What is the INDEPTH Network?
The International Network for the Demographic Evaluation of Populations and their Health (INDEPTH) Network is an umbrella organization for a group of independent health research centres operating health and demographic surveillance system (HDSS) sites in low- and middle-income countries (LMICs). Founded in 1998, it brought together a number of existing HDSS sites, and since then has encouraged newer HDSS sites to join.1
The purpose of this Editorial is to set the scene for a series of profiles from INDEPTH HDSS member sites, the first examples of which are published in this edition of IJE.2–5 All these profiles will follow a set pattern, to facilitate a systematic understanding of the multiplicity of HDSS sites involved in the Network and the various ways in which they are operated by their parent institutions. This Editorial therefore, follows the same general pattern as the individual profiles, but seeks to explore the epidemiological basis on which the HDSSs operate in general, and the role of the Network, rather than dealing with site-specific issues.
At the central level, the INDEPTH Network operates from its base in Accra, Ghana, as an international NGO and is also registered as a not-for-profit entity in the USA. The emphasis on the Network’s position as a Southern-led and -based organization was an important founding tenet, and this is very welcome in a world where vestiges of colonialism still occasionally surface in relation to health data and policy. Day-to-day operations are led by the Executive Director (O.S.), and governance and oversight are provided by an international Board of Trustees and a Scientific Advisory Committee (chaired by P.B.).
Why was the INDEPTH Network set up and what does it cover now?
The raison d’être behind the emergence of the Network was the apparently intractable lack of reliable population-based data on health across many LMICs in Africa, Asia and Oceania. Recognizing that there are no quick fixes in terms of achieving universal individual registration of populations in LMICs,6 the Network represents a medium-term attempt to break the link between material and data poverty.7 Epidemiology in many LMICs suffers from a dual lack of reliable population data and human capacity to make use of them. The immediate consequence is that health policy making often lacks its essential evidence base, with the possible effect of failing to use scarce resources effectively in some of the world’s poorest countries.
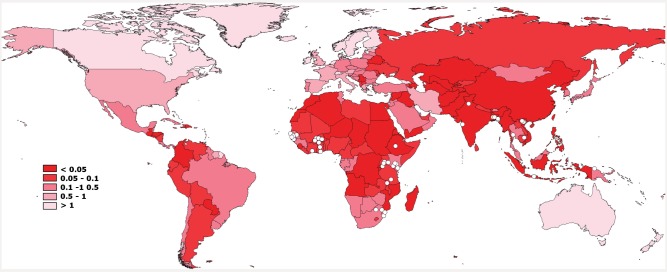
There are considerable global disparities in terms of epidemiological research output per population. Figure 1 shows the countries of the world shaded by a crude measure of this, namely the number of PubMed hits for a search on (‘epidemiology’ and <country>) per 1000 population. Much of Africa and Asia falls under the level of 0.05 per 1000, corresponding to rates which represent less than one-twentieth of some of the world’s leading countries in terms of epidemiological output. Superimposed on the map in Figure 1 are the current 43 HDSS sites run by 36 member centres of the INDEPTH Network. Although the locations of these sites are somewhat serendipitous, rather than being strategically planned, it is evident that there is considerable coverage across the areas of the world that lack substantial epidemiological output. Thus, it is clear that the INDEPTH Network, through these 43 sites in 20 countries, collectively following a population of 3.2 million people, does indeed offer possibilities for filling some of the global gaps in epidemiology.
Figure 1.
Countries of the world classified by PubMed citations for (‘epidemiology’ and <country>) per 1000 population, also showing the location of 43 HDSS site members of the INDEPTH Network (white dots)
Where are the INDEPTH HDSSs?
From the outset, the INDEPTH Network has operated by accepting as members already functioning independent health research centres that run HDSSs. Therefore, the Network has little influence over the locations or geographical distribution of member HDSS sites. However, since the concept of an HDSS would be somewhat irrelevant in countries with universal population registration, in practice there is self-selection of site locations in places where the lack of other reliable population-based data justifies the considerable effort involved in launching an HDSS. As is evident from Figure 1, this means that HDSS sites are located across Africa, Asia and Oceania, but by no means randomly. Several countries contain multiple HDSS sites, whereas many epidemiologically poor countries contain none.
What populations are covered by the HDSSs and how are they followed up?
HDSSs set out to collect epidemiological data (risks, exposures and outcomes) within a defined population on a longitudinal basis. In terms of Pearce’s classification scheme for epidemiological study designs,8 this places HDSSs as representing ‘the most comprehensive approach since they use all of the available information on the source population over the risk period’.
Unlike many epidemiological study designs, in which study participants are somehow selected to represent particular population subgroups, HDSSs generally set out to cover a real-life population and see what happens epidemiologically over a period of years and even decades. Issues of representativity and sampling are nevertheless critical considerations for all HDSSs, and need to be considered at the outset, when often little is known about potential target populations. Many HDSSs have started from intentions of covering an area that is at least subjectively thought to be typical of wider areas, maybe up to national levels. A chicken-and-egg situation arises, however, in that the motivation for having an HDSS is driven by a recognized lack of population-based health data, so that at the outset, very little may be known about candidate areas and maybe even less about the wider situation. There are no simple solutions to this conundrum.
