Abstract
Objectives
To identify factors that predict response to belimumab treatment in the phase 3 BLISS trials of autoantibody-positive systemic lupus erythematosus (SLE) and further analyse clinical efficacy in various patient subsets.
Methods
The BLISS trials compared belimumab 1 and 10 mg/kg versus placebo, all plus standard SLE therapy, over 52 or 76 weeks. Pooled subgroup analyses of week 52 SLE responder index rates (the primary endpoint in both trials) were performed based on demographic characteristics and baseline disease activity indicators. Pooled multivariate analysis was performed to determine predictors of response and treatment effect.
Results
Pooled univariate and multivariate analyses (N=1684) identified baseline factors associated with an increased benefit of belimumab versus placebo. These factors included the Safety Of Estrogens In Lupus Erythematosus National Assessment–Systemic Lupus Erythematosus Disease Activity Index (SELENA–SLEDAI) ≥10, low complement, anti-dsDNA positivity and corticosteroid use. Efficacy outcomes were assessed in the low complement/anti-dsDNA-positive and SELENA–SLEDAI ≥10 subgroups. Week 52 SLE Responder Index rates in the low complement/anti-dsDNA-positive subgroup were 31.7%, 41.5% (p=0.002) and 51.5% (p<0.001) with placebo and belimumab 1 mg/kg and 10 mg/kg, respectively; corresponding rates in the SELENA–SLEDAI ≥10 subgroup were 44.3%, 58.0% (p<0.001) and 63.2% (p<0.001). Further analysis of secondary endpoints in the low complement/anti-dsDNA-positive subgroup showed that compared with placebo, belimumab produced greater benefits regarding severe flares, corticosteroid use and health-related quality of life.
Conclusions
These findings suggest that belimumab has greater therapeutic benefit than standard therapy alone in patients with higher disease activity, anti-dsDNA positivity, low complement or corticosteroid treatment at baseline.
ClinicalTrials.gov
identifiers NCT00424476 and NCT00410384
Systemic lupus erythematosus (SLE) is a chronic, heterogeneous autoimmune disease associated with considerable morbidity, increased mortality and poor health-related quality of life (HRQoL).1 2 Anti-double-stranded DNA antibodies and low complement (C) levels are associated with more severe disease;3–8 the European League Against Rheumatism (EULAR) Task Force recommends that serum C3/C4 and anti-dsDNA be considered for monitoring patients with SLE because these markers may provide prognostic information on general outcome and the involvement of major organs, and have diagnostic utility in assessing SLE activity and flares.9
In the phase 3 BLISS trials over 52 (BLISS-52) or 76 (BLISS-76) weeks, treatment with belimumab—a soluble B lymphocyte stimulator-specific inhibitor—combined with current standard SLE therapy had superior responder rates (as assessed by the SLE Responder Index; SRI) compared with standard therapy alone in patients with autoantibody-positive SLE.10 11 The designs of these two trials were based on the results of a phase 2 study of belimumab, which showed evidence of efficacy in patients with autoantibody-positive SLE.12 Belimumab is currently indicated in the EU as ‘add-on therapy in adult patients with active, autoantibody-positive SLE with a high degree of disease activity (eg, low complement and anti-dsDNA positivity) despite standard therapy’. The present report describes analyses of baseline demographic and disease characteristics that were performed to identify factors that predicted response to belimumab treatment in the two BLISS studies. In addition, key efficacy findings are explored in the subgroup of patients who had low complement levels and were anti-dsDNA positive at baseline, a characteristic that was associated with both a high degree of disease activity at baseline and subsequent response to belimumab therapy.
Methods
BLISS-52 (N=865; ClinicalTrials.gov NCT00424476) and BLISS-76 (N=819; ClinicalTrials.gov NCT 00410384) were randomised, double-blind, placebo controlled, multicentre trials comparing belimumab 1 and 10 mg/kg plus standard therapy with placebo plus standard therapy in patients with active SLE. The trials had similar clinical designs that have been described in detail previously.10 11 All patients had a Safety Of Estrogens In Lupus Erythematosus National Assessment–Systemic Lupus Erythematosus Disease Activity Index (SELENA–SLEDAI) score of 6 or greater at screening, were autoantibody positive (antinuclear antibody ≥1:80 or anti-dsDNA ≥30 IU/ml), and had received stable standard therapy for 30 days or more before the study. Patients received standard therapy plus belimumab or placebo by intravenous infusion on days 0, 14 and 28, and then every 28 days to week 48 (BLISS-52) or 72 (BLISS-76). Patients had progressive restrictions on concurrent immunosuppressive and antimalarial medications and corticosteroids during the trials.
