ABSTRACT
Purpose: As the numbers of Canadians aged 65 years and over increases over the next 20 years, the prevalence of chronic conditions, including arthritis, will rise as will the number of falls. Although known fall-risk factors are associated with hip and knee osteoarthritis (OA), minimal research has evaluated fall and fracture risk and/or rates in this population. Thus, the purpose was to summarize research on fall and fracture risk in older adults with hip or knee OA and to develop a conceptual framework of fall-risk screening and assessment. Method: The International Classification of Functioning, Disability and Health, clinical practice guidelines for fall-risk screening, and a selected literature review were used. Results: Gaps exist in our knowledge of fall and fracture risk for this population. Muscle performance, balance, and mobility impairments have been identified, but little is known about whether personal and environmental contextual factors impact fall and fracture risk. Physical activity may help to prevent falls, but non-adherence is a problem. Conclusion: A need exists to assess fall risk in older adults with hip and knee OA. Promoting regular physical activity by focusing on disease- and activity-specific personal contextual factors may help direct treatment planning.
Key Words: accidental falls, pain, osteoarthritis, risk factors
RÉSUMÉ
Objectif : Le nombre de Canadiens de 65 ans et plus augmentera au cours des 20 prochaines années et la prévalence des maladies chroniques, dont l'arthrite, sera en hausse, tout comme le nombre de chutes. Bien que des facteurs de risques de chute connus soient associés à l'arthrose du genou ou de la hanche, une somme minimale de recherches a évalué les risques ou les taux de chutes et de fractures chez ce segment de la population. En conséquence, l'objectif de cette étude était de dresser un résumé des recherches réalisées sur les risques de chute ou de fracture chez les adultes plus âgés aux prises avec de l'arthrose au genou ou à la hanche, et d'élaborer un cadre conceptuel pour le dépistage et l'évaluation des risques de chute. Méthode : La Classification internationale du fonctionnement, du handicap et de la santé (CIF), qui forme les directives cliniques pour le dépistage des risques de chute, et une revue documentaire sélective ont été utilisées. Résultats : Il existe des lacunes dans nos connaissances relatives aux risques de chute et de fracture au sein de ce segment de la population. La dégradation de la performance musculaire, de l'équilibre et de la mobilité a été établie, mais on sait peu de choses en ce qui a trait aux répercussions possibles de facteurs contextuels personnels ou environnementaux sur les risques de chute ou de fracture. L'activité physique peut aider à prévenir les chutes, mais la non-adhésion des patients à un programme d'activité physique pose problème. Conclusion : Une évaluation des risques de chute chez les adultes plus âgés souffrant d'arthrose du genou ou de la hanche est nécessaire. La promotion de l'activité physique régulière, en se concentrant sur les facteurs contextuels personnels propres à la maladie ou à l'activité, pourrait aider directement la planification du traitement.
Mots clés : facteurs de risque, chutes accidentelles, douleurs, arthrose
Osteoarthritis (OA) affects 1 in 10 Canadians1 and is a common cause of functional deterioration in older adults. As Canada's population continues to age, with increasing numbers of people living beyond 80 years, the prevalence of OA is predicted to increase substantially. Long-term disability due to OA in Canada accounts for almost 80% of the economic costs of arthritis, at nearly $3.5 billion per year.2 The average annual cost related to hip and knee OA per individual in Canada is $12,200, and the number of people with OA on disability is expected to double by 2020.3
There is a significant financial and public health focus in Canada on reducing wait times for total joint replacements, the most common surgical intervention for hip and knee OA.4 In conjunction with improving Canadians' access to surgery, other, more conservative efforts are needed to address downstream management of lower-extremity arthritis. Doing so should also improve pre-surgery functional status, possibly increasing the time span before surgery is required or even reducing the need for surgery. Physical therapists are vital members of the health care team needed to address the risk factors associated with declining health that is related to OA. The spiral of pain, decreased mobility, strength, and balance that is associated with hip and knee OA, combined with fear and anxiety, can result in loss of independence and can diminish the ability to engage in effective self-management strategies for arthritis such as physical activity.
Further, the presence of OA, although associated with increased bone mineral density in the area of OA, is not necessarily protective of fragile hip fractures.5–7 The reason for this is not known, but may be related to an increased incidence of falling in older adults with lower extremity OA, which exposes them to greater risk of fracture. In a review of 16 fall-risk studies,8 one of the priority risks identified was the presence of any type of arthritis, which had a higher mean relative risk (RR) of predicting future falls than either age or cognitive status. Lower-limb weakness, slower gait, decreased mobility, and pain—all outcomes of hip OA—were also established fall-risk factors.8,9 People with hip or knee OA are at a higher risk of falls, and their future risk significantly increases if they have joint pain and a prior history of falling.10–12 Therefore, it would be prudent to identify older adults who have OA and are at a higher risk of falling and to encourage them to engage in appropriate treatment strategies.