Even after identifying a target area for an HDSS, there are a number of possible design considerations. A range of different sampling strategies can be used within the target area, that have both epidemiological and practical implications.9 In practical terms, one important consideration is whether the final population is defined as being within a contiguous area or in a collection of small areas (e.g. discrete villages) within a wider area. This has important logistic implications in terms of organizing and maintaining on-going surveillance, as well as affecting the definition of migration events (see below). The independent INDEPTH HDSSs naturally include a mixture of approaches to initially identifying target areas, within-area sampling and population contiguity.
The overall size of the population within an HDSS is a further important factor, as is the case in any epidemiological study. However, an HDSS is not a classic sample survey, and so determining the size of the target population is not straightforward. Size is of course driven by considerations of the rarest event(s) of interest, which for most HDSSs are mortality-related outcomes. If specific causes of mortality are of particular concern, then the overall population size needs to be based on numbers relating to the nth ranked cause of interest.10 Current INDEPTH member HDSS sites range in population size from tens of thousands up to around a quarter of a million. In most HDSSs the overall numbers are driven by mortality outcomes, with the result that surveillance of particular more common outcomes (such as morbidity and social measures) may in some situations be more effectively undertaken using a sample drawn from within the overall HDSS population.
During the life of the INDEPTH Network, the technological and methodological possibilities for obtaining and using geographical data have advanced considerably, to the point where recording the latitude and longitude of every residential unit, and other salient features, in an HDSS using global positioning system (GPS) technology have become commonplace.
Once an HDSS population is defined, an initial detailed census is usually undertaken to capture details of all residents and the social units in which they live. This usually involves assigning unique identifiers to all the residents and social units encountered in the census, using a numbering system that has sufficient capacity for expansion to reflect the addition of future residents and social units. It is not simple to arrive at generic definitions of social units across cultures and traditions, and individual HDSSs have to handle these issues in ways that make sense for their own context, both for physical structures (housing) and groups of inhabitants (families). INDEPTH has tried to standardize definitions as far as possible by publishing a resource kit for HDSS design on its website. This initial census then forms the basis of a database system that is updated on a regular basis to reflect the dynamic cohort of people living within the HDSS, as conceptualized in Figure 2. An important consideration is to determine the modality of the regular update rounds. Since HDSSs operate by definition in populations that are not otherwise enumerated, and generally have weak infrastructures, the norm is that local staff have to be recruited to undertake regular update visits to all the social units in the defined area. This forms a major component of the ongoing effort of running an HDSS, and consequently issues such as the frequency of update rounds need to be considered very carefully. Different INDEPTH HDSSs use various update frequencies, from one to four annual rounds. Certain types of events, e.g. neonatal mortality, are likely to be particularly sensitive to recall bias, which in turn is related to update frequency. Thus, it tends to be the case that more frequent updates are needed in high mortality or high migration settings, whereas in societies that are more stable, or at later stages of demographic transition, less frequent updates may prove adequate.
Figure 2.
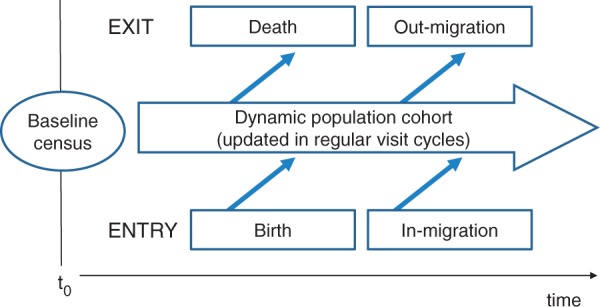
Conceptual structure of the dynamic cohort model used by INDEPTH Health and Demographic Surveillance System (HDSS) sites
What is being measured and how are the HDSS databases constructed?
Having set up an HDSS, the next challenge is to track the progress of the dynamic cohort shown in Figure 2 by regularly updating a series of core parameters, detailed below. Naturally, the operation of an HDSS is not confined only to these core activities, and most HDSSs will have specific agendas defining what other parameters they may need to handle, e.g. in relation to the epidemiology of specific diseases, the execution of clinical trials, monitoring the effectiveness of health systems and other important issues that can be built onto the basic HDSS platform.
Social units
Keeping track of social units is a challenging issue, since it involves both physical structures (that can be newly built, in existence or be demolished) and the family groups associated with physical structures (that can migrate in or out as complete groups, or particular individuals can migrate to join or leave a group). In some cultures the physical structures may be large and complex compounds, perhaps housing up to 100 people and possibly containing subunits based on a polygamous social structure. At the other end of the spectrum, nuclear families may occupy small, discrete dwellings. Many HDSSs also aim to gather data on socio-economic status, often reflected by a basket of parameters including details of the physical structure, as well as owning traditional and modern assets.