The primary endpoint in both trials was the SRI rate at week 52. The SRI is a composite responder index that includes one measure of disease activity improvement (≥4-point decrease in SELENA–SLEDAI score) and two measures to ensure that the improvement in disease activity is not offset by a worsening of disease in organ systems (ie, no new British Isles Lupus Assessment Group A and no more than one new B scores) or by a decline in overall health status (ie, <0.3-point increase from baseline in Physician's Global Assessment score).10–13 The SELENA–SLEDAI score reduction drives the SRI response as a score reduction generally requires normalisation of laboratory parameters or resolution, rather than only partial improvement, of a clinical manifestation. A 4-point reduction is, therefore, considered clinically meaningful.14 In addition, dose increases of concomitant medications, which would suggest disease worsening, were not allowed beyond protocol-specified limitations, thus further enhancing the clinical relevance of an SRI response in these studies. Patients who withdrew or required changes in background drugs for SLE other than those permitted by protocol were judged to be treatment failures.
Subgroup analyses of SRI rates at week 52 (also referred to as univariate analyses) were performed based on demographic characteristics (eg, age, sex, race, ethnicity, region) and baseline disease activity indicators (eg, SELENA–SLEDAI score, serological activity, corticosteroid and immunosuppressant use). Data from the phase 3 trials were pooled to allow for maximum sample size within subgroups. Analyses of categorical variables, including the primary endpoint, were performed using a logistic-regression model. Analysis of covariance was used for continuous variables, such as the change from baseline endpoints. Analyses of time to flares were performed using Cox regression. These analyses were adjusted for baseline stratification factors and were not subjected to any adjustments for multiple testing.
The analyses were performed in combined data from the two phase 3 studies to achieve a more stable estimate of belimumab's global treatment effect, as the studies were essentially identical in design and the effects of belimumab on the endpoints of interest were similar between the studies. In addition to the individual subgroup analyses, a multivariate analysis was performed based on pooled data to determine predictors of response and the effect of treatment adjusted for predictive factors. A main-effect logistic-regression model was developed using a stepwise forward selection process to identify baseline factors predictive of SRI response at week 52 irrespective of the treatment received. An interaction logistic-regression model, in which factors meeting a 0.05 significance level from the main-effect model were retained, was then used to determine how response to belimumab versus placebo varied across different categories within a baseline characteristic (ie, independent treatment-effect modifiers).
Multivariate analyses identified high disease activity—patients with both low complement levels and anti-dsDNA positivity, and those with SELENA–SLEDAI scores of 10 or greater—as being predictive of a response to belimumab treatment. Patients with low complement/anti-dsDNA positivity are immunologically active, at high risk of severe flares,6 and easily identifiable by laboratory studies readily available in the clinical setting. Furthermore, the presence of high disease activity in the low complement/anti-dsDNA-positive subgroup in the trials was supported by the high frequency of corticosteroid use (91.4%) (table 1). With regard to the SELENA–SLEDAI ≥10 subgroup, although SELENA–SLEDAI is a validated measure of disease activity, this assessment is not commonly used by physicians outside of the clinical trial setting. Results in the present report on the SELENA–SLEDAI ≥10 subgroup have, therefore, been limited to the primary efficacy endpoint.
Table 1.
Baseline characteristics of total pooled phase 3 population and low complement/anti-dsDNA-positive subgroup
| Total phase 3 pooled (n=1684) | Low complement/anti-dsDNA positive (n=876) | |
|---|---|---|
| Mean SELENA–SLEDAI score ±SD | 9.7±3.8 | 10.8±3.8 |
| SELENA–SLEDAI ≥10, % | 52.1 | 65.5 |
| Proteinuria (≥2 g/24 h), % | 5.9 | 8.8 |
| Anti-dsDNA (≥30 IU/ml), % | 69.4 | 100 |
| IgG (>16.2 g/l), % | 44.2 | 53.0 |
| Low C3 (<90 mg/dl), % | 45.0 | 75.3 |
| Low C4 (<16 mg/dl), % | 56.1 | 91.4 |
| Corticosteroid use, % | 86.3 | 91.4 |
| >7.5 mg/day, % | 58.0 | 63.5 |
| Immunosuppressant use, % | 48.7 | 53.4 |
| Mean SLICC damage index score ±SD | 0.8±1.2 | 0.7±1.1 |
| Mean PGA score ±SD | 1.4±0.5 | 1.4±0.5 |
C, complement; Ig, immunoglobulin; PGA, Physician's Global Assessment; SELENA–SLEDAI, Safety Of Estrogens In Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index; SLICC, Systemic Lupus International Collaborating Clinics.
