Abstract
Background In the USA, different standards are usually set for spirometric values in African-American and white populations. It is unclear to what extent the lower lung function found in African-Americans is ‘normal’ in the sense of having no adverse consequences.
Methods African-American and white participants in the Atherosclerosis Risk in Communities (ARIC) limited access data set, from four communities in the USA had spirometric testing at baseline beginning in 1986 and were followed up to assess survival to the end of 2002.
Results Forced Expiratory Volume in 1 s (FEV1) and Forced Vital Capacity (FVC) were lower in the African-American than the white sample both for men and women and adjustment for potential confounders had little effect on the estimated difference {difference in FVC after adjustment: men, −0.68 l [95% confidence interval (95% CI) −0.75 to −0.61]; women, −0.41 l (95%CI −0.45 to −0.36)}. The FEV1/FVC ratio was slightly greater among African-American than white participants [difference: men, 1.5% (95%CI 0.7–2.1); women, 1.7% (95%CI 1.1–2.2)]. After adjustment for age and height, survival was similar in each ethnic group for any given level of FVC before and after adjustment for potential confounders. The hazard ratio for African-American compared with white participants was 1.24 for men (95% CI 0.91–1.69) and 0.96 for women (95% CI 0.66–1.38).
Conclusions A given FVC has the same prognostic significance for ‘normal’ African-American and white participants. It is inappropriate to use ethnic norms when assessing prognosis.
Keywords: Mortality, African-Americans, European Continental Ancestry Group, vital capacity, Forced Expiratory Volume
Introduction
It is usual practice to provide separate standards of ventilatory function for different ethnic and racial groups.1 The basis for this is the observed difference in lung volumes between representative samples of asymptomatic non-smoking individuals. The assumption is that the lower lung function of some ethnic minorities measured under these conditions is constitutional and not pathological. However, symptoms are a poor predictor of lung function2 and smoking explains only a small part of the variation in lung function.3 Other important predictors of lung function are strongly related to social conditions in early life4,5 and are very likely to confound any association with ethnicity. More recently, Chinn et al.6 have provided an alternative method for deciding which norms for ventilatory function are more appropriate by assessing the strength of their association with future prognosis.
Assumptions about the ‘normality’ of these differences have important implications for the assessment of lung disease in individuals and populations. This is particularly so when assessing international variations in disease, but is also important in the many populations that are increasingly of mixed ethnicity. We have therefore used the Atherosclerosis Risk in Communities (ARIC) study7 to measure the extent to which lung function has a different prognostic implication in white and African-American participants.
Materials and Methods
Participants in the ARIC Study were drawn from the general population of four American communities, Forsyth County, North Carolina, Jackson Mississippi, the north western suburbs of Minneapolis, Minnesota and Washington County, Maryland. In Jackson, only African-Americans were included in the sample. In total, 4000 participants were to be selected from each centre, in the age group of 45–64 years.6
The protocol was ambitious and mainly aimed at identifying potential risk factors for cardiovascular disease. Importantly from the point of view of this analysis, the participants had their ventilatory function assessed by spirometry.8 The Forced Expiratory Volume in 1 s (FEV1) and Forced Vital Capacity (FVC) were measured using a volume-displacement water-sealed spirometer. From a minimum of five forced expiratory manoeuvres, at least three acceptable blows were required and the best of these selected according to the contemporary American Thoracic Society (ATS) guidance.9,10 Quality control was managed from a central monitoring service at Johns Hopkins University.8 Subjects were followed up over the following years with annual telephone questionnaires and using community-wide surveillance procedures based on the National Heart Lung Blood Institute Community Cardiovascular Surveillance Program (CCSP).7 Any deaths were noted.
The limited access data set includes those participants in the ARIC cohort who gave informed consent for their data to be used in this way, and in some instances has small subgroups recoded to preserve anonymity. We analysed only individuals who were asymptomatic at baseline (excluding those reporting persistent cough or phlegm, wheeze, breathlessness or doctor-diagnosed asthma, chronic bronchitis or emphysema), who had usable spirometry (at least two reproducible manoeuvres out of at least three judged to be acceptable), and who had complete data on a number of variables that potentially confounded the associations of lung function and ethnic group with mortality.
Ethnic group was divided into black and non-black in the limited access dataset. The non-black population in the ARIC study was 99.6% white, 0.3% Asian and 0.1% American or Alaskan Indian.11 To be consistent with National Health and Nutrition Examination Survey (NHANES) and other large surveys, we refer to the black population as African-American and the non-black population as white. Baseline differences between characteristics of African-American and white participants were assessed using t-tests and chi-squared tests, looking at men and women separately. The differences between mean FEV1, FVC and FEV1/FVC ratio in African-American and white participants were further adjusted for other covariates using multivariable linear regression.
