Abstract
The treatment of painful osteoporotic vertebral compression fractures using transpedicular cement augmentation has grown significantly over the last two decades. The benefits of balloon kyphoplasty compared to conservative treatment remain controversial and are discussed in the literature. The complication rates of vertebroplasty and kyphoplasty are considered to be low. The focus of this study was the analysis of acute and clinically relevant complications related to this procedure. In our department, all patients treated between February 2002 and February 2011 with percutaneous cement augmentation (372 patients, 522 augmented vertebral bodies) were prospectively recorded. Demographic data, comorbidities, fracture types, intraoperative data and all complications were documented. The pre- and postoperative pain-level and neurological status (Frankel-Score) were evaluated. All patients underwent a standardized surgical procedure. Two hundred and ninety-seven patients were treated solely by balloon kyphoplasty; 216 females (72.7%) and 81 males (27.3%). Average patient age was 76.21 years (±10.71, range 35–98 years). Average American Society Anestesiologists score was 3.02. According to the Orthopedic Trauma Association classification, there were 69 A 1.1 fractures, 177 A 1.2 fractures, 178 A 3.1.1 fractures and 3 A 3.1.3 fractures. Complications were divided into preoperative, intraoperative and postoperative events. There were 4 preoperative complications: 3 patients experienced persistent pain after the procedure. In one case, the pedicles could not be visualized during the procedure and the surgery was terminated. One hundred and twenty-nine (40.06%) of the patients showed intraoperative cement leaking outside the vertebras, one severe hypotension and tachycardia as reaction to the inflation of the balloons, and there was one cardiac arrest during surgery. Postoperative subcutaneous hematomas were observed in 3 cases, 13 patients developed a urinary tract infection, and 2 patients died during hospitalization. Twenty-four patients (8.1%) returned because of new pain events and 23 patients reported a new painful fracture. Balloon kyphoplasty is a save and effective procedure to treat patients with painful vertebral compression fractures. Rapid patient mobilization after kyphoplasty, as well as a prompt reintegration into the social environment, are possible. Compared to other surgical procedures, especially in patients with an average age of 75 years, balloon kyphoplasty seems to offer some advantages. However, the procedure still has a potential for serious complications and should be performed by well trained personnel.
Key words: balloon kyphoplasty, outcome, complications, vertebral compression fractures.
Introduction
Vertebroplasty and kyphoplasty, the percutaneous injection of various bone cements into affected vertebral bodies, have been used in painful osteoporotic vertebral fractures. The technique of percutaneous injection was first described by Galibert et al.1 Following the introduction of the balloon kyphoplasty,2 in which a void in the vertebral body is created using an inflatable balloon prior to cement augmentation, treatment numbers of both procedures have been rising significantly.
According to the criteria of evidence-based medicine, there is only one level Ib evidence study,3 that shows the benefits of balloon kyphoplasty compared to conservative treatment, especially in the early course after osteoporotic fractures. It was possible to observe efficacy with regard to a significant reduction in pain in 87% of the patients undergoing vertebroplasty and in 92% of the patients undergoing kyphoplasty.4 Overall, the complication rate of both procedures is considered to be low.4–6
After successful treatment of osteoporotic fractures, the indication for kyphoplasty was extended to painful hemangiomas and metastatic lesions of the vertebral bodies. Balloon kyphoplasty offers the potential to restore the height of the vertebral body. It is obvious that this depends on the type (e.g. compression, burst or collapse) and age (fresh, vertebral cleft) of the fracture, as well as the positioning of the patient during surgery.
In the trauma setting, patients can be subdivided into three groups. The first group consists of young patients with a high impact injury. Even though some authors suggest treating these patients with balloon kyphoplas-ty it is far from a standard procedure.7 The second group consists of elderly, mostly osteoporotic, patients with reduced strength of the vertebral bodies and minor or no trauma. Many of these patients report a history of no trauma or can not remember when pain began. These patients are often able to walk and, according to the guidelines, initial conservative treatment is recommended. The third group consists of patients with traumatic fractures (e.g. burst fractures) and accompanying osteoporosis. Most of these patients are hospitalized and bedridden on account of immobilizing pain. These patients are a challenge for the spine surgeon. Balloon kyphoplasty offers an alternative to conservative treatment and to conventional stabilizing spine surgery. Both conservative and surgical treatment are at risk of serious complications. Another problem is the classification of vertebral fractures and the question as to which fracture types should be treated by balloon kyphoplasty. There is no uniform classification of vertebral injuries that adresses acute traumatic fractures in the same way as chronic osteoporotic vertebral fractures. No valid classification considers the different pathology or the character of a fresh or a chronic vertebral fracture. For this reason, standard fracture types that could be considered as indications for ballon kyphoplasty or vertebroplasty can not be created.
