Abstract
Introduction
To assess the effect of brow ptosis on visual function and quality-of-life (QoL), and to determine what measures are associated with post-surgical change in functional status.
Methods
Prospective longitudinal study. Fifteen consecutive patients undergoing brow-lift surgery from February 2009 to August 2010. Main outcome measures: pre- and post-operative eyelid position (ie, distance mm from corneal reflex to upper skin fold (FRD1), lowest brow hair to lower limbus (LLB), centre of lower lid to upper lid skin fold (LLF)) and number of points missing in ‘superior' and ‘superior plus elsewhere' Humphrey 120-point visual field, as well as a Quality-of-life and Visual Function questionnaire before and after brow lift surgery.
Results
The strongest correlation between pre-op functional index score and any pre-op objective measure was visual fields (r=−0.46, P<0.085). There was a mean 36-point increase in functional index score after brow lift surgery (P<0.001).
Self-reported preoperative functional impairment was the only outcome measure significantly (and strongly) associated with post-surgical improvement in functional status (r=−0.833, P<0.001).
Conclusions
Surgical repair of brow ptosis results in a measurable increase in health-related QoL. The preoperative QoL score is the best predictor of postoperative improvement in QoL. The best available objective preoperative parameter for indicating postoperative QoL improvement is visual fields. These two measures should be used to better predict successful surgical outcomes.
Keywords: brow ptosis, quality-of-life, brow-lift
Introduction
Current practice in the assessment of brow ptosis usually involves measurement of corneal reflex distance to the lowest brow hair at the centre and two extremities of brow with the patient in the primary position of gaze, and visual field testing.
This limited approach does not account for patients having differing criteria for a successful surgical outcome. Some, typically older patients, seek functional improvement such as a better visual field whereas others may desire an aesthetic enhancement by way of a change in brow position. Furthermore, there is no universally accepted and aesthetically ideal brow shape or position. A successful outcome from any procedure should directly relate to a reduction in, or resolution of, symptoms suffered by the patient.
It is well established that ocular disease has a negative impact on vision-related quality-of-life (QoL).1, 2, 3, 4, 5 In blepharoptosis patients, self-reported preoperative functional impairment is strongly associated with the degree of post-surgical functional improvement.5 There are no reports in the literature of the effect of brow ptosis on QoL and visual function, nor of the correlation between the following parameters of eyebrow position: FRD1 (the distance mm from corneal reflex to upper skin fold); LLB (the distance from lowest brow hair to lower limbus); LLF (the distance from centre of lower lid to upper-lid skin fold), and visual fields, QoL and visual function.
Furthermore, there are no nationally agreed NHS or insurance company criteria for reimbursement of brow lifts. Generally, symptomatic patients have a visual field test and photograph, although there are no universally accepted standards for these.
The aims of this study were the following: to assess the impact of brow ptosis and its repair on vision-related QoL; to investigate the relationships between objective and subjective measures of brow ptosis; and to determine what preoperative parameter can best predict postoperative patient satisfaction and hence, surgical success. In so doing, we wanted to provide a practicable guide for healthcare commissioners, to allow easier identification of patients likely to gain the most benefit from brow lift surgery.
Materials and methods
Fifteen consecutive patients undergoing direct brow lift surgery for functional improvement, from February 2009 to August 2010, were evaluated in this study. Informed consent was obtained from all study subjects and Buckinghamshire Hospitals NHS Trust Research Ethics Committee approved the project. It was undertaken in accordance with the Tenets of Helsinki.
Inclusion criteria were the following: 18 years of age or older; acquired brow ptosis; best corrected visual acuity equal to or better than 6/18 in at least one eye; no prior eyelid or eyebrow surgery; no concomitant ocular pathology; intraocular pressure ≤21 mm Hg; ability to undergo a complete ophthalmic examination including slit-lamp biomicroscopy, and a normal fundal appearance on clinical stereoscopic examination; ability to complete a Humphrey 120-point visual field test and questionnaire before surgery and six-to-eight weeks after surgery; and capacity to give informed consent for the operation and study. Acquired brow ptosis was defined as acquired drooping of the eyebrow/s below the superior orbital rim. Visual acuity was initially recorded in Snellen units, but because the Snellen fraction is not a true mathematical ratio, all Snellen acuity scores were then converted to LogMAR (logarithm of the minimal angle of resolution) units for database inclusion.6, 7 The logarithm of the inverse Snellen fraction approximates the LogMAR.8
Brow position was measured before and at 2 months after surgery from a standard colour photograph of the patient looking in the primary position (ie, distance mm from corneal reflex to upper skin fold (FRD1), lowest brow hair to lower limbus (LLB), centre of lower lid to upper skin fold (LLF)). All patients also underwent visual field testing and completed a Quality-of-life (QoL) and Visual Function questionnaire before and at two months post surgery. The number of points missing on 'superior' (SVF) and 'superior plus elsewhere' (VF) full-field Humphrey 120-point visual field, were recorded in addition to the test reliability indices (namely number of false positives, negatives and fixation losses).
