Summary
The endovascular approach is described in 113 middle cerebral artery (MCA) aneurysms. The treatment failed in six cases with no adverse clinical consequences. Out of the 107 treated cases, it was possible to obtain a complete occlusion in 50 aneurysms (47%), whereas a residual aneurysm neck was observed in 54 cases (50%). Follow-up angiograms were performed in 60 cases, showing a 22% rate of further thrombosis of the aneurysm. Recanalization of the aneur-ysm was observed in 8% of cases, which required re-treatment.
The technique-related permanent morbidity rate was 9% while the mortality rate was 2%. A review of the surgical and endovascular literature is presented. The endovascular approach is particularly indicated when normal MCA branches do not arise from the aneurysm base. It must be meticulously planned in all other cases. Endovascular coil treatment of MCA aneur-ysms is feasible, with acceptable morbi-mortality rates.
Key words: MCA aneurysms, endovascular treatment, coils
Introduction
The middle cerebral artery (MCA) is the third most common site for brain aneurysms and accounts for approximately 20% of all aneurysms. The majority of MCA aneurysms present with rupture13.
Of all ruptured brain aneurysms, MCA aneurysms present the highest incidence (34%) of intracerebral hematoma13. In addition, the neck, base, or body of MCA aneurysms may incorporate normal branches. These two characteristics explain why, historically, the majority of MCA aneurysms are treated by open surgery while only a minority are treated with the endovascular approach12.
In the past three years, however, relatively large series on endovascular treatment of MCA aneurysms have appeared in the literature, showing satisfactory anatomical and clinical results2,3,5,6,8,9.
We report our experience with the endovascular management of 113 MCA aneurysms using detachable coils.
Material and Methods
Patient Population
A consecutive series of 113 patients with MCA aneurysms is the subject of this report. The age of the 113 patients ranged from 16 to 79 years, with an average of 54 years. Seventy-one patients (63%) were females and 42 (37%) were males.
Clinical Presentation
As to the mode of presentation, 50 patients had an incidental aneurysm, 52 presented with SAH, nine with symptoms of mass effect, and two with TIA. Of the 52 patients that presented with SAH, 19 were in HH grade I, ten in grade II, ten in grade III, 11 in grade IV, and two in grade V.
Aneurysm Characteristics
Of the 113 aneurysms, 88 were small (4 to 15 mm in diameter), 15 were large (15 to 25 mm in diameter), and ten were giant (more than 25 mm in diameter).
As to the size of the aneurysm neck, 59 aneurysms had a small neck (4 mm or less), 43 a wide neck (more than 4 mm), and 11 were fusiform.
Indications for Endovascular Treatment
Endovascular treatment rather than surgical clipping was performed for the following reasons. In 29 patients poor medical condition/poor grading contraindicated surgery. Previous surgical clipping had failed in 12 cases. Surgery was refused by 35 patients. Endovascular treatment was performed in the remaining 37 patients due to anticipated surgical difficulties.
Technique
General anesthesia and systemic heparinization were utilized in all cases. After microcatheterization of the aneurysm, GDC coils (Boston Scientific Neurovascular, Fremont, California) or Matrix coils (Boston Scientific Neurovascular, Fremont, California) were delivered and detached into the aneurysm until dense aneurysm packing was achieved, trying not to compromise the ostium of the surrounding MCA branches. An embolization was considered to be complete when there was no contrast filling of the dome, body or neck of the aneurysm. A neck remnant was defined as residual filling of part of the neck of an aneurysm; an incomplete embolization was indicated by contrast agent in the body of the aneurysm.
In six of the 113 cases endovascular treatment was attempted and failed, with no adverse clinical consequences. Therefore only 107 of the 113 aneurysms were actually treated.
Follow-up Studies
Immediate clinical outcome was recorded for all patients as well as the immediate anatomical result of the endovascular treatment. It was possible to perform clinical follow-up studies in all patients. Follow-up angiography was performed in 60 of the 107 treated patients.
Results
Clinical Outcome
At the clinical follow-up studies, 92 (86%) of the 107 treated patients were either clinically unchanged or improved.
In three cases (3%) a worsening of the mass effect was observed.
In ten cases (9%) a new permanent neurological deficit was detected, which persisted at the follow-up studies. The neurological deficit was severe in four patients, moderate in three, and mild in three. These neurological deficits consisted of hemianopia in one case, aphasia and hemiplegia in one case, personality disorders in one case, aphasia in two cases, and sensory-motor deficit in five cases.
Two deaths (2%) occurred: one of the two patients died from inadvertent occlusion of the aneurysm parent artery. The other death was due to the rupture of a large aneurysm eight months after treatment.
Considering only the 49 patients with incidental aneurysms, the permanent morbidity rate was 6% (three cases) while the mortality rate was 2% (one case).
