Abstract
Purpose
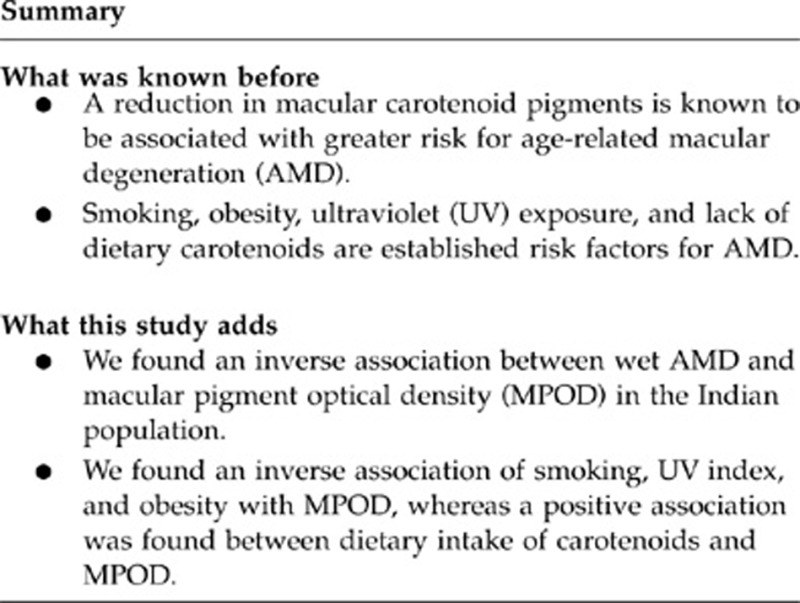
To investigate macular pigment optical density (MPOD) in patients with and without wet age-related macular degeneration (AMD) and to elucidate the association between MPOD and the risk factors for AMD in an Indian population.
Methods
Thirty-three subjects with wet AMD and 29 controls above 50 years old underwent MPOD measurement with the ‘Macular Densitometer'. The subjects were also tested for their smoking history, lifetime ultraviolet (UV) exposure, dietary intake of carotenoids, and body mass index (BMI).
Results
Smokers had a higher risk for AMD than the non-smokers (P=0.032) and a lower MPOD level than non-smokers (mean (95% CI)) (0.16 (0.09–0.23) vs 0.28 (0.22–0.34), adjusted P=0.026). Subjects with lowest UV exposure had higher MPOD than those with the highest (0.46 (0.38–0.54) vs 0.17 (0.01–0.33), P=0.01). MPOD was significantly lower among those with the lowest quartile of dietary intake of carotenoids (0.14 (0.08–0.21) vs 0.25 (0.13–0.36), P=0.012). Smoking, obesity, and UV index showed an inverse association with the MPOD. Low MPOD, smoking, and UV exposure had 5.11 (1.73–15.08), 3.54 (1.08–11.57), and 5.24 (1.06–25.96) odds for AMD, respectively, whereas higher dietary intake of carotenoids showed a protective effect for AMD.
Conclusion
We found an inverse association between wet AMD and MPOD. Among the established risk factors of wet AMD, we found an inverse association of smoking, UV index, and obesity with MPOD, whereas a positive association was found between dietary intake of carotenoids and MPOD.
Keywords: macular pigment optical density, age-related macular degeneration, ultraviolet index, smoking, obesity, dietary carotenoids
Introduction
Various epidemiological studies have shown varying association of age-related macular degeneration (AMD) and macular pigment (MP). Although few reported an inverse association,1, 2, 3, 4 most of them failed to prove any relationship.5, 6, 7 Moreover, the data from these western studies cannot be extrapolated to the Indian population. Nolan et al8 studied the association of macular pigment optical density (MPOD) with risk factors for AMD in Irish subjects and reported that there is a relative lack of MP in association with the risk factors for AMD. There exists an interplay between the risk factors of AMD and the factors influencing MPOD level. Increasing age, smoking, ultraviolet (UV) exposure, and obesity influence the occurrence of AMD, as well as the levels of MPOD.8, 9, 10, 11, 12, 13 Another important determinant of the level of MPOD is the dietary intake of carotenoids.14 With this background, the aim of this study was to investigate MPOD in patients with and without wet AMD in an Indian population and to elucidate the relationship of MPOD with established risk factors for AMD in this population.
Materials and methods
Between the years 2003 and 2006, a genome-wide association study (GWAS) was conducted in southern India (unpublished data) for the estimation of genetic risk factors for wet AMD in Indian ethnicity. In the southern Indian population, dry AMD is being evaluated in an ongoing population-based study at our institute (SN-CARE, unpublished data). As wet AMD is less common, it is difficult to evaluate the disease in a population-based study. Hence, GWAS was specifically designed to evaluate wet AMD in southern Indian population. It was a case–control study consisting of 230 individuals of south Indian ethnicity aged ≥50 years, out of which 120 were unrelated cases and 110 were their age-matched controls. These subjects were recruited from the vitreo-retinal outpatient clinic at the eye institute. The ancestral origin/ethnicity of the subjects was established through self-reporting or an open questionnaire. Informed consent was obtained from the subjects. Out of the subjects who participated in the GWAS, 33 cases and 29 controls were recruited for the present study. The study was conducted after approval from the institutional review board was obtained, and the principles of the Declaration of Helsinki were followed. Inclusion criteria of cases for the present study included age ≥50 years, the presence of wet AMD,15 and a best-corrected visual acuity (BCVA) of ≤6/60 (log MAR 1.0). In patients with unilateral wet AMD, the diseased eye was included in the study. In patients having bilateral advanced AMD, the eye with the better BCVA (but still ≤6/60) was included. If both the eyes of the subject had wet AMD and similar BCVA, then one eye was tested randomly. The subjects having any ocular pathology other than wet AMD, and those who underwent vitreo-retinal surgery and retinal laser photocoagulation were excluded from the study. Healthy eyes without any ocular pathology were included as age-matched controls. One eye of each control was tested randomly to minimize any potential order effect.
