Abstract
Background: Although dietary recommendations have focused on restricting saturated fat (SF) consumption to reduce cardiovascular disease (CVD) risk, evidence from prospective studies has not supported a strong link between total SF intake and CVD events. An understanding of whether food sources of SF influence these relations may provide new insights.
Objective: We investigated the association of SF consumption from different food sources and the incidence of CVD events in a multiethnic population.
Design: Participants who were 45–84 y old at baseline (n = 5209) were followed from 2000 to 2010. Diet was assessed by using a 120-item food-frequency questionnaire. CVD incidence (316 cases) was assessed during follow-up visits.
Results: After adjustment for demographics, lifestyle, and dietary confounders, a higher intake of dairy SF was associated with lower CVD risk [HR (95% CI) for +5 g/d and +5% of energy from dairy SF: 0.79 (0.68, 0.92) and 0.62 (0.47, 0.82), respectively]. In contrast, a higher intake of meat SF was associated with greater CVD risk [HR (95% CI) for +5 g/d and a +5% of energy from meat SF: 1.26 (1.02, 1.54) and 1.48 (0.98, 2.23), respectively]. The substitution of 2% of energy from meat SF with energy from dairy SF was associated with a 25% lower CVD risk [HR (95% CI): 0.75 (0.63, 0.91)]. No associations were observed between plant or butter SF and CVD risk, but ranges of intakes were narrow.
Conclusion: Associations of SF with health may depend on food-specific fatty acids or other nutrient constituents in foods that contain SF, in addition to SF.
INTRODUCTION
As a key measure to prevent cardiovascular disease (CVD)5, the US Dietary Guidelines for Americans recommend a restriction of saturated fat (SF) consumption (1). However, despite convincing evidence that SF consumption raises plasma LDL in humans and causes atherosclerosis in animal models (2), findings from many prospective cohort studies have not supported any significant association between SF intake and risk of CVD (3, 4). A recent meta-analysis that included 16 prospective cohort studies showed pooled RR estimates (95% CIs) for extreme quintiles of SF intake of 1.07 (0.96, 1.19) for coronary heart disease (CHD), 0.81 (0.62, 1.05) for stroke, and 1.00 (0.89, 1.11) for total CVD in participants 30–89 y of age (4).
The absence of an association between SF consumption and CVD risk in these studies could partly relate to differences in the comparison nutrient. For example, although clinical trials showed that the replacement of SF with polyunsaturated fat reduced CHD risk (5), evidence has suggested that a modification of an SF-rich diet toward a carbohydrate-rich diet, which is the most common scenario in the United States and other populations, may have little effect on CVD risk (6, 7). The absence of an association could also partly relate to divergent effects of SF on different lipid fractions. In comparison with carbohydrates, higher SF consumption not only increases LDL but also increases HDL and decreases triglycerides, with little net effect on the ratio of total:HDL cholesterol (8), which is considered a better predictor of CHD events than is total cholesterol or any individual lipid measurement (9–11).
In addition to these possible explanations, it is plausible that effects of SF consumption could vary depending on its food source. For example, red meat, which is a common source of SF, contains dietary cholesterol and heme iron that may increase CVD risk (12, 13). Processed red meats and deli meats also contain high amounts of sodium and other preservatives that may have unfavorable effects on CVD risk factors (14). In contrast, dairy foods, which are a major source of SF in most populations, are also sources of beneficial nutrients including vitamin D, potassium, phosphorus, and calcium that might counterbalance the unfavorable physiologic effects of SF (15, 16). Other sources of SF include certain plants and vegetable oils that may contain other protective fatty acids and phytochemicals (17–19). Each of these different food sources also contains different proportions of specific SFAs (eg, myristic, lauric, and stearic), which have differential effects on blood lipid and could differentially influence CVD. However, despite these important differences between food sources of SF, few previous studies have evaluated how SF from different food sources relates to the development of CVD.
To elucidate these relations, we investigated the association of SF consumption from different food sources and the incidence of CVD events in participants in the Multi-Ethnic Study of Atherosclerosis (MESA). We hypothesized that associations with incident CVD would be influenced by food sources that delivered SF. Specifically, we hypothesized that meat SF would be positively associated with CVD, whereas dairy and plant SF would be unassociated or inversely associated with CVD.
SUBJECTS AND METHODS
Study population
Aims and study design of the MESA cohort have been previously described (20). In 2000, 6814 adults aged 45–84 y who were free of clinical CVD were recruited from the following 6 US communities: Baltimore City and County, MD; Chicago, IL; Forsyth County, NC; New York, NY; Los Angeles County, CA; and St Paul, MN. Cohort examinations were conducted in 2000–2002 (baseline), 2002–2003, 2004–2005, and 2005–2007. Protocols were approved by local institutional review boards; all participants provided written informed consent.
In this analysis, we excluded participants with daily energy intakes <600 or >6000 kcal/d (n = 801) and subjects with unreliable information (incomplete forms, too few or too many foods reported per day, a high frequency of foods skipped, or too many foods coded with the same frequency or serving size) (n = 577) (21). In addition, we excluded participants who did not return for an examination after baseline (n = 35) as well as subjects previously diagnosed with type 2 diabetes (n = 859) at baseline because of the potential for recent dietary change to bias measures of association.
Information on demographics, education, medication use, physical activity, smoking, and drinking habits was self-reported at baseline.
Dietary assessment
At the baseline examination, participants were asked to report the average frequency of consumption of specific food items over the previous year by using a modified-Block (22) 120-item food-frequency questionnaire (FFQ), with modifications to include Chinese food and beverage items (23, 24). Correlations between total fat intake derived from the original FFQ and total fat intake derived from the average of eight 24-h recalls were 0.66 in non-Hispanic whites, 0.59 in African Americans, and 0.58 in Hispanics living in rural areas (23). Correlations were slightly stronger for SF estimates and were 0.77 in non-Hispanic whites, 0.62 in African Americans, and 0.62 in rural Hispanics (23). Associations between macronutrient intakes and plasma lipid concentrations were evaluated to test the criterion validity of the modified MESA-specific FFQ (24).