The Quality-of-life and Visual Function (QoLVF) instrument was the same as that used by Federici et al,5 because there have been no previous QoL studies designed specifically for brow lift surgery. This is the closest comparable study even though it is concerned with blepharoptosis not brow ptosis. The instrument has been validated in that it has been found to be feasible and acceptable in terms of time needed to respond, lack of ambiguity and so on, but it is not a proven instrument with known reliability.3, 5 It focusses on activities and symptoms that would potentially be adversely affected by visual field loss associated with brow ptosis. It comprises four main domains: daily activities, current economic status, visual symptoms, and well being. The 12 questions on activities are mainly concerned with core activities of daily living such as reading, watching television, walking without assistance, performing housework and kitchen chores, and hanging or reaching for objects above eye level. The remaining thirteen questions focus on well-being (for example, current energy level and self image), economic status and symptoms such as a heavy feeling or ache around the eyes and having to raise eyebrows to see. It has been described elsewhere.5 Responses were on a scale from one to five, with one indicating no impairment and five indicating severe impairment. If, for reasons other than visual impairment, a patient did not perform an activity, then they did not have to answer (or score) that question, and that item was not included in the scoring. No minimum number of item replies was needed. Informed consent was obtained from each patient. Questions 1 to 25 on the pre- and post-operative instruments are identical, but the last two questions on the postoperative component addressed satisfaction with surgical outcome. This enabled statistical comparison (t-test for paired data). To generate a composite score (a ‘functional index'), the formula was applied to the first 25 questions: functional index=100–25 [(sum of responses/no. of questions answered)−1]. The functional index was then calibrated such that the score ranged from 0 (least function retained) to 100 (most function retained), as described in previous studies.5, 9, 10 Pre- and post-operative instruments were numbered. A staff member not involved in the patients' surgical care administered them with instructions in plain envelopes, allowing confidential completion by patients. The surgeon was blind to the results until all postoperative data had been collected. Database access was restricted to the two authors by means of computer password.
For statistical purposes, and to more accurately reflect binocular function, a single (‘combined') value for the various bilateral measurements was determined, in addition to the individual measurements for each eye. For each category, the better-seeing eye was given a weight of 0.75 and the worse eye was given a weight of 0.25 (this is similar to the method used by Federici et al5 and by Scott et al1). This was done to take into account previous work suggesting a moderate correlation between the ability of a patient to perform vision-dependent activities and the vision of the better seeing eye.11
Statistical analyses
The Pearson correlation co-efficient was used to evaluate relationships between the various measurements, with statistical significance considered at P<0.05.
Data management and parametric statistical work were performed using Microsoft Excel. Non-parametric and regression analysis was performed using Wessa.net (http://www.wessa.net/).
Results
Descriptive statistics
Fifteen adult subjects (10 (67%) female; mean age at presentation, 65 (SD 10.0, range 48–81) years) were studied. Fourteen cases were bilateral and one case was unilateral in a patient with a fellow blind eye.
There was no statistically significant change in visual acuity in either eye, after surgery (right eye, t= −0.375, P>0.5, 95% CI −0.123 to 0.112; left eye, t= −0.141, P>0.5, 95% CI −0.16 to 0.16). One patient was withdrawn from the study as he failed to attend follow-up appointments.
Descriptive statistics for the variables measured in this study are shown in Table 1. Pre-surgical and post-surgical measurements are denoted by the prefixes ‘pre' and ‘post', respectively. The suffixes ‘c' represents the combined eyes for a particular measurement. The postoperative change (difference) is defined as the preoperative value subtracted from the postoperative value, and is denoted by the prefix ‘d'. The preoperative and postoperative functional indices are denoted as pre-IDX and post-IDX, respectively, with the post-surgical difference in index represented as dIDX.
