Abstract
Background The South-East Asia region (SEAR) accounts for one-quarter of the world's population, 40% of the global poor and ∼30% of the global disease burden, with a disproportionately large share of tuberculosis (35%), injuries (30%), maternal (33%) and <5-year-old mortality (30%). In this article, we describe the disease burden and status of epidemiological research and capacity in the SEAR to understand, analyse and develop capacity in response to the diverse burdens of diseases in the region.
Methods Data on morbidity, mortality, risk factors, social determinants, research capacity, health education, workforce and systems in the SEAR were obtained using global data on burden of disease, peer-reviewed journals, World Health Organization (WHO) technical and advisory reports, and where available, validated country reports and key informants from the region.
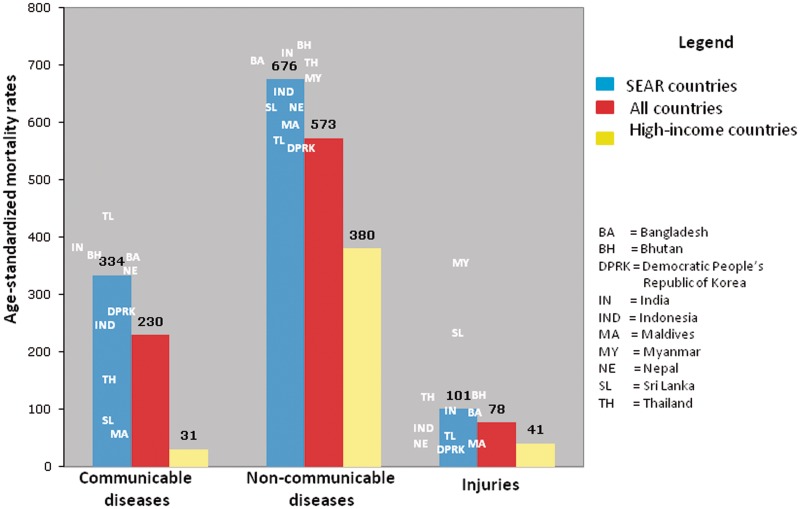
Results SEAR countries are afflicted with a triple burden of disease—infectious diseases, non-communicable diseases and injuries. Of the seven WHO regions, SEAR countries account for the highest proportion of global mortality (26%) and due to relatively younger ages at death, the second highest percentage of total years of life lost (30%). The SEAR exceeds the global average annual mortality rate for all three broad cause groupings—communicable, maternal, perinatal and nutritional conditions (334 vs 230 per 100 000); non-communicable diseases (676 vs 573 per 100 000); and injuries (101 vs 78 per 100 000). Poverty, education and other social determinants of health are strongly linked to inequities in health among SEAR countries and within socio-economic subgroups. India, Thailand and Bangladesh produce two-thirds of epidemiology publications in the region. Significant efforts to increase health workforce capacity, research and training have been undertaken in the region, yet considerable heterogeneity in resources and capacity remains.
Conclusions Health systems, statistics and surveillance programmes must respond to the demographic, economic and epidemiological transitions that define the current disease burden and risk profile of SEAR populations. Inequities in health must be critically analysed, documented and addressed through multi-sectoral approaches. There is a critical need to improve public health intelligence by building epidemiological capacity in the region.
Keywords: Epidemiology, South-East Asia region, research capacity, training capacity, social determinants, workforce
Introduction
This article is part of a series commissioned by the International Epidemiological Association (IEA) for all World Health Organization (WHO) regions, to provide an overview of the state of health and epidemiology in the South-East Asia region (SEAR). The purpose of the series is to describe the state of health and epidemiology for: strategic planning purposes of the IEA; use by government and non-governmental organizations (NGOs) involved in epidemiological training, research and capacity building; and the general interest of readers of this journal. In this article, we describe the mortality, morbidity, risk factors and social determinants of health associated with SEAR countries, as well as the epidemiological capacity and output in the region.
There are 11 countries in the WHO SEAR—Bangladesh, Bhutan, Democratic People's Republic of Korea (DPRK), India, Indonesia, the Maldives, Myanmar, Nepal, Sri Lanka, Thailand and Timor-Leste. The member countries of the WHO SEAR bear a disproportionate burden of disease, with 25% of the world's population (Table 1) and 30% of the global disease burden.1 Government spending on health care (as a percentage of gross domestic product) in SEAR varies widely from 2.2% in Indonesia to 13.6% in Timor-Leste (Table 1). The annual population growth rate for the region is currently estimated at one-half (1.24, 2005–10) of its peak growth rate, which occurred during the 1960s (2.51, 1961–70)2—with significant between-country variations for 2005–10 (0.3 = DPRK; 3.33 = Timor-Leste). One-third of SEAR residents are living in urban areas.3 The health workforce in the region also varies considerably from 3 physicians, 2.7 nurses and 4 hospital beds per 10 000 in Bangladesh to 32.9 physicians, 41.2 nurses and 132 beds in DPRK.3
Table 1.
Demographic, economic and health profiles for countries in the SEAR (2008)
| Category | Indicators | Thailand | Bangladesh | Bhutan | India | Maldives | Nepal | Sri Lanka | Timor-Leste | DPRK | Myanmar | Indonesia | World | High income |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population growth | Total (million) | 67 | 160 | 0.7 | 1140 | 0.3 | 28.8 | 20 | 1 | 24 | 50 | 227 | 6697 | 1069 |
| Annual growth (%) | 0.5 | 1.4 | – | 1.3 | – | 1.7 | 0.7 | 3.3 | 0.3 | 2.1 | 1.2 | 1.1 | 0.5 | |
| >65 years (% total) | 7 | 4 | 5 | 5 | 4 | 4 | 7 | 3 | 9 | 5 | 6 | 7 | 15 | |
| Economy | GNI/ capita | 3670 | 520 | 1900 | 1040 | 3640 | 400 | 1780 | 2460 | – | – | 1880 | 8654 | 39 687 |
| Annual growth GDP (%) | 2.5 | 6.2 | 13.8 | 6.1 | 5.2 | 5.3 | 6 | 13.2 | 1.7 | 12.7 | 4.8 | 1.7 | 0.5 | |
| Health financing | Total expenditure on health (% GDP) | 3.7 | 3.4 | – | 4.1 | – | 5.1 | 4.2 | 13.6 | 3.6 | – | 2.2 | 9.7 | 11.2 |
| General government expenditure on health (% total) | 73.2 | 33.6 | – | 26.2 | – | 39.7 | 47.5 | 84.6 | 83.7 | – | 54.5 | 59.6 | 61.3 | |
| Per capita total expenditure on health (USD) | 136 | 15 | – | 40 | – | 20 | 68 | 58 | 22 | – | 42 | 806 | 4406 | |
| Development | HDI (Index, rank) | 0.654 (92) | 0.469 (129) | – | 0.519 (119) | 0.602 (107) | 0.428 (138) | 0.658 (91) | 0.502 (120) | 0.877 (12) | 0.451 (132) | 0.600 (108) | 0.624 | – |
Source: The World Bank, World Development Indicators 2010.
