Abstract
The aim of the present study was to evaluate incidence, degree and impact of tibial tunnel widening (TW) on patient-reported long-term clinical outcome, knee joint stability and prevalence of osteoarthritis (OA) after isolated anterior cruciate ligament (ACL) reconstruction. On average, 13.5 years after ACL reconstruction via patella-bone-tendon-bone autograft, 73 patients have been re-evaluated. Inclusion criteria consisted of an isolated anterior cruciate ligament rupture and reconstruction, a minimum of 10-year follow-up and no previous anterior cruciate ligament repair or associated intra-articular lesions. Clinical evaluation was performed via the International Knee Documentation Committee (IKDC) score and the Tegner and Lysholm scores. Instrumental anterior laxity testing was carried out with the KT-1000™ arthrometer. The degree of degenerative changes and the prevalence of osteoarthritis were assessed with the Kellgren-Lawrence score. Tibial tunnel enlargement was radiographically evaluated on both antero-posterior and lateral views under establishment of 4 degrees of tibial tunnel widening by measuring the actual tunnel diameters in mm on the sclerotic margins of the inserted tunnels on 3 different points (T1–T3). Afterwards, a conversion of the absolute values in mm into a 4 staged ratio, based on the comparison to the results of the initial drill-width, should provide a better quantification and statistical analysis. Evaluation was performed postoperatively as well as on 2 year follow-up and 13 years after ACL reconstruction. Minimum follow-up was 10 years. 75% of patients were graded A or B according to IKDC score. The mean Lysholm score was 90.2±4.8 (25–100). Radiological assessment on long-term follow-up showed in 45% a grade I, in 24% a grade II, in 17% a grade III and in additional 12% a grade IV enlargement of the tibial tunnel. No evident progression of TW was found in comparison to the 2 year results. Radiological evaluation revealed degenerative changes in sense of a grade II OA in 54% of patients. Prevalence of a grade III or grade IV OA was found in 20%. Correlation analysis showed no significant relationship between the amount of tibial tunnel enlargement (P>0.05), long-term clinical results, anterior joint laxity or prevalence of osteoarthritis. Tunnel widening remains a radiological phenomenon which is most commonly observed within the short to midterm intervals after anterior cruciate ligament reconstruction and subsequently stabilises on mid and long- term follow-up. It does not adversely affect long-term clinical outcome and stability. Furthermore, tunnel widening doesn't constitute an increasing prevalence of osteoarthritis.
Key words: anterior cruciate ligament reconstruction, long-term follow-up, IKDC-score, tibial tunnel widening, osteoarthritis, long-term anterior laxity.
Introduction
Bone tunnel enlargement after anterior cruciate ligament reconstruction (ACL) represents a well documented phenomenon after anterior cruciat ligament surgery.1–5 In general, the exact aetiology of bone tunnel enlargement after ACL reconstruction is unknown. Mechanical and biological theories have been proposed to explain tunnel widening.6–8 Mechanical factors include motion of the graft within the tunnel, fixation methods/devices, stress shielding of the graft, improper graft placement, and accelerated rehabilitation.3,7,9–11 Biological factors represent graft swelling, use of allograft tissue, synovial fluid propagation within the tunnels, and increased cytokine levels.6,8,12,13 The process is most likely multi-factorial, arising both from mechanical and biological aetiologies. Furthermore there are many reasons for ACL reconstruction to fail, including adequate new trauma, graft rupture and graft insuffiency and tunnel lysis or enlargement.12,14,15 Tunnel enlargement in the revision setting represents a difficult technical challenge with possible compromise of graft placement, fixation, and graft incorporation.1,3,8,16 This may include the need for a staged reconstruction and additional operative procedure with significant costs. There have been several observations regarding the timing and progression of tunnel widening.3,4,16–18 The tunnel diameter increase seems to be significantly higher within the short term interval after surgery and afterwards stabilizes on midterm interval.2,4,5,18 Finally, some authors report of a decrease in tunnel diameter at 3 years after surgery.3,19 Although many authors have reported on the presence of tunnel enlargement, none has shown this to be clinical significance on short- and mid-term intervals with respect to laxity, increased failure rates or progression of degenerative changes.2–4 From current literature, tunnel widening does not appear to correlate with a poor clinical result, but on the other hand, there is only very few data beyond 3 years.2,4,17 One of the main reasons for anterior cruciate ligament reconstruction is to avoid progressive degenerative changes and secondary osteoarthritis.20–23 Therefore, purpose of the present study was to evaluate the incidence, degree and impact of tibial tunnel widening (TW) after isolated anterior cruciate ligament reconstruction with patella-bone-tendon-bone (PBTB) autgraft via a transtibial approach on long-term follow-up. The study group hypothesised that in terms of potential persisting micro-instability and consecutive potential incomplete graft incorporation tunnel widening continues and furthermore provides a significant impact on patient-reported long-term clinical outcome, long-term stability and prevalence of osteoarthritis.
