice | 39 | 66.1 | 6 | 10.7 |
| Defectiveness/Shame | 30 | 53.57 | 4 | 7.14 |
| Approval-Seeking/Recognition-Seeking | 29 | 51.78 | 5 | 8.9 |
| Enmeshment/Undeveloped Self | 27 | 48.2 | 6 | 10.7 |
| Dependence/Incompetence | 26 | 46.4 | 4 | 7.14 |
| Vulnerability To Harm Or Illness | 25 | 44.64 | 6 | 10.7 |
| Mistrust/Abuse | 25 | 44.64 | 5 | 8.9 |
| Entitlement/Grandiosity | 24 | 42.9 | 3 | 5.35 |
| Failure | 13 | 23.2 | 7 | 12.5 |
| Negativity/Pessimism | 12 | 21.4 | 5 | 8.9 |
| Emotional Inhibition | 12 | 21.4 | 6 | 10.7 |
| Subjugation | 10 | 17.9 | 4 | 7.14 |
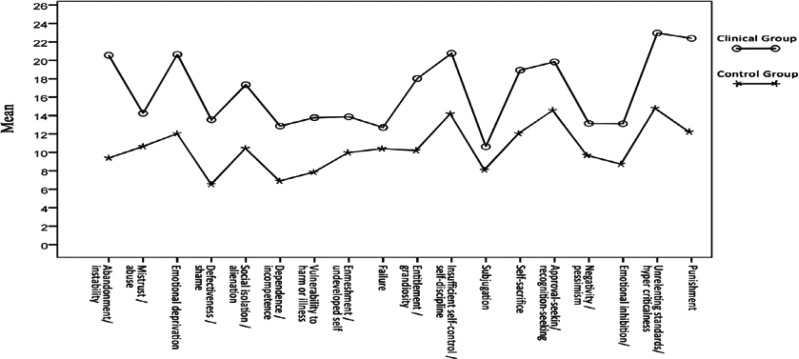
Means for schemas in both clinical and control groups are presented in Figure 1. The means for all EMSs in the clinical group are higher than the control group. This difference is especially more apparent in Abandonment/Instability, Emotional Deprivation, Social Isolation /Alienation, Entitlement /Grandiosity, Insufficient Self-Control/Self-Discipline, Self-Sacrifice, Approval-Seeking/Recognition-Seeking, Unrelenting Standards/Hyper criticalness, and Punishment schemas.
Figure 1.
Means for Early Maladaptive Schemas in Clinical and Control Groups
In order to analyze the differences between the means for EMSs in the two sample groups, multivariate analysis of variance (MANOVA) was performed. According to Table 2, the two groups differ significantly in terms of EMSs (F18, 93=53.530, P<.0001, Partial η2= .912) and EMSs Domains (F5, 106=44.970, P<.0001, Partial η2= .68).
Table 2.
Results of multivariate analysis of variance for comparing means for Early Maladaptive Schemas and Schema Domains in Clinical group with non-clinical group
| Effect | Value | F | Sig. | Partial Eta Squared |
|---|---|---|---|---|
| Wilk's Lambda (Schemas) | .088 | 53.530 | .0001** | .912 |
| Wilk's Lambda (Schemas Domains) | .320 | 44.970 | .0001** | .680 |
*P≤0.05
P≤0.01
Using Bonferroni adjustment (α<.002), the analysis of each EMSs is presented in table 3. As depicted in table 3, a significant difference was observed in all EMSs between the clinical and control groups. The largest effect sizes (the most difference among two groups) belonged to Abandonment/Instability (Partial η2= .733), Punishment (Partial η2=.644), Unrelenting Standards/Hyper criticalness (Partial η2=.6), Defectiveness/Shame (Partial η2=.592), Dependence/Incompetence (Partial η2= .533), and Entitlement/Grandiosity (Partial η2= .521). Moreover, a significant difference was also observed in all EMS‘s Domains between the two groups. The largest effect sizes of Domains were related to Disconnection & Rejection (Partial η2= .602) and Over vigilance & Inhibition (Partial η2= .638).
Table 3.