The clinical benefits and advantages of vertebral augmentation procedures must be weighed against the complications that can occur. We, therefore, decided to critically analyze all procedures that were performed at our institution regarding safety and complications.
Materials and Methods
All patients treated with percutaneous cement augmentation of vertebral bodies between February 2002 and February 2011 were prospectively analyzed. A total of 372 patients were evaluated with a total of 544 augmented vertebral bodies. The average age of our patients was 76.21 (±10.71, range 35–98) years. Demographic data such as age, gender and duration of symptoms were documented (Table 1). Comorbidities of the patients were evaluated and scored corresponding to the American Society of Anesthesiologists (ASA) score. All vertebral fractures were classified according to the Orthopedic Trauma Association (AO/OTA) classification of traumatic vertebral injuries.8 Besides the documentation of intraoperative data, such as duration of surgery and cement volume used, the focus of the present study was to identify all complications that were associated with balloon kyphoplasty. All patients treated by percutaneous vertebroplasty or patients who had combinations of dorsal instrumentation and balloon kyphoplasty were excluded from this study. The complications were divided into preoperative (e.g. wrong indication), intraoperative (e.g. cement leakage, injury during access) and postoperative (e.g. urinary tract infection, hematoma, revision) complications.
Table 1. Demographics of the patient population.
| Demographics | |
|---|---|
| Age | 76.21 years (±10.71, range 35–98 years) |
| N. patients | 297 |
| Ratio males vs females | 81 : 216 |
| Mean ASA score | 3.02 |
| Inpatient stay | 10.42 days (±5.9, median 9, range 2–42) |
| Duration of surgery | 44.5 minutes (±18.3, median 37, range 12–112) |
| Fluoroscopy | 184 seconds (±111.1, median 138, range 6–870) |
| Cement volume | 7.7 ml (±2.9, median 7.6, range 1–18) |
| VAS preoperative | 8.1 (±0.87, median 8, range (6 –10) |
| VAS postoperative | 1.71 (±1.1, median 2, range 0 –8) |
ASA, American Society of Anesthesiologists; VAS, visual analogue score.
All patients received conventional X-rays on two planes before and after balloon kyphoplasty. In cases of suspected involvement of the posterior wall of the vertebral body, computed tomography was also performed. In all cases, magnetic resonance imaging (MRI) was performed to identify the level of injury, age of the fracture and to identify additional bone bruises in other spine segments. If due to technical reasons (e.g. cardiac pacemaker) an MRI could not be carried out, a scintigraphy was conducted to differentiate between acute and older fractures.
Pain and neurological status were recorded before and after surgery, and on the day of discharge from the hospital. The visual analog scale (VAS) score was used to measure patient pain. This visual scale ranging from 0 (no pain) to 10 (maximum pain). The Frankel score was used to confirm neurological status.9
All data were expressed as percentages, mean, median and standard deviations.
Surgical technique
All kyphoplasty procedures were performed under general anesthesia with the patients positioned prone. In all cases, a bipedicular approach under fluoroscopic control using one image intensifier that was rotated through 90° was used. Balloon-kyphoplasty was performed according the manufacturer's indications (Kyphon, Medtronic).
The objective was to place the balloons close to the injured superior endplate and/or the base plate in the anterior two-thirds of the vertebra in order to achieve a good repositioning of the endplate and to stabilize the anterior part of the vertebra. We tried to almost completely fill the anterior two-thirds of the vertebra with cement in order to achieve a good mechanical stability of the vertebra, which is in compliance with the 3-column theory of Louis.10
High balloon volumes were necessary to fill out the vertebras. In order to avoid a peripheral cement extravasation, it is essential to wait until the cement has become highly viscous.
