Abstract
The Karonga Health and Demographic Surveillance System (Karonga HDSS) in northern Malawi currently has a population of more than 35 000 individuals under continuous demographic surveillance since completion of a baseline census (2002–2004). The surveillance system collects data on vital events and migration for individuals and for households. It also provides data on cause-specific mortality obtained by verbal autopsy for all age groups, and estimates rates of disease for specific presentations via linkage to clinical facility data. The Karonga HDSS provides a structure for surveys of socio-economic status, HIV sero-prevalence and incidence, sexual behaviour, fertility intentions and a sampling frame for other studies, as well as evaluating the impact of interventions, such as antiretroviral therapy and vaccination programmes. Uniquely, it relies on a network of village informants to report vital events and household moves, and furthermore is linked to an archive of biological samples and data from population surveys and other studies dating back three decades.
Keywords: Demography, epidemiology, census, sub-Saharan Africa, Malawi, HIV, population dynamics, vital statistics, mortality, cause of death, life expectancy
Origins of the Karonga HDSS
The Karonga Prevention Study (KPS), established in the Karonga District of rural northern Malawi, has focused on epidemiological, clinical and immunological studies of infectious diseases of public health importance. The KPS was designed in 1979, initially as a large cohort study of risk factors for leprosy, covering the entire district of Karonga. In the 1980s,1 two total population surveys were conducted to identify and examine individuals and to collect socio-economic and other household level data. In 1986, the programme assumed responsibility for district-wide tuberculosis diagnosis and treatment, and in the same year, KPS became the largest vaccine trial in Africa, with our investigation of the effects of Bacillus Calmette-Guérin and/or killed M.leprae against both leprosy and tuberculosis (TB).2 TB epidemiological studies continue district wide today.3 In 1987, studies were conducted that established the presence of HIV, which has since then become a major theme of our research.
The Karonga HDSS was initiated in 2002 principally to provide a platform for epidemiological studies of HIV and HIV-associated infectious disease and to monitor the impact of interventions. The location of the Karonga HDSS was determined largely by the availability of HIV prevalence and incidence data that identified the first cases in the area in 1982 through retrospective testing of archived material.4 The Karonga HDSS became a member of the INDEPTH international network of field sites with continuous demographic evaluation of populations and their health in developing countries (http://www.indepth-network.org) in 2004, and was one of the founder sites of the ALPHA network for analysis of longitudinal, population-based HIV/AIDS data in Africa (http://www.lshtm.ac.uk/eph/psd/alpha) in 2005.
What does the Karonga HDSS cover now?
The core Karonga HDSS generates data on basic demographic indices, as well as cause-specific mortality for all age groups; population level data have also been routinely collected on vaccine coverage and socio-economic status. Active case finding for TB (via cough inquiry) has also been conducted.
The current programme, which commenced in 2006, combines detailed clinical and behavioural studies in individuals, with population-based epidemiological and demographic studies to: (i) monitor changes in HIV incidence and transmission of drug resistant virus; (ii) assess changes in sexual behaviour and attitudes through both quantitative and qualitative studies; (iii) measure HIV-attributable mortality and morbidity; (iv) identify factors affecting anti-retroviral treatment (ART) adherence; (v) evaluate socio-economic and demographic impact of HIV and provide estimates of future trends in the HIV epidemic (to identify target areas for future interventions); (vi) evaluate the success of the programme for prevention of mother-to-child transmission of HIV; (vii) understand the impact of new vaccine introduction on child mortality and, more recently, (viii) explore in detail contact patterns and the transmission dynamics of M.tuberculosis. To this end, multiple population level surveys have generated comprehensive data on sexual behaviour, fertility intentions, HIV and herpes simplex virus-2 sero-prevalence and incidence, detailed educational attainment and socio-economic status, anthropometry in children and mothers and tuberculin skin tests in children aged under 5 years. Furthermore, these data are linked to health facility data from ART, antenatal and paediatric clinics.
Research plans for the near future include an expansion into the area of non-communicable diseases, particularly diabetes and hypertension (which account in part for an increasingly high burden of disease in this setting), an increased emphasis on intervention studies and establishment of an urban partner site in Lilongwe.
Photograph 1.
Karonga HDSS—survey team recruiting family for survey (written consent obtained from participants). Photograph: Vijay Bansode
Where is the Karonga HDSS area?