Original data sources include WHO, UNICEF, UNFPA and WHO National Health Accounts (Health Financing data).
GDP, gross domestic product; GNI, Gross National Income; US, Unites States; HDI, Human Development Index.
Methods
The most recent global and regional data were used to summarize the descriptive epidemiology of mortality, disease burden, risk factor contribution, inequalities, public health and epidemiological capacity. For discrepancies between national and international estimates, country-level experts were consulted and both sets of estimates were provided (e.g. Table 2). Medline-indexed peer-reviewed journal articles were searched in ‘PubMed’ (http://www.ncbi.nlm.nih.gov/pubmed/) to quantify epidemiological research output from the 11 SEAR countries. Regional WHO conference proceedings and publications, and key informants were used to provide overviews of epidemiological education, training, research capacity, funding and workforce in the SEAR.
Table 2.
Life expectancy and mortality rates, using international and national (in parentheses) data sources, in SEAR countries compared with global data
| Country/region | Life expectancy (years) | Healthy life expectancy (years) | Neonatal mortality ratea | Infant mortality ratea | <5-year-old mortality ratea | Adult mortalityb | Maternal mortalityc |
|---|---|---|---|---|---|---|---|
| Bangladesh | 65 (65) | 56 | 30 (41) | 41 (53) | 52 (88) | 234 | 340 (380) |
| Bhutan | 63 (66) | 55 | 34 | 52 (40) | 79 (61) | 228 | 200 (255) |
| DPRK | 70 (68) | 59 | 18 | 26 (21) | 33 (46) | 167 | 250 (97) |
| India | 65 (65) | 56 | 34 (37) | 50 (57) | 66 (85) | 212 | 230 (301) |
| Indonesia | 68 (69) | 60 | 19 (20) | 30 (32) | 39 (46) | 190 | 240 (307) |
| Maldives | 75 (73) | 64 | 8 (8) | 11 (12) | 13 (16) | 84 | 37 (72) |
| Myanmar | 64 (60–64) | 50 | 33 (40) | 54 (50) | 71 (67) | 231 | 240 (380) |
| Nepal | 67 (61) | 55 | 26 (34) | 39 (48) | 48 (61) | 196 | 380 (281) |
| Sri Lanka | 71 (73) | 63 | 9 | 13 (11) | 16 (16) | 182 | 39 (47) |
| Thailand | 70 (69) | 62 | 8 (10) | 12 (24) | 13 (28) | 205 | 48 (14) |
| Timor-Leste | 67 (58) | 53 | 27 (32) | 48 (98) | 56 (140) | 195 | 370 (420–800) |
| SEAR | 65 | 57 | 31 | 45 | 59 | 209 | 240 |
| Global | 68 | 59 | 24 | 42 | 60 | 176 | 260 |
| Low income | 57 | 49 | 36 | 75 | 117 | 321 | 580 |
| Lower middle income | 68 | 61 | 26 | 42 | 57 | 176 | 230 |
| Upper middle income | 71 | 61 | 11 | 19 | 22 | 184 | 82 |
| High income | 80 | 70 | 4 | 6 | 7 | 88 | 15 |
aPer 1000 live births (Source: World Health Statistics 2011, WHO Regional Office for South-East Asia and 11 Health Questions about the 11 SEAR Countries, WHO 2007, in parentheses).
bPer 1000 live births (Source: World Health Statistics 2011, WHO Regional Office for South-East Asia and 11 Health Questions about the 11 SEAR Countries, WHO 2007, in parentheses).
cPer 100 000 live births (Source: World Health Statistics 2011, WHO Regional Office for South-East Asia and 11 Health Questions about the 11 SEAR Countries, WHO 2007, in parentheses).
Descriptive epidemiology
Life expectancy, mortality and morbidity
SEAR countries are in a state of epidemiologic transition4 whereby traditional infectious diseases, such as diarrhoea and pneumonia, co-occur with non-communicable diseases (NCDs), such as cardiovascular diseases (CVDs), diabetes and mental disorders. If the rising mortality due to injuries is also considered,4 these countries face a triple burden of mortality and morbidity resulting from communicable diseases (CDs), NCDs and injuries. This is reflected by the high age-standardized mortality rates for all these conditions in the SEAR as compared with the global and high-income country averages (Figure 1). The SEAR has experienced the highest percent increase of all WHO regions in life expectancy at birth from 1990–2009 (59–64 years for males and 59–67 years for females).3 Yet, compared with other WHO regions, individuals of SEAR countries are relatively younger and face a lower life expectancy (65 years) than the global average (68 years).5 There is also wide variation within the region, ranging from life expectancy of 64 years in Myanmar to 75 years in the Maldives (Table 2).3
Figure 1.
Age-standardized mortality rates for CDs, NCDs and injuries in SEAR countries compared with averages for the world and high-income countries. Source: World Health Statistics 2011, WHO
Nearly one-third of the world's child deaths occur in the SEAR, where the median level of child mortality (59 per 1000 live births, 2009) is >8 times greater than that of high-income countries (7 per 1000 live births, 2009; Table 2). Three-fourths of these deaths are due to diarrhoeal diseases, pneumonia and neonatal conditions.3 Average neonatal and infant mortality rates in the SEAR (31 and 45 per 1000 live births, respectively) are also higher than the global averages (24 and 42 per 1000 live births, respectively).3 Rates of <5-year-old mortality, of which 68% are attributable to infectious diseases,6 have been declining in the region (Figure 2) and countries such as Sri Lanka and Thailand, have already shown progress towards reaching millennium development goal (MDG) of 4 (16 and 13 per 1000 births, 2009, respectively).3
Figure 2.