Births
Capturing details of new births is a critical function of any HDSS, since births form a major part of new entrants to the cohort and are critical to any analyses of fertility. In some settings, traditional behaviours around childbirth (e.g. going to stay at the maternal grandmother’s residence for the birth and neonatal period) may make births more difficult to record accurately. There is a particular difficulty around detecting early neonatal deaths, and separating these reliably from intra-partum stillbirths, and this becomes more difficult with less frequent update rounds.
Migrations
Tracking details of migration patterns is one of the most complex areas in HDSSs, fundamentally comprising people moving into the surveillance area, within the area and out of the area. Many of these complexities are reflected in INDEPTH’s monograph on migration.11 Every type of migration needs to be defined by rules (involving duration, intent, destination, etc.) which are appropriate to the population concerned. Some communities experience regular patterns of seasonal migration, related to employment or agricultural production. The possibility of multiple moves per individual over a period of time must be incorporated, and a further challenge can be the reliable re-identification of an individual on in-migration as being the same person who previously moved out. The design of an HDSS site in terms of the contiguity of the surveyed population is also important, since local moves in a non-contiguous population may be classified as in- and out-migrations, whereas similar moves in a contiguous area would amount to within-site migrations.
Deaths
Deaths, documented by age and sex, are a critical outcome measure for every HDSS and, in addition to reporting basic mortality rates, are an essential component in formulating life tables and other demographic measures for HDSS populations. As noted above, one of the most difficult issues involves reliably identifying early neonatal deaths.
Causes of death
Identifying the causes of death is a much more difficult issue in populations where most deaths do not occur in health facilities. The only realistic approach to attributing the cause of death is by carrying out verbal autopsy (VA) interviews with relatives or caretakers of deceased individuals, and then using those data to arrive at a likely cause of death. The INDEPTH Network was closely associated with developing a WHO standard instrument for VA interviews.12 In many HDSSs, interpretation of the VA data was done by giving the VA data to local physicians, often more than one per case, in order to arrive at a consensus cause. However, this is an expensive and time consuming process that is gradually being superseded for most purposes by the application of computer-based probabilistic models.13 INDEPTH is currently part of a new round of VA tool development in conjunction with WHO, which aims to simplify and shorten the VA process, as well as moving the scope of VA beyond research settings into non-enumerated populations.
Databases
Maintaining a database that reflects all the details of the population in a dynamic cohort is one of the most demanding tasks for most HDSSs, and a range of different approaches are used. The longitudinal nature of the HDSS data demands the use of relational database management systems (RDBMS) to handle the considerable volume of data involved over long periods of time. The basic principles of implementing an RDBMS for an HDSS have not changed fundamentally since the 1980s, when one of the longest-standing INDEPTH member HDSS sites made the transition to an RDBMS system.14 However, appropriate hardware and software resources have progressed through several generations of development in the meantime, and that is reflected in the current range of implementations across the INDEPTH Network. These include implementations built on proprietary RDBMS systems such as Microsoft FoxPro™, Microsoft Access™ and Structured Query Language (SQL), as well as generic systems made available for the use of HDSS sites, such as the Household Registration System from the Population Council,15 subsequently re-engineered as the paperless SQL-based ‘Open-HDS’. As commercial hardware and software specifications move on (e.g. Microsoft’s decision to cease supporting FoxPro™), long-term HDSS operations are sometimes forced to migrate their database operations onto new platforms, which is not a trivial matter for long-term databases linked to live surveillance.
Ethical issues
Running an HDSS over a long period raises a range of ethical issues that are different in some respects from those pertaining to many epidemiological studies. In the first place, the core HDSS data on vital events that are routinely collected in an HDSS population tend to be considered as research data, and subject to research ethics approval and informed consent, even though in countries that implement universal vital registration, it is regarded as a civic duty or even a legal obligation to provide such data. But, however population data are viewed, there are essential standards of confidentiality and anonymity that must be safeguarded. In HDSS data, there are three particularly critical types of data in this respect. Individual identities (whether by name or some other identifier) have to be protected at all stages of the process—from field interviewers observing adequate standards of confidentiality through database systems (and their backups) being held securely, to not revealing identifiers in any data sharing or outputs. Closely coupled with this, since HDSSs now commonly collect the GPS locations of households, it is important to also regard these data as confidential, since in principle they can be used to identify and locate households, and thereby their residents. Anonymizing GPS data is a much more difficult issue than simply removing names from a database.16 Third, HDSS databases typically accumulate a large volume of personal, often medical, data (such as HIV status) that are sensitive and must be kept confidential.
Key findings and publications
Outputs from the INDEPTH Network mentioned here comprise those that are based on data from more than one HDSS site, or which make external comparisons. The individual HDSS site profile papers will provide further details of site-specific outputs. The INDEPTH Network website (www.indepth-network.org) provides information about the Network, its organization and current activities.