To ascertain the risk factors for AMD, a detailed questionnaire was administered including the demographic, lifestyle, and medical history of the subjects. Smoking history was elicited and smoking pack year was then calculated by using the following formula: {(number of cigarettes smoked per day × number of years smoked)/20}.16 Smokers were defined as those who had smoked in the past or were currently smoking. Non-smokers were those who have never smoked in their lifetime.16 A semiquantitative food-frequency questionnaire (FFQ) was used to estimate the dietary consumption of lutein and zeaxanthin, which included questions about the usual intakes of the Indian foods rich in lutein and zeaxanthin.17
The lifetime ocular UV exposure data collection was performed as per the Melbourne visual impairment project model.18 In short, it contained collection of data on details of migration, the use of protective devices based on questionnaire, and details on UV radiation exposure at the location based on geographic location.
A comprehensive eye examination was done, including assessment of the BCVA (modified ETDRS chart, Light House Low Vision Products, New York, NY, USA); Slit-Lamp examination (Zeiss SL 130, Carl Zeiss, Jena, Germany) and intraocular pressure measurement were recorded using the Goldmann applanation tonometer (Zeiss AT 030, Carl Zeiss), followed by assessment of MPOD with ‘Macular Densitometer' (Macular Metrics Corp., Rehoboth, DE, USA). All the subjects were naive in psychophysical tasks. Retinal photographs were obtained after pupillary dilatation, using 30° three-field stereoscopic digital photography with a Carl Zeiss fundus camera (Visucamlite, Jena, Germany). Dilated retinal evaluation was performed with indirect ophthalmoscopy to exclude other retinal pathologies.
MPOD was calculated using the Macular Densitometer, based on the principle of heterochromatic flicker photometry (HFP).19 MPOD was measured at 0.50° eccentricity from fovea, regardless of the wet AMD lesion location or size. Subjects requiring distance refractive error correction were provided the correction in trial frames or allowed to wear their spectacles.
The dimension of the target was a solid disc of 0.5° arc radius (to derive a measure at 0.50° foveal eccentricity). A small black dot was present at the centre of the solid discs as a fixation aid. The wavelength composition of the test stimulus alternated between a 460-nm (peak macular pigment absorbance) and a 540-nm, 1.7-log Td reference field (minimal macular pigment absorbance) in a yoked manner. The parafoveal reference measurement was measured by asking the subjects to fixate on a red light located precisely at 7° from the central fixation. Subtracting the foveal from the parafoveal sensitivity measurement yields an optical density measure of MP.19
The subjects were trained until they were able to confidently recognize the null zone (ie, zone of no/minimal flicker). The starting flicker frequency was set at 10–11 Hz. For participants having difficulty adjusting the knob on their own, we performed the task on their behalf, instructing the subject to notify us immediately upon cessation of the flicker sensation. Readings were deemed reliable and included in the study only if the standard deviation of the readings (radiance measurements of the 460-nm light that provides a null zone) did not exceed 0.20 log units.
To ensure quality control, we standardized all the examinations and diagnostic procedures, calibrated each instrument every day, and assessed its reproducibility by measuring the data multiple times. The scale for measuring the weight was calibrated with a known weight once a week. The collected data were scrutinized manually before its entry into the computer.
Statistical analysis
Statistical analyses were performed using SPSS Windows version 14.0 (SPSS Science, Chicago, IL, USA). The normality of distribution was checked for all factors by Kolmogorov–Smirnov analysis. The data in the study followed normal distribution, and hence we used the parametric tests to determine significance. The estimated power for two sample means of the study for MPOD in cases (mean: 0.23, SD: 0.13, n=33) and control (mean: 0.44, SD: 0.18, n=29) was calculated to be 0.9994 by using STATA 10.0 (Stata Corporation, College Station, TX, USA). Chi-square test was used to compare proportions among AMD status with the independent categorical variables. Univariate and multivariate analyses were performed with AMD as the dependent variable. Independent effects of factors on AMD were assessed using logistic regression. The Student's t-test and one-way ANOVA were used for comparing MPOD with the independent variables. Adjusted mean differences were calculated using ANCOVA. Correlation coefficients were calculated by Pearson's analysis. Linear regression was applied to examine relationships between MPOD (dependent variable) and AMD, age, gender, hypertension, body mass index (BMI), UV index, smoking history, and dietary carotenoids (independent variables). A P-value of ≤0·05 was considered significant. The cutoff for low MPOD was calculated based on a receiver operating characteristic (ROC) analysis performed to assess the ability of MPOD to discriminate between subjects with and without AMD by calculating the area under the ROC curve.
Results
Table 1 summarizes the demographic, medical, lifestyle, anthropometric, and ocular characteristics of the study subjects. As expected, an AMD patient was more likely to be an older male, who is a smoker, with the highest level of UV exposure, the lowest level of dietary carotenoid consumption, and a low level of MPOD. The mean age was similar between controls and cases (68.69±6.81 for controls and 71.85±7.6 years for cases, P=0.092).