Results
Baseline characteristics of the pooled BLISS-52 and BLISS-76 population are shown in table 1. High disease activity was common, as indicated by SELENA–SLEDAI scores of 10 or greater in 52% of patients, corticosteroid use in 86% and anti-dsDNA positivity in 69%. In addition, 45% of patients had low C3 levels and 56% had low C4 levels. In the pooled analysis of BLISS-52 and BLISS-76 (N=1684), SRI rates at week 52 were 38.8% with placebo and 46.2% with belimumab 1 mg/kg and 50.6% with 10 mg/kg. Between-treatment differences for belimumab versus placebo were 7.4% (OR 1.4, 95% CI 1.1 to 1.8, p=0.006) with 1 mg/kg and 11.8% (OR 1.7, 95% CI 1.3 to 2.2, p<0.001) with 10 mg/kg.
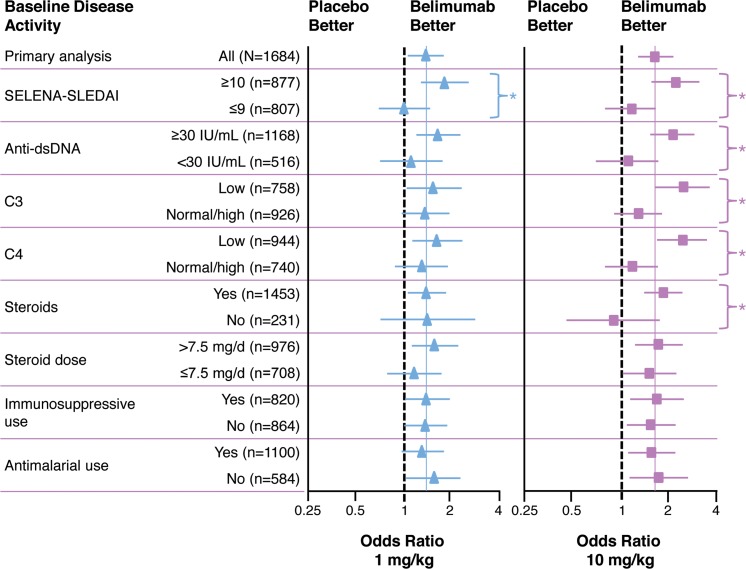
Univariate subgroup analysis
Patients with higher baseline disease activity—denoted by a higher SELENA–SLEDAI score, low complement levels, detectable anti-dsDNA, or treatment with corticosteroids—had a greater response to belimumab versus standard therapy alone than did those without these characteristics (figure 1). The greater benefit of belimumab treatment in patients with high disease activity was more marked with 10 mg/kg than with 1 mg/kg, suggesting a dose-related effect—eg, the week-52 SRI rate was higher with 10 mg/kg versus 1 mg/kg in those who had a SELENA–SLEDAI score of 10 or greater (63.2% vs 58.0%), were positive for anti-dsDNA antibodies (51.1% vs 45.4%), or had low C3 (50.8% vs 39.9%) or C4 (50.8% vs 41.7%) levels. Treatment by subgroup interactions (p<0.10) were observed for SELENA–SLEDAI (score ≥10 vs ≤9) with both belimumab 1 and 10 mg/kg, and for anti-dsDNA antibodies (≥ vs <30 IU/ml), C3 (low vs normal/high level), C4 (low vs normal/high) and corticosteroid use (yes vs no) with 10 mg/kg. No significant interaction was observed for corticosteroid dose (> vs ≤7.5 mg/day), antimalarial use (yes vs no) or immunosuppressive use (yes vs no). For demographic variables, the only significant interaction observed was for region with belimumab 10 mg/kg, an interaction driven by better SRI rates in the western Europe/Australia/Israel regions (24.3% with placebo, and 36.8% and 51.9% with belimumab 1 and 10 mg/kg, respectively; p<0.05; n=217) than in all other regions.
Figure 1.
OR for SLE Responder Index rates in univariate disease activity subgroup analysis. Horizontal lines are 95% CI. Vertical dashed reference lines represent OR of 1, which indicates no difference between belimumab and placebo, while points to right of lines indicate higher responses for belimumab versus placebo and points to left of line indicate lower responses for belimumab versus placebo. Point estimates for OR for overall treatment effect (coloured solid vertical lines) are 1.41 for belimumab 1 mg/kg and 1.68 for 10 mg/kg. *Interaction p<0.1. C, complement; SELENA–SLEDAI, Safety Of Estrogens In Lupus Erythematosus National Assessment-Systemic Lupus Erythematosus Disease Activity Index.