One of the clear strengths of a network such as INDEPTH is its potential to collate data from member HDSS sites into outputs that enable systematic comparisons to be made. The first major INDEPTH output was a monograph published in 2002 that outlined basic HDSS concepts and gave details of 22 HDSS site members at that time.17 Two further monographs relating to health equity in small areas18 and migration11 followed in 2005 and 2009, respectively. In a different format, using a supplement in an open-access journal, three sets of multi-site papers were published in 2009–10. The first related to cross-site findings on non-communicable disease risk factors from a group of INDEPTH member HDSS sites in Asia.19–27 The second related to mortality clustering across a range of INDEPTH member HDSS sites28–36 and the third to results from eight INDEPTH member HDSS sites, which participated in the WHO–SAGE programme on ageing.37–46 The latter Supplement represented an innovation for the INDEPTH Network with the combined dataset used for the analyses also being published online together with the papers. Publications based on these public-domain data are now emerging.47
A number of other papers have considered particular issues at the Network level.48–53 In addition, there have been some outputs that have involved inter-site collaborations but not included wide representation across the Network.54–59 In some cases, multiple INDEPTH members are also members of other research networks such as the RTS,S Clinical Trials Partnership60 and the Alpha Network.61 Several other studies have made comparisons between HDSS data from single INDEPTH HDSS sites and other sources.62–65
Future analysis plans
As well as the substantial and continuing volume of outputs from individual HDSS sites, the INDEPTH Network will continue to produce multi-site outputs in particular topic areas. Current priorities include comparative assessments of fertility and cause-specific mortality patterns, as well as retrospective analyses of HDSS data against correspondingly timed weather data, which offer insights into the possible future population effects of changes in climatic conditions.
Strengths and weaknesses
HDSS sites represent an inherently strong epidemiological design, giving considerably greater analytical scope than can be achieved from e.g. cross-sectional approaches. However, the resources required to run an HDSS effectively are very considerable, particularly since the greatest gaps in health data are generally found in more logistically challenged environments. Not least this makes it very difficult for many HDSS sites to recruit and retain highly competent personnel, particularly those with experience in database management and epidemiological analysis, with the result that HDSS sites sometimes find it difficult to maximize their outputs.
A recurrent issue that arises in considering HDSS data is how the site populations are, or are not, representative of the wider surrounding populations. Although this does not pose any technical issues in terms of analysing data within an HDSS site, it is of concern when it comes to interpreting HDSS data into wider epidemiological and policy arenas. There are no simple solutions to this issue, since HDSSs are always located in places where little is known about the surrounding population. It is possible to make comparisons with other data sources, such as national censuses and cluster sample surveys,62–65 but these sources come with their own disadvantages such as greater recall bias, and hence it is very difficult to attribute causes to observed differences. An empirical investigation into this issue used Swedish national data from 1925, a time when Sweden shared many characteristics with contemporary LMICs.66 This showed that the majority of individual counties could have been taken as adequately representative of the national population, and the less representative counties were self-evidently so (including the capital city and the most remote regions). Although this does not offer any absolute evidence about the representativity of INDEPTH member HDSS sites, it suggests that it is not reasonable to assume by default that HDSS populations are unrepresentative.
The diversity observed across the INDEPTH member HDSS sites is a further source of both strength and weakness. As discussed earlier, there has never been any master plan for establishing HDSS sites in particular locations, and there are also significant (but often locally appropriate) detailed methodological differences between HDSS sites. This brings strength in terms of having highly functional and locally supported HDSS sites in many locations, something that might not have happened so effectively in trying to locate HDSS sites more systematically. However, it also brings some weaknesses when it comes to making comparisons across HDSS sites and between the countries that they represent. In contrast, the much stricter uniformity enforced across the Demographic and Household Survey (DHS) series of cross-sectional surveys makes comparisons simpler,67 but that stems from a completely different organizational paradigm. Nevertheless, the common core activities of all INDEPTH member DHSS sites, in following vital events longitudinally in a defined population, mean that the pooled INDEPTH data represent a major unified source of data on otherwise undocumented populations.
An interesting development in some situations, e.g. in China,68 is the concept of a distributed national network of HDSS-type surveillance, which perhaps represents a further intermediate step for the future. This has the advantage of being more widely representative, but at the same time bringing the advantages of a longitudinal approach. This may become a more common model as countries move towards universal individual registration.
Data sharing and collaboration
Data sharing issues have become increasingly important for all health researchers in recent years, and also continue to generate much debate.69 There is also a continuing dialogue between researchers and funders on these issues.70 The INDEPTH Network is firmly committed to the principles and practice of sharing data, as expressed in the INDEPTH Data Access and Sharing Policy document, available as Supplementary data at IJE online.
The issues involved in sharing HDSS data are complex. By the nature of the dynamic cohort, there is never any point in time when data collection is ‘complete’, and talking about sharing data at pre-determined intervals after completion is therefore not entirely helpful. Ways to work around these conceptual difficulties therefore have to be found, involving declaring particular periods of data from an HDSS as being ready for sharing at appropriate times. INDEPTH has already launched the iSHARE portal for making data from HDSS member sites publicly available (www.idepth-ishare.org) to bona fide users, not unlike the arrangements for access to DHS data sets.