We modelled the effects of FVC and ethnic group on overall mortality using Cox regression, adjusting for baseline age, height, body mass index (BMI), waist–hip ratio, sitting height, income category, current working status, most recent occupation, ever smoked, current smoking, pack-years of smoking, education level and systolic blood pressure. All these variables were selected because they could be associated with ethnicity, ventilatory function and/or mortality rate. We also looked at what happened if we included quadratic effects of the continuous variables age, height, BMI, waist–hip ratio, sitting height, pack-years and systolic blood pressure. We concluded that linear effects provided a good fit to the data for all the continuously-scaled variables except for systolic blood pressure, which we divided into quintiles (calculated separately for men and women). We have focused on vital capacity in this article because we had previously shown that vital capacity, rather than FEV1 or the FEV1/FVC ratio, is the main predictor of survival in the ‘normal’ population.12
Three different models were considered, using, respectively, raw FVC, FVC% predicted from NHANES white reference equations for all participants1 and FVC% predicted from NHANES African-American equations for African-American participants and white equations for white participants. In each case, the FVC variable was log-transformed, and the effect is reported as a hazard ratio (HR) per 10% increase. Taking logarithms of FVC and FVC% predicted produced better fitting models and made more conceptual sense in linear regression models because the two log values are linearly related.
To illustrate the association, we drew graphs of mortality against FVC% predicted (divided into quintiles), in African-American and white men and women. These analyses are stratified by ethnic group and make no prior assumption about the form of the relationship between FVC% predicted and mortality. In order to estimate absolute mortality rates at baseline (rather than just HRs), we used a fully-parametric Gompertz regression model (we noted little difference between effects estimated with Gompertz regression and with the semi-parametric, Cox regression model used for our main analyses). Mortality rates were adjusted for age and height. For illustration, we plotted mortality at age 55 years, and at a typical height (175 cm for men and 165 cm for women). Underneath the mortality curves, we drew the distribution of FVC% predicted in our cohort, shown as a density estimate obtained with the ‘kdensity’ command in Stata, using an Epanechnikov kernel and an optimal bandwidth for a normal distribution.13
All analyses were done with Stata 11 (Stata Corp, TX, USA).
The ARIC study was approved by local institutional review boards in the USA, and our analysis was approved by the Imperial College Research Ethics Committee.
Results
The study began in 1986 and recruited 15 792 participants. Of them, 15 732 gave permission for their data to be included in the ARIC limited access dataset. In total, 11 106 people were asymptomatic, 7631 of them had usable spirometry and 7489 of them had complete data. The limited access data set includes outcomes up until Dec 31, 2002 up to which time there were 792 deaths recorded over 102 576 person-years of follow-up.
The characteristics of asymptomatic individuals with usable spirometry and complete data are given in Table 1. The African-American men were younger with higher BMI and lower waist–hip ratio and shorter sitting height compared with the white men. The African-American women were significantly younger, taller, heavier, with higher waist/hip ratios and shorter sitting height compared with the white women. African-American participants of both sexes had significantly lower income, lower educational level and lower occupational group, were more likely to be current smokers but had smoked fewer pack-years and had higher systolic blood pressure. Both FEV1 and FVC were substantially lower in the African-American sample, as expected. The FEV1/FVC ratio, however, was lower in the white group indicating greater obstruction.
Table 1.
Baseline characteristics of asymptomatic individuals with usable spirometry and complete data [values are mean (SD) or percentage]
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| Characteristics | African- American (n = 578) | White (n = 2929) | P-value | African- American (n = 786) | White (n = 3196) | P-value |