Materials and Methods
Between January 1994 and December 1995 a total of 166 isolated ACL reconstructions were performed at our institution. Inclusion criteria for the present study consisted of an i) isolated primary arthroscopic ACL replacement (no concurrent meniscus or cartilage surgery; ii) no previous knee ligament surgery; iii) a normal contralateral knee. Exclusion criteria were additional ligamentous injuries, significant articular surface damage or meniscus lesions or evident osteoarthritic lesions (17 patients) or concomitant medial collateral ligament repair (13 patients) at the time of reconstruction as well as osteoarthritic changes (>grade I according to Kellgren-Lawrence). Operative treatment was performed within 2 –3 weeks from injury. During the entire follow up period, 11 patients (7%) suffered a graft rupture due to adequate new trauma. Graft failure occurred on average 38 (range 12–120) months after reconstruction. Secondary partial or total medial meniscectomy was performed in 24 patients and lateral meniscectomy was performed in 12 patients. During the follow-up period additional 14 patients (8%) suffered a contra-lateral ACL rupture and were excluded. At two year follow-up, the study group consisted of 126 patients. On long-term follow there were 78 patients, with 73 patients having a complete data record, which accounts for an overall follow-up rate of 44% at 13.5 (range 10–15.5) years after ACL reconstruction. Ádditional reasons for the high rate of loss on final follow-up additionally accounted for geographical limitations with an inability to attend for follow-up examinations and furthermore abovementioned intermittent operative procedures. The study group on long-term follow up therefore consisted of 46 male and 27 female patients. The median age was 43 years (range 24–63). In 53 cases the right knee and in 20 cases the left knee was affected. The study was approved by the local ethical committee.
Operative technique and rehabilitation
Operative technique was standardised in all patients: ACL reconstruction was performed via an autogenous BTB graft from the middle third of the patellar tendon. The central third of the patella (10 mm in width) was harvested through a single longitudinal incision. The graft was removed with a rectangular bone plug (20–25 mm in length). Afterwards an arthroscopic-assisted reconstruction was used. The ruptured ACL was debrided and the anatomical tibial and femoral footprints were identified and left intact. The exact tibial tunnel placement was performed using the drill-guide under arthroscopic view through the posterior part of the middle of the tibial ACL footprint. The exact angle of the tibial guide was determined by the sum of the intertendinous portion of the graft in mm (N) plus 7 according to the N+7 rule.24 The extra-articular portion of the guide was set midway between the apex and the posteromedial border the tibia. To create the femoral tunnel a 5-mm offset guide system was placed transtibially at the posterior margin of the intercondylar notch. Bone blocks were positioned in the tunnel and the autograft was placed with its cortical edge oriented posteriorly within the femoral tunnel. The position of the femoral tunnel was determined with the knee in 120° of flexion using the 5 mm offset instrument. Femoral graft fixation was performed by press-fit positioning in the inserted tunnels and by additional joint-distant mini-plate-fixation via a lateral incision. Exact intra-articular graft position of the tibial tunnel was performed with the knee in 90° of flexion, positioned in the footprint of its anatomical insertion. Afterwards tibial graft fixation was performed by press-fit fixation and additional joint distant staple fixation. After femoral fixation the affected knee was cycled several times to assess graft fixation and isometry and for the final tibial fixation staples were used to fix the threads outside the tunnel. Postoperatively all patients were immobilized in a full extension orthesis for two days. Our concept of rehabilitation allows a free range of motion of the knee. Isometric muscle exercises were then started without any limitations and full weight bearing was allowed according to the patients' pain level. During the entire rehabilitation period of 6 weeks we provided no additional external protection via use of a restricting orthesis. High-demand pivoting sports activities were allowed after six to nine months.
Assessments
Clinical follow-up evaluation was performed according to the International Knee Documentation Committee (IKDC) standard evaluation Form and the scores of Tegner and Lysholm.25–27 Clinical evaluation was performed at 2 years follow-up as well as on 10–15 year follow-up. Furthermore the pre-trauma status was documented. Assessment of the anterior laxity was carried out with the KT 1000™ arthrometer (Medmetric, San Diego, CA, USA) according to the IKDC graduation (degree of differential instrumental laxity in side comparison).28 According to the IKDC graduation, we defined differential anterior laxity as follows: IKDC grade A represents a differential anterior laxity <2 mm, IKDC grade B 3–5mm, IKDC grade C 6–10 mm, IKDC grade D >10 mm. Radiographic evaluation of the tibial tunnel was performed on antero-posterior (AP) and strict lateral (L) views under establishment of 4 degrees of tibial tunnel enlargement. Therefore based on conventional radiographs in 3 planes, the study group firstly calculated the actual tunnel diameters in mm measuring the sclerotic margins of the inserted tunnels on 3 different points (T1–T3) under assistance of a radiologist. The diameter of the tibial tunnel was measured 1 cm distal to the ACL insertion at proximal (T1), middle (T2), and distal (T3) location (Figure 1).
Figure 1.
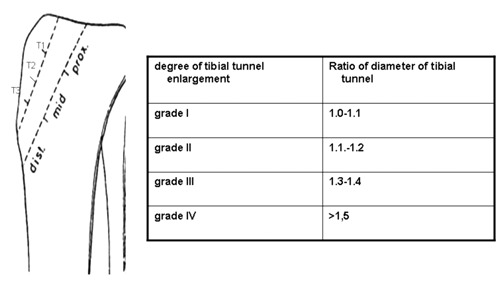
Calculation of the tibial tunnel enlargement.