Trends in infant and <5-year-old mortality rates among 11 SEAR countries from 1990–2009 for meeting MDG 4. Source: World Health Statistics 2011, WHO
More than one-fifth of the world's adult (15–59 years) mortality burden was due to CDs occurring in the SEAR.4 The top three contributors were lower respiratory infections (24.8%), diarrhoeal diseases (12.1%) and tuberculosis (9.6%). HIV/AIDS accounts for only 3.7% of CD mortality in SEAR compared with 21.5% in Africa, where it is the primary cause of CD death.4 Although there is a wide variation in the maternal mortality ratio (MMR) in SEAR countries (Timor-Leste and Sri Lanka at 420 and 47 deaths per 100 000 live births, respectively, Table 2), the region as a whole has experienced a steep decline in the MMR (from 580 in 1990 to 240 in 2008 per 100 000 live births)7 towards meeting MDG 6. Moreover, there is wide variation between member SEAR countries. Whereas Myanmar, Timor-Leste and India have the highest mortality rates for CDs (461, 444 and 363 per 100 000, respectively), the Maldives and Sri Lanka have rates (59 and 79 per 100 000, respectively) closer to the European region (Figure 1).3 In 2010, 49 poliomyelitis cases were reported from SEAR (42/49 from India, which reported only 1 case in 2011),8 273 from the African region and no case from any of the other five WHO regions.3
NCDs account for the majority of mortality in the SEAR (50.4% in 2004), with cardiovascular disease contributing to half of these deaths (25.4% of all SEAR deaths, 2004).9 The highest rates in the region were observed in Bhutan (735 per 100 000) (Figure 1). Malignant neoplasms accounted for 15.5% of SEAR mortality in 2004.4 The SEAR has the second highest incidence of liver cancer in the world, in both men (6.7 per 100 000) and women (3.0 per 100 000).10 Cancers of the breast,1 cervix2 and colo-rectum3 rank as the most common cancers in women (26.1, 24.4 and 6.5 per 100 000, respectively), whereas cancers of the lung,1 lip and oral cavity2 and colo-rectum3 are most common in men (16.6, 8.4 and 7.4 per 100 000, respectively).10 Respiratory diseases, including chronic obstructive pulmonary disease and asthma, are the third largest contributor to NCD mortality (13.7%) in the region.4
Disability-adjusted life years (DALYs) estimate the burden of disease by measuring the gap between a population's ideal health and its current situation.5 When considering years of life lost in DALYs, the burden of disease in the SEAR was still greater for NCDs (44.1%) than for communicable, maternal, perinatal and nutritional conditions considered together (41.7%).4 The five most common conditions for the SEAR burden of diseases (percentage of total DALYs) in 2004 were lower respiratory infections (6.4%), diarrhoeal diseases (5.2%), ischaemic heart disease (4.9%), unipolar depressive disorders (4.8%) and prematurity and low birthweight (4.1%).4 Mental disorders play a large role in the global morbidity burden—unipolar depressive disorders are the leading cause of disease in women aged 15–44 years of all countries.4 In low- and middle-income countries, mental disorders are associated with 4 of the 10 leading causes for years of healthy life lost (YLD)—unipolar depressive disorders, alcohol use disorders, schizophrenia and bipolar disorders.4 Among NCDs in SEAR, neuropsychiatric disorders were the largest contributor to disability-adjusted life years (26.7%), more than CDs (21.5%).4
Nearly one-third of the world's morbidity and mortality burdens of injury-related disease occur in the 11 SEAR countries [29% (2004) and 30% (2008), respectively].9 The highest age-standardized mortality rates in the world are in the SEAR, where two-thirds of injury-related deaths are due to unintentional injuries, and where more than half a million deaths (58%) resulted from natural disasters in 1996–05.9 Injury-related mortality rates in the region range from 44 per 100 000 in children aged 10–14 years to 666 per 100 000 for adults ≥80 years.4 Overall, the age-standardized mortality rate for injuries is 101 per 100 000 in SEAR, with the highest rates observed in Myanmar (347 per 100 000; Figure 1).3
Risk factors
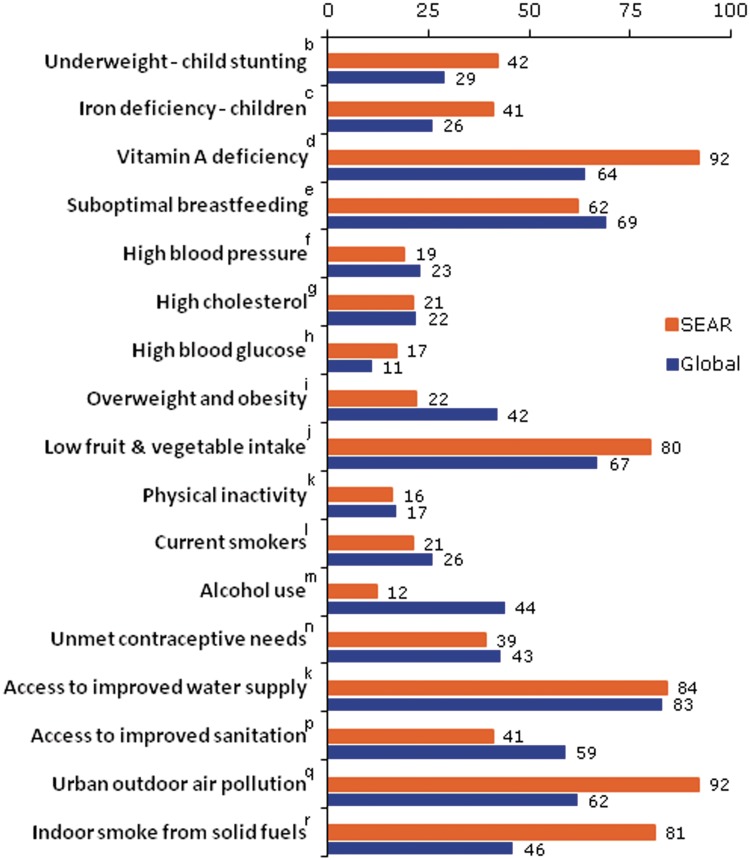
The leading risk factors contributing to disease burden (measured in DALYs) in the SEAR are underweight (7.8% of SEAR DALYs), unsafe water, sanitation and hygiene (4.6%), high blood pressure (3.0%), high blood glucose (3.0%) and suboptimal breastfeeding (2.9%).5 Over two-thirds of the world's malnourished children are living in 11 SEAR countries, where over one-quarter (27%) of children <5 years of age suffer from malnutrition.9 The underlying causes of undernutrition/prematurity (17%), pneumonia and other severe infections (50%) and diarrhoeal diseases (17%) account for more than two-thirds (68%) of <5-year-old mortality in the world.5 The regional prevalence of low birthweight is 18%, with wide variation in member countries from 7% in DPRK and 9% in Thailand to >30% in India and Bangladesh.9 Low birthweight and underweight arising from inadequate diet, frequent and severe infections and suboptimal breastfeeding are further compounded by vitamin and mineral deficiencies (e.g. iron, zinc and vitamin A) leading to high burdens of disease in children.5 In the SEAR, vitamin A deficiency is a serious public health problem among <5-year-old children; subclinical forms of vitamin A deficiency are seen in over one-fifth of children in Bangladesh and nearly one-third of children <5 years of age in Nepal.9 Anaemia affects >600 million South-East Asians, with 48% of pregnant women in the region estimated to be iron deficient.11
The highest incidence of diarrhoeal diseases in the world is observed in the SEAR (1276.5 million cases in 2004; 27.6% of 4620.4 million occurring globally)11 where unsafe water, sanitation and hygiene are the primary risk factors. Diarrhoeal diseases are the second largest contributor to DALYs in the SEAR, where 60% of the urban population and only 30% of the rural population have access to improved sanitation (2008).5 More than 13 million children in SEAR continue to die from vaccine-preventable diseases due to no/incomplete immunizations.9 Two-thirds of the world's deaths associated with indoor smoke pollution, including lower respiratory infections, chronic obstructive pulmonary disease and lung cancer also occur in low-income countries such as some SEAR member countries, where solid fuel is used for cooking by 87% of the population living in rural areas.5
Risk factors for chronic NCDs are rising rapidly in SEAR countries and afflicting much younger populations than in high-income countries. As a result, the loss of DALYs associated with diet-related risk factors—high blood pressure, high glucose, overweight and obesity, high cholesterol, low fruit and vegetable intake—and physical inactivity is now greater in SEAR member countries than in high-income countries.5 Figure 3 shows the prevalence of selected risk factors for major causes of morbidity and mortality comparing the SEAR with the global average.