| Age (years) | 53.2 (5.9) | 54.3 (5.7) | <0.001a | 52.7 (5.5) | 53.7 (5.6) | <0.001a |
| Height (cm) | 176.1 (6.6) | 176.4 (6.4) | 0.30a | 163.5 (5.8) | 162.2 (5.9) | <0.001a |
| BMI (kg/m2) | 27.9 (4.6) | 27.4 (3.7) | 0.009a | 30.1 (5.8) | 26.2 (5.1) | <0.001a |
| Waist–hip ratio | 0.94 (0.05) | 0.96 (0.05) | <0.001a | 0.89 (0.08) | 0.88 (0.08) | <0.001a |
| Sitting height (cm) | 89.9 (3.3) | 92.9 (3.3) | <0.001a | 84.6 (3.2) | 86.5 (3.2) | <0.001a |
| Income (%) | <0.001b | <0.001b | ||||
| <$16 000 | 29.9 | 6.3 | 42.0 | 11.7 | ||
| $16 000–$35 000 | 34.6 | 27.6 | 31.9 | 33.0 | ||
| >$35 000 | 25.1 | 62.9 | 15.6 | 50.2 | ||
| Not reported | 10.4 | 3.2 | 10.4 | 5.1 | ||
| Working status (%) | <0.001b | <0.001b | ||||
| Homemakerc | 12.2 | 23.7 | ||||
| Employed | 80.1 | 79.1 | 77.1 | 64.7 | ||
| Unemployed | 3.6 | 1.3 | 2.3 | 2.0 | ||
| Retired | 16.3 | 19.6 | 8.4 | 9.7 | ||
| Most recent occupation (%) | <0.001b | <0.001b | ||||
| Managerial/ professional specialty, or retired | 41.0 | 53.1 | 45.3 | 54.3 | ||
| Technical/ sales/ admin support | 9.2 | 18.6 | 16.2 | 30.2 | ||
| Service occupations | 9.2 | 2.8 | 26.5 | 8.4 | ||
| Precision production/ craft/ repair | 15.6 | 14.5 | 0.0 | 1.5 | ||
| Operators/ fabricators/ laborers | 22.7 | 9.6 | 9.9 | 5.3 | ||
| Missing/other | 2.4 | 1.3 | 2.2 | 0.3 | ||
| Ever smoked (%) | 67.5 | 67.8 | 0.88b | 41.7 | 44.1 | 0.23b |
| Current smoker (%) | 33.6 | 17.5 | <0.001b | 23.9 | 18.3 | <0.001b |
| Pack-years of smoking (if ever smoked) | 22.6 (18.9) | 29.2 (21.8) | <0.001a | 15.7 (13.5) | 19.7 (16.5) | <0.001a |
| Education (%) | <0.001b | <0.001b | ||||
| Grade school | 18.0 | 4.7 | 10.3 | 2.9 | ||
| High school—did not graduate | 17.5 | 9.1 | 18.8 | 9.6 | ||
| High school graduate | 21.1 | 28.3 | 23.0 | 43.1 | ||
| Vocational school | 6.4 | 10.0 | 8.4 | 8.4 | ||
| College | 20.1 | 33.3 | 21.4 | 29.4 | ||
| Grad/professional school | 17.0 | 14.6 | 18.1 | 6.7 | ||
| Systolic blood pressure | 129.3 (20.3) | 119.4 (15.7) | <0.001a | 126.6 (20.5) | 116.3 (17.2) | <0.001a |
| FEV1 (l) | 3.10 (0.56) | 3.56 (0.65) | <0.001a | 2.34 (0.41) | 2.60 (0.44) | <0.001a |
| FVC (l) | 4.09 (0.64) | 4.82 (0.77) | <0.001a | 3.00 (0.51) | 3.45 (0.53) | <0.001a |
| FEV1/FVC | 76.0% (6.8) | 73.9% (6.6) | <0.001a | 78.0% (6.1) | 75.5% (5.7) | <0.001a |
aFrom t-test.
bFrom chi-squared test.
cIn the data set, male subjects who reported they were homemakers were given a missing value for current working status to help preserve anonymity. Since these participants could not be identified, they were not included in the analysis.
Table 2 shows clear differences in ventilatory function between ethnic groups and the effect of adjusting for a list of available anthropometric and social variables. The effects of these adjustments, displayed as differences between rows in Table 2 are negligible, except in the case of the FEV1/FVC ratio, where the advantage seen for African-American participants is somewhat diminished, but still significant for both men and women after adjustment.
Table 2.
Effect of sequential adjustment for potential confounders on ethnic differences (Δ) (African-American–white) in spirometric values
| Variable | FEV1 Δ (l) (95% CI) | FVC Δ (l) (95% CI) | FEV1/FVC Δ (%) (95% CI) |
|---|---|---|---|
| Men | |||
| − | −0.46 (−0.51 to −0.40) | −0.73 (−0.80 to −0.66) | 2.1 (1.5 to 2.7) |
| + age, height | −0.49 (−0.53 to −0.44) | −0.75 (−0.80 to −0.70) | 1.8 (1.2 to 2.3) |
| + sitting height | −0.44 (−0.49 to −0.39) | −0.69 (−0.75 to −0.63) | 1.9 (1.2 to 2.5) |
| + waist–hip ratio, BMI | −0.51 (−0.57 to −0.46) | −0.73 (−0.80 to −0.67) | 1.0 (0.3 to 1.7) |
| + ever smoked, current smoker, pack-years | −0.48 (−0.54 to −0.43) | −0.71 (−0.77 to −0.65) | 1.2 (0.5 to 1.9) |
| + income, working status, most recent occupation, education | −0.45 (−0.50 to −0.39) | −0.68 (−0.75 to −0.61) | 1.5 (0.7 to 2.1) |
| Women | |||
| − | −0.27 (−0.30 to −0.23) | −0.44 (−0.49 to −0.40) | 2.5 (2.0 to 2.9) |
| + age, height | −0.33 (−0.36 to −0.30) | −0.53 (−0.56 to −0.49) | 2.4 (2.0 to 2.8) |
| + sitting height | −0.29 (−0.32 to −0.25) | −0.47 (−0.51 to −0.43) | 2.4 (1.9 to 2.8) |
| + waist–hip ratio, BMI | −0.29 (−0.32 to −0.25) | −0.43 (−0.46 to −0.39) | 1.3 (0.8 to 1.8) |
| + ever smoked, current smoker, pack-years | −0.27 (−0.30 to −0.24) | −0.41 (−0.45 to −0.37) | 1.5 (1.8 to 2.7) |
| + income, working status, most recent occupation, education | −0.26 (−0.30 to −0.22) | −0.41 (−0.45 to −0.36) | 1.7 (1.1 to 2.2) |
Δ, difference.