Nutrient intakes from diet were estimated by multiplying the frequency and serving size for each food consumed by the nutrient content of that food (Nutrition Data Systems for Research; University of Minnesota). Intakes of SF from different food sources were estimated separately by multiplying the SF content in selected food items by the daily food-intake frequency and the age- and sex-specific and portion-size gram weights. Subsequently, food-specific SF intakes were estimated by summing the SF intake from dairy, meat, butter, plant sources, and mixed animal and plant sources (see Table S1 under “Supplemental data” in the online issue for a detailed list of food sources). Additional questions on consumption of low-fat foods and types of cooking fat were taken into account when intakes were calculated. All nutrient values were adjusted for energy intakes by using the residuals method (25).
Ascertainment of CVD
Total CVD events comprised the incidence of myocardial infarction, resuscitated cardiac arrest, definite and probable angina, CHD death, stroke, stroke death, or other CVD or atherosclerotic death. CHD events were defined as the incidence of myocardial infarction, resuscitated cardiac arrest, definite and probable angina, or CHD death. We also performed sensitivity analyses, with the exclusion of angina, to evaluate only hard CVD events. Information on cardiovascular incidence was obtained through cohort examinations, follow-up calls, medical record abstractions, or obituaries. Medical records were obtained on 98% of reported hospitalized events and 95% of outpatient procedures (26). Self-reported diagnoses and CVD-related records (death certificates, autopsy reports, and medical records) were reviewed by a medical endpoints committee. Deaths for subjects with loss to follow-up were identified by contacting family members. A standard protocol was used to classify events and assign incident dates on the basis of records available (27, 28).
Statistical analysis
Restricted cubic spline analysis (29) showed no evidence of a threshold or nonlinear relation between each SF source subtype and CVD risk. Therefore, we used Cox proportional hazards to estimate HRs and 95% CIs of food-specific SF estimates evaluated in quintiles and also for each 5-g SF/d difference and each 5% of total energy difference in SF intake. We also performed similar analyses restricted to CHD events. To minimize potential confounding, we evaluated 3 multivariable models. Model 1 was adjusted for sex, age (y), race-ethnicity, energy intake (kcal/d), and field center. Model 2 included additional adjustment for education level (less than high school, high school, or more than high school), active leisure (walking, sport, and conditioning in metabolic min/wk), sedentary leisure (television viewing, reading, and light sitting activities in metabolic min/wk), alcohol intake (ethanol g/d), smoking (never, former, or current smoker and number of pack-years of cigarette smoking), BMI (in kg/m2), dietary supplement use (at least weekly; yes or no), and cholesterol-lowering medication use (yes or no). Finally, model 3 included additional adjustment for intakes of fruit and vegetables (servings/d) and energy-adjusted intakes of dietary fiber (g/d), dietary vitamin E (IU/d), trans fat (g/d), and PUFA (g/d). We estimated the effect of the substitution of SF from a specific source for the same percentage of SF from another source by including SF from each source expressed as energy density in model 2. Differences between linear coefficients and the corresponding covariance matrix were used to obtain HRs and 95% CIs (30, 31). All analyses were performed with SAS 9.2 software (SAS Institute). All P values were 2-sided, and P < 0.05 indicated statistical significance.
RESULTS
During 36,364 person-years of follow-up between 2000 and 2010, a total of 316 new cases of CVD were identified, including 231 CHD events. Dairy, mixed animal and plant items, and meat (including red and processed meat, fish, and poultry) were the primary sources of SF in the MESA population and accounted for 35%, 26%, and 18% of total SF intake, respectively. Correlations between food-specific sources of SF consumption were weak and ranged from −0.12 to 0.15 (Table 1). Correlations of each SF source with total SF were variable from as low as 0.07 for plant SF to as high as 0.62 for dairy SF.
TABLE 1.
Correlations between estimates of SF from different sources in the MESA (n = 5209)1
| Dairy SF | Meat SF | Butter SF | Plant SF | SF from mixed sources | |
| Total SF | 0.62 | 0.36 | 0.37 | 0.07 | 0.33 |
| Dairy SF | 1 | −0.04 | 0.11 | −0.001 | −0.12 |
| Meat SF | 1 | 0.1 | −0.04 | 0.15 | |
| Butter SF | 1 | 0.09 | 0.11 | ||
| Plant SF | 1 | −0.06 |
Correlations were adjusted for age, sex, and race-ethnicity. All correlations were significant at the 0.05 significance level except for the correlation between dairy and plant SF (r = −0.001). MESA, Multi-Ethnic Study of Atherosclerosis; SF, saturated fat.
In unadjusted comparisons, a higher total SF intake was associated with generally worse cardiovascular risk factors and behaviors, including higher BMI, greater tobacco use, lower physical activity, lower dietary supplement use, and lower intakes of fiber, dietary vitamin E, and alcohol (Table 2). Findings were generally similar for each of the food-specific sources of SF consumption (data not shown).
TABLE 2.