Table 1. Characteristics of the study subjects and associations betweenpotential risk factors and age-related macular degeneration (AMD).
| Variable | Control (n=29)n (%) | Case (n=33)n (%) | P-value |
|---|---|---|---|
| Gender | |||
| Female | 16 (55.2) | 10 (30.3) | |
| Male | 13 (44.8) | 23 (69.7) | 0.048 |
| Age (in years) | |||
| ≤ 69 | 17 (58.6) | 11 (33.3) | 0.046 |
| 70–74 | 7 (24.1) | 9 (27.3) | 0.778 |
| ≥ 75 | 5 (17.2) | 13 (39.4) | 0.055 |
| BMI | |||
| Lean | 4 (13.8) | 3 (9.1) | 0.696 |
| Normal | 9 (31.0) | 9 (27.3) | 0.745 |
| Overweight | 7 (24.1) | 4 (12.1) | 0.217 |
| Obese | 9 (31.0) | 17 (51.5) | 0.103 |
| Smoking status | |||
| Non smoker | 24 (82.8) | 19 (57.6) | 0.032 |
| Smoker | 5 (17.2) | 14 (42.4) | |
| UV index | |||
| First quartile | 10 (34.5) | 7 (21.2) | 0.243 |
| Second quartile | 8 (27.6) | 6 (18.2) | 0.377 |
| Third quartile | 8 (27.6) | 9 (27.3) | 0.978 |
| Fourth quartile | 3 (10.3) | 11 (33.3) | 0.037 |
| H/O hypertension | |||
| Absent | 20 (69.0) | 16 (48.5) | 0.103 |
| Present | 9 (31.0) | 17 (51.5) | |
| Dietary carotenoid (mg/d) | |||
| First quartile | 1 (3.4) | 14 (42.4) | <0.0001 |
| Second quartile | 8 (27.6) | 8 (24.2) | 0.819 |
| Third quartile | 9 (31.0) | 7 (21.2) | 0.378 |
| Fourth quartile | 11 (37.9) | 4 (12.1) | 0.035 |
| MPOD | |||
| High | 20 (69.0) | 10 (30.3) | 0.002 |
| Low | 9 (31.0) | 23 (69.7) | |
Abbreviations: BCVA, best-corrected visual acuity; BMI, body mass index; H/O, history of; mg/d, milligram per day; UV, ultraviolet.
Bold values are statistically significant.
In Table 2, the potential risk factors for AMD were assessed with univariate analyses. When age was entered in the logistic regression as a covariate, for each unit (a year) increment of age for subjects ≥75 years of age there was a 4.02 (95% CI 1.12–14.45, P=0.033)-fold increment of AMD in the study population. Smoking was significantly associated with increased risk of AMD, the unadjusted odds ratio being 3.54 (95% CI 1.08–11.57, P=0.037). A significant dose–response relationship was not observed for any of the other measures of cigarette smoking, such as years of smoking or pack years of smoking (data not shown, P>0.05). Low MPOD (OR 5.11, 95% CI 1.73–15.08, P=0.003) and fourth quartile of UV index (OR 5.24, 95% CI 1.06–25.96, P=0.043) were other significant factors associated with increased risk of AMD, whereas dietary intake of carotenoids was protective for all the quartiles (2nd, 3rd, and 4th quartile had only 7%, 6%, and 3% chance of getting AMD (P=0.022, 0.012 and 0.002), respectively).
Table 2. Univariate logistic regression analysis to study the effect ofvarious risk factors on AMD.
| Variable | Unadjusteda | P-value |
|---|---|---|
| |
OR (95% CI) |
|
| Gender | ||
| Female | 1 | |
| Male | 2.83 (0.99–8.03) | 0.050 |
| Age (in years) | ||
| ≤69 | 1 | |
| 70–74 | 1.98 (0.57–6.90) | 0.280 |
| ≥75 | 4.02 (1.12–14.45) | 0.033 |
| BMI | ||
| Lean | 1 | |
| Normal | 1.33 (0.23–7.74) | 0.749 |
| Overweight | 0.76 (0.11–5.28) | 0.783 |
| Obese | 2.52 (0.46–13.80) | 0.287 |
| Smoking status | ||
| Non smoker | 1 | |
| Smoker | 3.54 (1.08–11.57) | 0.037 |
| UV index | ||
| First quartile | 1 | |
| Second quartile | 1.07 (0.26–4.49) | 0.925 |
| Third quartile | 1.61 (0.41–6.24) | 0.493 |
| Fourth quartile | 5.24 (1.06–25.96) | 0.043 |
| H/O of hypertension | ||
| Absent | 1 | |
| Present | 2.36 (0.83–6.69) | 0.106 |
| Dietary carotenoid (mg/d) | ||
| First quartile | 1 | |
| Second quartile | 0.07 (0.01–0.68) | 0.022 |
| Third quartile | 0.06 (0.01–0.53) | 0.012 |
| Fourth quartile | 0.03 (0.00–0.27) | 0.002 |
| MPOD | ||
| High | 1 | |
| Low | 5.11 (1.73–15.08) | 0.003 |
Abbreviations: BCVA, best-corrected visual acuity; BMI, body mass index; H/O, history of; mg/d, milligram per day; UV, ultraviolet.
1 is reference with which odds ratio is calculated.
Bold values are statistically significant.