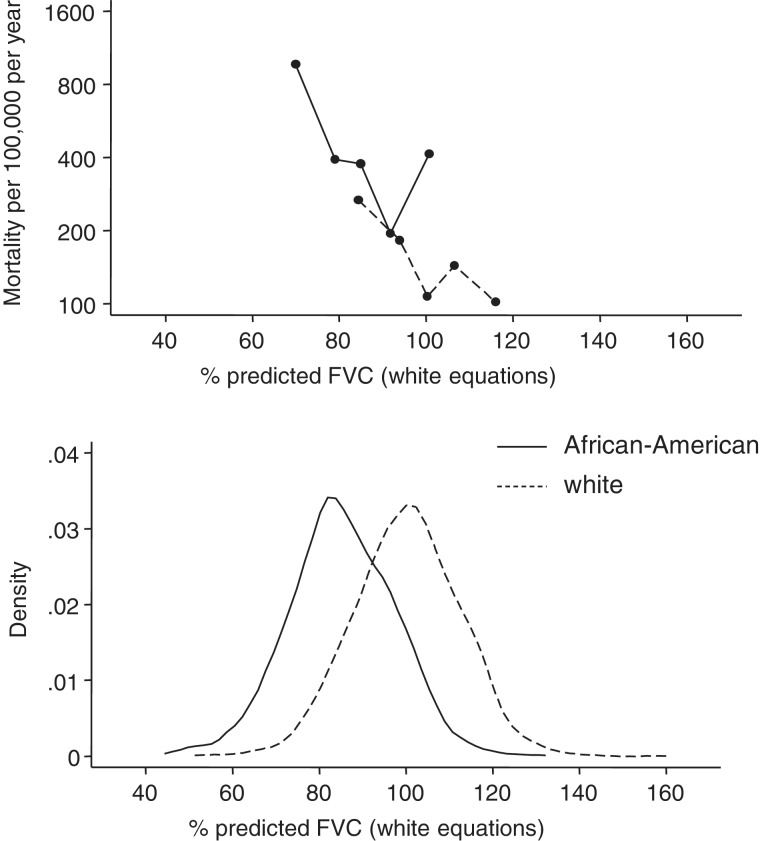
Figure 1 shows in the lower panel the distribution of FVC in white and African-American women as a percentage of the predicted value for white participants in the NHANES survey. The lower distribution of values in the African-American women is apparent. The upper panel displays the mortality rates in subjects with the corresponding FVC at baseline. For both African-American and white women, mortality falls more or less linearly on a logarithmic scale as FVC increases, though the decline in mortality may flatten out at higher levels of FVC. For any FVC% predicted, the mortality is approximately the same for both ethnic groups. Table 3 gives the same information in terms of regression coefficients and for three different models. The first set of results use no explicit external norm but effectively adjust the FVC internally by adjusting for the variables in Table 1 (including age and height). The second set of results use FVC% predicted from age and height using white reference equations, in addition to including height and age independently in the model. Not surprisingly, these results are virtually identical to the first set, since age and height are already included in the model. For every 10% increase in FVC, mortality falls by 11% (HR = 0.89, 95% CI 0.83–0.94) in men and by 17% in women (HR = 0.83, 95% CI 0.77–0.89). After adjusting for FVC, the mortality is 4% lower in the African-American women than in the white women (HR = 0.96, 95% CI 0.66–1.38). This difference is not statistically significant.
Figure 1.
Distribution of percent predicted FVC and its relationship with mortality, in African-American and white women, using white reference equations from NHANES
Table 3.
Effects on mortality of FVC and ethnic groupa
| Men |
Women |
|||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | P-value | HR | (95% CI) | P-value | |
| Model 1 | ||||||
| FVCb | 0.89 | (0.83–0.94) | <0.001 | 0.83 | (0.77–0.89) | <0.001 |
| African-American vs white | 1.24 | (0.91–1.69) | 0.17 | 0.96 | (0.66–1.38) | 0.81 |
| Model 2 | ||||||
| FVC% predicted from white equationsb | 0.89 | (0.83–0.94) | <0.001 | 0.83 | (0.77–0.89) | <0.001 |
| African-American vs white | 1.24 | (0.91–1.69) | 0.17 | 0.95 | (0.66–1.38) | 0.80 |
| Model 3 | ||||||
| FVC% predicted from ethnically specific equationsb | 0.89 | (0.83–0.94) | <0.001 | 0.83 | (0.77–0.89) | <0.001 |
| African-American vs white | 1.56 | (1.15–2.10) | 0.004 | 1.44 | (1.01–2.07) | 0.046 |
aEffects are mutually adjusted and also adjusted for the variables in Table 1 (excluding lung function measures).
bEffect per 10% increase.