In the existing version of iSHARE, data files from the participating HDSS sites are arranged in separate event files (births, deaths, migrations), but plans are underway to standardize iSHARE data into a common event-based data format. The common event attributes involved are shown in Table 1, and the range of different possible events are listed in Table 2. This structure will allow all participating sites to present HDSS core data in a straightforward and standardized format, which will facilitate a wide range of possible analytical approaches.
Table 1.
Common event attributes for the INDEPTH data specification
| Attribute | Variable name | Description |
|---|---|---|
| Record number | RecNr | A sequential number uniquely identifying each record in the data file |
| Centre identifier | CentreId | An identifier issued by INDEPTH to each member centre of the format CCCSS, where CCC is a sequential centre identifier and SS is a sequential identifier of the site within the centre in the case of multiple site centres |
| Individual identifier | IndividualId | A number uniquely identifying all the records belonging to a specific individual in the data file. For data anonymization purposes, this number should not be the same as the identifier used by a contributing centre to identify the individual, but the contributing centre should retain a mapping from this identifier to their identifier |
| Country identifier | CountryId | ISO 3166-1 numeric code of the country in which the surveillance site is situated |
| Location identifier | LocationId | Unique identifier associated with a residential unit within the site and is the location where the individual was or became resident when the event occurred. For data anonymization purposes, this identifier should not be the same as the identifier used internally by the contributing centre, but the contributing centre should retain a mapping of this identifier to their internal location identifier |
| Date of birth | DoB | The date of birth of the individual |
| Event | EventCode | A code identifying the type of event that has occurred (Table 2) |
| Event date | EventDate | The date on which the event occurred |
| Observation date | ObservationDate | Date on which the event was observed (recorded), also known as surveillance visit date |
| Event count | EventCount | The total number of events associated with this individual in this data set |
| Event number | EventNr | A number increasing from 1 to EventCount for each event record in order of event occurrence |
Table 2.
Event types for the INDEPTH data specification
| Event | Code | Definition | Attributes | Attribute description |
|---|---|---|---|---|
| Birth | BTH | The birth of an individual to a resident female |
|
|
| Enumeration | ENU | Starting event for all individuals present at the baseline census of the surveillance area. It is the date on which the individual was first observed to be present in the surveillance area during the baseline census | ||
| In-migration | IMG | The event of migrating into the surveillance area | Origin | Classification scheme to be developed |
| Out-migration | OMG | The event of migrating out of the surveillance area | Destination | Classification scheme to be developed |
| Location exit | EXT | The event of leaving a residential location within the surveillance area to take up residence in another residential location within the surveillance area | Destination | The LocationId of the location within the surveillance area to which the individual relocated |
| Location entry | ENT | The event of taking up residence in a residential location within the surveillance area following a location exit event. Note that location exit and entry are actually two parts of the same action of changing residential location and as such happen on the same event date | Origin | The LocationId of the residential location from which the individual moved |
| Death | DTH | The death of the individual under surveillance. The date of death is the event date |
|
|
| Delivery | DLV | The event of a pregnancy end after 28 weeks of gestation, which may or may not result in the birth of one or more individuals (represented in this dataset by a BTH event linked to this delivery event) |
|
|
| Observation end | OBE | An event inserted when a data set is right censored at an arbitrary date and this individual remained under surveillance beyond this date. The right censor date is the date of this event | ||
| Last observation | OBL | An event indicating the last point in time on which this individual was observed to be present and under surveillance. Event date equals observation date in this instance. Normally there should be no individuals with this event as their last event if the right censoring date is prior to the start of the last complete census round | ||
| Observation | OBS | Used to record characteristics of individuals under surveillance valid at the time of the observation. Could be used to record aspects such as educational attainment, employment status or anthropometry measures. Specific examples of this event are not part of the minimum core individual dataset, but are specified to allow for site or working group needs |
Conclusion
Our aim here is to describe the essential nature of the INDEPTH Network as a background to detailed profiles of constituent member HDSS sites. Although all those sites have important differences, the huge volume of detailed individual data generated across Africa, Asia and Oceania by the Network constitutes a unique resource of great value to demographers, epidemiologists and health planners.
Supplementary Data
Supplementary Data are available at IJE online.
Funding
Osman Sankoh is funded by core support grants to INDEPTH from the Hewlett Foundation, Gates Foundation, Sida/GLOBFORSK and Wellcome Trust.