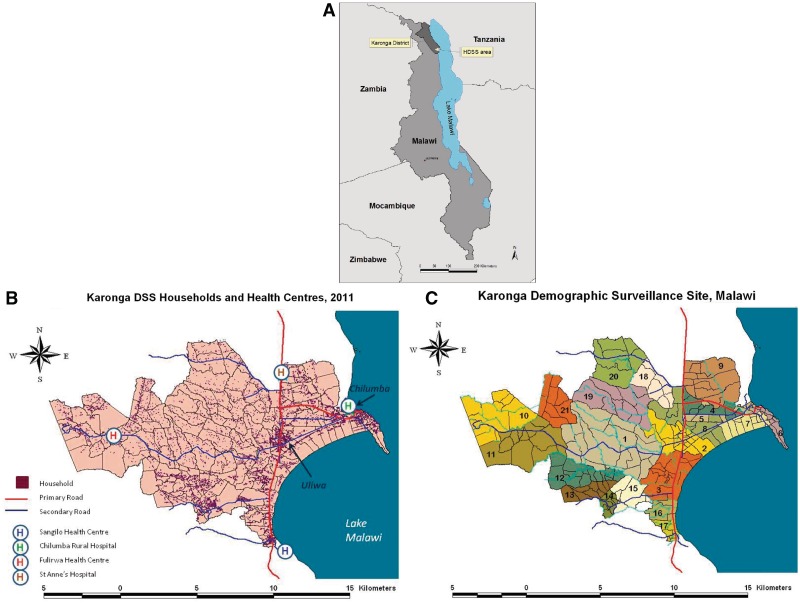
The Karonga HDSS surrounds the port village of Chilumba, on Lake Malawi, in the southern part of Karonga District (Figure 1a), where the project headquarters are found. The surveillance area is located between latitudes 10.38° and 10.50°S and longitudes 34.08° and 34.27°E, covering an area of approximately 135 km2. The lake shore and the Nyika National Park form the boundaries to the east and west, respectively, whereas the boundaries to the north and south are delineated by village boundaries—and here three (of four) health facilities that serve the area are found (Figure 1b). The climate is hot and dry from September to December, with rains from January to May, and cool and dry from June to August. The Karonga HDSS population is predominantly rural, and the economy is based upon subsistence agriculture, fishing and petty trading. In the rural area, the households are scattered, although a higher density of households exist in two semi-urban settlements—a trading centre (Uliwa) on the main road from Tanzania into Malawi, and Chilumba itself (Figure 1b). Approximately 15% of the Karonga HDSS population live in these semi-urban areas, and 50% live within one kilometre of a tarmac road.
Figure 1.
(A) Location of Karonga district and Karonga HDSS in Malawi; (B) map of Karonga HDSS showing household distribution, primary and secondary roads and location of health facilities; (C) map of Karonga HDSS showing cluster and reporting group boundaries. Data and boundaries from Karonga HDSS databases at end 2011
Before the initial enumeration, meetings were held with the Wasambo (the traditional authority with responsibility for the area), and additional sensitisation sessions were held with the group village headmen (each representing several villages). During the baseline census, further meetings were held with each village headman and the ndunas (village elders) before entering each new location to gain consent for establishing a camp and to conduct the survey. At this time, ndunas and other responsible community individuals were recruited as key informants to report vital events and household migrations.
Handheld global positioning system devices were used to map the surveillance area and to mark village boundaries, major and minor roads and tracks, rivers, key institutions (such as health facilities and schools) and individual household locations. Each village was further divided into smaller geographical areas (known as clusters) that represent 20–30 households. Groups of approximately 10 clusters in a defined geographical area were combined to form the 21 reporting groups, which make up the surveillance area (Figure 1c). The geographical data are stored in ARC-info.
Who is covered by the Karonga HDSS and how often have they been followed up?
At the end of 2011, 35 730 individuals from 8285 households were under observation in the Karonga HDSS. Members of each household within the geographical boundaries are invited to participate (and visitors were also captured in the baseline survey). In practice, refusal is on a household rather than an individual basis, and less than 1% of households (usually those of spiritualists or other objecting religions) do not participate. For the purpose of the Karonga HDSS, a household is defined as a group of individuals who usually live together and recognize the same household head, although two or more households may share a household head, as frequently occurs within polygynous unions. A member of a household is a person who is accepted as belonging to the household and may include schoolchildren who temporarily live somewhere else during term-time. A visitor is defined as someone who is expected to return to their home elsewhere, irrespective of their duration in the current household. The definitions of household, member and visitor are based on cultural perceptions.