In order to provide a better quantification and statistical analysis of the tunnel enlargement, the study group determined 4 degrees of tunnel widening by converting the absolute values in mm into a 4 staged ratio, based on the comparison between the results of the initial drill-width and direct postoperative x-ray with regard to the actual measured values. The maximum diameter on each location (T1–T3) was used to define the ratio as tunnels might be of different shapes. The establishment of a 4 staged ranking systems should also assure a minimization of radiographic errors to due projection the diameter of the tibial tunnel. Grade I TW was defined as a ratio of 1.0–1.1 of the diameter of the tibial tunnel between the T1–T3 locations. Grade II was defined as a ratio of 1.1–1.2, grade III as a ratio of 1.3–1.4 and grade IV should constitute for a ratio of >1.5. The tunnels were furthermore classified as cone, linear or cavitatory according to Peyrache et al.29 The degree of degenerative changes to evaluate the incidence of radiographic tibio-femoral and patello-femoral knee osteoarthritis was determined via application of the radiological scale of Kellgren and Lawrence.30 Radiographic evaluation of the pre-trauma status supplemented the overall radiographic assessment. Evidence of degenerative changes in sense of grade II osteoarthritis (OA) or more according to the Kellgren-Lawrence scale were used to define OA whereas grade III and grade IV degenerative changes should account for symptomatic OA.30
Statistical analyses
Statistical analysis was performed by using the software SPSS 17.0. version for windows.
Correlations were regarded as significant at P<0.05 concerning the Pearson-Chi square test and the Kruskal-Wallis test.
Results
International knee documentation committee evaluation
Clinical evaluation showed a deterioration of the clinical conditions during long-term course in comparison to the results on two year follow-up after ACL reconstruction (Table 1).
Table 1. Evaluation of clinical results according to the International Knee Documentation Committee (IKDC) score and evaluation of anterior laxity via the KT-1000 arthrometer according to the IKDC score.
| 2 years/midterm Follow up |
13.5 years/longterm Follow up |
||
|---|---|---|---|
| A. Evaluation | IKDC A | 64.3% (N=81) | 58.9% (N=43) |
| Clin. Results according to the IKDC score | IKDC B | 30.2% (N=38) | 31.5% (N=23) |
| IKDC C | 5.5% (N=7) | 8.2% (N=6) | |
| IKDC D | 0% (N=0) | 1.4% (N=1) | |
| B. Evaluation | IKDC A | 37.3% (N=47) | 23.3% (N=17) |
| Ant. Laxity according to the IKDC score | IKDC B | 47.6% (N=60) | 47.9% (N=35) |
| IKDC C | 14.3% (N=18) | 23.3% (N=17) | |
| IKDC D | 0.8% (N=1) | 5.5% (N=4) |
IKDC, International Knee Documentation Committee.
Two years after ACL reconstruction, functional assessment revealed 47 patients (37.3%) with an IKDC A grade, 60 patients (47.6%) with an IKDC B grade, additional 18 patients (14,3%) with a grade C scoring and only 1 patient (0.8%) was graded D according to the IKDC criteria. On long-term follow-up, 17 (23%) patients with an IKDC A grade, 35 (48%) patients with an IKDC B grade, 17 (23%) patients with an IKDC C grade and 4 (5.5%) patients with an IKDC D graduation could be detected. However, in total 75% of all patients could be graded A or B according to the IKDC score. Criteria for a deterioration of the clinical results on long-term follow-up consisted e.g. of pain and progressive swelling of the knee joint at strong load or symptoms of graft withdrawal within the subjective IKDC questionnaire. Furthermore an evident extensive deficit, intermittent intra-articular effusion formation or a striking differential laxity on assessment with the KT-1000 arthrometer™ accounted for worse results within the objective IKDC evaluation.
Lysholm score/Tegner activity score
Clinical assessment showed a deterioration of the average values within long-term course During the entire follow-up period there was also a decrease in the activity level. Practice of pivot and contact sports decreased from 77.8% to 45.2%. Furthermore, competitive involvement decreased from 65% to 18.5%. In contrast the rate of 76% of patients still participating in sports at final follow-up was excellent (55 of 73) (Table 2).
Table 2. Knee function and activity level according to the Lysholm scoring scale and the Tegener activity scale, respectively throughout the entire study period. The results are given as mean values and range.
| Before injury | 2 years | 13,5 years | |
|---|---|---|---|
| Knee function: lysholm scoring scale | 95.7 (65–100) | 92.4 (35–100) | 90.2 (25–100) |
| Activity level: tegener activity score | 5.8 (2–10) | 5.4 (2–10) | 4.9 (1–10) |
Assessment of anterior laxity (Lachman test)
Assessment of the anterior translation with the KT-1000 arthrometer™, according to the IKDC graduation, showed a slight deterioration on long-term follow-up in comparison to the results at two year follow-up. However, overall long-term knee joint stability remained satisfactory to excellent 13.5 years after anterior cruciate ligament reconstruction (Table 1).