Figure 3.
Prevalencea of selected risk factors comparing SEAR countries to the global averages. Source: Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks, Geneva World Health Organization 2009. aEstimates are for the population most relevant to the risk factor—alcohol, physical inactivity are for ages 15+ years; blood pressure, cholesterol, overweight and fruits and vegetables are for ages 30+ years; iron, vitamin A and underweight are for <5 years and females 15–44 years for lack of contraception. Many risk factors were characterized at multiple levels—here they are collapsed to show exposure or no exposure, or a selected level, or means or prevalence exceeding a commonly used threshold. bPrevalence of stunting defined as height for age >2 years standard deviations below the WHO reference standard for children aged 0–4 years. cIron deficiency anaemia defined in terms of blood haemoglobin level. dPrevalences were estimated based on the percentage of children <5 years old living in areas classified as vitamin A deficient based on population survey data for low plasma or tissue retinol levels and xerophthalmia, with information on coverage of vitamin A supplementation programmes. eNot exclusively breastfed to 6 months (%). fFor persons aged ≥30 years, systolic blood pressure ≥140 mmHg (%) gFor persons aged ≥30 years, 1 mmol/l = 38.7 mg/dl; 6 mmol/l = 232 mg/dl. hFor persons aged ≥30 years, 5.55 mmol/l = 100 mg/dl; 7 mmol/l = 125 mg/dl. iFor persons aged ≥30 years. Body mass index (BMI) is defined as weight (kg) divided by height (m) squared. jPersons aged ≥30 years, less than 5 servings per day (%). kPersons aged ≥15 yrs, inactive (%). lPersons aged ≥15 years. mPersons aged ≥15 years. Average serving assumed to correspond to 80 g. nProportion of women who want to prevent or space conception and are not using modern contraceptive methods. oProportion of the population with improved or regulated water supply. pProportion of the population with improved sanitation coverage or full sewage treatment. qConcentration of particles less 10 µm (µg/m3). rProportion using biofuel
The average increases in body mass index (BMI) for SEAR men and women from 1980–2008 [0.7 kg/m2 per decade (0.4, 1.1) and 1.0 kg/m2 per decade (0.5, 1.5)] is >50% greater than increases in the world averages [0.4 (0.2, 0.6) and 0.5 (0.3, 0.7)] for men and women, although the average levels are low compared with other regions.12 The effects of high BMI on mortality also occur at younger ages in SEAR countries compared with the world population (among deaths caused by high BMI, 40% occur in people <60 years old in SEAR countries vs 18% worldwide).5 High blood pressure is the most significant risk factor for mortality in the region (attributable deaths = 1 438 000 deaths) where the risk of dying from high blood pressure at any age is more than double that in high-income countries.5 High blood glucose is the second highest attributable risk factor for mortality in the SEAR (attributable deaths = 1 044 000 deaths) where mean fasting plasma glucose levels are amongst the highest in WHO regions, and where 54 million diabetics and an additional 63 million individuals are estimated to be living with impaired glucose tolerance.13 India alone contributes 40 million diabetes cases—the highest number of diabetics in the world.
Tobacco use is the third most important cause of mortality in SEAR countries, where 39.4% of adult males smoke some type of a tobacco product (attributable deaths = 1 037 000 deaths).3 There is wide variation of tobacco use within the region however, from 2.1% in Sri Lankan females to 27.9% in Nepalese women.3 The highest prevalence in the region is observed in Indonesia, where two-thirds of adult men report using tobacco (61.7%, 2006).3 Recently released data from the global adult tobacco survey (GATS) conducted in 14 countries in 2008–09 are available for several SEAR member countries, including Bangladesh and Thailand,14 where there are high rates of tobacco use among males (58.0 and 46.4%, aged >15 years, respectively) but more variation among females (28.7 and 9.1%, aged >15 years, respectively). In both countries, Bangladesh and Thailand, smokeless tobacco is more common in females (27.9 and 6.3%) than males (26.4 and 1.3%, respectively).15 The impact of tobacco use includes both chronic diseases and infectious diseases and in countries such as India, has a larger impact on mortality for tuberculosis than that for other respiratory diseases (38% of tuberculosis deaths vs 31% of respiratory disease deaths associated with smoking).16 Alcohol consumption is a significant contributor to worldwide mortality, with 2.3 million estimated to die from alcohol-related causes.9 Alcohol consumption also varies widely in the SEAR, with very low rates in Bangladesh to >50% of males consuming alcohol in Nepal, Thailand and Sri Lanka, and alcohol dependence reported for 19.4 and 25% of the populations in Thailand and Nepal, respectively.9
Recent evidence on early life determinants of chronic disease suggests that low birthweight and nutritional deprivation followed by rapid weight gain, physical inactivity and other factors associated with the gestational period and infancy may increase the risk of NCD outcomes, such as CVD and diabetes.17 Moreover, NCDs such as diabetes can increase the risk of traditional infectious diseases affecting SEAR populations, such as tuberculosis,18,19 highlighting a confluence of risk factors that puts SEAR populations at very high risk of both CDs and NCDs.