Baseline characteristics of MESA participants free of prevalent type 2 diabetes by quintiles of total SF intake (n = 5209)1
| Quintiles of energy-adjusted total SF intake (g/d) |
||||||
| <14.5 | 14.5–17.1 | 17.2–19.2 | 19.3–22.2 | >22.3 | P-trend | |
| n | 1041 | 1043 | 1042 | 1042 | 1041 | |
| Median saturated fat intake (g/d) | 12.20 | 16.00 | 18.10 | 20.40 | 25.30 | |
| Age (y)2 | 62.1 ± 10.2 | 62.1 ± 10 | 62.5 ± 10.5 | 61.4 ± 10.6 | 61.1 ± 10.3 | <0.01 |
| Sex (% F) | 40.4 | 51.3 | 57.7 | 57.5 | 55.4 | <0.01 |
| Race-ethnicity (%) | <0.01 | |||||
| White | 37.0 | 38.5 | 40.0 | 44.3 | 55.6 | |
| African American | 23.3 | 25.1 | 23.9 | 26.4 | 23.4 | |
| Hispanic | 21.7 | 18.6 | 20.4 | 22.4 | 19.3 | |
| Chinese | 18.0 | 17.8 | 15.7 | 6.9 | 1.7 | |
| ≥12 y of formal education (%) | 84.0 | 82.9 | 83.0 | 84.2 | 85.6 | 0.76 |
| BMI (kg/m2)2 | 27.3 ± 4.9 | 27.4 ± 5 | 27.6 ± 5.4 | 28.4 ± 5.1 | 29 ± 5.8 | <0.01 |
| Physical activity (MET-min/wk)2 | ||||||
| Sedentary leisure | 1653 ± 1095 | 1638 ± 1105 | 1665 ± 1103 | 1663 ± 1127 | 1817 ± 1180 | <0.01 |
| Active leisure | 2797 ± 3323 | 2530 ± 2735 | 2528 ± 3370 | 2328 ± 2995 | 2285 ± 2695 | <0.01 |
| Cigarette pack-years | 10.1 ± 27.7 | 8.3 ± 15.5 | 10.2 ± 19 | 11.7 ± 20.7 | 16.2 ± 26.3 | <0.01 |
| Weekly dietary supplement use (percentage current) | 36.0 | 34.7 | 34.8 | 34.2 | 35.1 | <0.01 |
| HDL cholesterol (mg/dL)2 | 50.2 ± 14.1 | 51.8 ± 15.4 | 52.4 ± 15.2 | 51.9 ± 15.0 | 52.0 ± 15.4 | 0.01 |
| LDL cholesterol (mg/dL)2 | 117.2 ± 30.0 | 116.9 ± 31.4 | 117.9 ± 30.6 | 117.9 ± 30.8 | 118.4 ± 31.3 | 0.26 |
| Fasting glucose (mg/dL)2 | 90.0 ± 10.5 | 89.6 ± 10.3 | 89.8 ± 10.6 | 88.8 ± 10.3 | 89.5 ± 10.9 | 0.14 |
| SBP (mm Hg)2 | 126.5 ± 21.0 | 126.1 ± 21.3 | 126.0 ± 21.6 | 125.0 ± 21.1 | 124.1 ± 20.5 | <0.01 |
| DBP (mm Hg)2 | 73.1 ± 10.0 | 72.1 ± 10.3 | 71.5 ± 10.3 | 71.6 ± 10.2 | 71.2 ± 10.2 | <0.01 |
| Dietary intakes2 | ||||||
| Energy (kcal/d) | 1898 ± 783 | 1396 ± 628 | 1294 ± 600 | 1426 ± 678 | 1844 ± 818 | 0.77 |
| Alcohol (g/d) | 9.0 ± 18.6 | 5.9 ± 12.5 | 4.1 ± 8.2 | 4.3 ± 8.6 | 4.7 ± 10.2 | <0.01 |
| Fiber (g/d)3 | 22.4 ± 8.1 | 19 ± 4.9 | 17.2 ± 4.2 | 15.8 ± 4 | 13.1 ± 4.7 | <0.01 |
| Vitamin E (IU/d)3 | 8.8 ± 4.8 | 8.2 ± 2.7 | 8.3 ± 2.6 | 8.3 ± 2.7 | 7.9 ± 3.3 | <0.01 |
| SF from different sources (g/d)34 | ||||||
| Dairy | 2.8 ± 3.3 | 5.0 ± 2.4 | 6.0 ± 2.5 | 7.0 ± 3.2 | 10.2 ± 6.7 | NA |
| Meat | 1.8 ± 2.1 | 2.8 ± 2.0 | 3.2 ± 1.7 | 3.5 ± 2.2 | 3.8 ± 3.9 | NA |
| Processed meats | 0.25 ± 1.1 | 0.78 ± 1.1 | 0.94 ± 1.1 | 1.0 ± 1.4 | 1.4 ± 2.7 | NA |
| Unprocessed meats | 1.3 ± 1.8 | 1.8 ± 1.7 | 2.1 ± 1.3 | 2.2 ± 1.8 | 1.9 ± 2.6 | NA |
| Butter SF | 0.13 ± 1.3 | 0.57 ± 1.1 | 0.70 ± 1.2 | 0.86 ± 1.8 | 1.4 ± 3.5 | NA |
| Plant SF | 0.79 ± 1.0 | 0.87 ± 0.84 | 0.94 ± 0.80 | 0.94 ± 0.85 | 0.96 ± 1.2 | NA |
| SF from mixed animal and plant sources | 3.3 ± 2.5 | 4.2 ± 1.9 | 4.7 ± 2.0 | 5.2 ± 2.5 | 5.3 ± 3.7 | NA |
P-trend values were derived by using unadjusted regression models. DBP, diastolic blood pressure; MET, metabolic equivalent; NA, not applicable; SBP, systolic blood pressure; SF, saturated fat.
Values are means ± SEs.
Values were adjusted for total energy intake.
Values are medians ± SEs.
Total SF
The mean (±SE) percentage of total energy intake from SF was 10.2 ± 3.2%. In the minimally adjusted analysis that included age, sex, race, field center, and energy intake, total SF was modestly associated with lower risk of CVD. The association was strengthened after adjustment for other behavioral and lifestyle confounders (ie, education, alcohol use, smoking, dietary supplement and lipid-lowering medication use, physical activity, and BMI) and major dietary factors (ie, intakes of fiber, fruit and vegetables, vitamin E, trans fat, and PUFA); the HR associated with each 5-g/d greater intake of total SF was 0.86 (95% CI: 0.75, 0.97). Similarly, the HR of CVD associated with a 5-unit increase in the percentage of energy from total SF was 0.71 (95% CI: 0.56, 0.89) (Table 3). Results for CHD alone were very similar (see Table S3 under “Supplemental data” in the online issue).