Table 3 shows the multivariate regression analysis using AMD as the dependent variable, with low MPOD unadjusted at first, and then sequentially adjusted for various factors. Low MPOD adjusted for age and gender had a significantly increased risk of AMD (OR 4.35, 95% CI 1.43–13.23, P=0.009). Keeping the age–gender constant for all the further adjustments, diabetes mellitus added in the model had an OR of 4.76 (95% CI 1.52–14.93, P=0.007), hypertension had an OR of 3.9 (95% CI 1.26–12.1, P=0.018), and smoking had an OR of 3.89 (95% CI 1.25–12.09, P=0.019). Adjusting BMI and UV index also showed significant increased odds for AMD of 3.62 (95% CI 1.14–11.51, P=0.029) and 3.54 (95% CI 1.12–11.18, P=0.031), respectively.
Table 3. Multivariate logistic regression analysis of macular pigment optical density (MPOD) with AMD with sequential adjustment of risk factors.
| Variable |
Adjusted |
|
|---|---|---|
| OR (95% of CI) | P-value | |
| Low MPOD | 5.11 (1.73–15.08) | 0.003 |
| Low MPOD+age+ gender (male) | 4.35 (1.43–13.23) | 0.009 |
| Low MPOD+age+gender+HTN | 3.90 (1.26–12.10) | 0.018 |
| Low MPOD+age+gender+smoking | 3.89 (1.25–12.09) | 0.019 |
| Low MPOD+age+gender+BMI | 3.62 (1.14–11.51) | 0.029 |
| Low MPOD+age+gender+UV index | 3.54 (1.12–11.18) | 0.031 |
Abbreviations: BMI, body mass index; 95% CI, 95% confidence interval; HTN, systemic hypertension; MPOD, macular pigment optical density; OR, odds ratio; UV, ultra violet.
Table 4 summarizes the unadjusted and adjusted mean MPOD values in relation to all the variables among AMD cases and normal controls. There was no significant effect of age and gender upon the MPOD among the AMD cases and controls. Among the controls, the mean MPOD was found to be significantly low in the obese group than that in the normal controls (0.29 (0.18–0.40) vs 0.55 (0.45–0.66), adjusted P=0.003), and adjusted MPOD was 47% higher among the normal controls than in the obese. Smokers with AMD (cases) had lower average MPOD (0.16 (0.09–0.23)) (mean (95% CI)) than the non-smokers (0.28 (0.22–0.34)) (adjusted P=0.026). In the control group, mean MPOD was significantly low in the lowest quartile of UV index than that in the highest quartile (0.46 (0.38–0.54) vs 0.17 (0.01–0.33), P=0.01), and the adjusted MPOD was 63% higher among the lowest quartile of UV index. A small increase in mean MPOD was observed beyond all the quartiles of dietary lutein and zeaxanthin among the cases. After adjusting for other correlates of MPOD, there was a statistically significant difference in the mean MPOD between the first and last quartiles of dietary intake of carotenoids (0.14 (0.08–0.21) vs 0.25 (0.13–0.36), P=0.012) among the AMD cases. The adjusted MPOD at 0.5° was 44% higher in the fifth than in the first quartiles of dietary lutein and zeaxanthin among the cases. However, the presence of hypertension did not have a significant effect upon the MPOD level in both the groups.
Table 4. Unadjusted and adjusted mean macular pigment optical density values in wet AMD.
| Variable |
Control |
Case |
||||||
|---|---|---|---|---|---|---|---|---|
|
Unadjusted |
Adjusted |
Unadjusted |
Adjusteda |
|||||
| Mean±SD | P-value | Mean (95% of CI) | P-value | Mean±SD | P-value | Mean (95% of CI) | P-value | |
| Gender | ||||||||
| Male | 0.43±0.20 | 0.870 | 0.41 (0.32–0.49) | 0.390 | 0.20±0.12 | 0.101 | 0.23 (0.18–0.28) | 0.976 |
| Female | 0.44±0.17 | 0.46 (0.39–0.54) | 0.28±0.14 | 0.23 (0.15–0.31) | ||||
| Age | ||||||||
| ≤69 | 0.48±0.17 | 0.284 | 0.47 (0.40–0.55) | 0.361 | 0.19±0.11 | 0.610 | 0.19 (0.11–0.27) | 0.457 |
| 70–74 | 0.35±0.16 | 0.40 (0.28–0.52) | 0.23±0.14 | 0.27 (0.18–0.35) | ||||
| ≥75 | 0.43±0.21 | 0.36 (0.20–0.53) | 0.25±0.14 | 0.23 (0.16–0.31) | ||||
| BMI | ||||||||
| Lean | 0.57±0.25 | 0.016 | 0.65 (0.49–0.81) | 0.003 | 0.22±0.23 | 0.759 | 0.31 (0.14–0.48) | 0.298 |
| Normal | 0.54±0.17 | 0.55 (0.45–0.66) | 0.27±0.13 | 0.27 (0.18–0.35) | ||||
| Overweight | 0.37±0.12 | 0.36 (0.23–0.49) | 0.22±0.16 | 0.15 (0.02–0.27) | ||||
| Obese | 0.33±0.11 | 0.29 (0.18–0.40) | 0.21±0.11 | 0.21 (0.16–0.27) | ||||
| Smoking status | ||||||||
| Non smoker | 0.43±0.18 | 0.861 | 0.44 (0.39–0.50) | 0.741 | 0.27±0.12 | 0.041 | 0.28 (0.22–0.34) | 0.026 |
| Smoker | 0.45±0.20 | 0.42 (0.28–0.55) | 0.18±0.12 | 0.16 (0.09–0.23) | ||||
| UV index | ||||||||