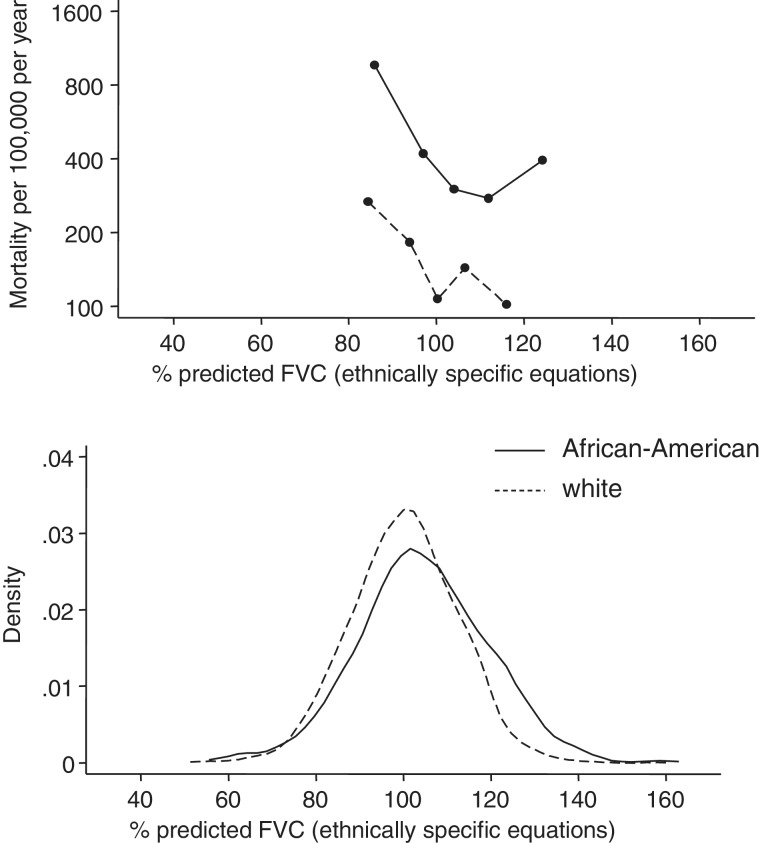
Figure 2 shows in the lower panel the distribution of FVC in white and African-American women as a percentage of the predicted value for white and African-American participants in the NHANES survey, respectively. Both distributions are centred on 100%, and have similar dispersion. However, the mortality among African-American women is higher at any given value of FVC% predicted than among white women. This is also shown in the third set of results in Table 3. After adjusting for FVC% predicted from ethnically specific reference equations, mortality is now 44% higher (HR = 1.44, 95% CI 1.01–2.07) in African-American women than in white women (P = 0.046), though the association between mortality and FVC has not changed.
Figure 2.
Distribution of percent predicted FVC and its relationship with mortality, in African-American and white women, using African-American and white reference equations from NHANES, respectively
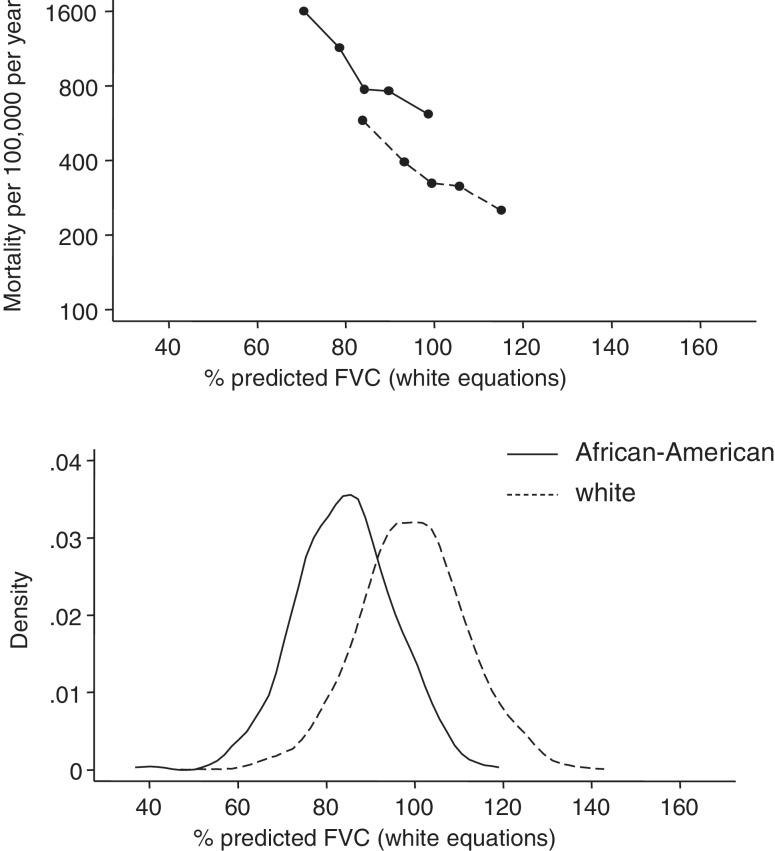
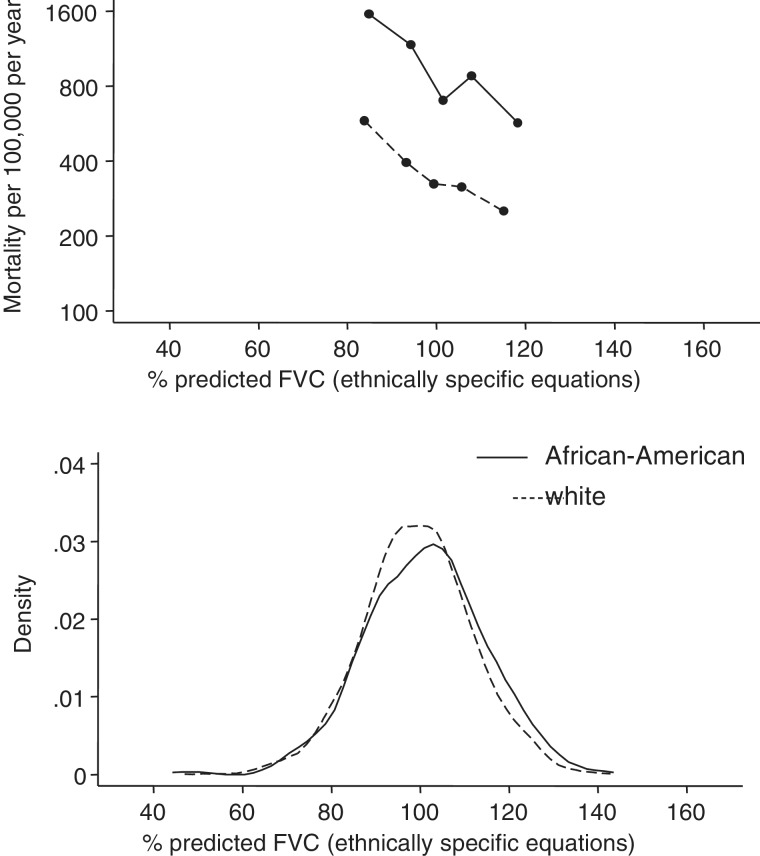
Figures 3 and 4, and Table 3, show a similar pattern for men. The overall mortality is higher in men, as expected, and the linear decrease in mortality with increasing FVC is more apparent at all levels of FVC. When adjusting for height and weight or by using the predicted values from the white equations, the African-American men have a slightly higher mortality than the white men (HR = 1.24, 95% CI 0.91–1.69), though this is not significant. When the ethnically specific equations are used to adjust the FVC, the HR increases to 1.56 (95% CI 1.15–2.10) and this is significant (P = 0.004). Again, the association between mortality and FVC does not change.