Photograph 2.
Karonga HDSS—nurse recruiting mother and child for paediatric disease surveillance in health facility (written consent obtained from participants). Photograph: Anna Molesworth
During the initial baseline census in each cluster, a key informant resident in that cluster was selected and trained to keep a real-time record of vital events and whole household movements within his or her group of households, by making notes pencilled in a printed household register generated from the baseline census data. A nominated KPS interviewer (supervisor) meets with the key informants representing each reporting group (of 10 or so clusters) at a designated location each month (monthly update) to update the supervisor’s household register for each cluster with the vital event reports. At this meeting, refreshments are provided, and the key informant is given a nominal sum (currently about $3) to compensate them for their time. When births are reported, the supervisor will visit the household immediately after the meeting to register the birth and administer a brief questionnaire; however, in the event of a death, a medical assistant will visit the household to register the death and to conduct a verbal autopsy after an appropriate mourning period (usually 2–3 weeks). If the birth, or death, is in a new household or if the death has resulted in household dissolution or out-migration, members of in-migrating households are registered, or departure information is sought on dissolved/departed households.
Every year, an annual update session is held with the key informants, at which they report whole household migrations during the previous 12 months, (and the vital events of the previous month are also reported). Migrations are reported annually to ensure that true demographic change is not obscured by the recording of temporary, frequently reversed, inter-household moves. The annual update meeting with key informants is followed by an annual re-census, which further identifies individual out- or in-migrations and gives an opportunity to conduct socio-economic interviews. At the next monthly update session, the supervisor and key informant are issued with revised household registers for each cluster that reflect updated information on migrations and vital events, and feedback is given on births and deaths in their village. From time to time, a key informant retires and a new one is trained.
Paper questionnaires are returned to the KPS data office, where, after registration, identity numbers are issued to new births, and migrants are investigated to see whether they have had previous contact with the programme, before issue or re-issue of identity numbers. Since its inception, the programme has used a rigorous identification process that facilitates reliable re-identification of individuals even if they have not been under observation for many years. Each individual has a static and unique identity number, as well as a unique Continuous Registration System (CRS) number [formed by concatenating the reporting group number, cluster number, household number and member number (place in that household when first identified)]. If individuals (or households) move within the Karonga HDSS, new CRS numbers will be assigned, but the identity number remains unchanged.
Of the 35 730 individuals under observation, at the end of 2011, 48% (16 818/35 730) were male, 18% (6265/35 730) were under 5 years and 48% (17 158/35 730) were under 15 years of age. In all, 47% (16 684/35 730) of the population were aged between 15 and 59 years, and 5% (1888/35 730) were aged 60 years and above.
An active community engagement programme is in place, which includes Key Informant Days, where groups of key informants visit the project headquarters for presentations on recent findings to feed back to the community. They visit the laboratories and data office to see how specimens and data are held, and participate in quizzes and dramas to facilitate understanding of the research process. Community sensitisation events (usually one per reporting group, with typical attendances of 200–800 people) are held at the time of introduction of new studies, with dancing, dramas and question and answer sessions.
What is measured and how have the Karonga HDSS databases been constructed?
The core data collected throughout the Karonga HDSS include individual and household identifying information, parent identification and spousal relationships at each time point. Sufficient data are collected to link individuals of all ages to both parents, facilitating genetic and orphan-hood studies. Basic socio-economic data are also collected as part of core Karonga HDSS activity. Verbal autopsies collect detailed data on symptoms and signs during the terminal illness, allowing assignment of cause of death following physician review or computer algorithm. Core data items are summarized in Table 1. Other data are collected in the context of Karonga-wide surveys, population samples or during health facility attendances.
Table 1.