Incidence of osteoarthritis
Radiographic assessment according to Kellgren and Lawrence revealed no signs of degenerative changes on pre-trauma assessment. On 2 year follow up as well as on long-term follow-up a marked increase of degenerative changes was detected (Figure 2).
Figure 2.
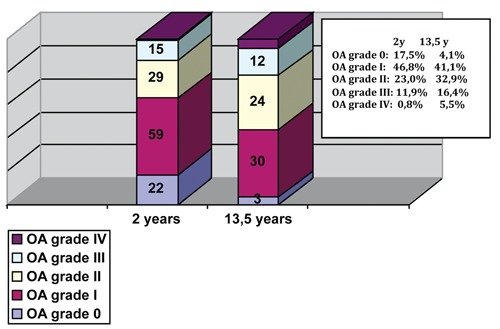
Prevalence of osteoarthritis according to the Kellgren Lawrence score.
Radiographic analysis of the tibial tunnel
The margins of the tunnels on the tibial side were well detected and easily identified on both antero-posterior and lateral views at 2 year and long-term follow-up. In contrast, directly postoperatively tunnel diameter, length and position could not be reliably determined. Therefore initial tunnel diameter was calculated from the width of the drill to create the tunnels during reconstruction. In order to minimize miscalculation of the tunnel size based on potential oblique and eccentric guide wire position, potentially leading to a larger tunnel diameter than the initial drill size, we standardised intra-operative tunnel placement and drill guide positioning and repeatedly controlled guide wire positioning via intra-operative x-ray imaging. On the femoral side the diameters tunnel were difficult to identify in particular on long-term follow-up due to total incorporation and therefore measurements were not made. Radiographic Assessment of the tibial tunnels and potential tunnel enlargement on 2 year follow-up showed in 46.8% a grade I, in 22.2% a grade II, in 16.7% a grade III and in additional 14.3% a grade IV enlargement of the tibial tunnel. No significant progression of TW was found in comparison to the 2 year results on long-term follow-up. 13.5 years after ACL-reconstruction in 45.2% a grade I, in 24.7% a grade II, in 17.8% a grade III and in additional 12.3% a grade IV enlargement of the tibial tunnel was detected (Figure 3).
Figure 3.
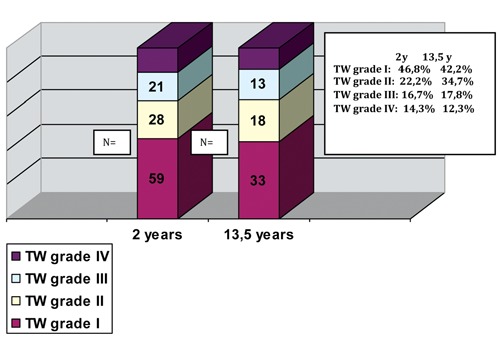
Prevalence of tibial tunnel widening.
Tunnel shape evaluation, according to Peyrache,29 predominantly revealed equal expansion of the tibial tunnels on two year follow-up as well on long-term follow-up. Linear expansion was detected in 85% and 86% upon radiological evaluation (Table 3).
Table 3. Evaluation of tunnel shapes at 2 years and 13.5 years.
| 2 years/midterm follow up | 13.5 years/long-term follow up | |
|---|---|---|
| Line | 84.9% (N=107) | 86.4% (N=63) |
| Cavitory | 10.3% (N=13) | 10.9% (N=8) |
| Cone | 4.8% (N=6) | 2.7% (N=2) |
Correlation analysis
On long-term follow-up, no significant correlation was found between the amount of tibial tunnel enlargement and clinical results according to the IKDC (P>0.05), Lysholm (P >0.05) or Tegner (P>0.05) scores. Furthermore, the study group found no significant correlations between the amount of tibial tunnel enlargement, increased anterior joint laxity (P>0.05) measured by a KT-1000 arthrometer™ or progression of degenerative changes according to Kellgren-Lawrence scale (P>0.05).
Discussion
Main purpose of the present retrospective clinical study was to evaluate the incidence, degree and impact of tibial TW after isolated anterior cruciate ligament reconstruction with PBTB autgraft via a transtibial approach on long-term follow-up. The study group hypothesised that in terms of potential persisting micro-instability and consecutive potential incomplete graft incorporation, tunnel widening continues and furthermore provides a significant impact on patient-reported long-term clinical outcome, long-term stability and prevalence of osteoarthritis.