Results
Between February 2002 and February 2011, 372 patients were treated with cement augmentation procedures of the spine. All together there were 544 augmented vertebral bodies. Fifty-nine patients were treated by percutaneous vertebroplasty. In 18 patients balloon kyphoplasty was combined with dorsal instrumentation. In 5 patients, besides balloon kyphoplasty, augmentation procedures were also performed (shield kyphoplasty, vertebral body stenting and RF-kyphoplasty). All these patients were excluded from the study analysis.
Two hundred and ninety-seven patients (216 females, 72.7%; 81 males, 27.3%) were treated only by balloon kyphoplasty. Average age of the patients was 76.21 (±10.71, range 35–98) years.
A significant amount of comorbidities were reported resulting in an average ASA score of 3.02 (ASA II, n= 46, 15.5%; ASA III, n=200, 67.3%; ASA IV, n=51, 17.2%). In 206 patients, the fractures were caused by falls from a low height, 12 patients had sustained traffic accidents, 2 patients suffered from epileptic seizures, and in 102 patients the pain developed spontaneously and no type of trauma was remembered. In 25 patients, the fracture was due to spine metastasis. Patient demographics are shown in Table 1.
According to the AO/OTA classification, there were 69 A 1.1 (endplate impression), 177 A 1.2 (wedge compression), 178 A 3.1.1 (incomplete cranial burst) and 3 A 3.1.3 (incomplete caudal burst) fractures. Twelve vertebral bodies were treated prophylactically.
Two hundred and seventy-three patients underwent a single operation, 23 patients were operated twice and one patient had to undergo surgery three times. A total of 439 vertebral bodies was augmented: one level, n=231 (71.7%); two levels, n=72 (22.4%); three levels, n=17 (5.3%); four levels, n=2 (0.62%); five levels, n=1 (0.31%). The time from trauma or onset of symptoms respectively to surgery ranged from 2 to 140 days (mean 18.6, ±19.9, median 13 days).
Seventy percent of the fractures were located in the area of the thoracolumbar junction (Figure 1).
Figure 1.
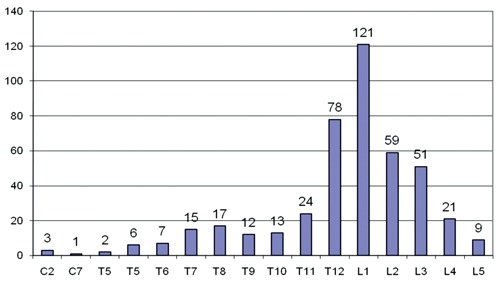
Height localisation of the affected vertebras.
Surgery lasted an average 44.5 (±18.3, median 37, range 12–112) minutes and fluo-roscopy an average 184 (±111.1, median 138, range 6–870) seconds. An average 7.7 mL of cement (±2.9, median 7.6, range 1–18) were injected into each vertebral body. The average VAS value decreased from 8.1 (±0.87, median 8, range 6–10) prior to surgery to 1.71 (±1.1, median 2, range 0–8) on the day of discharge. This was statistically significant (P< 0.05).
Inpatient treatment lasted an average 10.42 (±5.9, median 9, range 2–42) days. Eighty-eight patients (27.33%) were transferred for inpatient rehabilitation (Table 1).
Complications
Complications were divided into preoperative, intraoperative and postoperative events (Table 2).
Table 2. Complications.
| Complication | Preoperative, n. | Intraoperative, n. | Postoperative, n. |
|---|---|---|---|
| Pain persistance at the same level | 3 | ||
| No visualisation of pedicles possible | 1 | ||
| Cement leakage | 129 (40.06%) | ||
| Allergic reaction | 1 | ||
| Cardiac arrest | 1 | ||
| Subcutaneous hematoma | 3 | ||
| Urinary tract infection | 13 | ||
| Death | 2 | ||
| Presentatin of new pain | 24 | ||
| Presentation of new fractures | 23 (1 adjacent fracture) |
Preoperative complications
In 3 patients, the pain persisted at the same level after balloon kyphoplasty. All these patients had a bone bruise proven on preoperative MRI and other pathologies such as spinal canal stenosis were excluded. These 3 patients were considered non-responders to balloon kyphoplasty.