Figure 3.
Distribution of percent predicted FVC and its relationship with mortality, in African-American and white men, using white reference equations from NHANES
Figure 4.
Distribution of percent predicted FVC and its relationship with mortality, in African-American and white men, using African-American and white reference equations from NHANES respectively
The quality of the spirometry was different between the two ethnic groups with more unacceptable findings in the African-American sample. However, when we repeated the analyses using all available spirometry data regardless of quality, the results were qualitatively the same.
Discussion
Although African-Americans have lower forced vital capacity than white Americans, there is no evidence that a given forced vital capacity adjusted for age and height results in any difference in mortality for the two ethnic groups.
Current methods for setting norms for lung volumes assume that what is found in samples of the population without symptoms and without an obvious exposure to cigarettes or polluting industries is, by definition, normal. Whereas it may be ‘normal’ in the sense of ‘usual’, this analysis shows that it is not a benign difference without consequences.
Although there are substantial differences in ventilatory function between ethnic groups that are not accounted for by obvious potential confounders, the implication of any level of FVC for survival is equal in both African-American and white participants. Adjusting for ethnically specific norms does not change the association between FVC and survival but introduces an unexplained difference in survival between the two groups.
Because the range of lung function differs between the ethnic groups, it might be argued that we are unable to discuss differences at the ends of the range. However, a recent reassessment of the NHANES and Multi-Ethnic Study of Atherosclerosis (MESA) data has concluded that the difference in ventilatory function between ethnic groups is not related to age, sex or height.14
Normal values are used for different purposes and the implications of these findings will depend on the context in which spirometry is being undertaken. Diagnosis of obstructive disease will not be much affected as the FEV1/FVC ratio when adjusted for age, height and gender does not differ greatly between African-Americans and white Americans. When considering a restrictive disease, the index of suspicion will be lower in African-Americans with the same spirometry as a white American, but the diagnosis will need to be made on other grounds.
In assessing the severity of disease, if a given FVC carries the same prognosis for both ethnic groups, the use of ethnically specific norms may disadvantage African-Americans. At a public health level, this will disguise real disadvantage in the minority community and reduce the motivation to address the inequalities. At an individual level, it will underestimate impairment and potentially reduce the probability of treatment or of compensation. Internationally it will systematically underestimate the severity of disease burden as assessed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD),15 Body Mass Index, Airflow Obstruction, Dyspnoea and Exercise Capacity (BODE) index16 or Age, Dyspnoea and Airflow Obstruction (ADO) index17 methods in low- and middle-income countries.
In aetiological studies, it may still be important to adjust for ethnicity, though this will be a ‘black box’ adjustment for all those unknown causes of the difference in lung function between the ethnic groups. A clinical equivalent of this might be in deciding whether a particular exposure was likely to be responsible for lung function results. Our recommendation is that this adjustment is made explicitly and not through use of different predictive equations or norms. Interpretation of this difference can then be left to the reader.
This analysis does not identify the reasons for the disparity between African-American and white ventilatory function other than to discount sitting height, waist–hip ratio, BMI, smoking history, income, employment and educational achievement as major determinants of the difference. In this the results are more or less in line with other authors in relation to sitting height18 and even more elaborate attempts to explain the differences.19–21
It should not be surprising that adjustment for sitting height does not explain away the association between low lung function and all-cause mortality. Although African-Americans had a lower sitting height (Table 1) which showed some association with lower lung volumes (Table 2), leg length is inversely associated with insulin resistance, coronary heart disease,22 blood pressure, serum cholesterol, BMI23 and carotid intimal–medial thickness.24
Part of the explanation may be in the lower birthweight of African-American babies.25 FVC in later life has been consistently associated with low birthweight.26–30 This does not give a complete explanation. To start with, it begs the question of why African-American babies have low birthweights,31 and second, it does not exclude other factors later in life also making a contribution. Differences in lung function between other ethnic groups have also been noted including groups from the Indian subcontinent.32,33 In the UK, babies of mothers from the Indian subcontinent have even lower birthweights than those of mothers from Africa and the Caribbean.34 In the USA, a difference in lung function has been noted between established and new immigrants from the Indian subcontinent,35 suggesting that some of these differences, at least, are environmentally determined.