Social determinants of health
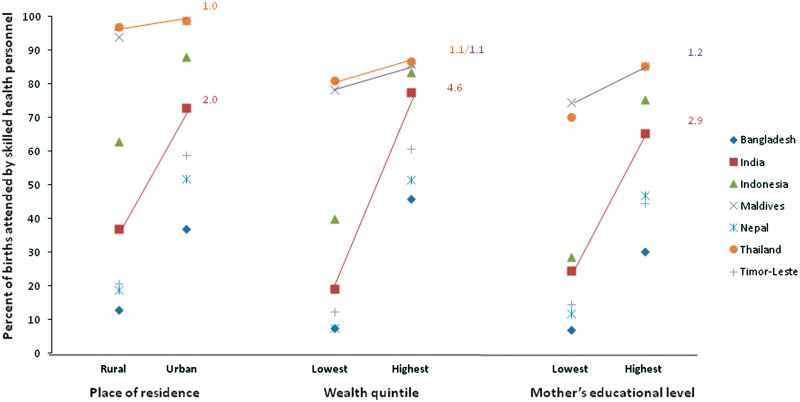
SEAR member countries host 40% of the world's poor, who face multiple challenges including poverty, education, unemployment, gender inequalities, access to safe drinking water and sanitation, migration, urbanization and globalization.20,21 The inequalities that stem from these social and economic challenges are important social determinants of health (SDH) that are linked to gross health inequities between and within SEAR member countries, with the exception of Thailand and Sri Lanka, which have nearly universal coverage of basic health services.20–22 The richest quintile of the populations in Nepal and Bangladesh are 12.03 and 10.3 times more likely, respectively, to have a skilled birth attendant at delivery than the poorest groups in these populations (Table 3).3 Children in the poorest quintile in India are three times more likely to die before their fifth birthday than children in the richest 20% of households.21 Measles immunization coverage was two times higher in the richest quintile in India, but the difference was only 30% and 10% higher in Sri Lanka and Bangladesh, respectively, when compared to the poorest quintile. Furthermore, reversal of the social gradient has been noted among chronic diseases, whereby the prevalence of cardiovascular risk factors (e.g. tobacco use, elevated blood pressure) and CVD is greater among the lowest socio-economic groups, who bear a disproportionate share of the burden.23–27 A social determinant perspective beyond the biomedical model of disease is important for addressing the triple disease burden afflicting SEAR populations. The socio-economic and political context, the socio-economic position, intermediary determinants and health systems factors have been described as four broad domains in the pathway towards health inequities.20 For example, one analysis on maternal and infant mortality rates, which are highly correlated with the presence of a skilled birth attendant, found that health system factors contributed to 19–26% (Indonesia and Nepal) of the inequities, whereas socio-economic position accounted for 53–58% (Bangladesh and Nepal) and socio-economic, political context for another 19–23% (Indonesia and Nepal).21 Interestingly, the inequities in skilled birth attendants in Thailand and Sri Lanka are low (where 97 and 96% of deliveries with skilled birth attendant, respectively), despite large inequities in wealth, because of policies that have provided near-universal coverage of maternal services in both these countries.21 Ultimately, the root causes of maternal, newborn and child mortality lie in gender inequality, education disparities, high fertility rates, low levels of awareness and health care access, especially among adolescent girls.22 When we compared mother's education, geographical location and household wealth among countries in the SEAR, we found the least health inequities in Thailand and the Maldives (Figure 4), which also had the lowest IMR and MMR rates in the region.
Table 3.
Health workforce in SEAR member countries
| SEAR countries | Physiciansa | Nursesa | Public health workersa | Community health workersa | Hospital bedsa |
|---|---|---|---|---|---|
| Bangladesh | 3.0 | 2.7 | 0.4 | 3.3 | 4.0 |
| Bhutan | 0.2 | 3.2 | 0.4 | 0.9 | 17.0 |
| DPRK | 32.9 | 41.2 | – | – | 132.0 |
| India | 6.0 | 13.0 | – | 0.5 | 9.0 |
| Indonesia | 2.9 | 20.4 | 0.3 | – | 6.0 |
| Maldives | 16 | 44.5 | – | 13.8 | 26.0 |
| Myanmar | 4.6 | 8.0 | 0.4 | 0.6 | 6.0 |
| Nepal | 2.1 | 4.6 | 0.1 | 6.3 | 50.0 |
| Sri Lanka | 4.9 | 19.3 | 1.1 | – | 31.0 |
| Thailand | 3.0 | 15.2 | 0.4 | – | 22.0 |
| Timor-Leste | 1.0 | 21.9 | 0.3 | 0.1 | – |
| SEAR | 5.4 | 13.3 | – | 0.9 | 11.0 |
| World | 14.0 | 29.7 | – | 4.0 | 29.0 |
Source: World Health Statistics 2011, WHO.
aPer 10 000 population.
Figure 4.
Health inequities in SEAR: births attended by skilled health personnel in SEAR countries according to geographical residence, wealth and mother’s education (higher ratios and steeper slopes indicate greater health inequities). Source: World Health Statistics 2011, WHO
In SEAR countries, health inequalities cannot be adequately addressed without a ‘beyond health’ approach that involves multiple sectors of society. A successful example of infant mortality reduction that reached beyond the borders of health is the maternal and child health programme (MCH) in Bangladesh, which had broad-reaching policies, was universally accessible, empowered women through education and has been linked to improving young female survival in the poorest of households.28 This is reflected in less inequity between the poorest and richest quintiles for <5-year-old mortality rates (e.g. the ratio is <2 in Bangladesh and Sri Lanka), whereas India and Indonesia have a >3-fold difference.21 Other studies have shown the importance of income inequality in influencing health outcomes, including infant mortality, childhood dental caries, self-rated health and eye health disparities.29–32 The WHO Commission on Social Determinants of Health outlines three recommendations for closing the gap in health inequities: (i) improve daily living conditions; (ii) tackle the inequitable distribution of power, money and resources; and (iii) measure and understand the problem and assess the impact of action.33 In the SEAR, social challenges that accelerate health inequities must be encompassed in an approach that creates partnerships across multiple sectors of society to change the social and physical landscape that impacts on the health of its individuals.