In another patient, the pedicles could not be visualized during the procedure and surgery was terminated. Careful preoperative examination of X-rays might have prevented this intraoperative problem.
Intraoperative complications
In 129 (40.06%) of the patients, there was cement leaking outside the vertebras: intervertebral disc spaces n=41, basivertebral plexus n=31, paravertebral n=101, pedicle, n=12 renal vein n=1, cement embolisation into the lungs n=2 (Figure 2).
Figure 2.
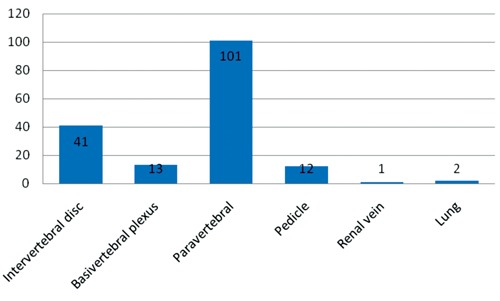
Localisation of the cement extravasations.
Fortunately, all cases of extravasation were clinically unremarkable. One young patient who suffered from secondary osteoporosis based on systemic mastocytosis reacted to the inflation of the balloons with severe hypotension and tachycardia.11 All symptoms of this patient resolved after resuscitation. One patient had cardiac arrest after the procedure was finished and the patient was moved in a supine position. Despite CPR, the patient died. An autopsy was not performed. There were no obvious intraoperative complications during surgery. No extravasation was observed on fluoroscopy.
Postoperative complications
Postoperatively it became necessary to release a subcutaneous hematoma in 3 cases. During their hospital stay, 13 patients were diagnosed with an urinary tract infection. Two patients died during their hospital stay. One female patient's death was caused by a mitral valve endocarditis; another female patient's death was caused by a cardiac insufficiency New York Heart Association Class 4 and a severe obstructive pulmonary disease.
Twenty-four patients (8.1%) returned because of newly occurring pain. Twenty-three patients started suffering from a new painful fracture that was successfully treated by kyphoplasty. One patient returned twice and was treated by balloon kyphoplasty for a total of three times. Most of the fractures occurred within the first three months after surgery. Only one fracture was adjacent to the initially treated vertebral body that underwent surgery. The other symptomatic fractures were satellite fractures and at least two segments away from the vertebras that were initially treated.
Discussion
Kyphoplasty has been successfully used in the treatment of painful osteoporotic compression fractures of vertebral bodies for several years. There is only one level I study in the literature. This study shows the benefits of this procedure compared to conservative treatment.3 In several systematic reviews it was possible to observe its efficacy with regard to a significant reduction in pain in 87% of the patients undergoing vertebroplasty and in 92% of the patients undergoing kyphoplasty.4 Overall, the complication rate of both procedures is considered to be low.4–6 The main complication is the leakage of cement that occurred in 41% of the vertebroplasties and in up to 30% of the kyphoplasties.4,12
Fractures of vertebral bodies were classified according to the AO classification.8 This classification was developed more to address acute traumatic fractures than osteoporotic or pathological fractures of the vertebral bodies. The AO classification does, however, provide a good description of fracture morphology. In patients with osteoporotic changed vertebras, fractures can be caused by considerably less force than in young patients.
Osteoporotic pathological fractures
The classification established by the AO/OTA mainly targets, like almost all trauma-related fracture classifications, the classification of fresh traumatic injuries. The classification of osteoporotic fractures, which generally occur spontaneously, are unrelated to a relevant trauma event or which cannot be remembered, is more difficult.
A semi-quantitative and morphological classification of osteoporotic compression fractures has been suggested by Genant et al.13 According to their morphological deformity, fractures are grouped into mild (20–25%), moderate (25–40%) and severe (<40%). Genant et al. differentiate between three main groups of fractures: wedge, biconcave and crush deformity. The disadvantage of this classification is that fractures of vertebral bodies with involvement of the posterior wall can not be categorized.
In this study, osteoporotic fractures were categorized according to the AO/OTA classification being aware that the classification has shortcomings in osteoporotic compression fractures.