Results of Tests of Between-Subjects Effects for comparing means for Early Maladaptive Schemas and Schema Domains in Clinical group with non-clinical group
| Source Dependent Variable (Schemas) | F | Sig. | Partial Eta Squared | |
|---|---|---|---|---|
| 1 stDomain | 1- Abandonment/Instability | 301.362 | .0001** | .733 |
| 2- Mistrust/Abuse | 33.477 | .0001** | .233 | |
| 3- Emotional Deprivation | 97.229 | .0001** | .469 | |
| 4- Defectiveness/Shame | 159.651 | .0001** | .592 | |
| 5- Social Isolation/Alienation | 85.013 | .0001** | .436 | |
| 2 stDomain | 6- Dependence/Incompetence | 125.755 | .0001** | .533 |
| 7- Vulnerability To Harm Or Illness | 81.507 | .0001** | .426 | |
| 8- Enmeshment/Undeveloped Self | 41.623 | .0001** | .275 | |
| 9- Failure | 14.099 | .0001** | .154 | |
| 3 rdDomain | ||||
| 10- Entitlement/Grandiosity | 119.555 | .0001** | .521 | |
| 11- Insufficient Self-Control/Self-Discipline | 78.949 | .0001** | .418 | |
| 4 thDomain | 12- Subjugation | 13.171 | .0001** | .107 |
| 13- Self-Sacrifice | 101.225 | .0001** | .479 | |
| 14- -Seeking/Recognition-Seeking | 54.369 | .0001** | .331 | |
| 5 thDomain | 15- Negativity/Pessimism | 25.981 | .0001** | .191 |
| 16- Emotional Inhibition | 59.848 | .0001** | .352 | |
| 17- Unrelenting Standards/Hyper criticalness | 178.946 | .0001** | .619 | |
| 18- Punishment | 198.668 | .0001** | .644 | |
| Schema Domains | Disconnection & Rejection | 166.202 | .0001** | .602 |
| Impaired Autonomy & Performance | 94.064 | .0001** | .461 | |
| Impaired Limits | 128.416 | .0001** | .539 | |
| Other-Directedness | 87.655 | .0001** | .443 | |
| Over vigilance & Inhibition | 193.741 | .0001** | .638 |
*P≤0.05
P≤0.01
Multivariate analysis of variance (MANOVA) was used to analyze the means differences of parenting origins between the clinical and control groups.
The two groups differed significantly in terms of parenting origins.
The only exceptions, where the means differences were not significant, were Mistrust/Abuse, Defectiveness/Shame, Dependence/Incompetence, and Failure in mother parenting origins, and Failure, Defectiveness/Shame, and Self-Sacrifice in father parenting origins. All other parenting origins were significantly different between the two sample groups. Opioid abuser group had higher scores in parenting origins than the control group.
Chi-squares were used to analyze the distribution of parental origins in EMSs. Using the cut point of YPI and YSQ, each person was assigned to one of the two following groups named “with Schema” or “without Schema”; and was also assigned to one of the two groups of 〜with parenting origin〝 or 〜without parenting origin〝 (2x2 Contingency Table). The goal was to examine whether individuals with EMSs have a parenting origin related to their EMSs. Results are shown in table 4 (Mother parenting origin) and table 5 (Father parenting origins)
Table 4.
Result of Chi Squared test for relation among Mother Parenting Origins and Schemas in clinical sample (n=56)
| parenting origin | Individual with Schema | Individual without Schema | χ2 | Sig. | ||
|---|---|---|---|---|---|---|
| With parenting origin | Without parenting origin | With parenting origin | Without parenting origin | |||
| 1-Abandonment/Instability | 47 | 6 | 1 | 2 | 6.01 | .01** |
| 2-Mistrust/Abuse | 19 | 6 | 3 | 28 | 2.52 | .119 |
| 3- Emotional Deprivation | 40 | 10 | 1 | 5 | 10.96 | .01** |
| 4-Defectiveness/Shame | 21 | 9 | 9 | 17 | 7.01 | .008** |
| 6-Dependence/Incompetence | 23 | 3 | 11 | 19 | 15.67 | .0001** |
| 7-Vulnerability To Harm Or Illness | 17 | 8 | 27 | 4 | 2.99 | .08 |
| 8-Enmeshment/Undeveloped Self | 17 | 10 | 9 | 20 | 5.73 | .01** |
| 9-Failure | 10 | 3 | 11 | 32 | 11.22 | .01** |
| 10-Entitlement/Grandiosity | 16 | 8 | 9 | 23 | 8.24 | .04** |
| 11-Insufficient Self-Control/Self-Discipline | 38 | 8 | 0 | 10 | 25.7 | .001** |
| 12-Subjugation | 8 | 2 | 16 | 30 | 6.86 | .009** |
| 13-Self-Sacrifice | 26 | 13 | 5 | 12 | 6.65 | .01** |
| 14-Approval-Seeking/Recognition-Seeking | 26 | 3 | 10 | 17 | 16.86 | .0001** |
| 15-Negativity/Pessimism | 12 | 0 | 12 | 32 | 20.36 | .0001** |
| 16-Emotional Inhibition | 11 | 1 | 20 | 24 | 8.15 | .004** |
| 17- Unrelenting Standards/Hyper criticalness | 28 | 19 | 4 | 7 | 1.63 | .2 |
| 18-Punishment | 28 | 20 | 1 | 7 | 5.77 | .01** |
*P≤0.05
P≤0.01
Table 5.
