Summary
The trigeminal artery is an anastomosis between the embryonic precursors of the vertebrobasilar and carotid systems, and may persist into adult life. The association of the persistent primitive trigeminal artery (PTA) with cerebral aneurysm is well documented in the literature and, in general, aneurysms are located in the anterior circulation. We describe a patient who presented with a panencephalic Fisher III subarachnoid hemorrhage due to rupture of an intracranial aneurysm. Digital arteriography showed a saccular aneurysm in the middle third of the basilar artery, adjacent to the junction with a persistent trigeminal artery. She was submitted to endovascular treatment with embolization of the basilar artery aneurysm with coils. Aneurysms at the PTA junction with the basilar artery are rare. This paper describes a case of PTA associated with an aneurysm in the basilar artery at PTA junction and briefly reviews the literature.
Key words: trigeminal artery, basilar artery, aneurysm, subarachnoid hemorrhage
Introduction
The trigeminal artery is an anastomosis between the embryonic precursors of the vertebrobasilar and carotid systems, and may persist into adult life, resulting from embryogenesis defects in 1 to 6/1000 angiographies 1,2. Its occurrence is related to the presence of the hypoplastic vertebral artery, arteriovenous malformations, cerebral aneurysms or other vascular malformations 1. The association of the persistent primitive trigeminal artery (PTA) with cerebral aneurysm is well documented in the literature and in general aneurysms are located in the anterior circulation 3. Aneurysms at the PTA junction with the basilar artery are rare 4. The objective of this paper is to describe a case of PTA associated with an aneurysm in the basilar artery at the PTA junction and briefly review the literature.
Case Report
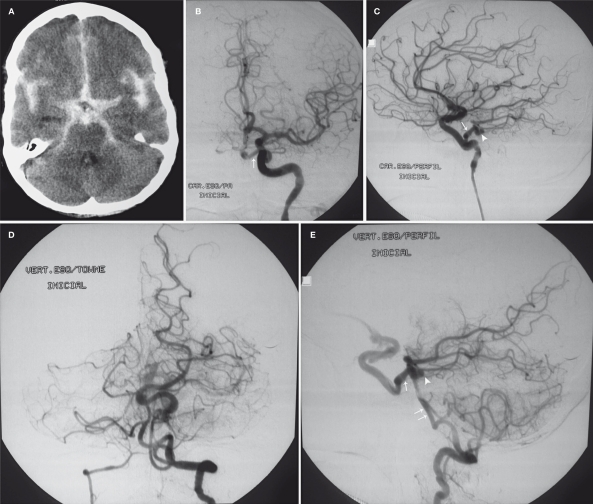
A 53-year-old woman had a sudden and intense episode of headache. At the emergency room, she presented with a panencephalic Fisher III subarachnoid hemorrhage (SAH) (Figure 1A) upon undergoing a computed tomography scan. The patient was in good clinical condition (Hunt and Hess I). Digital arteriography showed a saccular aneurysm (4×4 mm, with a 4 mm neck) in the middle third of the basilar artery, adjacent to the junction with the persistent trigeminal artery (Figure 1B-E) in addition to a small aneurysm in the anterior communicating complex.
Figure 1.
A) Computed tomography scan showing SAH Fisher III. Cerebral angiography of the left internal carotid artery (B - frontal incidence and C - lateral incidence) and the left vertebral artery (D - frontal incidence and E – lateral incidence) showing the persistent trigeminal artery (arrow) and the aneurysm (arrowhead) in its junction with basilar artery (double arrow).
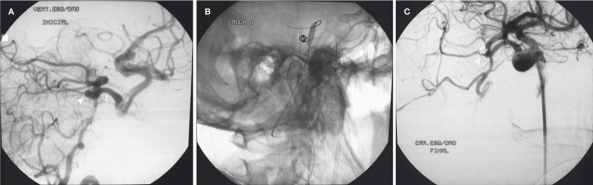
Figure 2.
Cerebral angiography in oblique incidence. A) Aneurysm in the basilar artery (arrowhead), in the junction with the persistent trigeminal artery (arrow). B) Microcatheterism of the aneurysm during the installation of coils, with inflated balloon. C) Final angiographic control showing the absence of opacification of the aneurysm (arrowhead).