Peer-reviewed epidemiological publications
We searched for recent peer-reviewed publications in ‘PubMed’ http://www.ncbi.nlm.nih.gov/pubmed/, with ‘epidemiology’ as a MeSH heading or ‘epidemiol*’ in the title or abstract, with countries in the SEAR either included as a MeSH heading or appearing in the title or abstract from 1 January 2000 to December 2010. Of all the peer-reviewed ‘epidemiology’ publications in ‘PubMed’, <5% (25 344/727 394) is from the SEAR. Whereas India contributes to more than a half (54.9%) of peer-reviewed epidemiology publications within the region, another 20.5% is published from Thailand and 6.8% from Bangladesh (Figure 5). The number of publications is likely underestimated by these search criteria as specific cities and/or institutions may be listed instead of a country in the abstract, title or MeSH heading, but represents the relative contribution of published output within the 11 member countries of the region. For all 11 countries in the region, a review of 2010 peer-reviewed publication topics showed that the majority of published material was focused on areas of infectious disease and maternal and child health (Figure 5) with a disproportionately low research output on injuries compared with the actual burden. Within the region, Sri Lanka, Thailand and India had the highest proportion of NCD publications in 2010 (Figure 5). NGOs also play an important role in epidemiological research output in the SEAR; a 10% random sample of December 2010 ‘PubMed’ publications for the region yielded 25.8% of the publications from private or non-governmental institutions.
Figure 5.
Epidemiological published literature for 11 member countries of the SEAR
Epidemiological education, training and research
A regional assessment in the year 2000 highlights a serious lack of appropriate public health or epidemiology training opportunities in most of the SEAR member countries.25 Although there are only 12 schools of public health for a population of >1.5 billion in the SEAR, there are multiple models of public health training that have emerged in the region, including the Rockefeller Foundation-supported Public Health Schools Without Walls initiative (PHSWOW), Field Epidemiology Training programmes (FETPs) and Training Programmes in Epidemiology and Public Health Interventions Network (TEPHINET). The International Clinical Epidemiology Network (INCLEN) for improving the epidemiological skills of clinicians and the Centre for Disease Control (CDC) programme on Management for International Health are other initiatives in the region with the objective to improve epidemiology research outputs based on the prevailing disease burden of the member countries. Supplementary Table 1 (available at IJE online) lists the programmes/institutions that offer epidemiological training and education for the 11 SEAR member countries in the region.
Three broad categories of epidemiology training exist in the region. The first includes long-term epidemiology training, including Master's and Doctorate programmes in clinical, field and applied epidemiology, and currently exist in Thailand, India, Indonesia, Bangladesh, Myanmar and Nepal.34 These also include FETPs available in 3 of the 11 SEAR countries (India, Indonesia and Thailand),35 which have classroom-based learning and field-based assignments with a wide variation in time spent doing fieldwork (15–75%). Higher degrees of epidemiology and public health are available at 8 of the 11 member SEAR member states. The second category includes short-term training that is based in organizations, including WHO collaborating institutions and ranges from 5 days to 3 months, with many being hosted by the University of Gadha Madah in Indonesia, FETP in Thailand and the National Institute of Communicable Diseases and National Institute of Epidemiology, Chennai in India. The third type of training is a course in epidemiology as part of a graduate and post-graduate training in preventive and social medicine or diploma programmes in community medicine and public health (excluding MBBS programmes that offer epidemiology/public health training, which produce large numbers of public health physicians).
The South-East Asian Public Health Education Institutes Network (SEAPHEIN) was launched in 2004 to collaborate with member countries in the region to improve and sustain the quality and relevance of public health education and has >35 member institutions. Newer FETP programmes in states such as Myanmar and Nepal are a demonstration of the emphasis given by governments in the region, but a critical mass of epidemiologists has not been reached; enrolment capacity is often unfulfilled and more training is required.
Health workforce and health systems
Human resources for health encompass all individuals whose primary responsibilities are to protect and promote the health of the population, including physicians and nurses, community-based health workers and volunteers, researchers, trainers, administrators and health educators. The per capita number of physicians and nurses in the SEAR is comparatively low at 5.4 and 13.3 per 10 000 compared with 28.6 and 78.6 per 10 000 in high-income countries, respectively (Table 3).3 Within SEAR member countries, the number of physicians ranges from <0.5 per 10 000 in Bhutan to 32.9 per 10 000 in DPRK.3 With existing strong community values and customs in SEAR countries, nearly all members of SEAR have utilized community participation—community-based health workers (CBHW) and volunteers (CHV)—to supplement existing health systems, empower local populations and to practise community-based health.36 Although there was a rapid expansion of this community-based system in many SEAR member countries during the 1980s,37 it was not sustainable, leading to a shortage of CBHWs and CHVs and contributing to the overall shortage of health care workers in the region, which is associated with many SEAR countries falling short of the MDGs.37
Strengthening the health workforce is one aspect of health systems strengthening, which is also dependent on health services delivery, leadership and governance, health financing, health information systems, management of medical products and other logistical supplies as well as monitoring and evaluation.38 One common focus of health systems development in the region has been to reinvigorate primary health care (PHC) at the district level38 as a means of improving key health outcomes, including MDGs 4, 5 and 6. Most countries in the region have taken steps towards a PHC strategy, including the decentralization of essential health care services to PHC centres (Nepal), the scaling up of accessibility and coverage of primary health care (Sri Lanka), the strengthening and re-financing of systems to remote rural levels (India, Thailand and Bangladesh) and a renewed focus on quality of services (Bhutan).38 Despite these efforts, there are challenges common to many of the countries, including lack of meaningful political support and financial resources, inappropriate skill mixes in the existing health workforce, increasing out-of-pocket health care expenditures, inadequate community involvement and collaboration between sectors and poor health information systems.38
Health statistics
Building epidemiological capacity relies on valid health statistics to develop an evidence base for planning and prioritizing health resources and interventions. The accuracy and timeliness of reporting and synchronization of data from local, subnational and national-level data sources are required for policy makers to identify health needs of the population. The analysis and dissemination of these data are also underutilized. Regional experts from SEAR determined that several factors were common to most countries with respect to building epidemiological capacity, including poor timeliness in reporting (Bangladesh, the Maldives and Sri Lanka), difficulties in engaging the private sector to contribute health statistics (Bangladesh and Nepal), limited support for analysis and dissemination (Bangladesh, Bhutan, Indonesia and Sri Lanka), low emphasis on NCDs (Bhutan), lack of comprehensive vital registration systems and underreporting (Bhutan and Sri Lanka), decreased user friendliness (Timor-Leste), underutilization of data for planning (Indonesia) and need for capacity building (Indonesia, the Maldives and Nepal).38 North Korea and Sri Lanka regularly provide updated health statistics categorized under broad headings that are being well utilized for health planning. Cause of death estimation is weak in the region with only one member state having vital registration data with at least 85% coverage4—the lowest of the WHO regions in the world. Furthermore, there are serious concerns about the quality of information on the cause of death, as a low proportion of deaths have medical attention at death. A wide variation in registration process both within and across countries, inadequate registration infrastructure and inadequate inter-sectoral collaboration between different agencies involved in vital status registration are important challenges in obtaining accurate mortality statistics in the region. Experts suggest that countries in the SEAR should focus on producing key health statistics, especially mortality and its causes.38
Limitations
The data presented in this article were retrieved from global reports on various parameters of health, but may have been missing for certain countries. For example, important data on social determinants of health (e.g. Gini coefficient) were not available from UN sources for the DPRK, and for certain health outcomes (e.g. MDGs) (Table 2), available WHO and country-level data were materially different. National surveys may yield estimates very different from international surveys, and we consulted country-level experts where there were discrepancies and provided both sets of estimates (international and country-level; Table 2), but our report is limited to the extent that missing data or discrepancies in national- and international-level estimates exist. Comparing rates across countries should be made with caution, especially with wide variations in population sizes (India: 1.19 billion and the Maldives: 309 000, 2009)3 that influence stability of estimates.