| First quartile | 0.48±0.21 | 0.350 | 0.46 (0.38–0.54) | 0.010 | 0.29±0.15 | 0.451 | 0.23 (0.12–0.34) | 0.938 |
| Second quartile | 0.46±0.17 | 0.51 (0.41–0.61) | 0.22±0.17 | 0.26 (0.15–0.36) | ||||
| Third quartile | 0.43±0.17 | 0.44 (0.35–0.52) | 0.23±0.08 | 0.22 (0.14–0.31) | ||||
| Fourth quartile | 0.26±0.04 | 0.17 (0.01–0.33) | 0.19±0.12 | 0.22 (0.14–0.29) | ||||
| H/O hypertension | ||||||||
| Absent | 0.46±0.18 | 0.379 | 0.46 (0.39–0.53) | 0.354 | 0.25±0.13 | 0.384 | 0.25 (0.19–0.31) | 0.238 |
| Present | 0.39±0.18 | 0.39 (0.28–0.50) | 0.21±0.12 | 0.20 (0.15–0.26) | ||||
| Dietary carotenoids | ||||||||
| First quartile | 0.67±NA | 0.256 | 0.58 (0.26–0.89) | 0.707 | 0.15±0.07 | 0.004 | 0.14 (0.08–0.21) | 0.012 |
| Second quartile | 0.37±0.15 | 0.41 (0.31–0.52) | 0.26±0.14 | 0.27 (0.19–0.35) | ||||
| Third quartile | 0.40±0.17 | 0.42 (0.32–0.52) | 0.34±0.09 | 0.33 (0.24–0.43) | ||||
| Fourth quartile | 0.49±0.19 | 0.46 (0.37–0.54) | 0.25±0.14 | 0.25 (0.13–0.36) | ||||
Abbreviations: BCVA, best-corrected visual acuity; BMI, body mass index; H/O, history of; UV, ultraviolet.
Adjusted for gender, age, BMI, smoking status, BCVA, UV index, H/O diabetes, H/O hypertension and dietary intake of carotenoids.
Bold values are statistically significant.
Table 5 shows the significant correlation among MPOD and various risk factors for MPOD, with MPOD showing the highest correlation with the dietary carotenoids (0.505), followed by smoking (−0.458), BMI (−0.387), UV index (−0.341), and age (−0.171).
Table 5. Correlation among MPOD and various risk factors.
| MPOD | P-value | Age | P-value | BMI | P-value | Smoking (pack years) | P-value | Dietary carotenoids | P-value | UV index | P-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MPOD | 1 | — | −0.171 | 0.184 | −0.387 | 0.002 | −0.458 | 0.048 | 0.505 | <0.0001 | −0.341 | 0.007 |
| Age | −0.171 | 0.184 | 1 | — | −0.259 | 0.042 | −0.004 | 0.986 | −0.089 | 0.492 | 0.112 | 0.385 |
| BMI | −0.387 | 0.002 | −0.259 | 0.042 | 1 | — | 0.087 | 0.723 | −0.177 | 0.169 | 0.175 | 0.173 |
| Smoking (pack years) | −0.458 | 0.048 | −0.004 | 0.986 | 0.087 | 0.723 | 1 | — | −0.445 | 0.056 | 0.064 | 0.794 |
| Dietary carotenoids | 0.505 | <0.0001 | −0.089 | 0.492 | −0.177 | 0.169 | −0.445 | 0.056 | 1 | — | −0.01 | 0.939 |
| UV index | −0.341 | 0.007 | 0.112 | 0.385 | 0.175 | 0.173 | 0.064 | 0.794 | −0.01 | 0.939 | 1 | — |
Bold values are statistically significant.
Table 6 summarizes the coefficient when analysed in a multiple linear regression model. This provides quantification of the relationship between MPOD and the variables. From this table we can conclude that a person with AMD has on an average 0.095 units of reduced MPOD compared with a person not having AMD. Similarly, we can also conclude that with every increase of 1 year in age the MPOD decreases by 0.002 units. Male gender has an MPOD that is lesser compared with that of the female gender by 0.016 units. Subjects with systemic hypertension have MPOD lower by 0.065 units in comparison with those without hypertension. With increasing BMI and UV index, there is a decrease in the MPOD level by 0.013 and 0.036 units, respectively. Smoking also has a negative influence on the MPOD level by 0.027 units, whereas with increase in dietary carotenoids the MPOD level increased by 0.014 units.
Table 6. Association between medical, lifestyle and anthropometric variables and MPOD for all the subjects.
| Variable |
Unstandardized coefficient |
Standardized coefficient |
|||
|---|---|---|---|---|---|
| B | SE | B | t | P-value | |
| Constant | 0.778 | 0.255 | 3.054 | 0.004 | |
| Presence of AMD | −0.099 | 0.042 | −0.267 | −2.358 | 0.022 |
| Age (years) | −0.003 | 0.003 | −0.105 | −0.976 | 0.333 |
| Gender (male) | −0.029 | 0.041 | −0.077 | −0.705 | 0.484 |
| History of hypertension | −0.051 | 0.037 | −0.135 | −1.357 | 0.181 |
| BMI | −0.013 | 0.004 | −0.305 | −2.978 | 0.004 |
| UV index | −0.037 | 0.023 | −0.170 | −1.617 | 0.112 |
| Smoking | −0.022 | 0.043 | −0.055 | −0.519 | 0.606 |
| Dietary carotenoids | 0.014 | 0.006 | 0.270 | 2.483 | 0.016 |
| N=62 | r2=0.548 | ||||
Abbreviation: AMD, age-related macular degeneration; BCVA, best-corrected visual acuity; BMI, Body mass index; SE, standard error; UV index, ultraviolet index.
Dependent variable=MP optical density; Gender (indicator variable: 1=male, 0=female).