Multivariate analysis
Analysis of factors associated with response irrespective of treatment group, while controlling for study and each of the significant predictors of response in the model, showed that belimumab significantly increased the odds of an SRI response at week 52 compared with standard therapy alone. A more marked effect was observed with belimumab 10 mg/kg (adjusted OR 1.5, 95% CI 1.2 to 1.9, p=0.002 with 1 mg/kg; adjusted OR 1.8, 95% CI 1.4 to 2.4, p<0.001 with 10 mg/kg). In addition, a multivariate analysis was performed to determine whether the response with belimumab versus standard therapy alone varied across different subgroups. This analysis generally supported the results of the individual subgroup analysis, again indicating that patients with greater baseline disease activity—as reflected by a SELENA–SLEDAI score of 10 or greater, corticosteroid use and low complement levels—benefited most from belimumab treatment (data not shown).
Outcomes in high disease activity subgroups
As the multivariate analyses identified indicators of high disease activity—either clinically or serologically, or both—as predictors of a response to belimumab treatment, efficacy outcomes were then assessed in the pooled BLISS trials in the two high disease activity subgroups noted previously: patients with both low complement levels and anti-dsDNA positivity, and patients with SELENA–SLEDAI scores of 10 or greater. Of the 1684 autoantibody-positive patients in the pooled dataset, 876 (52.0%) had low C3 or C4 levels and were anti-dsDNA positive, and 877 (52.1%) had SELENA–SLEDAI scores of 10 or greater. The two subgroups exhibited considerable overlap, with 574 patients (65.5%) in the low complement/anti-dsDNA-positive group having a SELENA–SLEDAI score of 10 or greater at baseline.
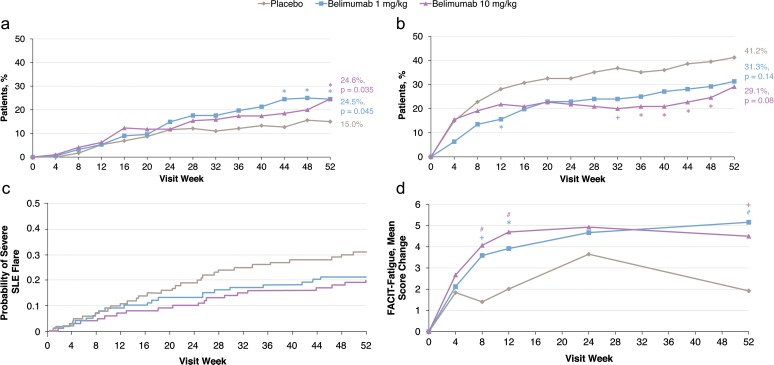
Primary efficacy endpoint in the low complement/anti-dsDNA-positive and SELENA–SLEDAI ≥10 subgroups
The SRI rates at week 52 in the low complement/anti-dsDNA-positive subgroup were 31.7% with standard therapy alone, 41.5% with belimumab 1 mg/kg (p=0.002) and 51.5% with belimumab 10 mg/kg (p<0.001; table 2, figure 2A). Corresponding rates in the SELENA–SLEDAI ≥10 subgroup were 44.3%, 58.0% (p<0.001) and 63.2% (p<0.001). Significant differences in SRI rates were observed between belimumab 10 mg/kg and placebo beginning at week 8 in both subgroups (except for week 20 in the SELENA–SLEDAI ≥10 subgroup, p=0.07), and between belimumab 1 mg/kg and placebo from week 28 in the low complement/anti-dsDNA-positive subgroup, and from week 36 in the SELENA–SLEDAI ≥10 subgroup (data not shown). To test the belimumab treatment effect in the low complement/anti-dsDNA-positive subgroup, a modified SRI analysis was performed excluding the complement and anti-dsDNA components from SELENA–SLEDAI scoring, as the 4-point reduction in the SELENA–SLEDAI score required for a SRI response can be achieved by normalisation of complement levels and anti-dsDNA antibodies. This analysis confirmed a treatment benefit with belimumab versus placebo at week 52 in the low complement/anti-dsDNA-positive subgroup (table 2, figure 2B).
Table 2.