Information collected or checked at routine events
| Main data item | Additional information |
|---|---|
| Household data | |
| Name of head of household | |
| Village name | |
| Date since household was in current location | |
| Latitude, longitude | |
| At in-migration to HDSS or birth registration | |
| Names | current and previous |
| Sex | |
| Date of birth | estimates as required |
| Date of in-migration | (in migrants only) |
| Name/identifier of mother | vital status of mother and household/village |
| Name/identifier of father | vital status of father and household/village |
| Previous contact with KPS | where last seen |
| Siblings alive in Karonga | shared parent(s) |
| Current household | when joined household |
| Position in household | |
| Was person seen or proxy informant used | informant name and relationship |
| Reason for immigration | (in-migrants only) |
| Previous household and village | (in-migrants only) |
| At recensus—additional information (as of 2011, changes over time) | |
| Relationship to household head | |
| Parental educational achievement | |
| Marital status | number of current spouses or co-spouses |
| Spouse identification details | dates of marriage |
| Educational achievement | |
| Main occupation | |
| Reason for leaving school | age at leaving school |
| Details of school absences | (if currently enrolled in school) |
| Vaccination history | (if less than 5 years old) |
| Bacillus Calmette-Guérin, Polio, Pentavalent, Measles | |
| Pneumococcal conjugate vaccine | |
| Mobile phone access | do they have exclusive use |
| Participation in mass campaigns | e.g. measles vaccine campaign, filariasis mass drug treatment |
| TB case finding, cough, haemoptysis | sputum collection |
| At death registration (accompanied by age-specific verbal autopsy form) | |
| Informant | informant name and relationship |
| Association with deceased during terminal illness | |
| Pregnancy details | (if neonatal death) |
| Health document review | |
| Vaccination history | (if less than 5 years old) |
| Date of death/stillbirth | |
| Category of place of death | name of health facility if required |
| Category of care sought during terminal illness | |
| At out-migration | |
| Date of migration | |
| Destination |
The detailed identifying information at first or renewed contact with the Karonga HDSS team enables linkage through the identity number system to all other data (more than 1 million individual contacts) and biological samples (more than 2 00 000) held by the programme.
Karonga HDSS data are double entered into MS Access 2007 databases as soon as any identification and coding procedures are complete, and discrepancies between the two databases are corrected weekly. The data are held in multiple event tables in the databases with a single view table describing all Karonga HDSS events. Daily data are extracted by a programmed script to integrate new data to the Karonga HDSS analysis database, to update the generic programme database holding records of every contact with an individual and to run consistency checks. The MS access data are held on a Linux server and backed up twice daily to external media.