TABLE 3.
HRs (95% CIs) of CVD for 5 g/d and 5% energy from SF from different sources (n = 5209; 316 new cases)1
| For each 5 g/d | P | For each 5% of energy | P | |
| Total SF | ||||
| Model 1 | 0.98 (0.89, 1.08) | 0.68 | 0.92 (0.76,1.10) | 0.35 |
| Model 2 | 0.93 (0.84, 1.03) | 0.16 | 0.82 (0.68, 1.00) | 0.04 |
| Model 3 | 0.86 (0.75, 0.97) | 0.02 | 0.71 (0.56, 0.89) | <0.01 |
| Dairy SF | ||||
| Model 1 | 0.90 (0.79, 1.02) | 0.10 | 0.79 (0.61, 1.01) | 0.06 |
| Model 2 | 0.86 (0.75, 0.98) | 0.03 | 0.72 (0.56, 0.93) | 0.01 |
| Model 3 | 0.79 (0.68, 0.92) | <0.01 | 0.62 (0.47, 0.82) | <0.01 |
| Meat SF | ||||
| Model 1 | 1.31 (1.09, 1.59) | <0.01 | 1.69 (1.15, 2.48) | <0.01 |
| Model 2 | 1.26 (1.04, 1.53) | 0.02 | 1.52 (1.03, 2.25) | 0.04 |
| Model 3 | 1.26 (1.02, 1.54) | 0.03 | 1.48 (0.98, 2.23) | 0.06 |
| Butter SF | ||||
| Model 1 | 0.93 (0.71, 1.22) | 0.59 | 0.94 (0.58, 1.52) | 0.79 |
| Model 2 | 0.88 (0.67, 1.16) | 0.37 | 0.85 (0.52, 1.40) | 0.53 |
| Model 3 | 0.87 (0.66, 1.15) | 0.33 | 0.83 (0.50, 1.37) | 0.47 |
| Plant SF | ||||
| Model 1 | 0.82 (0.44, 1.53) | 0.53 | 0.48 (0.16, 1.51) | 0.21 |
| Model 2 | 0.80 (0.42, 1.52) | 0.50 | 0.46 (0.15, 1.46) | 0.19 |
| Model 3 | 1.00 (0.50, 2.01) | 0.99 | 0.62 (0.18, 2.11) | 0.44 |
| Mixed sources of SF | ||||
| Model 1 | 1.06 (0.86, 1.31) | 0.60 | 0.97 (0.65, 1.46) | 0.90 |
| Model 2 | 1.00 (0.80, 1.24) | 0.99 | 0.87 (0.57, 1.32) | 0.46 |
| Model 3 | 1.01 (0.77, 1.32) | 0.96 | 0.83 (0.51, 1.36) | 0.51 |
All values are HRs (95% CIs). Values were derived from proportional hazards models adjusted as follows: model 1 included age (y), sex, race-ethnicity (non-Hispanic white, African American, Hispanic, and Chinese American), study center, and energy intake (kcal/d); model 2 included all variables in model 1 plus additional adjustment for education (<high school, high school, and >high school), alcohol intake (g/d), physical activity (active and sedentary leisure in metabolic equivalents-min per wk), BMI (in kg/m2), cigarette smoking (never, current, or former smoker and pack-years of cigarette smoking), dietary supplement use (>1/wk; yes or no), and use of cholesterol-lowering medication (yes or no); and model 3 included all variables in model 2 plus intakes of fruit and vegetables (servings/d) and energy-adjusted intakes of dietary fiber (g/d), dietary vitamin E (IU/d), trans fat, and PUFA (g/d). P-trend values were calculated by using median values of energy-adjusted nutrient quintiles as continuous variables in statistical models. CVD, cardiovascular disease; SF, saturated fat.
Dairy SF
In the minimally adjusted model, dairy SF was not significantly associated with CVD risk (Table 3). However, after additional adjustment for other demographic and lifestyle factors, higher intakes of dairy SF were associated with lower CVD risk (Table 3, model 2). Inverse associations of dairy SF with CVD risk were further strengthened by adjustment for other dietary habits, which indicated the presence of upward confounding (a bias toward harm) by these factors, including the consumption of dietary fiber, fruit and vegetables, PUFA, trans fat, and dietary vitamin E. In the fully adjusted model, each 5-g/d greater intake was associated with 21% lower risk [HR (95% CI): 0.79 (0.68, 0.92); Table 3, model 3]. Similarly, each 5-unit increase in the percentage of energy from dairy SF was associated with 38% lower risk of CVD [HR (95% CI): 0.62 (0.47, 0.82); Table 3, model 3]. Directions and magnitudes of associations were similar when CHD was evaluated separately (see Data supplement under “Supplemental data” in the online issue).
Meat SF
In the minimally adjusted model, meat SF intake was associated with higher risk of CVD [HR (95% CI) of 1.31 (1.09, 1.59) for each +5 g/d and 1.69 (1.15, 2.48) for each +5% of total energy from meat SF (Table 3, model 1)]. Associations were partly attenuated after additional adjustment for other demographic, lifestyle, and dietary factors [HR (95% CI) of 1.26 (1.02, 1.54) for each +5 g/d and 1.48 (0.98, 2.23) for each +5% of total energy (Table 3, model 3)], which indicated upward confounding (a bias toward harm) by these factors, as seen with dairy SF. Associations between meat SF and risk of CHD were similar to those for total CVD (see Table S2 under “Supplemental data” in the online issue).
Butter and plant SF
No associations were observed between butter, plant, or mixed sources of SF and total CVD or CHD risk (see Data supplement under “Supplemental data” in the online issue).
Associations with hard CHD
In sensitivity analyses in which angina was excluded from CVD endpoints, inverse associations of total, dairy, and plant SF with hard CVD were somewhat stronger, whereas the positive association of meat SF with hard CVD was slightly attenuated (data not shown).