Future challenges
The SEAR is experiencing an epidemic of chronic NCDs, with disadvantaged populations the hardest hit. Health care systems in member countries of the region need to be redesigned to deliver chronic care alongside short-term care for infectious, maternal and childhood diseases. Although maternal and child mortalities are declining in the SEAR, there are still major disparities, and greater equity across all sectors is the key to a sustainable achievement of the MDGs. In addressing the upstream determinants of health, non-health sectors such as education, labour, trade, agriculture, water and sanitation, public works and housing must be engaged in partnerships.
Overall, SEAR countries had fewer persons living with HIV in 2009 than in 1990; the number of new HIV infections decreased by nearly one-third (31%) between 2001 and 2009 in countries such as Thailand, Myanmar and India and remained low for countries such as Nepal, Sri Lanka, Bangladesh, Bhutan and the Maldives.39 In Indonesia however, the HIV incidence continues to rise39 and recent evidence suggests that along with the rising burden of NCDs, HIV/AIDS may explain the gaps in achieving MDGs in some SEAR member countries.40
Regional challenges in controlling existing and emerging infectious diseases are formidable and range from influencing the factors that drive disease emergence to making surveillance systems fit for purpose and ensuring that regional governance mechanisms work effectively to improve control interventions. Epidemiologists in academic, non-government and government-sponsored institutions should provide multiple channels for evidence-based research to influence informed policy. The SEAR is also a hotspot for emerging infectious diseases, including those with pandemic potential, and along with antibiotic resistance, needs better monitoring and communication systems in the region. This underlies the need for inter-country networks and cross-border collaboration in surveillance and response systems to reduce common threats,41 and places a greater burden on the region in responding to potential public health emergencies of international concern with adequate early notification, verification, assessment and public health response systems.42
Improving health indicators for the region also relies on the epidemiological research output from member countries of the SEAR and on conducting well-planned health research according to the prevailing health situation, and triple burden of disease, in the member countries. Our review of the literature suggests disproportionately low published output and areas of research that are not a reflection of actual burden of disease in the SEAR and among its member countries. Evidence-based health policy and practices in the region require a critical mass of epidemiologists to influence change;43 further training and education are required on the proper collection and uses of surveillance data regarding diseases afflicting the SEAR.44 Moreover, a trained workforce available for the routine collection and analysis of reliable, valid data could reduce large discrepancies between country-level and international statistics. For the region, the importance of climate change, emerging diseases and social determinants of health underscore the need for epidemiologists to focus on the social, ecological, psychological and economic aspects of diseases rather than just the physical. Epidemiological training at introductory and advanced levels is required for the development and enhancement of research capacity in low- and middle-income countries, including member states of the SEAR. Increased collaborations in education, training and capacity building should be encouraged to address common gaps, resource shortages and cultural environments for member states in the region.
Out-of-pocket health spending varies widely in the SEAR (e.g. 2% in Bhutan to 81% in Myanmar, 2007)20 and future initiatives should focus on universal health coverage to reduce inequities and financial barriers, especially for vulnerable groups. Recognizing the Commission of SDHs ‘beyond health’ approach for addressing the socio-economic factors that contribute to the inequities driving the health gaps will be necessary for strengthening health promotion, primary health care, health systems and responsiveness to emergencies and epidemics.20 Countries in the SEAR also have existing community values and customs that can be utilized for community-based action, advocacy, inequity reduction, including community health workers who can help address a severe shortage of health care workers41 in the region, and at the same time empower communities to participate in improving their own health.
A concentrated action is needed by policy makers, researchers and public health professionals and other stakeholders to address these challenges.
Supplementary Data
Supplementary Data are available at IJE online.
Funding
Wellcome Trust Capacity Building Grant (EPNCBD67, P.K.D); Wellcome Trust Capacity Strengthening Strategic Award to the Public Health Foundation of India and a consortium of UK universities (P.J.); National Heart Lung and Blood Institute, USA (HHSN286200900026C) and National Institute of Health, USA (1D43HD065249) research grants (D.P.).
Supplementary Material
Acknowledgements
We wish to acknowledge Prof. Shah Ebrahim, Director, South Asia Network for Chronic Disease (SANCD), Public Health Foundation of India (PHFI), New Delhi, India for his insightful comments on this article. We would like to thank Rajesh Mishra and Geetha Nambiar for their invaluable assistance with searches on epidemiological peer-reviewed literature in the region (SANCD, PHFI, India). D.P. developed the idea, corresponded with key experts in the region and oversaw, mentored and provided expertise on all aspects of the research and manuscript writing process. P.K.D. and P.J. conducted the research, writing and drafting of tables and figures. N.K.A. and P.M. provided insightful input on epidemiological status and training in the region; P.M., M.M., and R.D.S. offered expertise for their respective countries. All authors reviewed the final draft of the manuscript.
Conflict of Interest: None declared.
KEY MESSAGES.
There is a high burden of disease and mortality in SEAR countries.
Capacity to address this challenge in terms of human resources and infrastructure is limited and highly variable among SEAR countries.
Research output among SEAR largely comes from India, Thailand and Bangladesh.
There is a need to improve data gathering and surveillance, strengthen health management and information systems, build epidemiological capacity and address inequities in health in this region.