Table 1. Descriptive statistics.
| Variable | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| preSVFc | 23.9 | 14.54 | 0 | 52.5 |
| postSVFc | 5.23 | 8.77 | 0 | 29 |
| dSVFc | 18.67 | 13.25 | −1 | 44.5 |
| preVFc | 31.63 | 24.33 | 0 | 89.5 |
| postVFc | 10.37 | 16.85 | 0 | 54 |
| dVFc | 21.27 | 19.3 | −17.5 | 54.5 |
| preFRD1c | 1.37 | 0.88 | 0 | 2.3 |
| postFRD1c | 6.47 | 1.37 | 3.28 | 8.36 |
| dFRD1c | 4.82 | 1.51 | 1.84 | 7.5 |
| preLLLBc | 16.36 | 3.17 | 10.73 | 20.5 |
| postLLLBc | 18.68 | 2.45 | 16.2 | 22.52 |
| dLLLBc | 2.86 | 2.47 | 0 | 8.59 |
| preLLFc | 7.64 | 1.87 | 4.79 | 10.62 |
| postLLFc | 11.85 | 2.66 | 8 | 17.77 |
| dLLFc | 4.35 | 1.58 | 2.47 | 7.15 |
| preIDX | 50.47 | 14.07 | 16 | 73 |
| postIDX | 86.8 | 8.25 | 69 | 96 |
| dIDX | 36.13 | 15.66 | 10 | 61 |
Abbreviations: SD, standard deviation; Pre, pre-surgical measurement; Post, post-surgical measurement; d, postoperative change (difference); c, combined result of both eyes; IDX, functional index score; SVF, number of points missing in superior visual field; VF, number of points missing in ‘superior plus elsewhere' visual field; FRD1, distance in mm from corneal reflex to upper skin fold; LLB, distance in mm from lowest brow hair to lower limbus; LLF, distance mm from centre of lower lid to upper skin fold.
There was a strong positive correlation between preoperative (superior (SVF) and entire (VF)) visual field and post-surgical change in visual field (r=0.805, P=0.000 and r=0.721, P=0.002 for SVF and entire visual field, respectively), indicating that those with the greater visual field loss may have the greater ‘potential' for improvement in visual field after brow lift surgery. There was no significant correlation between preoperative brow position (preFRD1c, preLLBc, preLLFc) and either the change in the brow position after surgery (dFRD1c, dLLBc and dLLFc) or preoperative SVF or VF. The correlation coefficients (with their statistical significance) between the main variables in the study are presented as Supplementary data.
Functional index score
There was a mean 36-point increase in functional index score after brow lift surgery (P<0.001). Nobody had a reduced QoL score after surgery.
Improvement in QoL after surgery
There was no significant correlation between any preoperative objective measure and improvement in QoL after surgery. Only patients' preoperative subjective functional index score was significantly correlated with postoperative QoL improvement. This was a very strong correlation: r= −0.833, P<0.001. The lower the preoperative functional index score (ie, the worse the perceived QoL), the greater the QoL improvement after surgery (Figures 1 and 2).
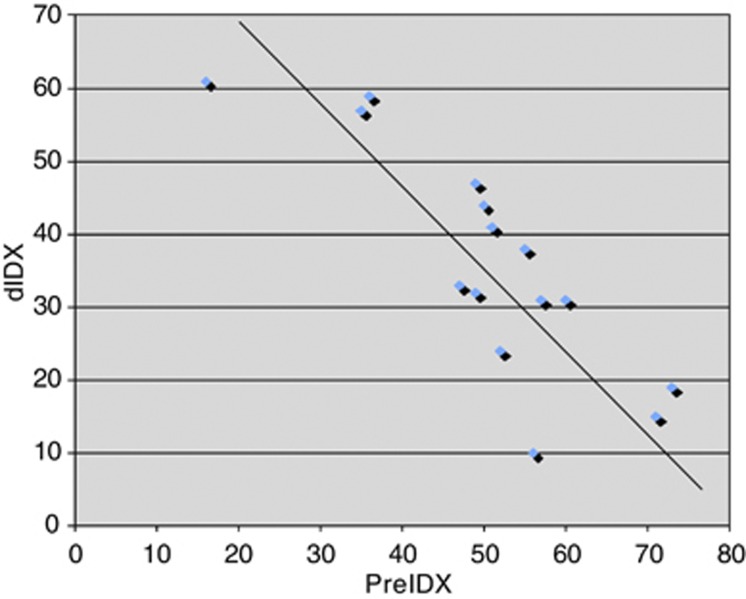
Figure 1.