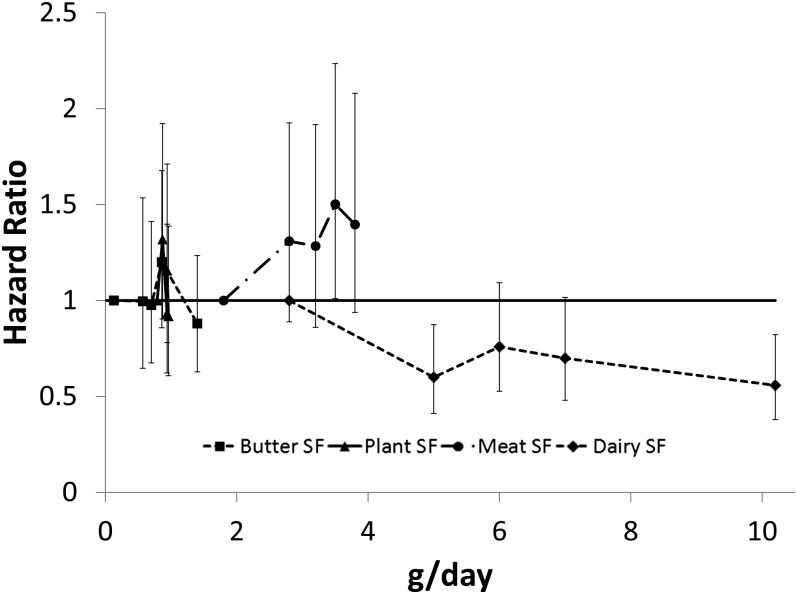
Risk across quintiles
When we evaluated risk across quintiles of SF consumption from each food source, a significant inverse association was seen for dairy SF [HR (95% CI) for extreme quintiles: 0.56 (0.38, 0.82); P-trend = 0.01], whereas meat SF was not statistically significantly associated with risk [HR (95% CI) for extreme quintiles: 1.40 (0.94, 2.08); P-trend = 0.12] (Figure 1). Butter and plant sources of SF were not associated with CVD risk, but ranges of SF consumption from these sources were quite narrow, which limited our ability to detect differences in risk across quintiles.
FIGURE 1.
HRs and 95%s of CVD risk according to quintiles of energy-adjusted SF from different sources (n = 5209). All values were derived from proportional hazards models with adjustment for age (y), sex, race-ethnicity (non-Hispanic white, African American, Hispanic, and Chinese American), study center, energy intake (kcal/d), education (<high school, high school, or >high school), alcohol intake (g/d), physical activity (active and sedentary leisure in metabolic equivalents-min/wk), BMI (in kg/m2), cigarette smoking (never, current, or former smoker and pack-years of cigarette smoking), dietary supplement use (>1/wk; yes or no), use of cholesterol-lowering medication (yes or no), intakes of fruit and vegetables (servings/d), and energy-adjusted intakes of dietary fiber (g/d), dietary vitamin E (IU/d), trans fat, and PUFA (g/d). P-trend values for dairy, meat, plant, and butter SF were 0.01, 0.12, 0.38, and 0.45, respectively. SF, saturated fat.
Isocaloric nutrient-substitution models
The substitution of 2% of energy from meat SF with a similar amount of energy from dairy SF was associated with 25% lower CVD risk [HR (95% CI): 0.75 (0.63, 0.91)] (Table 4). At 2000 kcal/d, this substitution would correspond to the exchange of 50 kcal or ∼5.5 g SF [eg, the replacement of ∼2 oz beef (∼57 g) or processed meat with one glass (∼240 mL) of whole milk or 1 cup of regular yogurt]. The replacement of energy from meat SF with butter or plant SF was associated with trends toward lower CVD risk, but 95% CIs were wide and findings were not significant, which was likely due to the low estimated intake of SF from these sources. The exchange of dairy SF with butter or plant SF, or butter SF with plant SF, was similarly not significantly associated with CVD risk, although again, 95% CIs were wide. When only CHD events were evaluated, results were similar to those for total CVD (see Table S3 under “Supplemental data” in the online issue).
TABLE 4.
HRs (95% CIs) for replacement of 2% percent of energy from SF from different food sources in the MESA (n = 5209; 316 new cases)1
| CVD | Model 2 |
| Dairy SF in replacement of meat SF | 0.75 (0.63, 0.91) |
| Butter SF in replacement of meat SF | 0.81 (0.64, 1.03) |
| Plant SF in replacement of meat SF | 0.63 (0.38, 1.03) |
| Butter SF in replacement of dairy SF | 1.08 (0.88, 1.33) |
| Plant SF in replacement of dairy SF | 0.83 (0.52, 1.33) |
| Plant SF in replacement of butter SF | 0.77 (0.48, 1.25) |
All values are HRs (95% CIs). Values were derived from proportional hazards models adjusted for age (y), sex, race-ethnicity (non-Hispanic white, African American, Hispanic, and Chinese American), study center, energy intake (kcal/d), education (<high school, high school, and >high school), alcohol intake (g/d), physical activity (active and sedentary leisure in metabolic equivalents-min per wk), BMI (in kg/m2), cigarette smoking (never, current, or former smoker and pack-years of cigarette smoking), dietary supplement use (>1/wk; yes or no), and use of cholesterol-lowering medication (yes or no). CVD, cardiovascular disease; MESA, Multi-Ethnic Study of Atherosclerosis; SF, saturated fat.
Subtypes of meat and dairy sources
When we separately evaluated types of meat, higher CVD risk was seen with intakes of SF from unprocessed meat [per +5 g/d, model 3 HR (95% CI): 1.48 (1.12, 1.93)] but not with intake of SF from processed meat [per +5 g/d, model 3 HR (95% CI): 1.07 (0.76, 1.49)]. However, in this cohort, the range of SF intake from processed meats was lower than that from unprocessed meats (90th percentile intake: 2.9 compared with 4.1 g/d, respectively), which potentially limited the detection of associations with processed meats. An ad hoc analysis of various dairy sources suggested that inverse associations between dairy SF and CVD may be driven by associations for whole-fat cheese rather than for low- or whole-fat milk (see Supplemental Figure 1 under “Supplemental data” in the online issue). Such ad hoc findings should be interpreted cautiously.