Key findings and publications
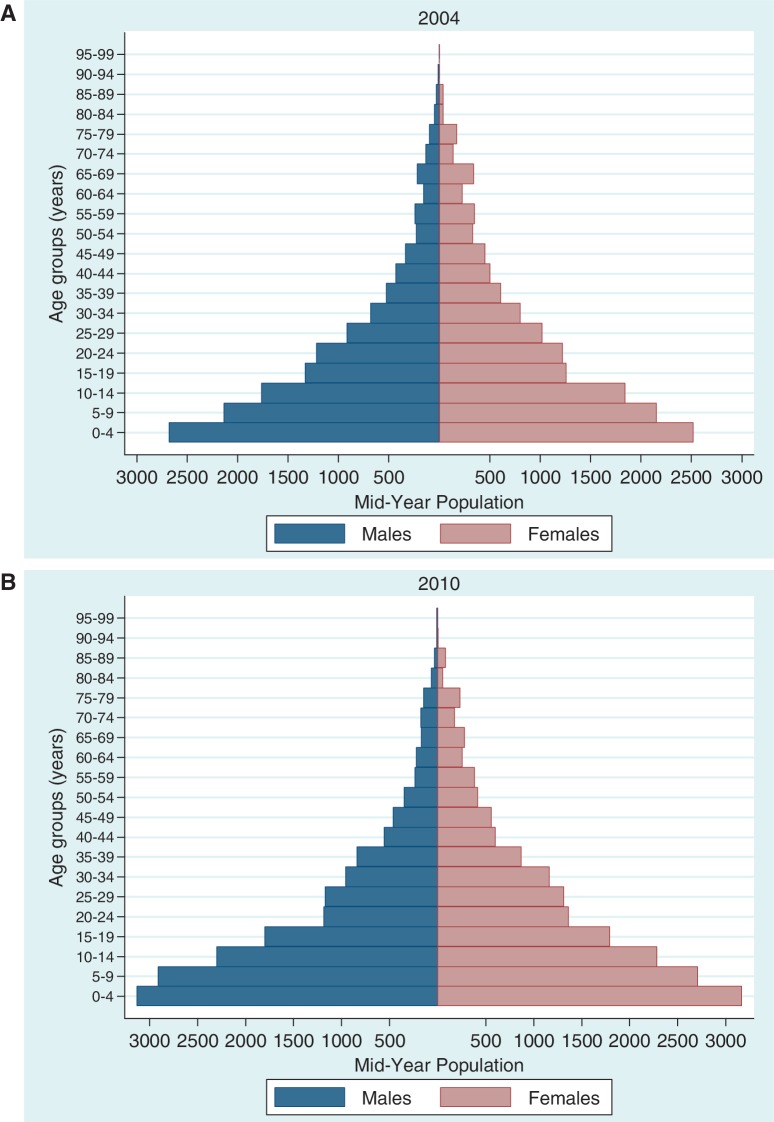
We established early on that our system of informants was reliable in capturing both births (97%) and deaths (99%),5 and the Karonga HDSS contributes these validated demographic data to INDEPTH monographs, which are routinely published (http://www.indepth-network.org/index.php?option=com_content&task=view&id=76&Itemid=164). Basic demographic indices for the period 2005–2010 are summarized in Table 2, and population pyramids from 2004 and 2010 are shown in Figures 2a and 2b. The pyramids reflect the significant mortality in young children, the mortality in young adults as a consequence of the HIV epidemic and the out-migration of teenagers and young adults of both sexes from this rural area to seek education and employment. The table shows dramatic sustained reductions in mortality in all age groups, except for neonates. Population growth is approximately 2.5% per annum, but this is largely driven, not by birth and death rates, but by the much higher in- and out-migration rates, with the latter predominating.
Table 2.
Demographic characteristics of the Karonga HDSS
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|
| Total population | 31,325 | 32,569 | 33,357 | 33,518 | 33,655 | 34,747 |
| Crude birth rate per 1000 PY | 46.6 | 43.8 | 43.1 | 39.8 | 40.2 | 37.3 |
| In-migration rate per 1000 PY | 93.9 | 81.9 | 68.3 | 72.0 | 78.1 | 73.2 |
| Out-migration rate per 1000 PY | 81.0 | 80.9 | 92.4 | 98.0 | 99.7 | 76.7 |
| Crude death rate per 1000 PY | 10.9 | 10.0 | 8.7 | 8.1 | 7.1 | 6.1 |
| Adult mortality rate per 1000 PY | 12.5 | 11.7 | 10.1 | 10.0 | 8.4 | 6.9 |
| Life expectancy at birth (years) | 57.7 | 59.0 | 62.0 | 62.9 | 66.8 | 69.4 |
| Neonatal mortality rate per 1000 live births | 24.7 | 20.4 | 23.1 | 20.3 | 24.5 | 15.5a |
| Post-neonatal mortality rate per 1000 live births | 30.2 | 28.1 | 18.9 | 21.8 | 17.8 | 19.4 |
| Infant mortality rate per 1000 live births | 54.9 | 48.6 | 42.0 | 42.1 | 42.3 | 35.0 |
| Under-five mortality rate per 1000 live births | 85.8 | 80.2 | 75.0 | 66.9 | 61.6 | 59.1 |
Basic vital statistics based on population estimates, 2005–2010.
aThis figure is correct; however, trend should not be over-interpreted as based on only 20–30 neonatal deaths per year. PY = per year
Figure 2.
Population pyramid of Karonga HDSS (A) 2004 and (B) 2010. Data represent individuals under observation at the mid-point of these years
Our most important findings to date relate to the impact of ART on the population. We showed the first evidence of a population-level decline in adult mortality (16% drop) because of the rapid scale-up of ART, free at the point of delivery, even though by that stage, only an estimated one-third of those in need had accessed ART.6 At that time, the improvements were confined to those near the roadside with easier access to the services provided in the district town. Subsequently, as a clinic opened within the Karonga HDSS area, a further decline in all-cause mortality (32% reduction) was observed. This extended to more remote areas,7 and estimated treatment coverage was 70%.