References
- 1.World Health Organization. 11 Questions About the 11 Sear Countries. New Delhi, India: World Health Organization; 2007. [Google Scholar]
- 2.United Nations. World Population Prospects 2006. New York: The United Nations; 2007. [Google Scholar]
- 3.World Health Organization. World Health Statistics 2011. Geneva: World Health Organization; 2011. [Google Scholar]
- 4.World Health Organization. Global Burden of Disease: 2004 Update. Geneva: World Health Organization; 2008. [Google Scholar]
- 5.World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva: World Health Organization; 2009. [Google Scholar]
- 6.Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Trends in Maternal Mortality: 1990 to 2008. Geneva: World Health Organization; 2010. [Google Scholar]
- 8.MMWR. Progress toward poliomyelitis eradication—India, January 2010—September 2011. MMWR Morbidity and Mortality Weekly Report. 2011;60:1482–86. [PubMed] [Google Scholar]
- 9.World Health Organization. Health Situation in South-East Asia Region 2001–2007. New Delhi, India: World Health Organization; 2008. [Google Scholar]
- 10.Ferlay JSH, Bray F, Forman D, Mathers C, Parkin DM GLOBOCAN 2008: 2008. Cancer Incidence and Mortality Worldwide. IARC CancerBase No. 10 2010 edn. Lyon: International Agency for Research on Cancer, 2008. [Google Scholar]
- 11.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 12.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Diabetes Federation. IDF Diabetes Atlas. Brussels: International Diabetes Federation; 2009. [Google Scholar]
- 14.Centers for Disease Control and Prevention. Cigarette Package health warnings and interest in quitting smoking—14 countries, 2008–2010. MMWR Morbidity and Mortality Weekly Report. 2011;60:645–51. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Differences by sex in tobacco use and awareness of tobacco marketing—Bangladesh, Thailand, and Uruguay, 2009. MMWR Morbidity and Mortality Weekly Report. 2010;59:613–38. [PubMed] [Google Scholar]
- 16.Jha P, Jacob B, Gajalakshmi V, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;358:1137–47. doi: 10.1056/NEJMsa0707719. [DOI] [PubMed] [Google Scholar]
- 17.Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 diabetes: a systematic review. JAMA. 2008;300:2886–97. doi: 10.1001/jama.2008.886. [DOI] [PubMed] [Google Scholar]
- 18.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldhaber-Fiebert JD, Jeon CY, Cohen T, Murray MB. Diabetes mellitus and tuberculosis in countries with high tuberculosis burdens: individual risks and social determinants. Int J Epidemiol. 2011;40:417–28. doi: 10.1093/ije/dyq238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Regional Consultation on Social Determinants of Health. New Delhi, India: World Health Organization; 2005. [Google Scholar]
- 21.World Health Organization. Health Inequities in the South-East Asia Region: Selected Country Case Studies. New Delhi, India: World Health Organization; 2009. [Google Scholar]
- 22.World Health Organization. Accelerating Progress Towards Achieving Maternal and Child Health Millennium Development Goals (MDGs) 4 and 5 in South-East Asia. Report No.: (SEA-CHD-7) New Delhi, India: World Health Organization; 2009. [Google Scholar]
- 23.Jeemon P, Reddy KS. Social determinants of cardiovascular disease outcomes in Indians. Indian J Med Res. 2010;132:617–22. doi: 10.4103/0971-5916.73415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta R, Kaul V, Agrawal A, Guptha S, Gupta VP. Cardiovascular risk according to educational status in India. Prev Med. 2010;51:408–11. doi: 10.1016/j.ypmed.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 25.Jain SC. Education and training—capacity building. J Health Pop Dev Ctries. 2000;3:39–42. [Google Scholar]
- 26.Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26(Suppl C):8C–13C. doi: 10.1016/s0828-282x(10)71075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kar SS, Thakur JS, Virdi NK, Jain S, Kumar R. Risk factors for cardiovascular diseases: is the social gradient reversing in northern India? Natl Med J India. 2010;23:206–09. [PubMed] [Google Scholar]
- 28.World Health Organization. The Regional Six-Point Strategy for Health Systems Strengthening Based on the Primary Health Care Approach. Report No.: (SEA-HSD-305) New Delhi, India: World Health Organization; 2007. [Google Scholar]
- 29.Ono K, Hiratsuka Y, Murakami A. Global inequality in eye health: country-level analysis from the Global Burden of Disease Study. Am J Public Health. 2010;100:1784–88. doi: 10.2105/AJPH.2009.187930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernabe E, Hobdell MH. Is income inequality related to childhood dental caries in rich countries? J Am Dent Assoc. 2010;141:143–49. doi: 10.14219/jada.archive.2010.0131. [DOI] [PubMed] [Google Scholar]
- 31.Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z. Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ. 2009;339:b4471. doi: 10.1136/bmj.b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schell CO, Reilly M, Rosling H, Peterson S, Ekstrom AM. Socioeconomic determinants of infant mortality: a worldwide study of 152 low-, middle-, and high-income countries. Scand J Public Health. 2007;35:288–97. doi: 10.1080/14034940600979171. [DOI] [PubMed] [Google Scholar]
- 33.CSDH. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Epidemiology and Related Training Capacity in Selected Countries of South-East Asia Region. Report No.: (SEA-EPID 130) New Delhi, India: World Health Organization; 2009. [Google Scholar]
- 35.White ME, McDonnell SM, Werker DH, Cardenas VM, Thacker SB. Partnerships in international applied epidemiology training and service, 1975–2001. Am J Epidemiol. 2001;154:993–99. doi: 10.1093/aje/154.11.993. [DOI] [PubMed] [Google Scholar]
- 36.UNICEF. What Works for Children in South Asia: Community Health Workers. Kathmandu: United Nations Children's Fund; 2004. [Google Scholar]
- 37.World Health Organization. Strategic Directions for Strengthening Community-Based Health Workers and Community Health Volunteers in the South-East Asia Region. Report No.: (SEA-HSD-311) New Delhi, India: World Health Organization; 2008. [Google Scholar]
- 38.World Health Organization. Regional Workshop on Health Statistics Reporting. Report No.: (SEA-HI-47) New Delhi, India: World Health Organization; 2007. [Google Scholar]
- 39.World Health Organization ROfS-EA. HIV/AIDS in the South-East Asia Region: Progress Report 2010. New Delhi: World Health Organization; Regional Office for South-East Asia, 2010. [Google Scholar]
- 40.Stuckler D, Basu S, McKee M. Drivers of inequality in Millennium Development Goal progress: a statistical analysis. PLoS Med. 2010;7:e1000241. doi: 10.1371/journal.pmed.1000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization. Cross-Border Collaboration on Emerging Infectious Diseases. Report No.: (SEA-CD-166) New Delhi, India: World Health Organization; 2007. [Google Scholar]
- 42.World Health Organization. International Health Regulations (2005) Geneva: World Health Organization; 2008. [Google Scholar]
- 43.Joint Learning Initiative. Human Resources for Health: Overcoming the Crisis. Cambridge, MA: Harvard University Press; 2004. [Google Scholar]
- 44.Bhopal R, Macfarlane GJ, Smith WC, West R. Management Executive Committee for the XIXWCoE. What is the future of epidemiology? Lancet. 2011;378:464–65. doi: 10.1016/S0140-6736(11)61147-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.