Supplementary Material
References
- 1.INDEPTH Network. Founding Document. http://www.indepth-network.org/index.php?option=com_content&task=view&id=43&Itemid=129 (10 April 2012, date last accessed) [Google Scholar]
- 2.Scott JA, Bauni E, Moisi J, et al. Profile: The Kilifi Health and Demographic Surveillance System (KHDSS) Int J Epidemiol. 2012;41:650–57. doi: 10.1093/ije/dys062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossier C, Soura A, Baya B, et al. Profile: The Ouagadougou Health and Demographic Surveillance System (Ouaga HDSS) Int J Epidemiol. 2012;41:658–66. doi: 10.1093/ije/dys090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanifi SMA, Al Mamun A, Paul A, et al. Profile: The Chakaria Health and Demographic Surveillance System (CHDSS) Int J Epidemiol. 2012;41:667–75. doi: 10.1093/ije/dys089. [DOI] [PubMed] [Google Scholar]
- 5.Crampin AC, Dube A, Mboma S, et al. Profile: The Karonga Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:676–85. doi: 10.1093/ije/dys088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AbouZahr C, Cleland J, Coullare F, et al. The way forward. Lancet. 2007;370:1791–99. doi: 10.1016/S0140-6736(07)61310-5. [DOI] [PubMed] [Google Scholar]
- 7.Byass P. The unequal world of health data. PLoS Med. 2009;6:e1000155. doi: 10.1371/journal.pmed.1000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pearce N. Classification of epidemiological study designs. Int J Epidemiol. 2012;41:393–97. doi: 10.1093/ije/dys049. [DOI] [PubMed] [Google Scholar]
- 9.Fottrell E, Byass P. Population survey sampling methods in a rural African setting: measuring mortality. Popul Health Metr. 2008;6:2. doi: 10.1186/1478-7954-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rao C, Porapakkham Y, Pattaraarchachai J, Polprasert W, Swampunyalert N, Lopez AD. Verifying causes of death in Thailand: rationale and methods for empirical investigation. Popul Health Metr. 2010;8:11. doi: 10.1186/1478-7954-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collinson M, Adazu K, White M, Findley S, editors. INDEPTH Network. The Dynamics of Migration, Health and Livelihoods. Surrey, UK: Ashgate Publishing; 2009. ISBN 978-0-7546-7875-5. [Google Scholar]
- 12.Baiden F, Bawah A, Biai S, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85:570–71. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fottrell E, Byass P. Verbal autopsy – methods in transition. Epidemiol Rev. 2010;32:38–55. doi: 10.1093/epirev/mxq003. [DOI] [PubMed] [Google Scholar]
- 14.Stephens J, Alonso PL, Byass P, Snow RW. Tropical epidemiology: a system for continuous demographic monitoring of a study population. Methods Inf Med. 1989;28:155–59. [PubMed] [Google Scholar]
- 15.Phillips JF, MacLeod BB, Pence B. The Household Registration System: computer software for the rapid dissemination of demographic surveillance systems. Demogr Res. 2000;2:6. [PubMed] [Google Scholar]
- 16.Clark A. Anonymising research data. NCRM Working Paper Series 7/06, ESRC National Centre for Research Methods, Leeds, 2006. http://eprints.ncrm.ac.uk/480/1/0706_anonymising_research_data.pdf (10 April 2012, date last accessed) [Google Scholar]
- 17.Sankoh O, Kahn K, Mwageni E, Ngom P, Nyarko P, editors. INDEPTH Network. Population and Health in Developing Countries Volume1: Population, Health and Survival at INDEPTH Sites. Ottawa: IDRC; 2002. ISBN 0-88936-948-8. [Google Scholar]
- 18.de Savigny D, Debpuur C, Mwageni E, Nathan R, Setel PW, editors. INDEPTH Network. Measuring Health Equity in Small Areas: Findings from Demographic Surveillance Systems. Surrey, UK: Ashgate Publishing; 2005. ISBN 0-7546-4494-4. [Google Scholar]
- 19.Ng N, Van Minh H, Juvekar S, et al. Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle-income countries. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1984. doi:10.3402/gha.v2i0.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng N, Hakimi M, Van Minh H, et al. Prevalence of physical inactivity in nine rural INDEPTH Health and Demographic Surveillance Systems in five Asian countries. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1985. doi:10.3402/gha.v2i0.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed SM, Hadi A, Razzaque A, et al. Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1986. doi:10.3402/gha.v2i0.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanungsukkasem U, Ng N, Van Minh H, et al. Fruit and vegetable consumption in rural adults population in INDEPTH HDSS sites in Asia. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1988. doi:10.3402/gha.v2i0.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krishnan A, Nongkynrih B, Kapoor SK, Pandav C. A role for INDEPTH Asian sites in translating research to action for non-communicable disease prevention and control: a case study from Ballabgarh, India. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1990. doi:10.3402/gha.v2i0.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Razzaque A, Nahar L, Van Minh H, et al. Social factors and overweight: evidence from nine Asian INDEPTH Network sites. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1991. doi:10.3402/gha.v2i0.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashraf A, Quaiyum MA, Ng N, et al. Self-reported use of tobacco products in nine rural INDEPTH Health and Demographic Surveillance Systems in Asia. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1997. doi:10.3402/gha.v2i0.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Minh H, Soonthornthada K, Ng N, et al. Blood pressure in adult rural INDEPTH population in Asia. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.2010. doi:10.3402/gha.v2i0.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huu Bich T, Thi Quynh Nga P, Ngoc Quang L, et al. Patterns of alcohol consumption in diverse rural populations in the Asian region. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.2017. doi:10.3402/gha.v2i0.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shabani J, Lutambi AM, Mwakalinga V, Masanja H. Clustering of under-five mortality in Rufiji Health and Demographic Surveillance System in rural Tanzania. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5264. doi:10.3402/gha.v3i0.5264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adjuik M, Kanyomse E, Kondayire F, Wak G, Hodgson A. Clustering of under-five mortality in the Navrongo HDSS in the Kassena-Nankana District of northern Ghana. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5233. doi:10.3402/gha.v3i0.5233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kanjala C, Alberts M, Byass P, Burger S. Spatial and temporal clustering of mortality in Digkale HDSS in rural northern South Africa. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5236. doi:10.3402/gha.v3i0.5236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Byass P, Fantahun M, Emmelin A, Molla M, Berhane Y. Spatio-temporal clustering of mortality in Butajira HDSS, Ethiopia, from 1987 to 2008. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5244. doi:10.3402/gha.v3i0.5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lutambi AM, Alexander M, Charles J, Mahutanga C, Nathan R. Under-five mortality: spatial-temporal clusters in Ifakara HDSS in South-eastern Tanzania. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5254. doi:10.3402/gha.v3i0.5254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alam N, Zahirul Haq M, Kim Streatfield P. Spatio-temporal patterns of under-five mortality in Matlab HDSS in rural Bangladesh. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5252. doi:10.3402/gha.v3i0.5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanifi SM, Haq MZ, Aziz RR, Bhuiya A. High concentration of childhood deaths in the low-lying areas of Chakaria HDSS, Bangladesh: findings from a spatial analysis. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5274. doi:10.3402/gha.v3i0.5274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nettey OE, Zandoh C, Sulemana A, Adda R, Owusu-Agyei S. Clustering of childhood mortality in the Kintampo Health and Demographic Surveillance System in Ghana. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5258. doi:10.3402/gha.v3i0.5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sartorius B, Kahn K, Vounatsou P, Collinson MA, Tollman SM. Space and time clustering of mortality in rural South Africa (Agincourt HDSS), 1992–2007. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5225. doi:10.3402/gha.v3i0.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kowal P, Kahn K, Ng N, et al. Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5302. doi:10.3402/gha.v3i0.5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mwanyangala MA, Mayombana C, Urassa H, et al. Health status and quality of life among older adults in rural Tanzania. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2142. doi:10.3402/gha.v3i0.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hirve S, Juvekar S, Lele P, Agarwal D. Social gradients in self-reported health and well-being among adults aged 50 and over in Pune District, India. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2128. doi:10.3402/gha.v3i0.2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Razzaque A, Nahar L, Akter Khanam M, Kim Streatfield P. Socio-demographic differentials of adult health indicators in Matlab, Bangladesh: self-rated health, health state, quality of life and disability level. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.4618. doi:10.3402/gha.v3i0.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Debpuur C, Welaga P, Wak G, Hodgson A. Self-reported health and functional limitations among older people in the Kassena-Nankana District, Ghana. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2151. doi:10.3402/gha.v3i0.2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Minh H, Byass P, Chuc NT, Wall S. Patterns of health status and quality of life among older people in rural Viet Nam. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2124. doi:10.3402/gha.v3i0.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ng N, Hakimi M, Byass P, Wilopo S, Wall S. Health and quality of life among older rural people in Purworejo District, Indonesia. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2125. doi:10.3402/gha.v3i0.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kyobutungi C, Egondi T, Ezeh A. The health and well-being of older people in Nairobi's slums. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2138. doi:10.3402/gha.v3i0.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xavier Gómez-Olivé F, Thorogood M, Clark BD, Kahn K, Tollman SM. Assessing health and well-being among older people in rural South Africa. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2126. doi:10.3402/gha.v3i0.2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ng N, Kowal P, Kahn K, et al. Health inequalities among older men and women in Africa and Asia: evidence from eight Health and Demographic Surveillance System sites in the INDEPTH WHO-SAGE Study. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5420. doi:10.3402/gha.v3i0.5420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stranges S, Tigbe W, Gómez-Olivé FX, Thorogood M, Kandala M-B. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among over 40,000 older adults from eight countries across Africa and Asia. Sleep. (in press) doi: 10.5665/sleep.2012. http://www.journalsleep.org/AcceptedPapers/SP-508-11.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Källander K, Kadobera D, Williams TN, et al. Social autopsy: INDEPTH Network experiences of utility, process, practices, and challenges in investigating causes and contributors to mortality. Popul Health Metr. 2011;9:44. doi: 10.1186/1478-7954-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sankoh OA, Ngom P, Clark SJ, de Savigny D, Binka F. Levels and patterns of mortality at INDEPTH demographic surveillance systems. In: Jamison DT, Feachem RG, Makgoba MW, editors. Disease and Mortality in Sub-Saharan Africa. 2nd. Washington (DC): World Bank; 2006. Chapter 7. [PubMed] [Google Scholar]