A recent paper has shown that ventilatory function is associated with the number of ‘black’ genes36 and the implication has been drawn by some that this implies a genetic origin for the lower ventilatory function in African-Americans. This is a serious over-interpretation of the evidence. Skin colour is the archetypical genetic trait associated with African ancestry, but has been clearly associated with many aspects of social disadvantage, regardless of race.37,38 Few would see this as good evidence on which to attribute social disadvantage in African-Americans to genetic causes in any usual sense of the term.
Ventilatory function adjusted for age, sex and height had the same prognosis for African-American as for white participants in the ARIC Study. Separate lung function equations should not, therefore, be used for the two different ethnic groups. For studies of prognosis, the same equations are shown here to be equivalent for white and African-American populations. This implies that international, or any other multi-ethnic studies that use lung volumes to assess the severity of COPD, using for instance the GOLD, BODE or ADO scores, should not use separate norms for different ethnic groups. In studies of aetiology, we suggest that the effect of race or ethnicity is reported explicitly, leaving open its interpretation. We suggest that the standards should be set by the group with the more advantaged background.
Funding
The Atherosclerosis Risk in Communities Study (ARIC) is conducted and supported by the National Heart Lung & Blood Institute (NHLBI) in collaboration with the ARIC Study Investigators. R.H.L. was supported by the Department of Health Policy Research Programme (#0120016).
Acknowledgements
We would like to express our gratitude to the investigators and staff of the ARIC study, who collected the data, and to Dr Neil Pride and Dr Sean Coady for helpful comments on an earlier draft. This manuscript was prepared using a limited access data set obtained from the NHLBI and does not necessarily reflect the opinions or views of the ARIC investigators or the NHLBI.
Conflict of interest: None declared.
KEY MESSAGES.
African-Americans have lower levels of ventilatory function than white Americans, and these are not adequately explained by known risk factors. This has led to ‘normative’ reference values being separately estimated for different ethnic groups and these are commonly used in practice.
This article demonstrates, however, that the same ventilatory function adjusted for age, sex and height predicts the same level of mortality in the different ethnic groups.
When using ventilatory function to assess severity of disease or prognosis, there is no justification for using ethnically specific reference values.
In epidemiological studies, ethnically specific reference values should not be used; instead the effect of ethnicity should be accounted for separately and regarded as ‘inadequately explained’.
References
- 1.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 2.Medbø A, Melbye H. What role may symptoms play in the diagnosis of airflow limitation? A study in an elderly population. Scand J Prim Health Care. 2008;26:92–98. doi: 10.1080/02813430802028938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salvi S, Barnes P. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374:733–43. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 4.Barker DJP, Osmond C. Childhood respiratory infection and adult chronic bronchitis in England and Wales. Br Med J. 1986;293:1271–75. doi: 10.1136/bmj.293.6557.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barker DJP, Godfrey KM, Fall C, Osmond C, Winter PD, Shaheen SO. Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. BMJ. 1991;303:671–75. doi: 10.1136/bmj.303.6804.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chinn S, Gislason T, Aspelund T, Gudnason V. Optimum expression of adult lung function based on all-cause mortality: results from the Reykjavik study. Respir Med. 2007;101:601–09. doi: 10.1016/j.rmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 7.The ARIC investigators. The atherosclerosis risk in communities (ARIC) study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 8.Mannino DM, Doherty DE, Buist AS. Global initiative on obstructive lung disease (GOLD) classification of lung disease and mortality: findings from the atherosclerosis risk in communities (ARIC) study. Respir Med. 2006;100:115–22. doi: 10.1016/j.rmed.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 9.Ferris BG. Epidemiology standardization project (American Thoracic Society) Am Rev Respir Dis. 1978;118:1–120. [PubMed] [Google Scholar]
- 10.ATS statement – snowbird workshop on standardization of spirometry. Am Rev Respir Dis. 1979;119:831–38. doi: 10.1164/arrd.1979.119.5.831. [DOI] [PubMed] [Google Scholar]
- 11. http://www.cscc.unc.edu/aric/pubuse (date last accessed 9 February 2012)
- 12.Lee ET, Wang JW. Statistical Methods for Survival Data Analysis. 3rd. New York: Wiley; 2003. [Google Scholar]
- 13.Silverman BW. Density Estimation for Statistics and Data Analysis. London: Chapman & Hall; 1986. [Google Scholar]
- 14.Burney PGJ, Hooper R. Forced vital capacity, airway obstruction and survival in a general population sample from the United States of America. Thorax. 2011;66:49–54. doi: 10.1136/thx.2010.147041. [DOI] [PubMed] [Google Scholar]