- Result of Chi Square test for relation among Father Parenting Origins and Schemas in clinical sample (n=56)
| parenting origin | Individual with Schema | Individual without Schema | χ2 | Sig. | ||
|---|---|---|---|---|---|---|
| With parenting origin | Without parenting origin | With parenting origin | Without parenting origin | |||
| 1-Abandonment/Instability | 40 | 13 | 0 | 3 | 7.29 | .005** |
| 2-Mistrust/Abuse | 17 | 8 | 7 | 24 | 11.66 | .001** |
| 3- Emotional Deprivation | 43 | 7 | 1 | 5 | 15.29 | .0001** |
| 4-Defectiveness/Shame | 23 | 7 | 4 | 22 | 20.95 | .0001** |
| 6-Dependence/Incompetence | 17 | 9 | 11 | 19 | 4.59 | .03* |
| 7-Vulnerability To Harm Or Illness | 20 | 5 | 14 | 17 | 7.04 | .008** |
| 8-Enmeshment/Undeveloped Self | 20 | 7 | 8 | 21 | 12.08 | .001** |
| 9-Failure | 9 | 4 | 12 | 31 | 7.27 | .007** |
| 10-Entitlement/Grandiosity | 21 | 3 | 6 | 26 | 25.96 | .0001** |
| 11-Insufficient Self-Control/Self-Discipline | 39 | 7 | 6 | 4 | 3.19 | 0.07 |
| 12-Subjugation | 6 | 4 | 20 | 26 | .901 | .34 |
| 13-Self-Sacrifice | 29 | 10 | 2 | 15 | 18.77 | .0001** |
| 14-Approval-Seeking/Recognition-Seeking | 25 | 4 | 13 | 14 | 9.28 | .002** |
| 15-Negativity/Pessimism | 11 | 1 | 8 | 36 | 22.71 | .0001** |
| 16-Emotional Inhibition | 12 | 0 | 11 | 33 | 21.91 | .0001** |
| 17- Unrelenting Standards/Hypercriticalness | 38 | 9 | 3 | 8 | 14.73 | .0001** |
| 18-Punishment | 41 | 7 | 2 | 6 | 14.04 | .0001** |
P≤0.05
P≤0.01
Discussion
This study was designed to compare EMSs among opioid-addicted and non-addicted individuals to evaluate the predominant EMSs in opioid dependence disorder, and finally to examine the relationship between EMSs and parental origins.
In recent years, some studies on Young theory have been oriented toward diagnosing the predominant EMSs in Axis I and II psychological disorders, such as depression (17), social phobias (21), personality disorder (20) and eating disorder (22). One of the main goals of the present study was to determine predominant EMSs in opioid dependence disorder. Results showed that in opioid dependent patients, Abandonment/ Instability, Mistrust/Abuse, Emotional Deprivation, Defectiveness/Shame, Dependence/ Incompetence, and Social Isolation/Alienation are predominant schemas that have the most frequencies and the greatest mean differences when compared with non-addicted males. These schemas belong to Impaired Limits, Overvigilance & Inhibition, and Disconnection & Rejection domains. According to Riso (11), addictive behaviors can be caused directly by activation of Impaired Limits schemas. Of course, findings showed that Overvigilance & Inhibition, and Disconnection & Rejection domains are also important in opioid dependence. Decouvelaere, Graziani, Fackiere-Eraldi, Rusinek, and Hautekeete (23) reported that schemas of the Impaired Limits domain and Mistrust/Abuse, self-sacrifice, and Abandonment/Instability are salient in alcohol dependent patients; their finding was consistent with ours. Likewise, in substance dependent patients, high scores on schemas of Emotional Deprivation and Vulnerability to harm were reported by Brotchie, Meyer, Copello, Kidney, and Waller (24). The present study also showed high frequency of Vulnerability to harm schema in dependent patients.
