Abstract
Epidermal cyst (EC) of the skin is a very common condition. Squamous cell carcinoma (SCC) very infrequently arises from EC. A 76-year-old Japanese woman was admitted to our hospital because of multiple papules in the nose and nasal cavity. The clinical diagnosis was sebaceous hyperplasia. An excisional biopsy was obtained from one papule. Histologically, the papule showed an EC. The EC communicated with the epidermis. Islands of atypical cells with hyperchromatic nuclei and infrequent pearl formation were recognized around and adjacent to EC. No connections were seen between the atypical cell islands and epidermis. The atypical cells had hyperchromatic nuclei and nucleoli. Mitotic figures and keratinous pearls were scattered. The HE diagnosis was probable SCC probably arising from EC. Immunohistochemically, the atypical cells were positive for pancytokeratin AE1/3, cytokeratin (CK) 5/6, CK14, CK18, CK 34BE14, EMA, p53, Ki-67 (labeling 90%), and p63. They were negative for pancytokeratin CAM5.2, CK7, CK8, CK19, CK20, vimentin, S100 protein, HMB45, synaptophysin, and CD56. CD68 was positive in histiocytes and giant cells in the foreign body reaction. The EC showed the same immunoprofile as the SCC, except for negative p53 and low Ki-67 labeling in the EC. The histological and immunohistochemical diagnosis was definite SCC arising from EC.
Keywords: Squamous cell carcinoma, epidermal cyst, immunohistology
Introduction
Epidermal cyst (EC) of the skin is a very common condition. It has been very infrequently reported that squamous cell carcinoma (SCC) arises from EC [1-3]. The author herein reports such a case.
Case report
A 76-year-old Japanese woman consulted to our hospital because of multiple nasal papules. Physical examination revealed multiple papules in the nose and nasal cavity. The clinical diagnosis was sebaceous hyperplasia. An excisional biopsy was obtained from one papule.
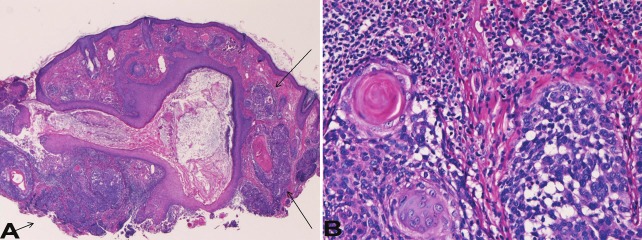
Histologically, the section showed an EC (Figure 1A). The cyst communicated with the epidermis (Figure 1A). The cyst resembled hair infundibulum and contained granular layer. Many foci of foreign body reaction were recognized in the nearby dermis. Islands of atypical cells with hyperchromatic nuclei and infrequent pearl formation were recognized around and adjacent to the epidermal cyst (Figure 1A). No connections were seen between the atypical cell islands and epidermis. Higher power view showed that the atypical cells had hyperchromatic nuclei (Figure 1B). Mitotic figures and keratinous pearls were scattered. The HE diagnosis was probable SCC probably arising from epidermal cyst.
Figure 1.
Histologicaly features. A: A very low power view of the lesion shows an epidermal cyst and atypical cell clusters (arrows). HE, x20. B: The high power view of the atypical cells show nuclear hyperchromasia, increased nucleo/cytoplasmic ration, and pearl formation. HE, x200.