Efficacy outcomes in low complement/anti-dsDNA-positive subgroup in pooled BLISS-52 and BLISS-76 population
| Efficacy outcome | Placebo (n=287) | Belimumab 1 mg/kg (n=284) | Belimumab 10 mg/kg (n=305) |
|---|---|---|---|
| SRI rate | |||
| SRI at week 52, % | 31.7 | 41.5 | 51.5 |
| p value | 0.002 | <0.001 | |
| Observed treatment difference vs placebo, % | 9.8 | 19.8 | |
| Modified SRI excluding complement and anti-dsDNA changes at week 52, % | 28.9 | 38.7 | 46.2 |
| p value | 0.001 | <0.001 | |
| Observed treatment difference vs placebo, % | 9.8 | 17.3 | |
| SRI at week 76 in BLISS-76, % | (n=131) 27.5 | (n=125) 36.0 | (n=134) 39.6 |
| p value | 0.10 | 0.02 | |
| Observed treatment difference vs placebo, % | 8.5 | 12.1 | |
| Secondary outcomes in pooled population | |||
| Patients with severe flare over 52 weeks, % | 29.6 | 20.4 | 19.0 |
| p value | 0.02 | 0.004 | |
| Observed treatment difference vs placebo, % | 9.2 | 10.6 | |
| Time to severe flare, HR (95% CI) | 0.67 (0.48, 0.94) | 0.61 (0.44, 0.85) | |
| Prednisone reduction by ≥25% from baseline to ≤7.5 mg/day during weeks 40–52, %* | (n=173) 12.1 | (n=188) 22.9 | (n=195) 18.5 |
| p value | 0.02 | 0.15 | |
| Observed treatment difference vs placebo, % | 10.7 | 6.3 | |
| SF-36 PCS score change from baseline at week 52, LS mean±SE | (n=287) 3.19±0.61 | (n=282) 4.57±0.59 | (n=297) 4.76±0.59 |
| p value | 0.03 | 0.01 | |
| Observed mean treatment difference vs placebo | 1.38 | 1.56 | |
| FACIT–Fatigue score improvement from baseline at week 52, LS mean±SE | 1.80±0.77 | 4.74±0.75 | 4.07±0.75 |
| p value | <0.001 | 0.004 | |
| Observed mean treatment difference vs placebo | 2.94 | 2.27 | |
Among patients with baseline prednisone dose greater than 7.5 mg/day.
FACIT, functional assessment of chronic illness therapy; HR, hazard ratio; LS, least squares; PCS, physical component summary; SF-36, short form 36; SRI, Systemic Lupus Erythematosus Responder Index.
Figure 2.
Systemic Lupus Erythematosus Responder Index rates in (a) pooled low complement/anti-dsDNA-positive subgroup (n=876), (b) pooled low complement/anti-dsDNA-positive subgroup with analysis excluding serology (n=876) and (c) low complement/anti-dsDNA-positive subgroup in BLISS-76 (n=390). *p<0.05; +p<0.01; #p<0.001.
To determine if responses in these subgroups persisted with longer treatment, outcomes by subgroup were assessed in the BLISS-76 trial, in which patients continued to receive belimumab or standard therapy alone to 76 weeks. In the low complement/anti-dsDNA-positive subgroup, SRI rates were higher with belimumab versus placebo, with significant differences observed with belimumab 10 mg/kg at weeks 52, 60, 68, 72 and 76 (figure 2C).