Evaluation of the clinical and functional results according to the subjective and objective questionnaire of IKDC score on long-term follow-up, showed a decrease in comparison to the midterm results. The results were comparable to those found in literature.21,22,31 Several authors reported of high satisfaction rates and good to excellent clinical outcomes according to the IKDC (80–92 points on average) score based on a population of similar age and overall constitution.15,21,22,31 In the present study the mean subjective IKDC score was 78.4 points on long-term follow-up. However, 75 % of all patients could be evaluated an IKDC A or IKDC B graduation. Lysholm and Tegner scores showed a deterioration of the patents' clinical constitution in comparison to the results 2 years after anterior cruciate ligament reconstruction. The median Tegner score of 5 at final follow-up is similar in comparison to studies with more than 10 years follow-up which have reported of Tegner scores between 4 and 6.2,21,22,31 The mean Lysholm score of more than 90 points on long-term follow-up was similar to other studies with more than 10 years follow-up that have reported of scores between 82–94 points.15,21,22,31 Assessment of long-term anterior laxity via the KT-1000™ arthrometer showed a deterioration of the average values. On the other hand overall results through the entire period of follow-up remained excellent. 79% of all patients showed a differential laxity <3 mm on long-term evaluation. Overall performance concerning the anterior translation measured on KT 1000™ arthrometer is comparable with results found by Lebel et al.31 as well as Øiestad et al.22 at mid-term to long-term follow-up, with 70% to 90% of patients having a KT-1000™ arthrometer result of less than 3 mm. Radiographic evaluation of degenerative changes radiological revealed radiological changes in up to 80% of patients. The majority of these changes was graded I and II OA according to the Kellgren-Lawrence- classification. The rate of severe osteoarthritis (grade III and IV OA) was 22%, which is comparable to other published long-term studies after ACL reconstruction.21–23,31
Evaluation of potential persisting tibial tunnel enlargement in the present study showed no further bone tunnel lysis on long-term follow-up with regard to the 2 year results. According to literature enlargement of the tibial tunnels takes part mostly within the first 6 months after operation and is continued until 12 months after reconstruction.1,3,16 Afterwards most of authors report only on minimal changes up to 2 years after reconstruction.3,5,32 Radiographic evaluation of the tunnel size in the present study showed a constant tunnel size and no significant changes were detected. Radiographic assessment of the tibial tunnels and potential tunnel enlargement on long-term follow-up showed in 45% a grade I, in 24% a grade II, in 17% a grade III and in additional 12% a grade IV enlargement of the tibial tunnel enlargement of the tibial tunnel according to the elected 4 stage ranking system of the present study. With regard to the present literature, our results are comparable to those of studies by Asik et al.17 and Plaweski et al.4 Both studies analysed the clinical impact of tibial tunnel enlargement after a 4 year minimum follow-up. Both studies did not detect a significant progression of tibial tunnel widening on long-term follow up with regard to the short and midterm results. Furthermore Chen et al.2 evaluating bone tunnel enlargement as well clinical condition with a 7 year follow-up period after anterior cruciate ligament reconstruction with hamstring autograft report of constant to minimal progression of the analysed tibial tunnel enlargement on final follow-up. In addition, all study groups' report of comparable clinical results with regard to our results according the IKDC classification and the scores of Lysholm and Tegner.2,4,17
Tibial tunnel enlargement, in the present study analysis, occured within the first 2 years after reconstruction without any significant changes beyond with regard to long-term follow-up. Direct comparison regarding the percentage of detected TW with other studies remains controversial because of different surgical techniques and calculation methods of TW. Within the present study calculation was based on conventional radiographs in 3 planes. The study group firstly calculated the actual tunnel diameters in mm measuring the sclerotic margins of the inserted tunnels on 3 different points (T1–T3) under assistance of a radiologist (Figure 1). Afterwards, to provide a better quantification and statistical analysis of the tunnel enlargement, the study group determined 4 degrees of tunnel widening by converting the absolute values in mm into a 4 staged ratio based on the comparison to the results of the initial drill-width and direct postoperative x-ray with regard to the actual measured values. The maximum diameter on each location (T1–T3) was used to define the ratio as tunnels might be of different shapes. Basic idea of this concept was a categorization of the patients' values to minimize potential errors due to radiographic projection and to enable a facilitated statistical analysis with regard to potential clinical impact. With regard to actual literature other authors also tried to categorize the values of tibial tunnel enlargement in a modified design in comparison to our ratio to provide a more clinically orientated analysis.4 Other studies performed computed tomography (CT) or magnetic resonance imaging (MRI) to focus in particular on the tunnel shape as three-dimensional structure.18,33 However, the use of advanced imaging procedures demands patient radiation to take into account and furthermore entails a relatively high cost. Various investigators have described different types of tunnel enlargement, which include cavity type, cone type, and line type tunnels.9,19,29,34 In accordance to other studies, radiological evaluation of the tunnel shape showed in more than 85% tunnel enlargement of the linear type on mid-term follow-up as well as on long-term evaluation.2,4,17 Other study groups, in contrast, have reported relatively uniformly shaped tunnels.19,35 Furthermore, the present study could not detect any significant clinical effects of tibial tunnel enlargement with regard to anterior laxity measurement via the KT-1000 arthrometer. Assessment of long-term anterior laxity via the KT-1000™ arthrometer showed a deterioration of the average values. On the other hand overall results through the entire period of follow-up remained excellent. 79% of all patients showed a differential laxity <3 mm on long-term evaluation. These results are in agreement with other studies evaluating the impact of tibial tunnel widening on anterior knee laxity.2,4,17 Like other recent evaluations we could not detect a significant correlation between the degree of tibial tunnel enlargement and the incidence of increased anterior knee laxity.2,4 Furthermore, we found no significant correlation between the amount of tibial tunnel enlargement and clinical results according to the IKDC score and the scores of Lysholm or Tegner. Correlation analysis did not reveal a significant correlation of potential progression of degenerative changes according to Kellgren-Lawrence classification and the amount of tibial tunnel widening. These results support the results of Asik et al.17 and of Plaweski et al.4 Both authors evaluating long-term impact of tibial tunnel widening could not demonstrate a significant correlation between the amount of tunnel enlargement and the actual clinical condition according the the IKDC score, the activity level according to Tegner and Lysholm nor instrumental stability according to the KT-1000 measurements.