Smoking status (0=never smoked, 1=past smoker).
Bold values are standardized coefficients that are statistically significant.
Prediction of MPOD
For a male subject with AMD, aged 60 years, without history of hypertension, with a BMI of 27, a UV index of 0.5, dietary carotenoid intake of 12 mg/day, and who is a smoker, the predicted MPOD=0.778+(−0.099) × 1+(−0.003) × 60+ (−0.029) × 1+(−0.051) × 0+(−0.013) × 27+ (−0.037) × 0.5+(−0.022) × 1+(0.014) × 12=0.246.
Discussion
Although wet AMD constitutes only 10–20% of patients with AMD, it is the most visually disabling form of AMD.20 Many studies have suggested an inverse association between risk of wet AMD and levels of MP in subjects' diet and serum.21, 22 The dry and wet subtypes of AMD may have different etiologies and risk factors, and the need to examine MP in wet AMD separately has been emphasized.23 Although MPOD has been researched extensively in wet AMD in Caucasian subjects,1, 2, 4 the same is not true for Indian subjects. In our south Indian population, dry AMD is already being evaluated in a large population-based study at our institute (unpublished data). As wet AMD is less common, it is difficult to evaluate the disease in a population-based study. Hence, the present study was specifically designed to elucidate the association between MPOD and wet AMD.
We found an inverse association between MPOD and wet AMD in the present study. Previous studies have shown lower levels of MPOD in subjects with AMD than in controls.1, 2, 3, 4 However, these studies had several limitations, including the lack of adjustment of the various factors affecting MPOD, lack of demonstration of an established association among the risk factors and the levels of MPOD, and applicability of most studies to western population. The data of such studies might not be extrapolated for the Indian population. Furthermore, it is difficult to compare the results of these studies owing to the differing methodologies used to measure MP.1, 2, 3, 4
As age is an established risk factor for AMD,13 a fundamental question to be raised is whether there is an age-related decline in MPOD. Although there are several studies that have reported on the relationship between age and MP levels, it is difficult to draw a firm conclusion because of inconsistencies in the design, measurement techniques, and the reported results.9 We did not find any significant relationship between MPOD and age, which persisted in our multiple linear regression (r2=0.029). This finding is similar to a study showing very minimal decline of the MPOD (r2=0.082) with age.8 Studies until now have shown the age-related change in MPOD to be varying between r=0.34 and −0.664.9 In addition, Jahn et al24 showed that there is a weak negative correlation between age and MPOD, where only 1.2% of the MPOD changes with age. HFP is the most commonly used technique for measuring MP in vivo, and has been validated against in vitro measurements.25 However, the majority of HFP techniques to date used reference points at 5° eccentricity (taken as a zero reference point); it is likely that such techniques result in underestimation of peak MPOD, as MP has been shown to extend beyond this reference point.9 In addition, with age, there is an extension of the lateral extent of MP, which can be a reason for the studies with HFP showing an age-related decline in MPOD.26
Cigarette smoking is another established risk factor for AMD.13 Hammond et al10 reported that current cigarette smokers had significantly less MPOD (53%) than the control subjects. Consistent with this, we also found that smokers had significantly lower MPOD (30%) than non-smokers. Further, we demonstrated an inverse relationship between smoking frequency and MPOD (r=−0.458, P=0.048), which is again consistent with the report of Hammond et al10 (r=−0.498, P<0.01). Similarly, Nolan et al8 showed an inverse relation between the two (r=−0.239, P<0.01). The possible explanations to account for a relative lack of MP among cigarette smokers include a poor diet (with consequentially reduced levels of antioxidants) and/or increased overall oxidant load associated with tobacco use.8 Interestingly, the relative lack of MP that we found for the smokers in this study cannot be attributed to poor dietary intake of the carotenoids, as the dietary intake was similar among the smokers and non-smokers. However, we did not look upon the serum concentration of the carotenoids for a confirmation.
Recently published studies pertaining to gender differences in MPOD are conflicting. Some studies report that men have higher (13–30%) MPOD than women, whereas others deny any relationship.27, 28, 29 The Indian MPOD normative data study found no significant association of overall MPOD with gender (unpublished data), which is consistent with the present study.
Consistent with most previous reports (r=−0.078 to −0.307),8, 12 we found a significant and inverse relationship between BMI and MPOD (r=−0.387, P=0.002), which could be due to the competition between retina and adipose tissue for the absorption and uptake of carotenoids.8, 12
To the best of our knowledge, even though sunlight exposure is a known risk factor of AMD no study to date has reported an association between the UV index and the level of MPOD.11, 13 This study provides evidence to this association, with a finding of reduced MPOD in subjects with higher UV index (r=−0.341, P=0.007). The subjects having the highest level of UV exposure had 47.5% lower MPOD than the lowest exposure.
Previous studies with FFQ have reported a positive relationship between dietary intake of lutein/zeaxanthin and the MPOD (r=0.16–0.82, P<0.001), which is similar to our results (r=0.505, P<0.0001).14, 28, 29, 30, 31, 32, 33 We found that MPOD was 48% higher in the highest level of dietary intake of carotenoids, which was previously reported to be 19–31%.14, 31, 32
The regression model eventually obtained is presented in Table 6. This model explains about 54.8% of the variation in MPOD. The independent variable that has more influence on the MPOD is given by the (absolute) value of the standardized coefficient beta: the greater the value, the more the influence of the variable. In this study, dietary carotenoids (beta=0.270) had the most significant influence on MPOD than the other factors.