Secondary efficacy endpoints in the low complement/ anti-dsDNA-positive subgroup
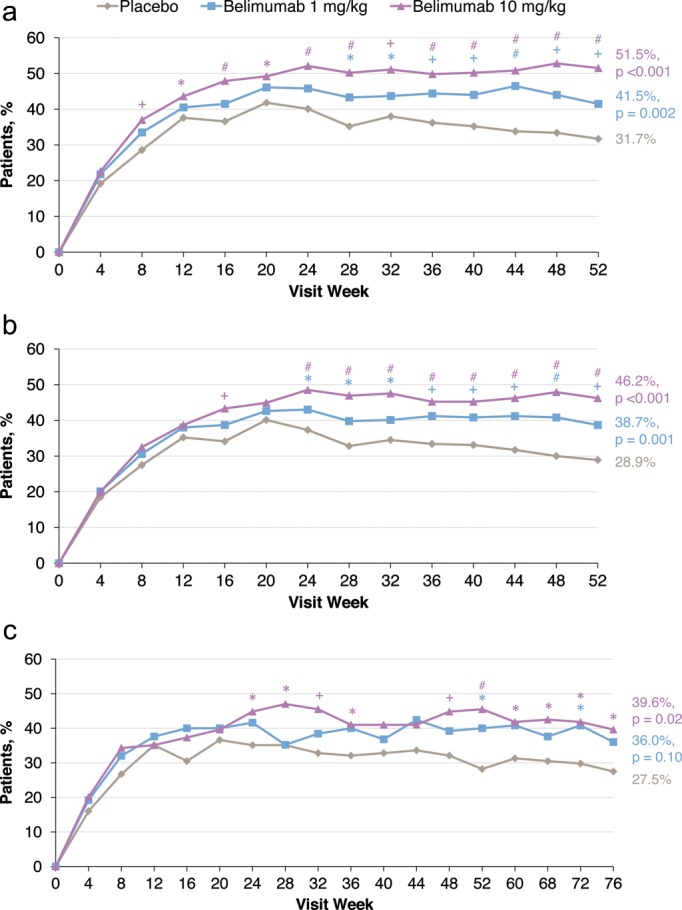
Further analyses of corticosteroid use, flare occurrence and HRQoL secondary endpoints were performed in the low complement/anti-dsDNA-positive subgroup. Of patients receiving a prednisone dose greater than 7.5 mg/day at baseline, more receiving belimumab than standard therapy alone had dose reductions of 25% or greater to 7.5 mg/day or less during weeks 40–52 and any dose reductions to 7.5 mg/day or less at week 52 (table 2, figure 3A), and fewer patients receiving belimumab had dose increases (figure 3B). Belimumab treatment significantly reduced the risk of a first severe flare (figure 3C), and rates of both severe flares (per patient-year: placebo, 0.63; belimumab 1 mg/kg, 0.43 [p=0.015]; belimumab 10 mg/kg, 0.37 [p<0.001]) and any flares (placebo, 3.31; 1 mg/kg, 2.44 [p<0.001]; 10 mg/kg, 2.20 [p<0.001]). With regard to HRQoL measures, both belimumab doses were associated with significantly greater improvements in Functional Assessment Of Chronic Illness Therapy–Fatigue scale scores at week 52, with differences observed as early as week 8 (table 2, figure 3D), and in short form 36 health survey physical component summary scores (least-squares mean treatment difference vs placebo: belimumab 1 mg/kg, +1.38 [p=0.03]; belimumab 10 mg/kg, +1.56 [p=0.01]; table 2).
Figure 3.
BLISS trial secondary endpoints in pooled low complement/anti-dsDNA-positive subgroup. (a) Proportions of patients with reduction in corticosteroid dose to 7.5 mg/day or less in patients receiving more than 7.5 mg/day at baseline (n=556). (b) Proportions of patients with increase in corticosteroid dose to more than 7.5 mg/day in patients receiving 7.5 mg/day or less at baseline (n=320). (c) Time to first severe flare (n=876). Hazard ratio (95% CI; p value) versus placebo: 0.67 (0.48–0.94; 0.02) for belimumab 1 mg/kg and 0.61 (0.44–0.85; 0.004) for belimumab 10 mg/kg. (D) Mean change in Functional Assessment Of Chronic Illness Therapy (FACIT)–Fatigue score (n=858). SLE, systemic lupus erythematosus. *p<0.05; +p<0.01; #p<0.001.
Safety in the low complement/anti-dsDNA-positive subgroup
In the low complement/anti-dsDNA-positive subgroup, the belimumab and placebo groups had similar rates of adverse events (AEs), AEs considered to be related to study treatment, severe AEs and AEs leading to dose interruption or discontinuation of study medication (table 3). Rates of serious AEs were somewhat higher with belimumab, but there was no excess of AEs within any individual system organ class. Furthermore, rates of serious infections were similar across treatment groups. The AE rates in the low complement/anti-dsDNA-positive subgroup were similar to those in the overall pooled population for the three treatment groups.
Table 3.
Adverse events in low complement/anti-dsDNA-positive subgroup
| AE | Placebo (n=287) | Belimumab 1 mg/kg (n=284) | Belimumab 10 mg/kg (n=305) |
|---|---|---|---|
| ≥1 AE, % | 92 | 92 | 93 |
| ≥1 Serious AE, % | 15 | 21 | 20 |
| ≥1 Serious infection, % | 7 | 8 | 5 |
| ≥1 Severe AE, %* | 14 | 16 | 17 |
| ≥1 Serious and/or severe AE, % | 20 | 25 | 26 |
| ≥1 AE resulting in discontinuation, % | 9 | 7 | 8 |
| Deaths, n (%)† | 1 (<1) | 2 (<1) | 3 (<1) |
Severe refers to grades 3 (severe: causing inability to perform usual activities) and 4 (life-threatening: potentially life-threatening or disabling, with significant medical intervention required).