A chart to show correlation between preoperative QoL (preIDX) and improvement in QoL (dIDX) after surgery. PreIDX, preoperative functional index score; dIDX, change in functional index score after surgery.
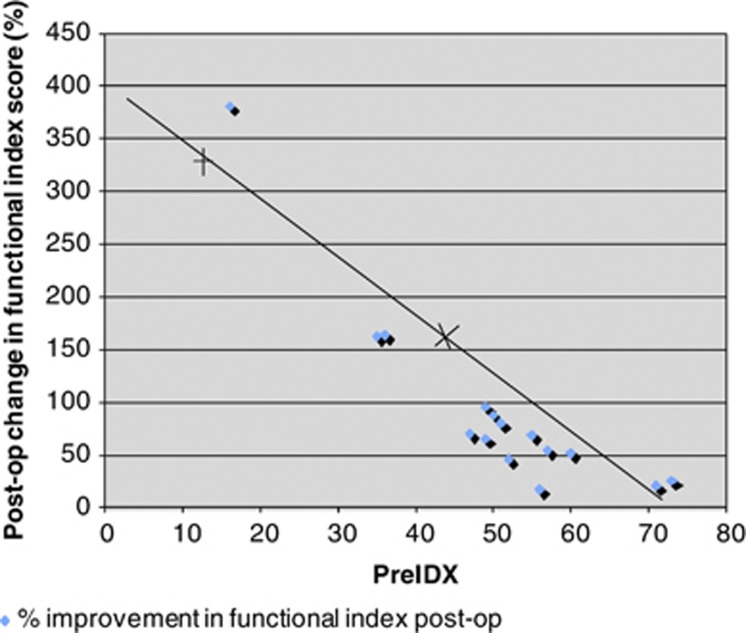
Figure 2.
A chart to show the correlation between preoperative QoL (preIDX) and the percentage improvement in functional status postoperatively. PreIDX, preoperative functional index score.
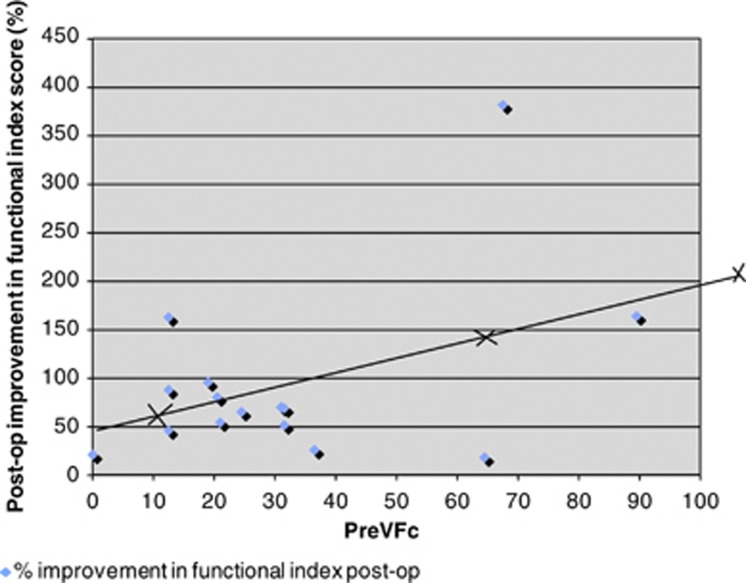
The strongest correlation between pre-op functional index score and any pre-op objective measure was with visual fields although this did not reach statistical significance (entire visual field, r= −0.46, P<0.085; superior visual field, r= −0.477, P<0.072). The visual field was the preoperative objective measure that correlated the most with postoperative percentage improvement in functional index: the greater the number of missing points on the visual field before surgery, that is, the higher the preVFc, the greater the percentage improvement in functional status after surgery (Figure 3). However, this association also failed to reach significance (r=0.462, P<0.1).