The patient underwent endovascular treatment with embolization of the basilar artery aneurysm with coils and a remodeling technique. An Envoy 6F guide catheter (Cordis, Miami Lakes, FL, USA) was positioned in the left vertebral artery and through it, a balloon catheter HyperGlide 4×15 (Micro Therapeutics, Irvine, CA, USA) was progressed and located in the basilar artery near the aneurysm neck. Despite proximal basilar artery hypoplasia, we did not find any difficulty in progression and positioning the balloon. Another Envoy 6F guide catheter (Cordis, Miami Lakes, FL, USA) was positioned in the left internal carotid artery. Through this device we advanced an Excelsior 1018 microcatheter (Boston Scientific Co., Natick, MA, USA) with a Transcend-14 microguide (Boston Scientific Co., Natick, MA, USA) through the trigeminal artery for aneurysmal sac catheterization. The aneurysm was embolized with MicruSphere coils (Micrus Endovascular, San Jose, CA, USA). The incidence used for the procedure was right anterior oblique. The patient was discharged on the fourth postoperative day without neurological deficits.
Discussion
During embryonic development, approximately on the 35th day of gestational age, the intracranial circulation is characterized by the connection between the carotid arteries and the precursor arteries of the vertebrobasilar system 1,5. The posterior circulation in embryogenesis begins to develop from the two longitudinal neural arteries, which fuse at the median line to form the basilar artery. A plexus is formed which is inferiorly supplied by the cervical intersegmentary arteries and four transitory anastomoses with the carotid artery which, in the rostrocaudal orientation are: the trigeminal, otic, hypoglossal and proatlantal intersegmental arteries 1,5,6. Upon the formation of the posterior communicating artery and the fusion of the longitudinal neural arteries into the basilar artery, these anastomotic vessels begin to wane until they completely disappear.
In some cases, there is no regression of the fetal connection between the internal carotid artery at its intracavernous segment with the superior third of the basilar artery, constituting the persistent trigeminal artery 1,6. The PTA is the remaining embryonic circulation most commonly found in adult life. It is located under the posterior communicating artery and is the most frequent type of primitive anastomosis (85%) between the carotid and basilar systems 1,7. It is present in 0.1-0.6% of individuals 1,2,6 and is associated with hypoplasia or absence of the ipsilateral posterior communicating artery. Furthermore, it is related to basilar and vertebral arteries hypoplasia, vascular malformations, aneurysms, hemangiomas and aortic arc alterations 1,3.
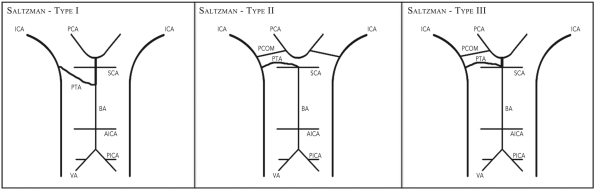
According to the Saltzman Classification (1958), there are three types of anatomical variations of the PTA 1,2 (Figure 3). In variation type I, the PTA installs itself in the basilar artery between the anterior inferior cerebellar artery (AICA) and superior cerebellar artery (SCA), in which case the supply of the distal arteries to the anastomosis depends entirely on the PTA. In this way, basilar arterial hypoplasia proximal to the anastomosis occurs and the posterior communicating artery may involute; in type II, the PTA installs itself in the basilar artery, but mainly supplies the superior cerebellar artery bilaterally. In this case, the posterior cerebellar artery (PCA) receives a flux from the corresponding posterior communicating artery; whereas in type III, there is a combination of the first two types in which the persistent anastomosis supplies both the SCA bilaterally and the PCA contralaterally 1,2. In the present case, the PTA installed itself in the basilar artery right below the superior cerebellar arteries, having proximal basilar arterial hypoplasia (Figure 1D,E), thus being classified as type I. There is yet another classification which takes into consideration the dependence (fetal type) or independence (adult type) of the posterior circulation in relation to the PTA 4, this being important in therapeutic planning.
Figure 3.
Schematic representation of the variations of the trigeminal persistent artery according to Saltzman; (comments in the discussion). ICA - internal carotid artery; SCA - superior cerebellar artery; PTA - persistent trigeminal artery; AICA - anterior inferior cerebellar artery; PICA - posterior inferior cerebellar artery; PCA - posterior cerebral artery; BA - basilar artery; VA - vertebral artery (modified from Ali et al. 1).
The majority of the carriers of PTA are asymptomatic 3. In the symptomatic patients, among clinical findings related to the presence of PTA are the symptoms of posterior circulatory hypoperfusion or posterior circulation carotid microembolization 3. In addition, the association with cerebral aneurysms, internal carotid arterial occlusion and the phenomenon of vascular “sequestering” between the basilar and carotid arteries have been described 1,3.