This is the first study showing an association between MPOD and risk factors for wet AMD in the Indian population. The inverse associations between MPOD and wet AMD observed in past studies1, 2, 3, 4 and in the present study could reflect the fact that lower MP was the consequence of loss of carotenoid-containing tissue secondary to advanced AMD. However, Bone et al2 evaluated both hypotheses in their study using theoretical models: whether individuals with low amounts of MP in their retinas are at greater risk of acquiring AMD, or whether low amounts of MP are merely a consequence of the disease. Their results were consistent with the first hypothesis. However, data from cross-sectional studies are still insufficient to rule out the possibility that having AMD might be contributing to the low levels of MP. Prospective studies are warranted that investigate MP with risk factors for AMD in the young normal population without disease, or in unaffected eye of subjects with unilateral AMD (in which the MPOD values would not be disturbed by the presence of wet AMD). One limitation of the present study is that the age matching between cases and controls was done to ±5 years. However, mean age was similar between cases and controls. Furthermore, as the patient population is small for a study that evaluates so many variables, the power of the study was calculated using various methods and was found to be high.
In conclusion, we report a significant inverse association of smoking habit, obesity, and UV index with MPOD, and a positive correlation between dietary carotenoids and MPOD in subjects with wet AMD in the Indian population.
The authors declare no conflict of interest.
References
- Beatty S, Murray IJ, Henson DB, Carden D, Koh H, Boulton ME. Macular pigment and risk for age-related macular degeneration in subjects from a Northern European population. Invest Ophthalmol Vis Sci. 2001;42:439–446. [PubMed] [Google Scholar]
- Bone RA, Landrum JT, Mayne ST, Gomez CM, Tibor SE, Twaroska EE. Macular pigment in donor eyes with and without AMD: a case-control study. Invest Ophthalmol Vis Sci. 2001;42:235–240. [PubMed] [Google Scholar]
- Obana A, Hiramitsu T, Gohto Y, Ohira A, Mizuno S, Hirano T, et al. Macular carotenoid levels of normal subjects and age-related maculopathy patients in a Japanese population. Ophthalmology. 2008;115:147–157. doi: 10.1016/j.ophtha.2007.02.028. [DOI] [PubMed] [Google Scholar]
- Bernstein PS, Zhao DY, Wintch SW, Ermakov IV, McClane RW, et al. Resonance Raman measurement of macular carotenoids in normal subjects and in age-related macular degeneration patients. Ophthalmology. 2002;109:1780–1787. doi: 10.1016/s0161-6420(02)01173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbertson FM, Peirson SN, Wulff K, Foster RG, Downes SM. Blue light-filtering intraocular lenses: review of potential benefits and side effects. J Cataract Refract Surg. 2009;35:1281–1297. doi: 10.1016/j.jcrs.2009.04.017. [DOI] [PubMed] [Google Scholar]
- Mainster MA, Turner PL. Retinal examination and photography are safe...is anyone surprised. Ophthalmology. 2010;117:197–198. doi: 10.1016/j.ophtha.2009.11.046. [DOI] [PubMed] [Google Scholar]
- LaRowe TL, Mares JA, Snodderly DM, Klein ML, Wooten BR, Chappell R. CAREDS Macular pigment study group macular pigment density and age-related maculopathy in the Carotenoids in age-related eye disease study. An ancillary study of the women's health initiative. Ophthalmology. 2008;115:876–883. doi: 10.1016/j.ophtha.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Nolan JM, Stack J, O' Donovan O, Loane E, Beatty S. Risk factors for age-related maculopathy are associated with a relative lack of macular pigment. Exp Eye Res. 2007;84:61–74. doi: 10.1016/j.exer.2006.08.016. [DOI] [PubMed] [Google Scholar]
- Berendschot TT, van Norren D. On the age dependency of the macular pigment optical density. Exp Eye Res. 2005;81:602–609. doi: 10.1016/j.exer.2005.03.019. [DOI] [PubMed] [Google Scholar]
- Hammond BR, Wooten BR, Snodderly DM. Cigarette smoking and retinal carotenoids: implications for age-related macular degeneration. Vision Res. 1996;36:3003–3009. doi: 10.1016/0042-6989(96)00008-9. [DOI] [PubMed] [Google Scholar]
- Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD. Sunlight exposure and the 10-Year incidence of age-related maculopathy. Arch Ophthalmol. 2004;122:750–757. doi: 10.1001/archopht.122.5.750. [DOI] [PubMed] [Google Scholar]
- Nolan J, O'Donovan O, Kavanagh H, Stack J, Harrison M, Muldoon A, et al. Macular pigment and percentage of body fat. Invest Ophthalmol Vis Sci. 2004;45:3940–3950. doi: 10.1167/iovs.04-0273. [DOI] [PubMed] [Google Scholar]