Figure 3.
A chart to show the relationship between preoperative visual field (PreVFc) and postoperative percentage improvement in functional index score. PreVFc=Mean (weighted average of both eyes) number of points missing in preoperative visual field (entire visual field).
All of the completed individual paired items on the instrument showed statistically significant (P<0.05) improvement except for question 3 (walking without assistance). Table 2a and Table 2b show the mean pre- and post-op scores and mean change in score for each activity and symptom. Nine activity and eight symptom items showed a change greater than one unit. Fine manual work was the activity showing greatest improvement after surgery (mean postoperative change 2.07, t= 5.766, P<0.001). The symptoms improving the most after surgery were ‘eyelids/eyebrows getting in the way of vision' (mean postoperative change 3.00, t=12.50, P<0.001) and ‘having to raise the eyebrows to see' (mean postoperative change=2.53, t= 8.664, P<0.001). According to question 26, all patients felt that their brow lift surgery was worthwhile and 93% (13/14) would recommend surgery to a friend or relative with a similar condition.
Table 2a. Mean pre- and postoperative scores and postoperative change for each activity.
| Activity | Number of responses | Mean pre-op score (SD) | Mean post-op score (SD) | Mean post-op change | t-test | P-value |
|---|---|---|---|---|---|---|
| Reading | 15 | 2.87 (1.51) | 1.07 (0.26) | 1.80 | 4.592 | <0.001 |
| Watching TV | 15 | 2.87 (1.13) | 1.07 (0.26) | 1.80 | 6.061 | <0.001 |
| Walking without assistance | 15 | 1.40 (0.83) | 1.00 (0.00) | 0.40 | 1.869 | <0.10 |
| Playing sport | 13 | 2.92 (1.19) | 1.21 (0.58) | 1.69 | 4.870 | <0.001 |
| Fine manual work | 15 | 3.37 (1.06) | 1.40 (0.63) | 2.07 | 5.766 | <0.001 |
| Working with a computer | 14 | 3.21 (0.97) | 1.20 (0.41) | 2.00 | 6.734 | <0.001 |
| Performing housework and kitchen chores | 14 | 2.57 (1.09) | 1.07 (0.26) | 1.50 | 5.155 | <0.001 |
| Reading road signs above or seeing traffic lights | 14 | 2.47 (1.36) | 1.21 (0.58) | 1.36 | 3.666 | <0.01 |
| Reading signs at side of road while driving | 15 | 2.60 (1.59) | 1.33 (0.49) | 0.13 | 2.947 | <0.02 |
| Performing occupation | 12 | 2.33 (1.30) | 1.27 (0.46) | 1.00 | 3.067 | <0.01 |
| Hanging or reaching objects above | 13 | 2.79 (1.31) | 1.21 (0.43) | 1.69 | 4.092 | <0.01 |
| Other | 8 | 2.75 (1.04) | 1.33 (0.65) | 1.25 | 3.049 | <0.02 |
Table 2b. Mean pre- and postoperative scores and postoperative change for each symptom.