The primary causes of death were: unknown with placebo; unknown and sepsis with belimumab 1 mg/kg; and cardiac arrest, acute infective diarrhoea and respiratory insufficiency with belimumab 10 mg/kg.
AE, adverse event.
Discussion
The BLISS-52 and BLISS-76 trials showed that belimumab plus standard SLE therapy resulted in significantly greater SRI rates than did placebo plus standard therapy at 52 weeks in antinuclear antibody-positive or anti-dsDNA-positive SLE patients.10 11 Univariate and multivariate analyses in the pooled population of the BLISS trials identified baseline factors associated with an increased benefit of belimumab treatment versus placebo. These factors consisted of SELENA–SLEDAI scores of 10 or greater, low complement levels, anti-dsDNA positivity and the requirement for corticosteroid treatment. Among these factors, SELENA–SLEDAI is a reliable index of SLE disease activity, although it is used primarily in clinical trials and in certain highly specialised centres. Although corticosteroid treatment is relatively subjective, dependent partly on physician experience and access to other treatments, it may be a sign of higher underlying disease activity. Complement and anti-dsDNA levels, however, are objective measures and routine laboratory tests that are widely available in clinical practice, and may be prognostic markers for major organ involvement. Monitoring of these serological markers is supported by EULAR recommendations for the management of SLE.9
In the multivariate analysis of SRI response, both belimumab doses plus standard therapy demonstrated a better treatment effect than standard therapy alone in all SELENA–SLEDAI score categories and corticosteroid dosing levels tested, and for patients with low C3 or C4 levels, with the 10 mg/kg dose appearing to provide greater benefit in all measures.
At baseline, 52% of the pooled BLISS trial population had low complement levels and were anti-dsDNA positive. The presence of high disease activity in this subgroup is supported by the observations that two-thirds of these patients had a SELENA–SLEDAI score of 10 or greater and nearly all required corticosteroid treatment at baseline. In addition, patients in this low complement/anti-dsDNA-positive subgroup were more difficult to treat with standard therapy alone as their SRI rate was 32% compared with 39% in the overall population and 44% in the SELENA–SLEDAI ≥10 subgroup. In this low complement/anti-dsDNA-positive subgroup, belimumab treatment was associated with significantly greater SRI rates at 52 weeks versus placebo, including when complement and anti-dsDNA changes were excluded from the calculation of the SELENA–SLEDAI score as a component of the SRI. For both these measures, the treatment differences for belimumab versus placebo in this subgroup were greater than those between belimumab and placebo in the total pooled BLISS population. In the BLISS-76 trial, SRI rates were numerically greater with belimumab 1 mg/kg and significantly greater with 10 mg/kg from weeks 52 to 76 in this subgroup, with the treatment differences also being greater than those in the total BLISS-76 population. Analysis of 52-week outcomes for BLISS trial secondary endpoints in this subgroup showed that belimumab treatment reduced the risk of a first severe flare, increased the proportion of patients with corticosteroid dose reductions, and decreased the proportion with corticosteroid dose increases, and improved HRQoL. In accordance with the phase 2 belimumab trial, these findings suggest that belimumab has a relatively greater benefit in patients with higher disease activity, or low complement levels or anti-dsDNA positivity, and are consistent with the mechanism of action of belimumab.12 15 16 Furthermore, the finding that these benefits were present when complement and anti-dsDNA changes were excluded from the SELENA–SLEDAI component of response demonstrates the benefits in clinical aspects and suggests that the benefits are not solely due to the resolution of serological activity.
The subgroup analysis comprises combined data from two separate clinical trials of patients from different international regions, and the retrospective nature of these analyses means the results need confirmation in a prospective study. As patients with severe active lupus nephritis or severe active central nervous system manifestations, as well as patients treated with other biological agents or intravenous cyclophosphamide, were excluded from the two trials, no conclusion can be drawn in these patients.
In summary, the subgroup data from the BLISS-52 and BLISS-76 clinical trials suggest that belimumab may be particularly effective in patients characterised by higher SLE disease activity at baseline, who are identified by anti-dsDNA positivity, hypocomplementaemia, or requiring treatment with corticosteroids. In these subgroups of patients, a range of clinical benefits with belimumab treatment was demonstrated, including improved disease activity, reduced risk of flares and an effect on steroid reduction. These findings may be of use to the practising clinician and may represent a first step towards identifying SLE disease characteristics in patients that can enhance the potential for a response to a given biological therapy.