DISCUSSION
In this large multiethnic cohort, a higher intake of dairy SF was associated with lower CVD risk. In contrast, a higher intake of meat SF was associated with higher CVD risk. Total SF was associated with slightly lower risk of incident CVD; this effect was driven by dairy SF, which was the greatest contributor to total SF consumption in this population. We observed no significant associations of plant or butter SF with CVD risk, but ranges of intake of SF from these sources were narrow. Directions and magnitudes of these findings were similar when analyses were restricted to incident CHD. Although other studies have compared associations of the overall consumption of dairy foods and different types of meat with CVD, to our knowledge, this was the first study in which associations of the SF component from different food sources with CVD risk were evaluated.
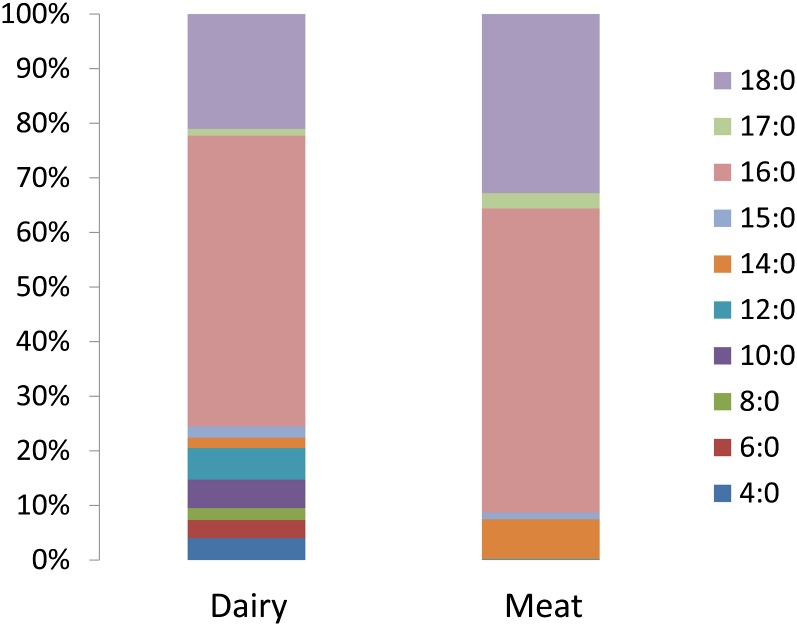
The observed differences in associations between food-specific SF and CVD may explain why overall SF consumption, summed from all sources, has not been significantly associated with incident CVD in numerous prospective cohort studies or in pooled analyses of these studies (4). These previous findings and our investigation do not raise questions about the established effects of SF consumption on plasma LDL. Rather, there are other potential explanations for our results. First, although food labels, dietary guidelines, and criteria for health claims consider only summed SF content and focus on LDL effects (1, 32, 33), these foods contain different proportions of different SFAs (ie, of varying carbon chain lengths) (Figure 2) that are known to have differing effects on various blood lipids and lipoproteins (8). For example, medium-chain SFAs, which are more common in dairy, raise HDL to a greater extent than does palmitic acid (SFA16:0), which composes the majority of SF in meats, producing favorable changes in the total cholesterol:HDL ratio compared with carbohydrate (8)
FIGURE 2.
Fatty acid profiles for dairy and meat products. The dairy profile corresponds to whole-fat American cheese; the meat profile corresponds to 15% fat ground beef. Data source: USDA National Nutrient Database for Standard Reference, Release 24 (http://ndb.nal.usda.gov/ndb/foods/list).
Second, it is plausible that the observed differences in risk cannot be explained by differences in SF per se but, instead, by differences in other components of foods that are more relevant than the SF content alone. Our analysis supports the idea that other components of meat or dairy (eg, sodium, other fatty acids, and other nutrients) may influence disease risk, perhaps through lipid or non–lipid-related pathways. Consistent with the concept of food synergy (34), our findings suggest that such other components might interact with SF and modify its relation with CVD risk by, for example, potentially offsetting its adverse effects (eg, other dairy components) or, conversely, by providing little benefit or even additional adverse effects (eg, other meat components). Consequently, health effects of the entire food rather than the content of any single nutrient might be most relevant to understanding associations between dietary consumption and health outcomes.
Few studies have reported associations between dairy products and CVD risk. In a recent meta-analysis that included 13,518 participants with 2283 CVD events from 4 prospective studies conducted in several countries, the pooled RR of total CVD associated with a 200 mL/d intake of all milk, which corresponds to 1–4 g dairy SF/d, was 0.94 (95% CI: 0.89, 0.99) (16). Conversely, the evaluation of CHD by using data from 6 prospective studies, which included ∼260,000 participants with 4391 CHD events, produced a pooled RR per 200-mL/d intake of all milk of 1.00 (95% CI: 0.96, 1.04) (16). In addition, no association was shown with total dairy intake (16). Unfortunately, only 2 of 6 studies in this meta-analysis included adjustment for potential dietary confounders. The general associations of higher SF consumption with a less-healthful lifestyle and diets overall, as evidenced by our data and the data of others (35, 36), indicate that SF and dairy consumption are likely to be confounded toward harm by other dietary habits, in particular the consumption of fiber, fruit and vegetables, PUFA, and vitamin E. In the recently published meta-analysis of milk consumption, the inverse association with CVD was observed only when fully adjusted models were used, which supports our explanation (16).