A low evidence level of studies that can be used for the determination of treatment strategies of thoracolumbar fractures has been documented by current systematic reviews.14–15 For this reason, treatment of thoracolumbar fractures remains controversial. There is also no agreement on what type of surgical stabilization should follow.
In the older patient population, the treatment objective is different to that in young patients. The restoration of a physiological axial skeleton is less important, in cases of limited activity level and limited life expectancy, than rapid mobilization that is low in risk as well as in pain. Another aim is a prompt reintegration in the patient's social environment. A conservative treatment is also recommended in cases of strong defective positions in old as well in very old patients to avoid the patient being exposed to surgical complications. Furthermore, the surgical treatment possibilities are also limited due to a decrease in bone quality. In some cases, an extensive exposure of the spine is necessary for dorsal stabilisation. In some patients, additional cement augmentation of the transpedicular screws is thought to improve stability. Due to the general risks of patients with an average age of 76.21 (±10.71, range 35–98) years and with an average ASA score of 3.02, a higher complication rate than that described by Knop et al.16 can be anticipated.
Postoperatively, pain intensity, measured on the visual analog scale, which prior to surgery amounted to an average of 8.1 (±0.87, median 8, range 6–10), was reduced to an average of 1.71 (±1.1, median 2, range 0–8) immediately after surgery. This difference is statistically significant (P<0.05). No senso-motoric deficits or radicular neurological symptoms were observed.
Compared to the complications in dorsal or ventral procedures described by Knop et al.16 the postoperative rate of complications that had to be revised in our collective was quite low: 3 hematomas needed decompression.
The main complication that occured was the high rate of cement extravasation (40,06%). The average rate of cement extravasation is quoted as being approximately 9%,4 whereas some authors who underwent kyphoplasty experienced percentages of up to 33%.17–20 Our cementing technique could be a reason for such a high rate of cement leakage. Our belief was that, besides reducing pain, the objective of kyphoplasty is to achieve mechanical stability of the anterior two-thirds of the vertebra. Louis defines an anterior column corresponding to the vertebral body and two posterior columns corresponding to the facet joints which together carry the load.10 In comparison, in the 2-column model of the AO, the posterior column also has a load-carrying function.
It is necessary to fill the vertebral bodies almost completely with cement in order to achieve mechanical stability in the area of the anterior column. During and after cement filling the posterior wall of the vertebral bodies has to be extremely well protected to avoid dorsal cement extravasation. As long as the cement does not leak dorsally, the cement can be carefully injected. In case of lateral cement extravasation or cement leaking into the intervertebral space, cementing should be stopped. In agreement with the data in the literature,21 all cement extravasations we observed were clinically irrelevant. The use of the eggshell technique might have reduced the leakage rate. This procedure was described by Greene et al.22 and includes another balloon placement once the cement has been inserted in order to better distribute the cement and maintain a viscous consistency.
Some studies have discussed an increased risk of adjacent fractures after a kyphoplasty.3,23,24 The present study involved no standardized radiological follow up since an additional exposure to radiation in cases of clinically unremarkable patients was not indicated and was not approved by the ethics comittee. All together, there were 24 patients (8.1%) with new painful vertebral fractures. Lindsay et al. describe a relative risk of 19.2% of suffering another fracture in the first year after the initial vertebral fracture.3 Two-thirds of the new fractures remain clinically unremarkable.
Possible limitations of this present study are that there was no clinical or radiological follow up. Defective positions, loss of reposition and subsequent asymptomatic fractures were not evaluated in this study since they play a minor role in the elderly patients we treated.
Conclusions
Balloon kyphoplasty is a save and effective procedure to treat patients with painful vertebral compression fractures. In cases of limited activity levels and limited life expectancy, the restoration of the physiological axial skeleton is less important than rapid mobilization. Another objective is a prompt reintegration into the patient's social environment. Compared to other surgical procedures, especially in patients with an average age of 75 years, balloon kyphoplasty seems to offer some advantages. The procedure still has the potential for serious complications and should be performed by well trained personnel.
We were not able to observe neurological complications in our patients. Main complications included asymptomatic cement leakages that was caused by the cementation technique and not by the procedure itself.