Acknowledgments
Editorial support (writing assistance, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by Matt Stenger and Eleanore Gross of BioScience Communications, New York, NY, USA, and was funded by Human Genome Sciences, Inc, Rockville, Maryland, USA, and GlaxoSmithKline, Uxbridge, UK.
Footnotes
Correction notice: This article has been corrected since it was published Online First. On page 2, in line 13, "no more than two new B scores)" was changed to "no more than one new B score)".
Contributors: All authors have read and approved the manuscript, and participated in study design, data acquisition, analysis, and interpretation, and manuscript drafting and revision.
Funding: This study was funded by Human Genome Sciences and GlaxoSmithKline.
Ethics approval: Ethics approval was granted by the institutional review boards at every clinical study site.
Competing interests: RFvV has received consultancy fees and honoraria from Human Genome Sciences and GlaxoSmithKline. MAP and RC have received payment for board membership and consultancy from Human Genome Sciences and GlaxoSmithKline. DAR, BNJ and CSK are employed by and own stock in GlaxoSmithKline. ZJZ and WF are employed by and own stock in Human Genome Sciences.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lau CS, Mak A. The socioeconomic burden of SLE. Nat Rev Rheumatol 2009;5:400–4 [DOI] [PubMed] [Google Scholar]
- 2.Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med 2008;358:929–39 [DOI] [PubMed] [Google Scholar]
- 3.Biesen R, Dähnrich C, Rosemann A, et al. Anti-dsDNA-NcX ELISA: dsDNA-loaded nucleosomes improve diagnosis and monitoring of disease activity in systemic lupus erythematosus. Arthritis Res Ther 2011;13:R26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merrill JT, Buyon JP. The role of biomarkers in the assessment of lupus. Best Pract Res Clin Rheumatol 2005;19:709–26 [DOI] [PubMed] [Google Scholar]
- 5.Nasiri S, Karimifar M, Bonakdar ZS, et al. Correlation of ESR, C3, C4, anti-DNA and lupus activity based on British Isles Lupus Assessment Group Index in patients of rheumatology clinic. Rheumatol Int 2010;30:1605–9 [DOI] [PubMed] [Google Scholar]
- 6.Petri M, Singh S, Tesfasyone H, et al. Prevalence of flare and influence of demographic and serologic factors on flare risk in systemic lupus erythematosus: a prospective study. J Rheumatol 2009;36:2476–80 [DOI] [PubMed] [Google Scholar]
- 7.Schur PH, Sandson J. Immunologic factors and clinical activity in systemic lupus erythematosus. N Engl J Med 1968;278:533–8 [DOI] [PubMed] [Google Scholar]
- 8.van den Berg L, Nossent H, Rekvig O. Prior anti-dsDNA antibody status does not predict later disease manifestations in systemic lupus erythematosus. Clin Rheumatol 2006;25:347–52 [DOI] [PubMed] [Google Scholar]
- 9.Bertsias G, Ioannidis JP, Boletis J, et al. EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis 2008;67:195–205 [DOI] [PubMed] [Google Scholar]
- 10.Furie R, Petri M, Zamani O, et al. ; BLISS-76 Study Group A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus. Arthritis Rheum. 2011;63:3918–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Navarra SV, Guzmán RM, Gallacher AE, et al. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Lancet 2011;377:721–31 [DOI] [PubMed] [Google Scholar]
- 12.Wallace DJ, Stohl W, Furie RA, et al. A phase II, randomized, double-blind, placebo-controlled, dose-ranging study of belimumab in patients with active systemic lupus erythematosus. Arthritis Rheum 2009;61:1168–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furie RA, Petri MA, Wallace DJ, et al. Novel evidence-based systemic lupus erythematosus responder index. Arthritis Care Res 2009;61:1143–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gladman DD, Urowitz MB, Kagal A, et al. Accurately describing changes in disease activity in systemic lupus erythematosus. J Rheumatol 2000;27:377–9 [PubMed] [Google Scholar]
- 15.Baker KP, Edwards BM, Main SH, et al. Generation and characterization of LymphoStat-B, a human monoclonal antibody that antagonizes the bioactivities of B lymphocyte stimulator. Arthritis Rheum 2003;48:3253–65 [DOI] [PubMed] [Google Scholar]
- 16.Halpern WG, Lappin P, Zanardi T, et al. Chronic administration of belimumab, a BLyS antagonist, decreases tissue and peripheral blood B-lymphocyte populations in cynomolgus monkeys: pharmacokinetic, pharmacodynamic, and toxicologic effects. Toxicol Sci 2006;91:586–99 [DOI] [PubMed] [Google Scholar]