Dairy contains several nutrients that could help explain the observed inverse association of dairy SF with CVD risk. Higher concentrations of plasma trans palmitoleic acid, which is a fatty acid shown primarily in dairy foods, have been recently associated with higher HDL, lower triglycerides, lower C-reactive protein, lower insulin resistance, and lower incident diabetes in adults in the Cardiovascular Health Study (37). Other dairy nutrients including calcium, potassium, and phosphorus could have antihypertensive effects that may contribute to inverse associations with CVD risk (19, 38, 39). Consistent with the importance of evaluating foods rather than single nutrients, it is feasible that the complex mixture of dairy-food constituents as a whole may be most relevant for health effects. For example, previous studies have shown that higher intakes of calcium and phosphorus from dairy foods, but not from other sources, were associated with lower blood pressure (19, 40).
Our findings for meat SF are in general agreement with previous studies that evaluated associations between CVD and meat intake. A recent meta-analysis that included >600,000 participants with 22,000 CHD events from 4 cohorts and one case-control study showed total meat intake to be associated with a trend toward higher CHD risk [RR (95% CI) per 100 g total meat/d: 1.27 (0.94, 1.72)] (14). In studies that separately evaluated processed meats compared with unprocessed red meats, a positive association was observed only for processed meats [RR (95% CI) per 50 g processed meats/d: 1.42 (1.07, 1.89)] but not unprocessed meats [RR (95% CI) per 100 g unprocessed meats/d: 1.00 (0.81, 1.23)] (14). On average, in the United States, processed meats and unprocessed red meats have similar SF contents, which suggests that other nutrients, such as sodium and nitrates in processed meats, might explain these differences (14). A more recent analysis from the Nurses’ Health Study also showed higher risk of CHD with total meat consumption [RR (95% CI) across quintiles: 1.29 (95% CI: 1.12, 1.49)] than with unprocessed red meat consumption [RR (95% CI) across quintiles: 1.13 (95% CI: 0.99, 1.30)], although associations were more similar when intakes were evaluated continuously (30). Overall, our findings support an adverse association of SF consumption from meats with CVD risk but suggest that additional investigations are needed to confirm potential differences by types of meats and other constituents.
Our study has several strengths. We used data from a large, multiethnic cohort study, which allowed us to investigate a greater variety of dietary behaviors and susceptibility to CVD outcomes than might be present in a more racially and ethnically homogeneous population. The prospective design allowed us to estimate the incidence of disease with less concern for reverse causation between diet and outcomes. Finally, the evaluation of SF intake from different food sources provide novel insights into the relation between SF, the foods studied, and CVD.
Limitations should be considered. Potential measurement errors in exposure assessment were likely, which, if random, would have attenuated measures of association in most circumstances (41, 42). Although we were able to adjust for a variety of major risk factors, we cannot exclude the possibility of residual confounding because of unmeasured or poorly measured factors. On the basis of the observed directions of confounding in our cohort, residual confounding would likely have led to an overestimation of harms of SF from meat sources and an underestimation of benefits of SF from dairy sources. The relatively low consumption of SF from processed meats, butter, and plant sources may have limited the statistical power to detect associations in this cohort. Finally, we recognize that inferences of causality are limited in observational studies, and results from isocaloric substitution models should be interpreted with caution.
In conclusion, we showed that associations between SF and incident CVD depend on the food source; the consumption of dairy SF is inversely associated with risk, and the consumption of meat SF is positively associated with risk. Our findings raise the possibility that associations of foods that contain SF with health may depend on specific fatty acids present in these foods or the complex admixture of other food constituents, in addition to SF.
Supplementary Material
Acknowledgments
We thank the other investigators, staff, and participants of the MESA for their important contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
The authors’ responsibilities were as follows—MCOO: project conception, research plan, statistical analysis, and writing of the manuscript; DM, DRJ, and JAN: project conception and detailed review of the research plan and manuscript; and DK, AGB, and CTS: project conception and detailed review of the manuscript. DM has received research grants from GlaxoSmithKline, Sigma Tau, Pronova, and the NIH for an investigator-initiated, not-for-profit clinical trial of fish-oil supplements and postsurgical complications; ad hoc travel reimbursement and/or honoraria for research presentations on diet and cardiometabolic diseases from the International Life Sciences Institute, Aramark, Unilever, SPRIM, and Nutrition Impact; ad hoc consulting fees from Foodminds and McKinsey Health Systems Institute; and royalties from UpToDate for an online chapter on fish oil. Harvard University has filed a provisional patent application that has been assigned to Harvard University and lists DM as a coinventor to the US Patent and Trademark Office for use of trans palmitoleic acid to prevent and treat insulin resistance, type 2 diabetes, and related conditions. DRJ is an unpaid member of the scientific advisory board of the California Walnut Commission. MCOO, JAN, DK, AGB, and CTS had no conflicts of interest to declare.
Footnotes
Abbreviations used: CHD, coronary heart disease; CVD, cardiovascular disease; FFQ, food-frequency questionnaire; MESA, Multi-Ethnic Study of Atherosclerosis; SF, saturated fat.