References
- 1.Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty] Neurochirurgie. 1987;33:166–8. [Article in German] [PubMed] [Google Scholar]
- 2.Wong W, Reiley MA, Garfin S. Vertebroplasty/Kyphoplasty. Journal of Woman's Imaging. 2000:117–24. [Google Scholar]
- 3.Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016–24. doi: 10.1016/S0140-6736(09)60010-6. [DOI] [PubMed] [Google Scholar]
- 4.Hulme PA, Krebs J, Ferguson SJ, Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976.) 2006;31:1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 5.Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J. 2007;16:1085–100. doi: 10.1007/s00586-007-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine (Phila Pa 1976.) 2006;31:2747–55. doi: 10.1097/01.brs.0000244639.71656.7d. [DOI] [PubMed] [Google Scholar]
- 7.Maestretti G, Cremer C, Otten P, Jakob RP. Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J. 2007;16:601–10. doi: 10.1007/s00586-006-0258-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 9.Waring WP, III, Biering-Sorensen F, Burns S, et al. 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010;33:346–52. doi: 10.1080/10790268.2010.11689712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Louis R. Berlin Heidelberg. New York: Springer; 1985. Die stabilisierende Funktion der Wirbelsäule. Die Chirurgie der Wirbelsäule; pp. 57–57. [Google Scholar]
- 11.Kruger A, Hamann C, Brendel C, et al. Multimodal therapy for vertebral involvement of systemic mastocytosis. Spine (Phila Pa 1976.) 2009;34:E626–8. doi: 10.1097/BRS.0b013e3181a6bc4f. [DOI] [PubMed] [Google Scholar]
- 12.Krueger A, Bliemel C, Zettl R, Ruchholtz S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009;18:1257–65. doi: 10.1007/s00586-009-1073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Genant HK, Jergas M, Palermo L, et al. Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The study of Osteoporotic Fractures Research Group. J Bone Min Res. 1996;11:984–96. doi: 10.1002/jbmr.5650110716. [DOI] [PubMed] [Google Scholar]
- 14.Thomas KC, Bailey CS, Dvorak MF, et al. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4:351–8. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 15.van der RN, de Lange ES, Bakker FC, et al. Management of traumatic thoracolumbar fractures: a systematic review of the literature. Eur Spine J. 2005;14:527–34. doi: 10.1007/s00586-004-0847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knop C, Bastian L, Lange U, et al. Complications in surgical treatment of thoracolumbar injuries. Eur Spine J. 2002;11:214–26. doi: 10.1007/s00586-001-0382-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J. 2004;13:496–501. doi: 10.1007/s00586-004-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kruger A, Zettl R, Ziring E, et al. Kyphoplasty for the treatment of incomplete osteoporotic burst fractures. Eur Spine J. 2010;19:893–900. doi: 10.1007/s00586-010-1281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lane JM, Hong R, Koob J, et al. Kyphoplasty enhances function and structural alignment in multiple myeloma. Clin Orthop Relat Res. 2004:49–53. doi: 10.1097/01.blo.0000131642.96984.74. [DOI] [PubMed] [Google Scholar]
- 20.Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine (Phila Pa 1976.) 2005;30:2806–12. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]
- 21.Lavelle W, Carl A, Lavelle ED, Khaleel MA. Vertebroplasty and kyphoplasty. Med Clin North Am. 2007;91:299–314. doi: 10.1016/j.mcna.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Greene DL, Isaac R, Neuwirth M, Bitan FD. The eggshell technique for prevention of cement leakage during kyphoplasty. J Spinal Disord Tech. 2007;20:229–32. doi: 10.1097/01.bsd.0000211276.76024.30. [DOI] [PubMed] [Google Scholar]
- 23.Becker S, Garoscio M, Meissner J, et al. Is there an indication for prophylactic balloon kyphoplasty? A pilot study. Clin Orthop Relat Res. 2007;458:83–9. doi: 10.1097/BLO.0b013e318034032c. [DOI] [PubMed] [Google Scholar]
- 24.Bula P, Lein T, Strassberger C, Bonnaire F. [Balloon kyphoplasty in the treatment of osteoporotic vertebral fractures: indications - treatment strategy - complications] Z Orthop Unfall. 2010;148:646–56. doi: 10.1055/s-0030-1250379. [Article in German] [DOI] [PubMed] [Google Scholar]