- 15.Medical Communications Resources, Inc. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. 2011 www.goldcopd.org (date last accessed 9 February 2012) [Google Scholar]
- 16.Celli B, Cote C, Marin J, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 17.Puhan M, Garcia-Aymerich J, Frey M, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: The updated BODE index and the ADO index. Lancet. 2009;374:704–11. doi: 10.1016/S0140-6736(09)61301-5. [DOI] [PubMed] [Google Scholar]
- 18.Whittaker AL, Sutton AJ, Beardsmore CS. Are ethnic differences in lung function explained by chest size? Arch Dis Child (Fetal and Neonatal Ed) 2005;90:F423–28. doi: 10.1136/adc.2004.062497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harik-Khan RI, Fleg JL, Muller DC, Wise RA. The effect of anthropometric and socioeconomic factors on the racial difference in lung function. Am J Respir Crit Care Med. 2001;164:1647. doi: 10.1164/ajrccm.164.9.2106075. [DOI] [PubMed] [Google Scholar]
- 20.Harik-Khan R, Muller D, Wise R. Racial difference in lung function in African-American and white children: Effect of anthropometric, socioeconomic, nutritional, and environmental factors. Am J Epidemiol. 2004;160:893–900. doi: 10.1093/aje/kwh297. [DOI] [PubMed] [Google Scholar]
- 21.Whitrow M, Harding S. Ethnic differences in adolescent lung function: anthropometric, socioeconomic, and psychosocial factors. Am J Respir Crit Care Med. 2008;177:1262–67. doi: 10.1164/rccm.200706-867OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith GD, Greenwood R, Gunnell D, Sweetnam P, Yarnell J, Elwood P. Leg length, insulin resistance, and coronary heart disease risk: The Caerphilly study. J Epidemiol Community Health. 2001;55:867–72. doi: 10.1136/jech.55.12.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunnell D, Whitley E, Upton MN, McConnachie A, Smith GD, Watt GCM. Associations of height, leg length, and lung function with cardiovascular risk factors in the midspan family study. J Epidemiol Community Health. 2003;57:141–46. doi: 10.1136/jech.57.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tilling K, Lawlor D, Smith G, Chambless L, Szklo M. The relation between components of adult height and intimal-medial thickness in middle age: the atherosclerosis risk in communities study. Am J Epidemiol. 2006;164:136–42. doi: 10.1093/aje/kwj184. [DOI] [PubMed] [Google Scholar]
- 25.Wilcox AJ. On the importance – and the unimportance – of birthweight. Int J Epidemiol. 2001;30:1233–41. doi: 10.1093/ije/30.6.1233. [DOI] [PubMed] [Google Scholar]
- 26.Stein CE, Kumaran K, Fall CHD, Shaheen SO, Osmond C, Barker DJP. Relation of fetal growth to adult lung function in south India. Thorax. 1997;52:895–99. doi: 10.1136/thx.52.10.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edwards CA, Osman LM, Godden DJ, Campbell DM, Douglas JG. Relationship between birth weight and adult lung function: Controlling for maternal factors. Thorax. 2003;58:1061–65. doi: 10.1136/thorax.58.12.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dezateux C, Lum S, Hoo A, Hawdon J, Costeloe K, Stocks J. Low birth weight for gestation and airway function in infancy: exploring the fetal origins hypothesis. Thorax. 2004;59:60–66. [PMC free article] [PubMed] [Google Scholar]
- 29.Canoy D, Pekkanen J, Elliott P, et al. Early growth and adult respiratory function in men and women followed from the fetal period to adulthood. Thorax. 2007;62:396–402. doi: 10.1136/thx.2006.066241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hancox RJ, Poulton R, Greene JM, McLachlan CR, Pearce MS, Sears MR. Associations between birth weight, early childhood weight gain and adult lung function. Thorax. 2009;64:228–32. doi: 10.1136/thx.2008.103978. [DOI] [PubMed] [Google Scholar]
- 31.Basso O, Wilcox A. Intersecting birth weight-specific mortality curves: solving the riddle. Am J Epidemiol. 2009;169:787–97. doi: 10.1093/aje/kwp024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aggarwal AN, Gupta D, Jindal SK. Comparison of Indian reference equations for spirometry interpretation. Respirology. 2007;12:763–68. doi: 10.1111/j.1440-1843.2007.01123.x. [DOI] [PubMed] [Google Scholar]
- 33.Fulambarker A, Copur A, Javeri A, Jere S, Cohen M. Reference values for pulmonary function in Asian Indians living in the United States. Chest. 2004;126:1225–33. doi: 10.1378/chest.126.4.1225. [DOI] [PubMed] [Google Scholar]
- 34.Moser K, Stanfield K, Leon D. Birthweight and gestational age by ethnic group, England and Wales 2005: introducing new data on births. Health Stat Q. 2008;39:22–55. [PubMed] [Google Scholar]
- 35.Fulambarker A, Copur A, Cohen M, et al. Comparison of pulmonary function in immigrant vs US-born Asian Indians. Chest. 2010;137:1398–404. doi: 10.1378/chest.09-1911. [DOI] [PubMed] [Google Scholar]
- 36.Kumar R, Seibold M, Aldrich M, et al. Genetic ancestry in lung-function predictions. N Engl J Med. 2010;363:321–30. doi: 10.1056/NEJMoa0907897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill ME. Color differences in the socioeconomic status of African American men: results of a longitudinal study. Social Forces. 2000;78:1437–60. [Google Scholar]
- 38.Hughes M, Hertel BR. The significance of color remains: A study of life chances, mate selection, and ethnic consciousness among black Americans. Social Forces. 1990;68:1105–20. [Google Scholar]