| Symptom | Number of responses | Mean pre-op score (SD) | Mean post-op score (SD) | Mean post-op change | t-test | P-value |
|---|---|---|---|---|---|---|
| Current vision | 15 | 3.07 (0.8) | 1.80 (0.56) | 1.27 | 4.774 | <0.001 |
| Current upper visual field | 15 | 3.87 (0.74) | 1.60 (0.63) | 2.20 | 8.429 | <0.001 |
| General level of health | 15 | 2.13 (0.64) | 1.87 (0.74) | 0.27 | 2.269 | <0.05 |
| Current energy level | 15 | 2.67 (0.90) | 2.33 (0.82) | 0.33 | 2.598 | <0.05 |
| Current general well-being | 15 | 2.27 (0.80) | 1.93 (0.70) | 0.33 | 2.598 | <0.05 |
| Current self-image | 15 | 2.73 (0.96) | 1.93 (0.46) | 0.80 | 3.292 | <0.01 |
| Current eye/eyelid/eyebrow appearance | 15 | 4.21 (0.80) | 1.80 (0.86) | 2.40 | 6.877 | <0.001 |
| Current economic status | 15 | 3.00 (0.85) | 2.53 (1.06) | 0.47 | 2.196 | <0.05 |
| Keeping chin in head-up position | 15 | 3.53 (0.83) | 2.43 (1.34) | 1.20 | 3.061 | <0.001 |
| Eyelids/eyebrows getting in way of vision | 15 | 4.20 (0.77) | 1.20 (0.41) | 3.00 | 12.50 | <0.001 |
| Having to raise eyebrows to see | 15 | 3.67 (1.11) | 1.13 (0.35) | 2.53 | 8.664 | <0.001 |
| Heavy feeling or ache around the eyes | 15 | 3.60 (1.40) | 1.47 (0.64) | 2.13 | 6.068 | <0.001 |
| Tearing, redness, burning, dryness of eyes | 15 | 3.13 (1.30) | 1.80 (0.94) | 1.33 | 4.182 | <0.001 |
Discussion
To date, there are no other reports in the literature, to our knowledge, concerning the effect of brow ptosis on QoL and visual function, nor of the correlation between the parameters of eyebrow position, visual fields, and QoL and visual function in patients with brow ptosis. There are only four published studies specifically concerning the effect of blepharoptosis on QoL and visual function.3, 5, 12, 13
We have shown that brow ptosis repair results in a measurable increase in health-related QoL. This is in keeping with other reports of patients with ophthalmic disease who are known to be at ‘high risk for reduced functional status/quality-of-life'.1 Improvement in vision after cataract surgery, penetrating keratoplasty or blepharoptosis surgery, for example, is associated with enhanced functional status.1, 4, 13, 14, 15
In this study, we calculated a functional index score, which examined a ‘weighted combined eye' visual function. This is considered a more accurate measure of binocular function. The change in functional index was calculated to assess the alteration in functional status after surgery and to evaluate the relationship between objective measures and the patients' perception of functional status and QoL.
Assessment of functional status is important. Clinical measures may objectively determine disease severity but they may fail to address more subjective aspects of pathology such as impact on daily life and general well being, for example, two patients may have the same degree of brow ptosis but differ in their individual response to it.15, 16, 17
Self-reported functional impairment is the only preoperative parameter significantly (and strongly) associated with postoperative improvement in functional status, for example, a preoperative functional index score of 50 correlates to a 125% improvement in functional index score postoperatively (Figure 2). This result is keeping with a study of blepharoptosis repair by Federici et al,5 who found that the parameter, most strongly associated with a change in functional status after surgery (dIDX), was patients' self-reported preoperative functional status, preIDX (r=−0.79, P<0.001). Patients with the worst functional index before surgery have the greatest improvement in QoL after surgery. These results are also consistent with reports on cataract surgery outcomes.1, 11
This study has shown a trend in visual field loss associated with brow ptosis, although this was not found to be statistically significant. Other studies have reported impaired visual field in blepharoptosis, with greater visual field loss being attributed to worse ptosis.3, 5 Visual impairment reduces QoL.18, 19 As such, it is reasonable to expect brow ptosis to have a negative effect on QoL, and corrective surgery to address this. In this study, we did not test visual fields after taping or manually elevating the eyelid because the results of the Federici study showed that taped/manually elevated VF measurements were not predictive of improvement in function after surgery.5 We have shown an enhancement in both visual field (mean dSVFc=18.7, SD 13.3; mean dVFc= 21.3, SD 19.3) and health-related QoL after brow lift surgery (although correlation of these two factors did not reach statistical significance). This is in line with previous studies of blepharoptosis repair.5
The best available objective preoperative parameter for predicting extent of postoperative QoL improvement is visual fields, as evidenced by the relationship between pre-operative visual fields and postoperative percentage improvement in functional index score (r=0.462, P<0.1). In their study of 97 patients (194 eyes) undergoing blepharoplasty and/or ptosis repair, Ho et al recently proposed the use of a modified HVF (the ‘Leicester Peripheral Visual Field test') and specified a visual field defect to help guide decision making for ptosis surgery.20 They considered that patients with certain visual field defects (namely 3 contiguous points missed up to 48 degrees) would benefit from intervention. (Interestingly, they also reported a false positive rate of 7.5% with this methodology). They advocate the use of QoL instruments as an adjunct to visual field testing in cases where no significant defect has been detected on visual field testing. Given our findings, however, namely the relative importance of the preoperative functional index score and the lack of a statistically significant correlation between preoperative visual field and patients' subjective impression of surgical success (by way of improved postoperative functional status), we would instead advise assessing both parameters in all patients before surgery. Furthermore, we recommend that more weight be given to a patient's opinion of symptom severity than to a visual field test. The negative relationship between pre-op QoL score (preIDX) and pre-op visual fields (preVFc) (r=−0.46, P<0.085) counters concerns regarding potential exaggeration of symptoms by patients.