Angiographic Outcome
As to the immediate anatomical results of the endovascular treatment, complete aneurysm occlusion was achieved in 50 (47%) of the 107 treated aneurysms. A neck remnant was observed in 54 (50%) aneurysms, while the body of the aneurysm was still partially open in three (3%) cases.
Of the 60 aneurysms analyzed by follow-up angiography, 42 (70%) showed unchanged degree of occlusion, 13 (22%) showed further thrombosis of the aneurysms, while five (8%) showed coil compaction. A second embolization was performed in these five cases.
Technical Complications
Periprocedural technical complications occurred in 12 (11%) cases. The aneurysm was perforated in one case. Untoward distal cerebral embolization was observed in seven cases. The aneurysm parent artery was inadvertently occluded in four cases. Chemical thrombolysis was performed in three of these cases, while chemical and/or mechanical angioplasty was performed in six cases. Both thrombolysis and angioplasty were performed in two cases.
Surgery
Surgical procedures were performed in 20 patients. A frontal or temporal hematoma was evacuated in nine patients. Surgical EC-MCA by-pass procedure(s) were performed prior to coiling of the aneurysms in the 11 patients with fusiform aneurysms. The post-embolization clinical outcome in these 11 patients did not disclose any new neurological deficit in nine cases, whereas the mass effect symptoms were worsened by the coiling procedure in two patients with one large and one giant aneurysm respectively.
Discussion
Anatomical Configuration of MCA Aneurysms
Middle cerebral artery (MCA) aneurysms account for 20% of all intracranial aneurysms (13). They can arise from the horizontal portion (M1) of the MCA (12%), from the bifurcation of the MCA (83%), from a secondary bifurcation (3%), and from the distal branches of the MCA (2%).
M1 aneurysms may arise at the origin of the temporopolar artery or at the origin of the anterior temporal artery. In some cases M1 aneurysms may arise from a large common trunk constituted by the temporopolar and anterior temporal branches. In some cases M1 aneurysms may arise at the origin of the lateral lenticulostriate arteries or at the origin of the lateral fronto-orbital artery. M1 aneurysms may also arise from a large common trunk constituted by the lenticulostriate and frontoorbital branches.
MCA bifurcation aneurysms arise at the bifurcation of the inferior trunk and superior trunk of M2. It is important to note that, in this kind of aneurysms, lenticulostriate branches may arise in close proximity of the neck of the aneurysm in 22% of cases13.
Fusiform aneurysms may arise from the MCA bifurcation itself or from one of the two trunks of the MCA bifurcation. In all these cases an extracranial-intracranial by-pass is indicated, prior to coiling of the entire aneurysm. This strategy was utilized in the 11 fusiform aneurysms of our series (vide supra).
MCA bifurcation aneurysms may have three configurations. The first configuration has a well defined neck which separates the aneurysmal sac from the MCA branches. These are the aneurysms in which the endovascular approach is particularly indicated (Figure 1). A second configuration has one or more MCA branches incorporated and arising from the aneurysm neck-base (Figure 2A,B). Especially in this latter configuration the endovascular intervention must be meticulously planned to avoid inadvertent occlusion of the major arterial trunks. A third configuration has one or more normal MCA branches arising from the aneurysm sac. In this configuration endovascular coiling is contraindicated unless a by-pass is placed before coiling. These morphologic features such as the incorporation of major branches into the aneurysmal neck-base increase the risk of normal vessel compromise and may lead to lower occlusion rates11.
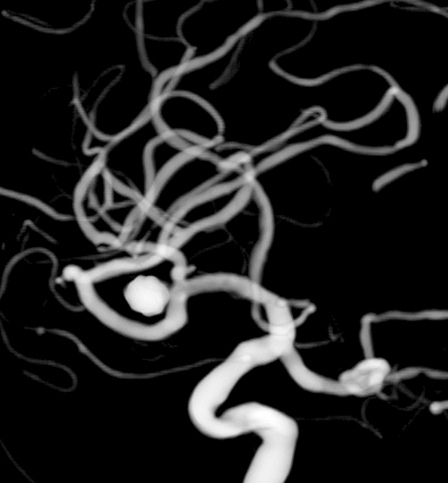
Figure 1.
One-year follow-up study showing persistent occlusion of an MCA aneurysm with coils. This is the configuration where there is a well-defined neck separating the aneurysm from the MCA branches (see discussion).