- 50.Bangha M, Diagne A, Bawah A, Sankoh O. Monitoring the millennium development goals: the potential role of the INDEPTH Network. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5517. doi: 10.3402/gha.v3i0.5517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ogutu BR, Baiden R, Diallo D, Smith PG, Binka FN. Sustainable development of a GCP-compliant clinical trials platform in Africa: the malaria clinical trials alliance perspective. Malar J. 2010;9:103. doi: 10.1186/1475-2875-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tatem AJ, Snow RW, Hay SI. Mapping the environmental coverage of the INDEPTH demographic surveillance system network in rural Africa. Trop Med Int Health. 2006;11:1318–26. doi: 10.1111/j.1365-3156.2006.01681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evans T, Abouzahr C. INDEPTH @ 10: celebrate the past and illuminate the future. Glob Health Action. 2008;1 doi: 10.3402/gha.v1i0.1899. doi: 10.3402/gha.v1i0.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tesfaye F, Nawi NG, Van Minh H, et al. Association between body mass index and blood pressure across three populations in Africa and Asia. J Hum Hypertens. 2007;21:28–37. doi: 10.1038/sj.jhh.1002104. [DOI] [PubMed] [Google Scholar]
- 55.Van Minh H, Ng N, Byass P, Wall S. Patterns of subjective quality of life among older adults in rural Vietnam and Indonesia. Geriatr Gerontol Int. 2012;12:397–404. doi: 10.1111/j.1447-0594.2011.00777.x. [DOI] [PubMed] [Google Scholar]
- 56.Fottrell E, Kahn K, Ng N, et al. Mortality measurement in transition: proof of principle for standardised multi-country comparisons. Trop Med Int Health. 2010;15:1256–65. doi: 10.1111/j.1365-3156.2010.02601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ng N, Winkler V, Van Minh H, Tesfaye F, Wall S, Becher H. Predicting lung cancer death in Africa and Asia: differences with WHO estimates. Cancer Causes Control. 2009;20:721–30. doi: 10.1007/s10552-008-9285-8. [DOI] [PubMed] [Google Scholar]
- 58.Ng N, Van Minh H, Tesfaye F, et al. Combining risk factors and demographic surveillance: potentials of WHO STEPS and INDEPTH methodologies for assessing epidemiological transition. Scand J Public Health. 2006;34:199–208. doi: 10.1080/14034940500204506. [DOI] [PubMed] [Google Scholar]
- 59.Serwaa-Bonsu A, Herbst AJ, Reniers G, et al. First experiences in the implementation of biometric technology to link data from Health and Demographic Surveillance Systems with health facility data. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.2120. doi:10.3402/gha.v3i0.2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Agnandji ST, Lell B, Soulanoudjingar SS, et al. First results of phase 3 trial of RTS,S/AS01 malaria vaccine in African children. N Engl J Med. 2011;365:1863–75. doi: 10.1056/NEJMoa1102287. [DOI] [PubMed] [Google Scholar]
- 61.Maher D, Biraro S, Hosegood V, et al. Translating global health research aims into action: the example of the ALPHA network. Trop Med Int Health. 2010;15:321–28. doi: 10.1111/j.1365-3156.2009.02456.x. [DOI] [PubMed] [Google Scholar]
- 62.Nhacolo AQ, Nhalungo DA, Sacoor CN, Aponte JJ, Thompson R, Alonso P. Levels and trends of demographic indices in southern rural Mozambique: evidence from demographic surveillance in Manhiça district. BMC Public Health. 2006;6:291. doi: 10.1186/1471-2458-6-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fottrell E, Enquselassie F, Byass P. The distribution and effects of child mortality risk factors in Ethiopia: a comparison of estimates from DSS and DHS. Ethiop J Health Dev. 2009;23:163–68. [Google Scholar]
- 64.Hammer GP, Kouyaté B, Ramroth H, Becher H. Risk factors for childhood mortality in sub-Saharan Africa: a comparison of data from a Demographic and Health Survey and from a Demographic Surveillance System. Acta Tropica. 2006;98:212–18. doi: 10.1016/j.actatropica.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 65.Byass P, Worku A, Emmelin A, Berhane Y. DSS and DHS: longitudinal and cross-sectional viewpoints on child and adolescent mortality in Ethiopia. Pop Health Metr. 2007;5:12. doi: 10.1186/1478-7954-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Byass P, Sankoh O, Tollman SM, Högberg U, Wall S. Lessons from history for designing and validating epidemiological surveillance in uncounted populations. PLoS ONE. 2011;6:e22897. doi: 10.1371/journal.pone.0022897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rutstein SO, Rojas G. Guide to DHS Statistics. Maryland: ORC Macro; 2006. http://www.measuredhs.com/pubs/pdf/DHSG1/Guide_DHS_Statistics.pdf (10 April 2012, date last accessed) [Google Scholar]
- 68.Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: history, current situation and challenges. Popul Health Metr. 2005;3:3. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chandramohan D, Shibuya K, Setel P, et al. Should data from demographic surveillance systems be made more widely available to researchers? PLoS Med. 2008;5:e57. doi: 10.1371/journal.pmed.0050057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sankoh O, Ijsselmuiden C. Sharing research data to improve public health: a perspective from the global south. Lancet. 2011;378:401–02. doi: 10.1016/S0140-6736(11)61211-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.