The schemas of Abandonment/Instability and Emotional Deprivation belong to Disconnection & Rejection domain. It‘s expected that one‘s needs-whose schemas are in this domain-for security, safety, stability, nurturance, empathy, sharing of feelings, acceptance, and respect will not be met in a predictable manner. Typically, the schemas of this domain are developed in families that are detached, cold, rejecting, withholding, lonely, explosive, unpredictable, or abusive. Likewise, Rees & Wilborn (25), Kaufman (13), and other researchers have said that interactions and relations in these families are dysfunctional. The patients scored higher on Impaired limits domain (Insufficient Self-Control/Self-Discipline). As Young described, these patients have deficiencies in internal limits, responsibility to others, or long-term goal-orientation. They have difficulty or refusal to exercise sufficient self-control and frustration tolerance and finally they lack sufficient social norm, commitment and personality solidary (10). These characteristics lead to difficulty in respecting the rights of others, cooperating with others, making commitments, or setting and meeting realistic personal goals. Therefore, these patients do not restrict themselves with rational limits; and such personality pattern can increase susceptibility to such abnormal behaviors as substance abuse. Insufficient self-control and lack of rational limits in our findings are similar to Verheul theory (26) about behavioral disinhibition pathway to addiction, that predicts individuals who score high in lack of limits, antisociability and impulsiveness have lower thresholds to deviant behaviors such as substance abuse.
Finally, it can be said that our finding is consistent with previous researches in that the role of personality in etiology of substance dependency was emphasized. Of course, as Verheul (26) mentioned, it does not mean that there are some pre-addictive personality, or addiction in symptoms of underlying personality disorder. It suggests that personality traits and characteristics are important ethological factors as described in behavioral diathesis-stress model-and must be noticed in clinical works. Results showed that the dependent group scored higher on almost all schemas. This finding was repeated in several studies (19, 23, 27). Our finding may reflect dysfunctional reactions to internal and external stimulations that may be resulted from their generalized-negative-thoughts. A schema develops primarily as a result of toxic childhood experiences. Relationship with parents is the most important part of experiences in early years of life, as described in many developmental theories, like object relation theory. One aim of the present study was to compare opioid dependent patients with non-dependent individuals in EMS‘s parenting origins, and to examine relation of EMSs and parenting origins. Our finding indicated that approximately all EMSs were related to their parenting origins. This finding endorses Young theory about the relation between EMSs and parenting origins. Note that this is one of the first researches about parenting origins, and more studies are required on this issue. Furthermore, results showed that opioid dependent patients score higher on parenting origins than non-dependent individuals. The greatest difference was related to parenting origins of punishment, Abandonment/Instability, Emotional Deprivation, and Emotional Inhibition (Mothers origins), and Emotional Inhibition, Approval-Seeking/Recognition-Seeking, Punishment, Abandonment/Instability, and Emotional Deprivation (Father origins). These findings are consistent with other previous researches (28, 31). Schenberg (32) described the parent of these patients as hot-tempered, punitive, careless and rejecting. Rees & Wilborn (25) said that parents of addicted individuals are hostile and careless or overprotective. Our finding indicates that parenting origins that seem to be punitive, emotionally deprived, emotionally inhibited, and unstable are common in opioid dependent patients. This parenting styles can result in impairing and frustrating child‘s emotional needs and emotional development. There is a general agreement among specialists that substance abuse is related to family dynamics and interactions. Family, as a unit, strives to regain stability and homeostasis, developing complex coping strategies and interactions which may contribute to the chronic course of the individual's drug abusing career. Parent psychological problems, parent substance use, and parenting behaviors have all been found to be important predictors of adolescent outcomes and paternal parenting behaviors are strong predictors of adolescent substance use (9, 28, 33). The awareness of such family processes and interactions is of utmost importance in understanding the nature and progression of the problem of drug abuse by the family member. Studies identified that most of the family relatives of opioid addicts interacted dysfunctionally. Explaining the procedure of schema‘s development and origins, Young (10) have referred to dysfunctional interactions among family members, especially child-parents relations, and noted that both overprotection and carelessness can frustrate gratifications of child‘s basic needs. Therefore, dysfunctional child-parents interactions were expected, and our finding also endorsed this point. The presence of such parenting origins as abandonment/ instability and emotional deprivation indicates distant interactions, and lack of emotions and solidarity.