REFERENCES
- 1.US Department of Agriculture and US Department of Health and Human Services Dietary guidelines for Americans, 2010. Washington, DC: US Government Printing Office, 2010 [Google Scholar]
- 2.Sanders TA. Fat and fatty acid intake and metabolic effects in the human body. Ann Nutr Metab 2009;55:162–72 [DOI] [PubMed] [Google Scholar]
- 3.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009;169:659–69 [DOI] [PubMed] [Google Scholar]
- 4.Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 2010;91:535–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med 2010;7:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard BV, Curb JD, Eaton CB, Kooperberg C, Ockene J, Kostis JB, Pettinger M, Rajkovic A, Robinson JG, Rossouw J, et al. Low-fat dietary pattern and lipoprotein risk factors: the Women's Health Initiative Dietary Modification Trial. Am J Clin Nutr 2010;91:860–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Micha R, Mozaffarian D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids 2010;45:893–905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–55 [DOI] [PubMed] [Google Scholar]
- 9.Kinosian B, Glick H, Preiss L, Puder KL. Cholesterol and coronary heart disease: Predicting risks in men by changes in levels and ratios. J Investig Med 1995;43:443–50 [PubMed] [Google Scholar]
- 10.Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH. A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med 1991;325:373–81 [DOI] [PubMed] [Google Scholar]
- 11.Assmann G, Schulte H, von Eckardstein A, Huang Y. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis 1996;124(suppl):S11–20 [DOI] [PubMed] [Google Scholar]
- 12.Lee DH, Folsom AR, Jacobs DR., Jr Iron, zinc, and alcohol consumption and mortality from cardiovascular diseases: the Iowa Women's Health Study. Am J Clin Nutr 2005;81:787–91 [DOI] [PubMed] [Google Scholar]
- 13.Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med 2009;169:562–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation 2010;121:2271–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldbohm RA, Chorus AMJ, Garre FG, Schouten LJ, van den Brandt PA. Dairy consumption and 10-y total and cardiovascular mortality: a prospective cohort study in the Netherlands. Am J Clin Nutr 2011;93:615–27 [DOI] [PubMed] [Google Scholar]
- 16.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, Geleijnse JM. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 2011;93:158–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Massey LK. Dairy food consumption, blood pressure and stroke. J Nutr 2001;131:1875–8 [DOI] [PubMed] [Google Scholar]
- 18.Engberink MF, Hendriksen MA, Schouten EG, van Rooij FJ, Hofman A, Witteman JC, Geleijnse JM. Inverse association between dairy intake and hypertension: the Rotterdam Study. Am J Clin Nutr 2009;89:1877–83 [DOI] [PubMed] [Google Scholar]
- 19.Alonso A, Nettleton JA, Ix JH, de Boer IH, Folsom AR, Bidulescu A, Kestenbaum BR, Chambless LE, Jacobs DR., Jr Dietary phosphorus, blood pressure, and incidence of hypertension in the atherosclerosis risk in communities study and the multi-ethnic study of atherosclerosis. Hypertension 2010;55:776–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–81 [DOI] [PubMed] [Google Scholar]
- 21.Nettleton JA, Steffen LM, Schulze MB, Jenny NS, Barr RG, Bertoni AG, Jacobs DR., Jr Associations between markers of subclinical atherosclerosis and dietary patterns derived by principal components analysis and reduced rank regression in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2007;85:1615–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol 1986;124:453–69 [DOI] [PubMed] [Google Scholar]
- 23.Mayer-Davis EJ, Vitolins MZ, Carmichael SL, Hemphill S, Tsaroucha G, Rushing J, Levin S. Validity and reproducibility of a food frequency interview in a multi-cultural epidemiology study. Ann Epidemiol 1999;9:314–24 [DOI] [PubMed] [Google Scholar]
- 24.Nettleton JA, Rock CL, Wang Y, Jenny NS, Jacobs DR., Jr Associations between dietary macronutrient intake and plasma lipids demonstrate criterion performance of the Multi-Ethnic Study of Atherosclerosis (MESA) food frequency questionnaire. Br J Nutr 2009;102:1220–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willett WC, Stampfer M. Implications of total energy intake for epidemiologic analyses : Willet W. (). Nutritional epidemiology. 2nd ed New York, NY: Oxford University Press, 1998:273–301 [Google Scholar]
- 26.Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med 2008;168:1333–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nettleton JA, Polak JF, Tracy R, Burke GL, Jacobs DR., Jr Dietary patterns and incident cardiovascular disease in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2009;90:647–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336–45 [DOI] [PubMed] [Google Scholar]
- 29.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551–61 [DOI] [PubMed] [Google Scholar]
- 30.Bernstein AM, Sun Q, Hu FB, Stampfer JE, Willet M, Willet WC. Major dietary protein sources and risk of coronary heart disease in women. Circulation 2010;122:876–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997;337:1491–9 [DOI] [PubMed] [Google Scholar]
- 32. US Food and Drug Administration. Health claims: general requirements. regulatory information. Report No. 21 CFR 101.14.
- 33. Office of Nutrition, Labeling, and Dietary Supplements of the US Food and Drug Administration. Guidance for industry: a food labeling guide. College Park, MD: US Food and Drug Administration; 2009.
- 34.Jacobs DR, Tapsell LC, Temple NJ. Food synergy: the key to balancing the nutrition research effort. Public Health Rev 2012;33:1–23 [Google Scholar]
- 35.Nettleton JA, Steffen LM, Mayer-Davis EJ, Jenny NS, Jiang R, Herrington DM, Jacobs DR., Jr Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2006;83:1369–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu FB, Stampfer MJ, Manson JE, Ascherio A, Colditz GA, Speizer FE, Hennekens CH, Willett WC. Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr 1999;70:1001–8 [DOI] [PubMed] [Google Scholar]
- 37.Mozaffarian D, Cao H, King IB, Lemaitre RN, Song X, Siscovick DS, Hotamisligil GS. Trans. -palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: A cohort study. Ann Intern Med 2010;153:790–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sacks FM, Willett WC, Smith A, Brown LE, Rosner B, Moore TJ. Effect on blood pressure of potassium, calcium, and magnesium in women with low habitual intake. Hypertension 1998;31:131–8 [DOI] [PubMed] [Google Scholar]
- 39.Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: A metaregression analysis of randomised trials. J Hum Hypertens 2003;17:471–80 [DOI] [PubMed] [Google Scholar]
- 40.Alonso A, Beunza JJ, Delgado-Rodriguez M, Martinez JA, Martinez-Gonzalez MA. Low-fat dairy consumption and reduced risk of hypertension: the Seguimiento Universidad de Navarra (SUN) cohort. Am J Clin Nutr 2005;82:972–9 [DOI] [PubMed] [Google Scholar]
- 41.Willet W. Nutritional epidemiology. 2nd ed New York, NY: Oxford University Press, 1998 [Google Scholar]
- 42.Dosemeci M, Wacholder S, Lubin JH. Does nondifferential misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol 1990;132:746–8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.