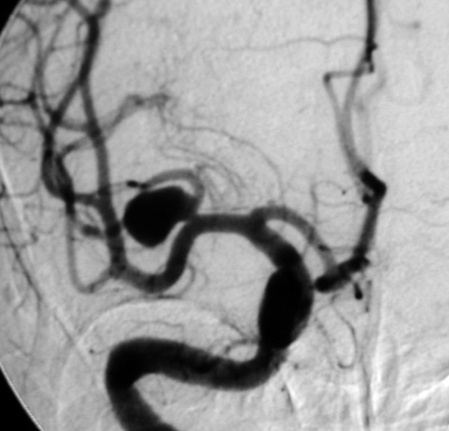
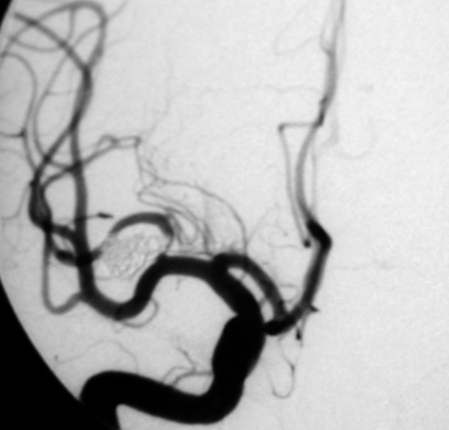
Figure 2.
A) Preoperative angiogram of an MCA aneurysm with a wide neck. This is the configuration where one or more MCA branches are incorporated and arise from the aneurysm neck-base (see discussion). B) Post-coiling angiogram showing complete occlusion of the aneurysm. There is impingement of the coils in the parent artery. This patient had a thromboembolic complication which led to a MILD permanent neurological deficit.
A.
B.
Intracerebral Hematoma in MCA Aneurysms
It is known that 50% of patients in HH grade III, and 100% of patients in HH grades IV and V present with a frontal or temporal intracerebral hematoma13 due to a ruptured MCA aneurysm. Whether the intracerebral hematoma needs to be evacuated or not depends on the severity of the mass effect upon the deep structures. In our series it was necessary to evacuate only nine intracerebral hematomas in spite of the fact that 23 patients were in HH grades III, IV, and V.
Surgical Results in MCA Aneurysms
In 2005 Baskaya1 reported the overall results of the surgical clipping of MCA aneurysms in 108 consecutive patients. In this series, 76 (70%) patients had a good outcome; in 19 (18%) patients the outcome was fair, in seven (6%) the outcome was poor, and six (6%) patients died. Considering only the 97 patients that had presented in HH grades 0 to III, 74 (76%) had a good outcome; in 14 (14%) the outcome was fair, in six (6%) the outcome was poor, and three (3%) patients died.
As to the overall outcome of other surgical series, Yasargil13, in 184 cases, reported 84% of good outcome, 11% of fair-poor outcome, and 5% of deaths. Flamm4 reported, in 114 cases, 87% of good outcome, 7% of fair-poor outcome, and 6% deaths. Rinne10, in a series of 457 cases, reported 62% of good outcome, 25% of fair-poor outcome, and 13% of deaths.
In 2007 Katz7 reported the surgical results in 42 MCA aneurysms. To highlight the difficulty of surgical clipping, he reported three unexpected remnants and two unexpected vessel occlusions, detected by postoperative angiography. Due to these findings, he advocated the use of intraoperative angiography for MCA aneurysms.
Endovascular Results in MCA Aneurysms
We found six literature reports on the endovascular treatment of MCA aneurysms2,3,5,6,8,9.
Bulsara et Al.2 reported the results in 71 selected cases. Cases with intracerebral hematoma causing significant mass effect and cases where normal branches arose from the sac of the aneurysm were excluded from the endovascular approach. Total aneurysm occlusion was achieved in 51% of the 71 cases. The permanent morbidity related to the procedure was 2.8%. The aneurysm recanalization rate at follow-up angiograms was 11%. No procedure-related mortality was reported.
Horowitz et Al6 reported the results in 30 equally selected cases. Total aneurysm occlusion was achieved in 80% of cases. The permanent morbidity rate related to the procedure was 7%.
Doerfler et Al 3, in a series of 33 MCA aneurysms, reported a complete occlusion rate of 76%. In four cases a transient neurological deficit was detected. The permanent morbidity rate due to the technique was 3%.
Hirota et Al5, in a series of 65 MCA aneurysms, reported a complete occlusion rate of 43%. In eight cases (12%) thromboembolic complications occurred, which eventually led to one case of permanent neurological deficit. In four cases the aneurysm was perforated during the procedure, with no mortality. Rebleeding occurred in two cases, that were retreated with additional coiling.
Lijima et Al8, in a series of 149 cases with MCA aneurysms, reported a complete occlusion rate of 77%, a residual neck remnant in 19.5% of cases, and a residual base-body of the aneurysm in 3.5% of cases. The reported treatment-related permanent morbidity rate was 2%, while the mortality rate was 3.5%.