Combining our data, with those from other INDEPTH/ALPHA demographic sites, with HIV data, we have confirmed the importance of local provision of ART for mortality improvement,8 validated projections of ART need from the age and sex profile of HIV-infected people9 and compared knowledge of HIV status and uptake of ART between demographic sites.10
Using the Karonga HDSS for structured sampling, we identified that early in the ART programme, screening for eligibility based on clinical staging alone would miss two-thirds of those eligible by combined clinical and CD4 staging.11 We investigated the gender differences in ART uptake combining quantitative and qualitative approaches, and found that the nurturing role of women was key to their early presentation, whereas men’s wider need for social acceptance resulted in delays.12
An analysis of cause-specific mortality has shown that, following the roll-out and decentralisation of ART, HIV/AIDS is no longer the leading cause of adult death in this area, and non-communicable causes such as cardiovascular disease predominate.13
Examining HIV incidence in discordant couples in a population-based programmatic setting study, shows that transmission is prevented by ART, whereas transmission from those who are untreated continues, with husband-to-wife transmission higher than wife-to-husband.14 Drug resistance mutations were found in 20% of drug-naive individuals in the Karonga HDSS area, although the clinical significance of these is uncertain.15
Childhood mortality studies have shown that HIV closed the survival gap between the children of the very poor and the rest of the population, as HIV in the early part of the epidemic was associated with greater wealth.16 Mortality rates in all child-age groups declined despite HIV17 even before ART was likely to have had an impact. One-fifth of all deaths in children aged under 15 years were attributable to HIV in this pre-ART period.17
Methodological studies nested within the Karonga HDSS demonstrated that although home-based rapid HIV testing is highly sensitive and specific,18 testing in surveys when a high proportion of individuals already know their status should be interpreted with caution, as underestimates arise because of selective test refusals.19 Methods to correct the bias have been explored.
In our sexual behaviour surveys, we triangulated reports of extra-marital partnerships to show that under-reporting by women was strongly age dependent, but that young men also under-reported in this setting.20 We also found that girls with early menarche start sex and marry early, leading to school drop-out, and that girls with late menarche had the same educational achievement as boys.21 Using our detailed sexual behaviour data, we have also explored the interpretation of the UNAIDS recommended methods of measuring concurrency in sexual relationships, thought to be key to understanding the dynamics of HIV transmission.22
We used our population-survey anthropometry data to investigate the effects of the new WHO Growth Standards on the measures of prevalence of stunting, underweight and wasting, compared with the previously used National Centre for Health Statistics reference, finding that the new standards gave higher estimates for all indices, especially in early infancy.23 There was no difference in their ability to identify risk factors for malnutrition.
Vaccination coverage in children was high eventually, but frequently delayed, particularly in those from poorer families and living at a distance from health facilities.24
For full KPS publications, visit http://www.lshtm.ac.uk/eph/ide/research/kps/publications/index.html, and ALPHA network articles are summarized at http://www.lshtm.ac.uk/eph/psd/alpha/publications/index.html.
Future analysis plans
Analyses are ongoing in many areas; we continue to evaluate the impact of HIV and ART on mortality, morbidity and socio-economic status. We are also undertaking a detailed analysis of child mortality trends and causes of death.
In a combined INDEPTH and ALPHA networks initiative, we are using our detailed verbal autopsy questionnaire data to validate Inter-VA (http://www.interva.net)—a computer model that facilitates interpretation of verbal autopsies and their application to populations by assigning probabilities of multiple causes to each death.
Another stream of work analyses data on fertility intentions and the impact of unplanned pregnancies on existing child welfare, the consistency of partners’ fertility desires within marital unions and the effect on fertility desire of knowledge of HIV. Uptake of modern methods of contraception and the relationship to expressed fertility intentions in HIV-positive, -negative and -discordant couples and the fertility of women already on ART are also being explored, as are fertility patterns and influences in both men and women.
We are exploring further the dynamics of educational achievement and sexual behaviour, and other influences on female retention in school.
A study of carriage of pneumococcus in a population birth cohort, both HIV exposed and unexposed, pre- and post-introduction of pneumococcal conjugate vaccine is currently being analysed and linked to the rates of morbidity from childhood pneumonias and other febrile illnesses in the Karonga HDSS area.
What are the main strengths and weaknesses?
A major scientific strength of the Karonga HDSS is the nesting of the demographic survey in the historic cohort dating from 1979 and the full linkage to longitudinal data (demographic, epidemiological, clinical) and biological samples, through our well-established identification procedures. These procedures also allow us to track individuals between households and areas and to identify formerly resident in-migrants even after decades of absence. Our presence throughout the district also allows tracing of individuals anywhere within Karonga (population: 250 000 individuals), if follow-up of specific individuals is required. Full parental linkage (both in and out of marriage) allows us to study genetic linkages, orphan-hood and male fertility patterns.