Reports in the literature show that when the trigeminal persistent artery is present, the incidence of aneurysm is around 12-14% 3,8. Of these, only 13% are in the trigeminal persistent artery, while the majority are found in the Willis circle 3,8. According to Takase et al. 4, only 12 cases of persistent trigeminal arterial trunk aneurysms had been reported as of 2004, eight of which presented subarachnoid hemorrhage 4.
Two types of aneurysms related to the PTA have been described: those which originate at the junction with the internal carotid artery (type I) and those which originate directly from the PTA (type II) 9. Aneurysms at the junctions with the basilar artery, as well as those in other regions of the Willis circle, have also been reported 4. In the present case, the aneurysm was located in the basilar artery, at the junction with the persistent trigeminal artery. It is believed that the hemodynamic alterations caused by the presence of the PTA determine a higher level of stress to the vessel, its dilation and consequent rupturing of the aneurysm 10.
The persistent trigeminal artery is identified in many cases by incidental findings in magnetic resonance imaging 3. In these cases, one may request complementary investigation with angiography, having other vascular alterations in mind, mainly aneurysms 1,3,4. Recently, the endovascular method has become the treatment of choice for PTA aneurysms 9. In addition to promoting treatment, this method can be utilized to evaluate the clinical significance of the PTA and of its perforating branches by occlusion testing, which can guide both the endovascular treatment and the microsurgical clipping 4,9. In the cases in which the independence of the circulation posterior to the PTA (adult type) is verified, the PTA can actually be occluded 4. On the other hand, when there is the fetal pattern, in which there is the dependence of blood flow of the PTA to the vasculature of the vertobasilar territory, the PTA must obligatorily be kept pervious. Thus, the presence of the persistent trigeminal artery associated with an aneurysm in the basilar artery is a rare condition. The management of this condition by means of endovascular techniques represents a viable alternative with good therapeutic results.
References
- 1.Ali S, Radaideh MM, Shaibani A, et al. Persistent trigeminal artery terminating in the posterior inferior cerebellar artery: case report. Neurosurgery. 2008;62:746–748 . doi: 10.1227/01.neu.0000317327.17225.f8. [DOI] [PubMed] [Google Scholar]
- 2.Varghese SPJ. Persistent trigeminal artery and associated vascular variations. Australasian Radiology. 2007;51:31–33 . doi: 10.1111/j.1440-1673.2007.01828.x. [DOI] [PubMed] [Google Scholar]
- 3.Cloft HJ, Razack N, Kallmes DF, et al. Prevalence of cerebral aneurysms in patients with persistent primitive trigeminal artery. J Neurosurg. 1999;90:865–867 . doi: 10.3171/jns.1999.90.5.0865. [DOI] [PubMed] [Google Scholar]
- 4.Takase T, Tanabe H, Kondo A, et al. Surgically treated aneurysm of the trunk of the persistent primitive trigeminal artery-case report. Neurol Med Chir (Tokyo) 2004;44:420–423 . doi: 10.2176/nmc.44.420. [DOI] [PubMed] [Google Scholar]
- 5.Padget DH. The development of the cranial arteries in the human embryo. Contrib Embryol. 1948;32:205–262 . [Google Scholar]
- 6.Lasjaunias P, Berenstein A, ter Brugge KG. The skull base and extradural arteries. 2nd ed. Heidelberg: Springer Verlag; 2001. Surgical neuroangiography; pp. 387–425 . Vol 1. [Google Scholar]
- 7.Zhang CW, Xie XD, Yang ZG, et al. Giant cavernous aneurysm associated with a persistent trigeminal artery and persistent optic artery. Korean J Radiol. 2009;10:519–522. doi: 10.3348/kjr.2009.10.5.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.George AE, Lin JP, Morantz RA. Intracranial aneurysm on a persistent primitive trigeminal artery: Case report. J Neurosurg. 1971;35:601–604 . doi: 10.3171/jns.1971.35.5.0601. [DOI] [PubMed] [Google Scholar]
- 9.Oizuka M, Kazekawa K, Tsutsumi M, et al. Hyperform remodeling balloon for the balloon occlusion test of persistent primitive trigeminal artery aneurysm. Neurol Med Chir (Tokyo) 2006;46:541–543 . doi: 10.2176/nmc.46.541. [DOI] [PubMed] [Google Scholar]
- 10.Ricolfi F, Decq P, Brugieres P, et al. Ruptured fusiform aneurysm of the superior third of the basilar artery associated with the absence of the midbasilar artery. J Neurosurg. 1996;85:961–965 . doi: 10.3171/jns.1996.85.5.0961. [DOI] [PubMed] [Google Scholar]