In the end mechanical and biological theories have been proposed for the explanation of tibial tunnel widening as a predominant radiological finding. According to actual literature there are different pathoetiologies to explain enlargement including variables like graft type, fixation technique or postoperative rehabilitation concepts.6–9,12 Mechanical factors include motion of the graft within the tunnel, fixation methods/devices, stress shielding of the graft, improper graft placement, and accelerated rehabilitation.7,11,19,34–36 The autologous BPTB graft complex as used for our patients provides a stiff construct along with rapid biologic bone-to-bone healing. Typically the tibial bone plug is fixed at a point distal to the joint line at a non-anatomic site, allowing increased graft motion within the proximal tibial tunnel. Moreover, this graft is of rectangular shape creating a dead space within the tibial tunnel proximal to the bone plug. This potential mismatch between the rectangular graft and the tunnel might constitute for persistent micro-motion in the sagittal plane (windshield wiper effect). With regard to actual literature ACL reconstruction by use of Hamstring autografts in comparison to BTB grafts in many previous studies in particular have exhibited higher rates of tunnel enlargement.3,5,9 Fixation of the hamstring tendons was performed by using a low stiffness construct, that is, fixation point distant from the joint line. This allows more graft elongation to occur with flexion and extension of the knee, and this has been referred to as the bungee effect in the literature.2,3,5,32 This longitudinal motion occurs particularly at the graft-tunnel interface. Subsequently, the femur has been the primary location of the tunnel widening secondary to its long tunnel length and subsequent pistoning of the graft within the tunnel. Additionally some authors argue that in particular suspensory fixation that is commonly used with hamstring graft reconstruction is responsible for this effect.1,5,9
Other studies have proved that besides mechanical factors in particular and biological factors are associated with tunnel enlargement.6,8,1,12,13 Complete graft to tunnel healing was stated by many different authors to be of cardinal assumption to prevent progressive tunnel enlargement.8,10,13,36 This process according to literature requires at least 10–12 weeks post reconstruction for the organization of the scar tissue and the development of Sharpey's fibers at the tendon-bone interface.8,10,36 With continuation of the graft maturation remodelling from fibrous tissue to mature bone occurs. The graft-to-tunnel fixation therefore seems to have an initial critical period prior to complete adherence. Factors affecting a potential lack of graft ingrowth include provocation of graft movement within the tunnel (weak fixation), too early movement of knee (aggressive rehabilitation or noncompliant patient).14–16,18 Regarding the BTB-graft as used for reconstruction in the present study, in general healing and incorporation of the bone block of the patellar tendon grafts is faster than hamstring grafts, and early stabilization is achieved, resulting in less micro-motion at the graft-tunnel interface. Apparently, the difference in biologic incorporation between the 2 grafts is the reason for complete obliteration of the femoral tunnel in 32% of patellar tendon graft patients reported previously.3,5,10 In accordance to these findings, we were not able to reliably determine the femoral tunnels on radiographic evaluation because of the complete tunnel obliteration. Some authors demonstrated the presence of synovial fluid between the graft and tunnel wall. Altered cytokine levels of e.g. interleukin 1, interleukin 6, interleukin 8, tumor necrosis factor alpha, and prostaglandin E2 contained in synovial fluid represent other biologic approaches for the explanation of tunnel enlargement. High levels of these cytokines may stimulate osteoclastic activity, leading to bone resorption.13 A persisting inflammatory process in chronic-ACL situations might be of significant contribution to bone osteolysis and subsequent tunnel widening.8,10,13,36 MRI based studies have shown synovial fluid tracking at the graft–bone tunnel interface.13
This study intended to evaluate incidence, long-term course and potential impact of detected tibial tunnel enlargement in particular focussing on long-term clinical outcome, knee joint stability and prevalence of knee osteoarthritis. On the other hand the current study set up provides certain limitations. The overall follow up rate was only 44%. Reason for the high rate of drop outs consisted mainly of the strict exclusion criteria after ACL reconstruction and intermittent operative treatment like partial menisectomy. Additional reasons for the high rate of loss on follow-up accounted for geographical limitations and the inability to attend for follow-up evaluation. Furthermore the present study is of retrospective design and principally focuses on a descriptive analysis, a control group is missing. In addition the presented trans-tibial ACL-reconstruction does account for today's standard operative technique, but on the other hand represented a popular and widely used operative method in the 90`s. Furthermore the measurement of the tibial tunnel using x-ray imaging does not represent the golden standard like CT-based measurements. CT based calculation of the tibial tunnel was not applicable due to the local ethic committee. Furthermore the initial tunnel diameter was calculated from the width of the drill to create the tunnels during reconstruction. In order to minimize miscalculation of the tunnel size based on potential oblique and eccentric guide wire position, potentially leading to a larger tunnel diameter than the initial drill size, we standardised intra-operative tunnel placement and drill guide positioning and repeatedly controlled guide wire positioning via intra-operative x-ray imaging. On the other hand the study was based on a homogenous study sample, a standardised operative procedure and postoperative rehabilitation as well as a short interval from injury to ACL reconstruction of only 2–3 weeks. In contrast to other studies we excluded patients with concomitant intra-articular injuries like significant articular surface damage, cartilage alterations therefore focussing only on isolated ACL injuries.