The methodological advantages of our system include the real-time reporting from village informants. This brings benefits not only from contemporaneous reporting (particularly important for birth registration in the presence of neonatal and infant mortality, and accurate verbal autopsies) but also enables the Karonga HDSS team to have a relatively low profile in the community. Other than the annual census or special surveys, a household is only visited if a vital event occurs.
Our active community engagement programme and long-standing involvement with disease control programmes (notably leprosy, tuberculosis and HIV) result in good relations with the community and generally high consent rates in all studies.
A potential limitation scientifically is that this is a heavily studied area with a consequent risk of study fatigue (although our experience is that this does not have major impact) or behaviour modification that may bias observational studies. In terms of the methods, as reporting of individual (rather than household) migrations by key informants has proved too difficult to implement, in-migrants who come and leave between two re-census periods may be missed from registration. Using key informants to report vital events by proxy means we cannot capture some sensitive events, such as pregnancies.
Data sharing and collaboration
Currently our data are held on site and are not available remotely. Applications to access HDSS data for collaborative analysis are encouraged and can be made by proposal submission to the Deputy Director/ Scientific Programme Manager: mia.crampin@lshtm.ac.uk (http://www.lshtm.ac.uk/eph/ide/research/kps/index.html). Subject to funding, in the next few years, selected Karonga HDSS data will be made available online via an open access site (e.g. via the INDEPTH platform), and procedures for applying for use and generating appropriate additional data sets will be streamlined.
Funding
The work is supported primarily by the Wellcome Trust, with use of facilities owned by the British Leprosy Relief Association and support for individual studies from many other funders, including Hewlett-ESRC.
Acknowledgements
Thanks to the participants in the Karonga HDSS area and particularly the key informants and traditional authorities for their support over the years. The support of the District Health Management Team of Karonga and the Ministry of Health of Malawi has been invaluable.
The Karonga HDSS relies on the energy, commitment and attention to detail of an excellent team of field staff (led by E.M.), and data officers with support from our clinical and laboratory departments and Jacky Saul, our data manager.
We look forward to new directions for the Karonga HDSS through the vision of the new director of Karonga Prevention Study, Prof Shabbar Jaffar.
We also appreciate the support from, and inspiring interaction with, other members of the INDEPTH and ALPHA networks.
Conflict of interest: None declared.
KEY MESSAGES.
Karonga HDSS is a health and demographic surveillance system of 35 000 individuals based on a validated and cost-effective community reporting structure.
Karonga HDSS was designed as a platform for epidemiological and clinical studies using well-established identification procedures enabling linkage to health and socio-economic data and archived biological specimens. Our capacity to re-identify individuals and to link children with both parents facilitates longitudinal investigations of individuals and families, spanning decades, including genetic relationships.
Current research areas include HIV, TB and other infectious diseases, and behavioural studies related to transmission, although in response to changing health priorities in Malawi, future plans include diversification to non-communicable diseases (e.g. hypertension and diabetes).
References
- 1.Ponninghaus JM, Fine PE, Bliss L, Sliney IJ, Bradley DJ, Rees RJ. The Lepra Evaluation Project (LEP), an epidemiological study of leprosy in Northern Malawi. I. Methods. Lepr Rev. 1987;58:359–75. doi: 10.5935/0305-7518.19870038. [DOI] [PubMed] [Google Scholar]
- 2.Ponnighaus JM, Fine PE, Sterne JA, et al. Efficacy of BCG vaccine against leprosy and tuberculosis in northern Malawi. Lancet. 1992;339:636–39. doi: 10.1016/0140-6736(92)90794-4. [DOI] [PubMed] [Google Scholar]
- 3.Crampin AC, Glynn JR, Fine PE. What has Karonga taught us? Tuberculosis studied over three decades. Int J Tuberc Lung Dis. 2009;13:153–64. [PMC free article] [PubMed] [Google Scholar]
- 4.Crampin AC, Glynn JR, Ngwira BM, et al. Trends and measurement of HIV prevalence in northern Malawi. Aids. 2003;17:1817–25. doi: 10.1097/00002030-200308150-00011. [DOI] [PubMed] [Google Scholar]
- 5.Jahn A, Crampin A, Glynn J, et al. Evaluation of a village-informant driven demographic surveillance system in Karonga, Northern Malawi. Demogr Res. 2007;16:2119–248. [Google Scholar]