Quadros et Al9, in a series of 59 MCA aneurysms, reported a complete occlusion in 42% of the aneurysms, a residual neck in 43.5%, and a residual base-body of the aneurysm in 14.5 percent of cases. Permanent morbidity due to the technique was 6%, while the mortality was 2% (perforation of the aneurysm).
In our series we observed a 47% complete occlusion rate, while a neck remnant was detected in 50% of cases. Notably, 22% of the controlled cases showed further thrombosis of the aneurysm at the follow-up angiogram. Coil compaction was observed in five (8%) of the controlled cases, requiring retreatment. As to the technique-related complications, we observed a 9% permanent morbidity rate and a 2% mortality rate, which includes a case of rebleeding from a subtotally occluded large aneurysm eight months after treatment. Longer term angiographic and clinical follow-up studies will be necessary to assess the long term durability of the procedure.
Different technologies, such as endovascular stents, compliant balloons for the balloon-assisted technique, and diverse coil shapes and coatings might improve the results of the endovascular approach in these highly complex lesions.
Conclusions
Endovascular treatment of MCA aneurysms is feasible, with acceptable morbi-mortality rates. Embolization is particularly indicated when normal branches do not arise from the base of the aneurysm. Endovascular treatment must be meticulously planned when one or more branches arise from the aneurysm neck-base. The presence of an intracerebral hematoma causing significant mass effect (and requiring rapid evacuation) contraindicates the endovascular approach.
References
- 1.Baskaya M, Coscarella E, et al. Surgical management of middle cerebral artery aneurysms. Neurosurgery Quarterly. 2005;15:201–210. [Google Scholar]
- 2.Bulsara K, Tolbert M, Alexander M. Experience in the endovascular management of 76 patients with middle cerebral artery aneurysms. Annual Meeting of the Congress of Neurological Surgeons; 2006 October 7-12; Chicago (Illinois). 2006. [Google Scholar]
- 3.Doerfler A, Wanke I, et al. Endovascular treatment of middle cerebral artery aneurysms with electrolytically detachable coils. Am J Neuroradiol. 2006;27:513–520. [PMC free article] [PubMed] [Google Scholar]
- 4.Flamm ES, Fein JM. Middle cerebral artery aneurysms. . In: Flamm ES, Fein JM, editors. Cerebrovascular Surgery. New York: Springer-Verlag; 1985. pp. 861–877. Vol III. [Google Scholar]
- 5.Hirota N, Musacchio M, et al. Angiographic and clinical results after endovascular treatment for middle cerebral artery berry aneurysms. Neuroradiology Journal. 2007;20:89–101. doi: 10.1177/197140090702000116. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz M, Gupta R, et al. Clinical and anatomical outcomes after endovascular coiling of middle cerebral artery aneurysms: report on 30 treated aneurysms and review of the literature. Surgical Neurology. 2006;66:167–171. doi: 10.1016/j.surneu.2005.12.022. [DOI] [PubMed] [Google Scholar]
- 7.Katz JM, Gologorsky Y, et al. Is routine intraoperative angiography in the surgical treatment of cerebral aneurysms justified? A consecutive series of 147 aneurysms. . Neurosurgery. 2006;58:719–727. doi: 10.1227/01.NEU.0000204316.49796.A3. [DOI] [PubMed] [Google Scholar]
- 8.Lijima A, Piotin M, et al. Endovascular treatment with coils of 149 middle cerebral artery berry aneurysms. Radiology. 2005;237:611–619. doi: 10.1148/radiol.2372041015. [DOI] [PubMed] [Google Scholar]
- 9.Quadros R, Gallas S, Noudel R, et al. Endovascular treatment of middle cerebral artery aneurysms as first option: a single center experience of 92 aneurysms. Am J Neuroradiol. 2007;28:1567–1572. doi: 10.3174/ajnr.A0595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rinne J, Hernesniemi J, Niskanen M. Analysis of 561 patients with 690 middle cerebral artery aneurysms: anatomic and clinical features as correlated to management outcome. Neurosurgery. 1996;38:2–11. doi: 10.1097/00006123-199601000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Son YJ, Han DH, Kim JE. Image-guided surgery for treatment of unruptured middle cerebral artery aneurysms. Operative Neurosurgery. 2007;61(Sup 2):ONS266–ONS272. doi: 10.1227/01.neu.0000303979.88880.06. [DOI] [PubMed] [Google Scholar]
- 12.Viñuela F , Duckwiler G, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysms: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86:475–482. doi: 10.3171/jns.1997.86.3.0475. [DOI] [PubMed] [Google Scholar]
- 13.Yasargil G. Middle cerebral artery aneurysms. In: Yasargil G, editor. Microneurosurgery. New York: Thieme Verlag; 1984. pp. 124–164. Vol II. [Google Scholar]