The main limitation of our study is that it involves relatively small numbers. We accept that this may account for the failure of any correlation between any preoperative objective measure (eg, visual fields) and either preoperative IDX or postoperative change in functional index to reach statistical significance. We chose our Quality-of-life and Visual Function instrument primarily to allow comparison with the nearest available study, namely that by Federici et al5 on blepharoptosis. It has been used in other similar studies, and is quick and easy to complete and has relevant questions similar to those used by the ophthalmologist in history-taking.3, 5 There is currently no universally accepted ‘gold-standard' instrument specifically concerning vision and functional impairment in this subset of patients. Despite being one of the most widely used of the visual function instruments, even the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25) is still not applicable to all patient subsets.21
In summary, this study has demonstrated that surgical correction of brow ptosis results in a measurable increase in health-related QoL. It has also shown that self-reported preoperative functional impairment is the only outcome measure significantly (and strongly) associated with postoperative increase in functional status, and that visual fields are the best available preoperative objective measure for estimating the expected extent of such improvement.
In the context of the current economic climate with a growing population, increasing healthcare demands and tighter control of healthcare budgets, the funding of certain oculoplastic procedures such as blepharoptosis and brow ptosis repair is coming under increased scrutiny. Healthcare commissioners are under greater pressure than ever to allocate limited resources in the most efficacious way. As such, we recommend assessing the subjective impact of brow ptosis and specifically asking the patient whether their eyelids or eyebrows get in the way of their vision and how much they feel they have to raise the eyebrows to see, as these are the symptoms that we have shown improved the most, after surgery. We advocate the use of the preoperative functional index score (in addition to a formal visual field test) as a practicable measure for healthcare commissioners, to guide decisions as to who would benefit most from surgery and who should be entitled to treatment. Eligibility for surgery may be determined by setting an arbitrary threshold level, for example, a pre-op score of 40 or less. This would correlate to 175% or more improvement in post-op QoL score. The threshold could then be revised in line with changes in available funding.
Conclusion
The preoperative functional index score is a key determinant of postoperative improvement in QoL and visual function. It should be used as a tool to guide decisions for reimbursement of brow lift surgery by Primary Care Trusts and medical insurers.
Acknowledgments
We thank Miss Emily Fletcher for her assistance with patient recruitment and data collection.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on Eye website (http://www.nature.com/eye)
This work was presented at the BOPSS (British Oculoplastic Surgery Society) Annual Meeting, Cardiff, Wales, June 2011, and ESOPRS (European Society of Oculoplastic and Reconstructive Surgery) Annual Meeting, Lake Como, Italy, September 2011.