- 6.Jahn A, Floyd S, Crampin AC, et al. Population-level effect of HIV on adult mortality and early evidence of reversal after introduction of antiretroviral therapy in Malawi. Lancet. 2008;371:1603–11. doi: 10.1016/S0140-6736(08)60693-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Floyd S, Molesworth A, Dube A, et al. Population-level reduction in adult mortality after extension of free anti-retroviral therapy provision into rural areas in northern Malawi. PLoS One. 2010;5:e13499. doi: 10.1371/journal.pone.0013499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Floyd S, Marston M, Baisley K, et al. The effect of antiretroviral therapy provision on all-cause and cause-specific mortality at the population level—a comparative analysis of data from 4 demographic surveillance sites. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2012.03032.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaba B, Kasamba I, Floyd S, et al. Using age-specific mortality of HIV infected persons to predict Anti-Retroviral Treatment need: a comparative analysis of data from five African population-based cohort studies. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2011.02943.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wringe A, Floyd S, Kazooba P, et al. Antiretroviral therapy uptake and coverage in four HIV community cohort studies in sub-Saharan Africa. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2011.02925.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGrath N, Kranzer K, Saul J, et al. Estimating the need for antiretroviral treatment and an assessment of a simplified HIV/AIDS case definition in rural Malawi. Aids. 2007;21(Suppl. 6):S105–13. doi: 10.1097/01.aids.0000299417.69432.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parrott FR, Mwafulirwa C, Ngwira B, et al. Combining qualitative and quantitative evidence to determine factors leading to late presentation for antiretroviral therapy in Malawi. PLoS One. 2011;6:e27917. doi: 10.1371/journal.pone.0027917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chihana M, Floyd S, Molesworth A, et al. Adult mortality and probable cause of death in rural northern Malawi in the era of HIV treatment. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2012.02929.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Price A, Glynn JR, Floyd S, et al., editors. Quebec, Canada: July 2011. Antiretroviral Therapy Reduces HIV Transmission in Discordant Couple in Northern Malawi. ISSTDR. [Google Scholar]
- 15.Bansode V, Drebert ZJ, Travers SA, et al. Drug resistance mutations in drug-naive HIV type 1 subtype C-infected individuals from rural Malawi. AIDS Res Hum Retroviruses. 2011;27:439–44. doi: 10.1089/aid.2010.0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jahn A, Floyd S, McGrath N, et al. Child mortality in rural Malawi: HIV closes the survival gap between the socio-economic strata. PLoS One. 2010;5:e11320. doi: 10.1371/journal.pone.0011320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jahn A, Floyd S, Crampin AC, et al. Declining child mortality in northern Malawi despite high rates of infection with HIV. Bull World Health Organ. 2010;88:746–53. doi: 10.2471/BLT.09.075085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Molesworth AM, Ndhlovu R, Banda E, et al. High accuracy of home-based community rapid HIV testing in rural Malawi. J Acquir Immune Defic Syndr. 2010;55:625–30. doi: 10.1097/QAI.0b013e3181f98628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karonga Prevention Study, unpublished data. 2012.
- 20.Glynn JR, Kayuni N, Banda E, et al. Assessing the validity of sexual behaviour reports in a whole population survey in rural Malawi. PLoS One. 2011;6:e22840. doi: 10.1371/journal.pone.0022840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glynn JR, Kayuni N, Floyd S, et al. Age at menarche, schooling, and sexual debut in northern Malawi. PLoS One. 2010;5:e15334. doi: 10.1371/journal.pone.0015334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glynn JR, Dube A, Kayuni N, et al. Measuring concurrency: an empirical study of different methods in a large population-based survey in northern Malawi and evaluation of the UNAIDS guidelines. AIDS. 2012 doi: 10.1097/QAD.0b013e328350fc1f. (in press) [DOI] [PubMed] [Google Scholar]
- 23.Prost MA, Jahn A, Floyd S, et al. Implication of new WHO growth standards on identification of risk factors and estimated prevalence of malnutrition in rural Malawian infants. PLoS One. 2008;3:e2684. doi: 10.1371/journal.pone.0002684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jahn A, Floyd S, Mwinuka V, et al. Ascertainment of childhood vaccination histories in northern Malawi. Trop Med Int Health. 2008;13:129–38. doi: 10.1111/j.1365-3156.2007.01982.x. [DOI] [PubMed] [Google Scholar]