With regard to our results evaluating incidence, long-term course, impact of detected tibial tunnel enlargement on long-term clinical outcome, knee joint stability and prevalence of knee osteoarthritis we can point out that a successfully incorporated graft remains stable and tunnel widening does not continue over the period of time. Enlargement of the tibial tunnel remains a radiological phenomenon which is most commonly observed within the short- to mid-term intervals after anterior cruciate ligament reconstruction and subsequently stabilises on mid and long- term follow-up. It does not adversely affect long-term clinical outcome and knee joint stability. Furthermore TW does not constitute for an increasing prevalence of osteoarthritis on long-term follow-up. It remains of vital importance to identify and establish reconstruction techniques that optimize graft biology, fixation, placement, and rehabilitation. Future research should be directed at preventing this phenomenon and evaluating the relationship of tunnel enlargement with knee laxity and the outcome of revision ligament surgery.
Conclusions
Anterior cruciate ligament reconstruction with the PBTB-autograft resulted in high patient satisfaction levels and good clinical results on long-term evaluation Tibial tunnel enlargement within the present study analysis occured within the first 2 years after reconstruction with PBTB-autograft without any significant changes beyond with regard to long-term follow-up. Correlation analysis showed no significant relationship between tibial tunnel enlargement, long-term clinical results, increased anterior joint laxity or prevalence of osteoarthritis. Prevalence of symptomatic osteoarthritis developed in about 20%.
References
- 1.Baumfeld JA, Diduch DR, Rubino LJ, et al. Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc. 2008;16:1108–13. doi: 10.1007/s00167-008-0606-y. [DOI] [PubMed] [Google Scholar]
- 2.Chen CH, Chang CH, Su CI, et al. Arthroscopic single-bundle anterior cruciate ligament reconstruction with periosteum-enveloping hamstring tendon graft: clinical outcome at 2 to 7 years. Arthroscopy. 2010;26:907–17. doi: 10.1016/j.arthro.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005;21:1337–41. doi: 10.1016/j.arthro.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 4.Plaweski S, Rossi J, Merloz P. Anterior cruciate ligament reconstruction: assessment of the hamstring autograft femoral fixation using the EndoButton CL. Orthop Traumatol Surg Res. 2009;95:606–13. doi: 10.1016/j.otsr.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Webster KE, Feller JA, Hameister KA. Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomized comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2001;9:86–91. doi: 10.1007/s001670100191. [DOI] [PubMed] [Google Scholar]
- 6.Deehan DJ, Cawston TE. The biology of integration of the anterior cruciate ligament. J Bone Joint Surg Br. 2005;87:889–95. doi: 10.1302/0301-620X.87B7.16038. [DOI] [PubMed] [Google Scholar]
- 7.Jagodzinski M, Foerstemann T, Mall G, et al. Analysis of forces of ACL reconstructions at the tunnel entrance: Is tunnel enlargement a biomechanical problem? J Biomech. 2005;38:23–31. doi: 10.1016/j.jbiomech.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi M, Nakagawa Y, Suzuki T, et al. A retrospective review of bone tunnel enlargement after anterior cruciate ligament reconstruction with hamstring tendons fixed with a metal round cannulated interference screw in the femur. Arthroscopy. 2006;22:1093–9. doi: 10.1016/j.arthro.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Kousa P, Järvinen TLN, Vihavainen M, et al. The fixation strength of six hamstring graft fixation devices in anterior cruciate ligament reconstruction. Part II: Tibial site. Am J Sports Med. 2003;31:182–8. doi: 10.1177/03635465030310020501. [DOI] [PubMed] [Google Scholar]
- 10.Wen CY, Qin L, Lee KM, et al. Grafted tendon healing in tibial tunnel is inferior to healing in femoral tunnel after anterior cruciate ligament reconstruction: a histomorphometric study in rabbits. Arthroscopy. 2010;26:58–66. doi: 10.1016/j.arthro.2009.06.025. [DOI] [PubMed] [Google Scholar]
- 11.Zantop T, Weimann A, Rummler M, et al. Initial fixation strength of two bioabsorbable pins for the fixation of hamstring grafts compared to interference screw fixation: single cycle and cyclic loading. Am J Sports Med. 2004;32:641–9. doi: 10.1177/0095399703258616. [DOI] [PubMed] [Google Scholar]
- 12.Menetrey J, Duthon VB, Laumonier T, Fritschy D. Biological failure of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc. 2008;16:224–31. doi: 10.1007/s00167-007-0474-x. [DOI] [PubMed] [Google Scholar]
- 13.Zysk SP, Fraunberger P, Veihelmann A, et al. Tunnel enlargement and changes in synovial fluid cytokine profile following anterior cruciate ligament reconstruction with patellar tendon and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2004;12:98–103. doi: 10.1007/s00167-003-0426-z. [DOI] [PubMed] [Google Scholar]