- Clemons TE, Milton RC, Klein R, Seddon JM, Ferris FL. 3rd. Age-Related Eye Disease Study Research Group. Risk factors for the incidence of advanced age-related macular degeneration in the Age- Related Eye Disease Study. Age Related Eye Disease Study report number 19. Ophthalmology. 2005;112:533–539. doi: 10.1016/j.ophtha.2004.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mares JA, LaRowe TL, Snodderly DM, Moeller SM, Gruber MJ, Klein ML, et al. CAREDS Macular Pigment Study Group and Investigators. Predictors of optical density of lutein and zeaxanthin in retinas of older women in the Carotenoids in Age-Related Eye Disease Study, an ancillary study of the Women's Health Initiative. Am J Clin Nutr. 2006;84:1107–1122. doi: 10.1093/ajcn/84.5.1107. [DOI] [PubMed] [Google Scholar]
- Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration the international ARM epidemiological study group. Surv Ophthalmol. 1995;39:367–374. doi: 10.1016/s0039-6257(05)80092-x. [DOI] [PubMed] [Google Scholar]
- Leffondré K, Abrahamowicz M, Siemiatycki J, Rachet B. Modeling smoking history: a comparison of different approaches. Am J Epidemiol. 2002;156:813–823. doi: 10.1093/aje/kwf122. [DOI] [PubMed] [Google Scholar]
- Hebert JR, Gupta PC, Bhonsle RB, Murti PR, Mehta H, Verghese F, et al. Development and testing of a quantitative food frequency questionnaire for use in Kerala, India. Public Health Nutr. 1998;1:123–130. doi: 10.1079/phn19980019. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Lee SE, Livingston PM, Bissinella M, Taylor HR. Ocular exposure to UV-B in sunlight: the Melbourne visual impairment project model. Bull World Health Organ. 1996;74:353–360. [PMC free article] [PubMed] [Google Scholar]
- Snodderly DM, Mares JA, Wooten BR, Oxton L, Gruber M, Ficek T. CAREDS Macular Pigment Study Group Macular pigment measurement by Heterochromatic flicker photometry in older subjects: the carotenoids and age-related eye disease study. Invest Ophthalmol Vis Sci. 2004;45:531–538. doi: 10.1167/iovs.03-0762. [DOI] [PubMed] [Google Scholar]
- Bressler NM. ‘Early detection and treatment of neovascular age related macular degeneration'. J Am Board Fam Pract. 15 (2):142–152. [PubMed] [Google Scholar]
- Anonymous. Antioxidant status and neovascular age-related macular degeneration. Eye Disease Case-Control Study Group Arch Ophthalmol 1993111104–109. [DOI] [PubMed] [Google Scholar]
- Seddon JM, Ajani UA, Sperduto RD, Hiller R, Blair N, Burton TC, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration Eye Disease Case-Control Study Group. JAMA. 1994;272:1413–1420. [PubMed] [Google Scholar]
- Cho E, Hankinson SE, Rosner B, Willett WC, Colditz GA. Prospective study of lutein/zeaxanthin intake and risk of age-related macular degeneration. Am J Clin Nutr. 2008;87:1837–1843. doi: 10.1093/ajcn/87.6.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahn C, Wüstemeyer H, Brinkmann C, Trautmann S, Mössner A, Wolf S. Macular pigment density in age-related Maculopathy. Graefe's Arch Clin Exp Ophthalmol. 2005;243:222–227. doi: 10.1007/s00417-004-0995-7. [DOI] [PubMed] [Google Scholar]
- Wooten BR, Hammond BR. Spectral absorbance and spatial distribution of macular pigment using heterochromatic flicker photometry. Optom Vis Sci. 2005;82:378–386. doi: 10.1097/01.opx.0000162654.32112.a1. [DOI] [PubMed] [Google Scholar]
- Chang Y, Lee FL, Chen SJ, Chen SF. Optical measurement of human retinal macular pigment and its spatial distribution with age. Med Phys. 2002;29:2621–2628. doi: 10.1118/1.1515761. [DOI] [PubMed] [Google Scholar]
- Hammond BR, Curran-Celentano J, Judd S, Fuld K, Krinsky NI, Wooten BR, et al. Sex differences in macular pigment optical density: relation to plasma carotenoid concentrations and dietary patterns. Vis Res. 1996;36:2001–2012. doi: 10.1016/0042-6989(95)00290-1. [DOI] [PubMed] [Google Scholar]
- Broekmans WM, Berendschot TT, Klöpping-Ketelaars IA, de Vries AJ, Goldbohm RA, Tijburg LB, et al. Macular pigment density in relation to serum and adipose tissue concentrations of lutein and serum concentrations of zeaxanthin. Am J Clin Nutr. 2002;76:595–603. doi: 10.1093/ajcn/76.3.595. [DOI] [PubMed] [Google Scholar]
- Curran-Celentano J, Hammond BR, Ciulla TA, Cooper DA, Pratt LM, Danis RB. Relation between dietary intake, serum concentrations, and retinal concentrations of lutein and zeaxanthin in adults in a Midwest population. Am J Clin Nutr. 2001;74:796–802. doi: 10.1093/ajcn/74.6.796. [DOI] [PubMed] [Google Scholar]
- Bone RA, Landrum JT, Cao Y, Howard AN, Alvarez-Calderon F. Macular pigment response to a supplement containing mesozeaxanthin, lutein and zeaxanthin. Nutr Metab. 2007;4:1–8. doi: 10.1186/1743-7075-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond BR, Johnson EJ, Russell RM, Krinsky NI, Yeum KJ, Edwards RB. Dietary modification of human macular pigment density. Invest Ophthal Vis Sci. 1997;38:1795–1801. [PubMed] [Google Scholar]
- Nolan JM, Stack J, O'connell E, Beatty S. The relationships between macular pigment optical density and its constituent carotenoids in diet and serum. Invest Ophthal Vis Sci. 2007;48:571–582. doi: 10.1167/iovs.06-0864. [DOI] [PubMed] [Google Scholar]
- Berendschot TT, Goldbohm RA, Klöpping WA, van de Kraats J, van Norel J, van Norren D. Influence of lutein supplementation on macular pigment, assessed with two objective techniques. Invest Ophthalmol Vis Sci. 2000;41:3322–3326. [PubMed] [Google Scholar]