One notable finding was about the differences among maternal and paternal origins. Almost all paternal and maternal origins significantly differed between abusers and non-abusers. One exception was the origins of mistrust/ abuse and self-sacrifice schema. Actually, only differences of paternal origins of mistrust/ abuse schema, and maternal origins of self-sacrifice schema were significant. Coley (31) has noted that father–child relationships are influenced by behavioral factors more than mother-child relationships; and Kauffman‘s studies (13) showed that almost 89% of mother-child relationships were overprotective and enmeshed, and only 3% were disengaged. On the other hand, 41% of father–child relationships were enmeshed, and 42% were disengaged. Mistrust, abuse, and misbehavior in fathers-child relations, and dysfunctional emotional engagements in mothers-child relations in addictive individual‘s families can be construed from our findings as well.
One restriction of this research was the sample group. All participants were male. It must be noticed that substance abuse pathology– and thus predominant EMSs in females may be different. The result of this study may not be generalized to female abuser population. Moreover, this study was conducted on opioid abuser patients and more studies on other drugs are needed.
Conclusion
Some schemas are more frequent in opioid abusers. Recognizing predominant EMSs may be useful in conceptualization of clinical cases and in helping therapists to design therapeutic plans specifically for each disorder. Presence of EMSs in a patient can affect therapeutic outcomes. As Young noted (10) this patients may be a 〜therapeutic failure〝 for classic treatment models. Therefore, it is strongly suggested that therapists design therapeutic plans according to EMSs.
References
- 1.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 2.Ekhtiari H, Jillson I. Prevalence of Opioid Abuse in Iran. Quarterly Journal of Addiction. 2008;10:123–126. [Google Scholar]
- 3.Kay J, Tasman A. Essentials of Psychiatry. New York: Wiley & Sons; 2006. [Google Scholar]
- 4.Sadock BJ, Kaplan HI, Sadock VA. Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical psychiatry. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 5.Mokri A. Brief Overview of the Status of Drug Abuse in Iran. Arch Iranian Med. 2002;5:184–190. [Google Scholar]
- 6.Ehsan-Manesh M, Karimi-Keisami I. [A review of the history and several studies regarding substance abuse in Iran] Q J Andisheh va Raftar. 1998;5:62–78. [Google Scholar]
- 7.Sayadi-anari AR, Khaleghi E, Esmaeili A, Nazer M. [Demographical characteristics of patient with opioid dependence] Q J Andisheh va Raftar. 2000;8:29–38. [Google Scholar]
- 8.Young JE. Cognitive Therapy for Personality Disorders: a schema-focused approach. Sarasota, FL: Professional Resource Press; 1994. [Google Scholar]
- 9.Beck AT, Freeman AM, Davis DD. Cognitive therapy of personality disorders. 2rd ed. New York: Guilford Press; 2004. [Google Scholar]
- 10.Young JE, Klosko JS, Weishaar ME. Schema therapy: a practitioner's guide. New York: Guilford Press; 2003. [Google Scholar]
- 11.Riso LP. Cognitive schemas and core beliefs in psychological problems: a scientist-practitioner guide. Washington, DC: American Psychological Association; 2007. [Google Scholar]
- 12.Magnavita JJ. Handbook of personality disorders: theory and practice. New York: Wiley & Sons; 2004. [Google Scholar]
- 13.Kaufman E. Family structures of narcotic addicts. Int J Addict. 1981;16:273–282. doi: 10.3109/10826088109038828. [DOI] [PubMed] [Google Scholar]
- 14.Ball SA, Legow NE. Attachment theory as a working model for the therapist transitioning from early to later recovery substance abuse treatment. Am J Drug Alcohol Abuse. 1996;22:533–547. doi: 10.3109/00952999609001679. [DOI] [PubMed] [Google Scholar]