- 14.Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–57. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 15.Steiner ME, Murray MM, Rodeo SA. Strategies to improve anterior cruciate ligament healing and graft placement. Am J Sports Med. 2008;36:176–89. doi: 10.1177/0363546507311690. [DOI] [PubMed] [Google Scholar]
- 16.Jarvela T, Moisala AS, Paakkala T, Paakkala A. Tunnel enlargement after double-bundle anterior cruciate ligament reconstruction: a prospective, randomized study. Arthroscopy. 2008;24:1349–57. doi: 10.1016/j.arthro.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 17.Asik M, Sen C, Tuncay I, et al. The mid- to long-term results of the anterior cruciate ligament reconstruction with hamstring tendons using Transfix technique. Knee Surg Sports Traumatol Arthrosc. 2007;15:965–72. doi: 10.1007/s00167-007-0344-6. [DOI] [PubMed] [Google Scholar]
- 18.Moisala AS, Jarvela T, Paakkala A, et al. Comparison of the bioabsorbable and metal screw fixation after ACL reconstruction with a hamstring autograft in MRI and clinical outcome: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2008;16:1080–6. doi: 10.1007/s00167-008-0593-z. [DOI] [PubMed] [Google Scholar]
- 19.Choi NH, Lee JH, Son KM, Victoroff BN. Tibial tunnel widening after anterior cruciate ligament reconstructions with hamstring tendons using Rigidfix femoral fixation and Intrafix tibial fixation. Knee Surg Sports Traumatol Arthrosc. 20101;18:92–7. doi: 10.1007/s00167-009-0951-5. [DOI] [PubMed] [Google Scholar]
- 20.Keays SL, Newcombe PA, Bullock-Saxton JE, et al. Factors involved in the development of osteoarthritis following anterior cruciate ligament surgery. Am J Sports Med. 2010;38:455–63. doi: 10.1177/0363546509350914. [DOI] [PubMed] [Google Scholar]
- 21.Mihelic R, Jurdana H, Jotanovic Z, et al. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop. 2011;35:1093–7. doi: 10.1007/s00264-011-1206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–43. doi: 10.1177/0363546509338827. [DOI] [PubMed] [Google Scholar]
- 23.Streich NA, Zimmermann D, Bode G, Schmitt H. Reconstructive versus non-reconstructive treatment of anterior cruciate ligament insufficiency. A retrospective matched-pair long-term follow-up. Int Orthop. 2011;35:607–13. doi: 10.1007/s00264-010-1174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller MD, Hinkin DT. The N + 7 rule for tibial tunnel placement in endoscopic anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:124–6. doi: 10.1016/s0749-8063(96)90234-0. [DOI] [PubMed] [Google Scholar]
- 25.Anderson AF, Irrgang JJ, Kocher MS, et al. International Knee Documentation Committee. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34:128–35. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 26.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–4. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 27.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–9. [PubMed] [Google Scholar]
- 28.Tyler TF, McHugh MP, Glim GW, et al. Association of KT-1000 measurements with clinical tests of knee stability 1 year following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:540–5. doi: 10.2519/jospt.1999.29.9.540. [DOI] [PubMed] [Google Scholar]
- 29.Peyrache MD, Djian P, Christel P, Witvoet J. Tibial tunnel enlargement after anterior cruciate ligament reconstruction by autogenous bone-patellar tendon-bone graft. Knee Surg Sports Traumatol Arthrosc. 1996;4:2–8. doi: 10.1007/BF01565989. [DOI] [PubMed] [Google Scholar]
- 30.Kellgren JH, Lawrence JS, Bier F. Genetic factors in generalized Osteoarthritis. Ann Rheum Dis. 1963;22:237–55. doi: 10.1136/ard.22.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lebel B, Hulet C, Galaud B, et al. Arthroscopic reconstruction of the anterior cruciate ligament using bonepatellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36:1275–82. doi: 10.1177/0363546508314721. [DOI] [PubMed] [Google Scholar]
- 32.Kobayashi M, Nakagawa Y, Suzuki T, et al. A retrospective review of bone tunnel enlargement after anterior cruciate ligament reconstruction with hamstring tendons fixed with a metal round cannulated interference screw in the femur. Arthroscopy. 2006;22:1093–9. doi: 10.1016/j.arthro.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 33.Marchant MH, Jr, Willimon SC, Vinson E, et al. Comparison of plain radiography, computed tomography, and magnetic resonance imaging in the evaluation of bone tunnel widening after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1059–64. doi: 10.1007/s00167-009-0952-4. [DOI] [PubMed] [Google Scholar]
- 34.Ahn JH, Park JS, Lee YS, Cho YJ. Femoral bioabsorbable cross-pin fixation in anterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1093–9. doi: 10.1016/j.arthro.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 35.Ma CB, Francis K, Towers J, et al. Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy. 2004;20:122–8. doi: 10.1016/j.arthro.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 36.Rodeo SA, Kawamura S, Kim HJ, et al. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: An effect of graft-tunnel motion? Am J Sports Med. 2006;34:1790–800. doi: 10.1177/0363546506290059. [DOI] [PubMed] [Google Scholar]