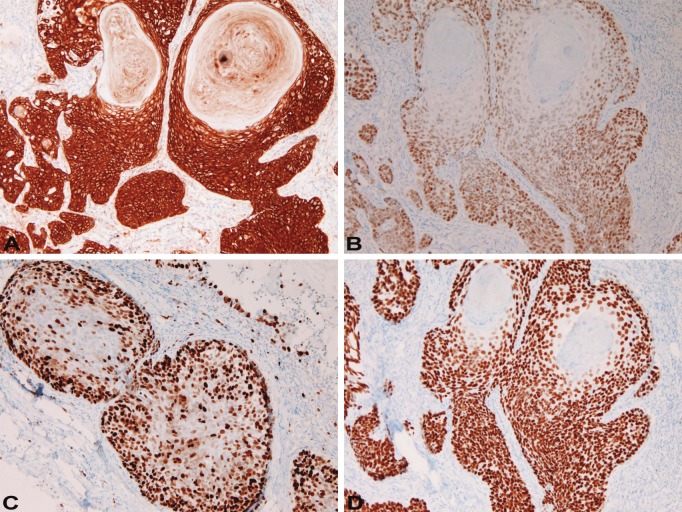
An immunohistochemical study was performed with the use of Dako Envision method, as previously described [4,5]. Immunohistochemically, the atypical cells were positive for pancytokeratin AE1/3, cytokeratin (CK) 5/6 (Figure 2A), CK14, CK18, CK 34BE14, EMA, p53 (Figure 2B), Ki-67 (labeling 90%) (Figure 2C), and p63 (Figure 2D). They were negative for pancytokeratin CAM5.2, CK7, CK8, CK19, CK20, vimentin, S100 protein, HMB45, synaptophysin, and CD56. CD68 was positive in histiocytes and giant cells in the foreign body reaction. The EC showed the same immunoprofile as the SCC, except for negative p53 and low Ki-67 labeling in the EC. The histological and immunohistochemical diagnosis was definite SCC arising from EC.
Figure 2.
Immunohistochemical features of atypical cells. They were positive for cytokeratin 5/6 (A), p53 protein (B), Ki-67 antigen (labeling 90%) (C), and p63 (D). A-D: x200.
Discussion
The atypical cells next to the EC (infundibular cyst) are SCC histologically and immunohistochemically. The SCC in the present case was strongly suspected by histology and confirmed by immunohistochemistry. Immunohistochemical demonstration of CK, p63, p53, and high Ki-67 labeling indicates SCC. The origin of SCC was unclear. Although direct connection between SCC and EC was not seen in this section, it is highly suggested that the SCC and EC was connected in other places. The similar immunoprofile between SCC and EC supports that the SCC arose from EC. The close spatial association between SCC and EC may support this. The SCC was not continuous with epidermis, suggesting that the SCC did not arise from epidermis. The possibility remains that the SCC might arose from the hair infundibulum.
Finally, the present case had multiple small papules in the nose and nasal cavity. The present biopsy is the only one of such papules. The histology of other papules remained to be solved.
References
- 1.Lopez-Rios F, Rodriguez-Peralto JL, Castano E, Benito A. Squamous cell carcinoma arising in a cutaneous epidermal cyst: case report and literature review. Am J Dermatopathol. 1999;21:174–177. doi: 10.1097/00000372-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Cameron DS, Hilsinger RL Jr. Squamous cell carcinoma in an epidermal inclusion cyst: case report. Otolaryngol Head Neck Surg. 2003;129:141–143. doi: 10.1016/S0194-59980300466-2. [DOI] [PubMed] [Google Scholar]
- 3.Malone JC, Sonnier GB, Hughes AP, Hood AF. Poorly differentiated squamous cell carcinoma arising within an epidermal cyst. Int J Dermatol. 1999;38:556–558. doi: 10.1046/j.1365-4362.1999.00704.x. [DOI] [PubMed] [Google Scholar]
- 4.Terada T, Kawaguchi M, Furukawa K, Sekido Y, Osamura Y. Minute mixed ductal-endocrine carcinoma of the pancreas with predominant intraductal growth. Pathol Int. 2002;52:740–746. doi: 10.1046/j.1440-1827.2002.01416.x. [DOI] [PubMed] [Google Scholar]
- 5.Terada T, Kawaguchi M. Primary clear cell adenocarcinoma of the peritoneum. Tohoku J Exp Med. 2005;206:271–275. doi: 10.1620/tjem.206.271. [DOI] [PubMed] [Google Scholar]