- 15.First MB, Spitzer RL, Gibbon M, Williams JM. Tehran: Faradid; 2006. Structured clinical interview for DSM–IV Axis I disorders. Mohammad khani P, Jahani Tabesh A, Tamannaaei far Sh (Persian translators) [Google Scholar]
- 16.Schmidt NB, Joiner TE, Young JE, Telch MJ. The schema questionnaire: Investigation of psychometric properties Gild the hierarchic structure of a measure of maladaptive schemes. Cognit Ther Res. 1995;19:295–321. [Google Scholar]
- 17.Lee CW, Taylor G, Dunn J. Factor structure of the schema questionnaire in a large clinical sample. Cognit Ther Res. 1999;23:441–451. [Google Scholar]
- 18.Sheffield A, Waller G, Emanuelli F, Murray J. Is comorbidity in the eating disorders related to perceptions of parenting? Criterion validity of the revised Young Parenting Inventory. Eat Behav. 2006;7:37–45. doi: 10.1016/j.eatbeh.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 19.Ghiasi M. Iran, Isfahan: University of Isfahan; 2008. [Validity and reliability of Young Schema Questionary (3rd. Short-form) in patient with psychological disorder and non-patient individuals in Tehran] Thesis for Master degree. [Google Scholar]
- 20.Salavati M. Predominant Schemas and effectiveness of schema therapy in women patients with borderline personality disorder. Thesis for PhD of clinical psychology. Iran, Tehran: Tehran Psychiatric Institute; 2006. [Google Scholar]
- 21.Pinto-Goyveia J, Castilho P, Galhardo A, Cunha M. Early maladaptive schemas and social phobia. Cognitive therapy research. 2006;30:571–584. [Google Scholar]
- 22.Cooper M, Hunt J. Core beliefs and underlying assumptions in bulimia nervosa and depression. Behav Res Ther. 1998;36:895–898. doi: 10.1016/s0005-7967(98)00068-0. [DOI] [PubMed] [Google Scholar]
- 23.Decouvelaere F, Graziani P, Gackiere-Eraldi D, Rusinek S, Hautekeete M. [Hypothesis of existence and development of early maladaptive schemas in alcohol-dependent patients] Journal of Therapie Comportementale and Cognitive. 2002;12:43–48. [Google Scholar]
- 24.Brotchie J, Meyer C, Copello A, Kidney R, Waller G. Cognitive representations in alcohol and opiate abuse: the role of core beliefs. Br J Clin Psychol. 2004;43:337–342. doi: 10.1348/0144665031752916. [DOI] [PubMed] [Google Scholar]
- 25.Rees CD, Wilborn BL. Correlates of drug abuse in adolescent: a comparison of families of drug abusers with families of non-drug abusers. Journal of youth and adolescence. 1983;12:55–63. doi: 10.1007/BF02092114. [DOI] [PubMed] [Google Scholar]
- 26.Verheul R. Co-morbidity of personality disorders in individuals with substance use disorders. Eur Psychiatry. 2001;16:274–282. doi: 10.1016/s0924-9338(01)00578-8. [DOI] [PubMed] [Google Scholar]
- 27.Lotfi R, Donyavi V, Khosravi Z. Comparison Of Early Maladaptive Schemas Between Personality Disorder (cluster B) and Normal Subjects. Journal of ARMY University of medical sciences of the Islamic Republic of IRAN. 2007;5:1261–1266. [Google Scholar]
- 28.Sartorius N, Leff J. Families and Mental Disorders: From Burden to Empowerment. New York: Wiley & Sons; 2005. [Google Scholar]
- 29.Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clin Psychol Rev. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- 30.Harris E, Curtin L. Parental Perceptions, Early Maladaptive Schemas, and Depressive Symptoms in Young Adults. Cognitive Therapy and Research. 2002;26:405–416. [Google Scholar]
- 31.Coley RL, Votruba-Drzal E, Schindler HS. Trajectories of parenting processes and adolescent substance use: reciprocal effects. J Abnorm Child Psychol. 2008;36:613–625. doi: 10.1007/s10802-007-9205-5. [DOI] [PubMed] [Google Scholar]
- 32.Schenberg T. Children of substance users: The Relationship of perceived parental rejection to child emotional functioning, Unpublished doctoral dissertation. San Diego: California School of Professional Psychology; 1998. [Google Scholar]
- 33.Beck AT, Wright FD, Newman CF, Liese BS. Cognitive Therapy of Substance Abuse. New York: Guilford Press; 2001. [PubMed] [Google Scholar]