Supplementary Material
References
- Scott IU, Schein OD, West S, Bandeen-Roche K, Enger C, Folstein MF. Functional status and quality of life measurement among ophthalmic patients. Arch Ophthalmol. 1994;112:329–335. doi: 10.1001/archopht.1994.01090150059023. [DOI] [PubMed] [Google Scholar]
- Lee PP, Spritzer K, Hays RD. The impact of blurred vision on functioning and well-being. Ophthalmology. 1997;104:390–396. doi: 10.1016/s0161-6420(97)30303-0. [DOI] [PubMed] [Google Scholar]
- Battu VK, Meyer DR, Wobig JL. Improvement in subjective visual function and of life outcome measures after blepharoptosis surgery. Am J Ophthalmol. 1996;121:677–686. doi: 10.1016/s0002-9394(14)70634-8. [DOI] [PubMed] [Google Scholar]
- Mangione CM, Philips RS, Lawrence MG, Seddon JM, Orav EJ, Goldman L. Improved visual function and attenuation of declines in health-related quality of life after cataract extraction. Arch Ophthalmol. 1994;112:1419–1425. doi: 10.1001/archopht.1994.01090230033017. [DOI] [PubMed] [Google Scholar]
- Federici TJ, Meyer DR, Lininger LL, Bartley GB. Correlation of the vision-related functional impairment associated with blepharoptosis and the impact of blepharoptosis surgery. Ophthalmology. 1999;106 (9:1705–1712. doi: 10.1016/S0161-6420(99)90354-8. [DOI] [PubMed] [Google Scholar]
- Cassard SD, Patrick DL, Daminano AM, Legro MW, Tielsch JM, Diener-West M, et al. Reproducibility and responsiveness of the VF-14. An index of functional impairment in patients with cataracts. Arch Ophthalmol. 1995;113:1508–1513. doi: 10.1001/archopht.1995.01100120038005. [DOI] [PubMed] [Google Scholar]
- Spaeth EB, Fralick FB, Hughes WF. Estimation of loss of visual efficiency. Arch Ophthalmol. 1955;54:462–468. doi: 10.1001/archopht.1955.00930020468021. [DOI] [PubMed] [Google Scholar]
- Ferris FL, Kassof A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–96. [PubMed] [Google Scholar]
- Mangione CM, Philips RS, Seddon JM, Lawrence MG, Cook EF, Dailey R, et al. Development of the ‘Activities of daily vision scale' measure of visual functional status. Med Care. 1992;30:1111–1126. doi: 10.1097/00005650-199212000-00004. [DOI] [PubMed] [Google Scholar]
- Fletcher AE, Ellwein LB, Selvaraj S, Vijaykumar V, Rahmathullah R, Thulasiraj RD. Measurements of visual function and quality of life in patients with cataracts in southern India. Report of instrument development. Arch Ophthalmol. 1997;115:767–774. doi: 10.1001/archopht.1997.01100150769013. [DOI] [PubMed] [Google Scholar]
- Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–638. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- Asano ME, Osaki MH. Quality of life assessment in patients with blepharoptosis. Arq Bras Oftalmol. 2006;69 (4:545–549. doi: 10.1590/s0004-27492006000400016. [DOI] [PubMed] [Google Scholar]
- Cahill KV, Bradley EA, Meyer DR, Custer PL, Holck DE, Marcet MM, et al. Functional indications for upper lid ptosis and blepharoplasty surgery a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118 (12:2510–2517. doi: 10.1016/j.ophtha.2011.09.029. [DOI] [PubMed] [Google Scholar]
- Mendes F, Schaumberg DA, Navon S, Steinert R, Sugar J, Holland EJ, et al. Assessment of visual function after corneal transplantation: the quality of life and psychometric assessment after corneal transplantation (Q-PACT) study. Am J Ophthalmol. 2003;135 (6:785–793. doi: 10.1016/s0002-9394(02)02278-x. [DOI] [PubMed] [Google Scholar]
- Hornberger J, Lernert LA. Variation among quality-of-life surveys. Theory and practice. Med Care. 1996;34 (12 Suppl:DS23–DS33. [PubMed] [Google Scholar]
- Calman KC. Quality of life in cancer patients-an hypothesis. J Med Ethics. 1984;10:124–127. doi: 10.1136/jme.10.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- Kempen GI, Ballemans J, Ranchor AV, van Rens GH, Zijlstra GA.The impact of low vision on activities of daily living, symptoms of depression, feelings of anxiety and social support in community-living older adults seeking vision rehabilitation services Qual Life Res 2011. e-pub ahead of print 17 November 2011; doi: 10.1007/s11136-011-0061-y [DOI] [PMC free article] [PubMed]
- Brown RL, Barrett AE. Visual impairment and quality of life among older adults: an examination of explanations for the relationship. J Gerontol B Psychol Sci Soc Sci. 2011;66 (3:364–373. doi: 10.1093/geronb/gbr015. [DOI] [PubMed] [Google Scholar]
- Ho SF, Morawski A, Sampath R, Burns J. Modified visual field test for ptosis surgery (Leicester Peripheral Field Test) Eye. 2011;25:365–369. doi: 10.1038/eye.2010.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marella M, Pesudovs K, Keefe JE, O'Connor PM, Rees G, Lamoureux EL. The psychometric validity of the NEI VFQ-25 for use in a low-vision population. Invest Ophthalmol Vis Sci. 2010;51 (6:2878–284. doi: 10.1167/iovs.09-4494. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.