The American Geriatrics Society/British Geriatrics Society recently updated guidelines for fall-risk identification and management for older adults by producing a clinical algorithm.13 The premise of the clinical algorithm is to describe the decision-making and intervention process for community-dwelling adults, aged 65 years and older, who present to a clinical setting or an acute care setting (e.g., emergency department). The initial screening questions focus on identifying key fall-risk factors; individuals who present with either two or more falls or an acute fall in the past 12 months, or who have difficulty with walking and balance, then undergo a multi-factorial assessment.
The algorithm was developed from the broad population of community-dwelling older adults. However, we do not know whether the detailed assessment in the algorithm captures the unique factors associated with certain higher-risk conditions, particularly OA. Understanding this issue would allow health professionals to more effectively apply the guidelines to the individual decision making that is part of clinical practice. In particular, since the presence of either hip or knee OA may increase fall risk, it would be important to review research evidence to identify whether any additional factors should be assessed once patients with OA present with a history of falls and/or experience difficulty with balance or walking.
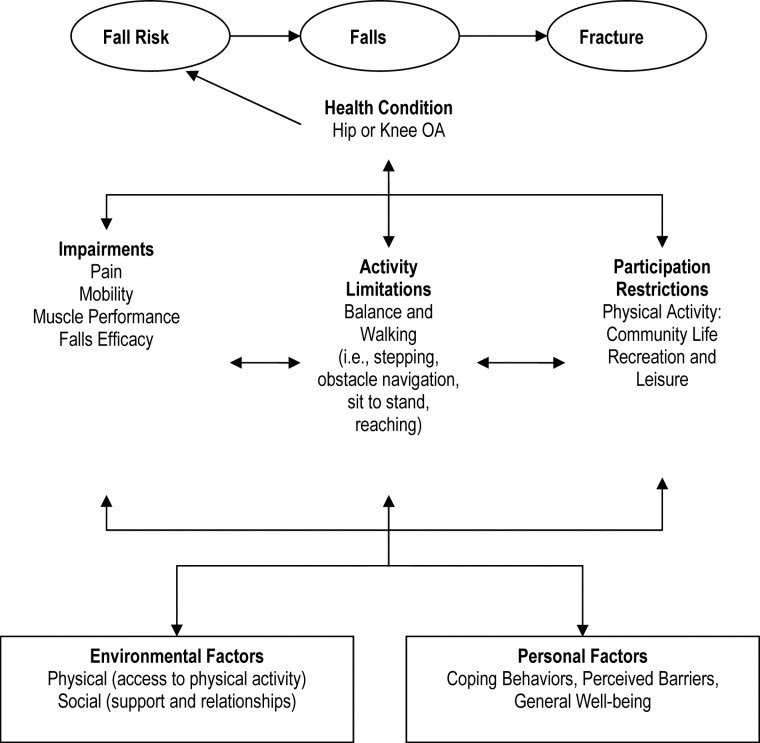
This literature review can be guided by the International Classification of Functioning, Disability, and Health (ICF)14 and could help physical therapists apply evidence-based screening algorithms to target populations (see Figure 1). The ICF provides a conceptual framework for describing health and health-related states, which would be helpful in providing a scientific basis for studying outcomes and determinants of health, such as hip or knee OA and fall risk in this population. The ICF defines two parts: (1) Functioning and Disability, which includes body functions and structures, activities, and participation in life situations; and (2) Contextual Factors, which includes the two domains of environmental and personal factors (see Figure 1).
Figure 1.
The impairments, activity limitations, participation restrictions, and contextual factors related to fall risk in older adults with hip or knee osteoarthritis.
Examples of impairments linked to fall risk are body functions, such as emotion, sleep, energy, pain, joint mobility, and muscle power; and structures associated with movement, cardiovascular, or neurological systems.15 The extent of a person's limitations or difficulties in executing tasks or activities, defined as activity limitations and participation restrictions, provides a performance qualifier by describing the person's actual performance within the societal context of his or her current environment or involvement in life situations. Examples of activity limitations are difficulties with mobility tasks, such as walking, reaching, carrying, or driving. Participation restrictions could include difficulty with mobility within the lived experience of being able to participate in physical activity, recreation, or employment. In the clinician's short list,15 activity limitations are defined as “capacity qualifiers,” whereby the clinician assesses the individual's capacity to execute the task with or without assistance, whereas participation restrictions are defined as “performance qualifiers,” which describe the performance of activities within the societal context of “the lived experience.” The contextual factors in the ICF that influence performance include the physical and social psychological environment in which one lives as well as other personal factors that are not part of the health condition but can play a role in disability at all levels, such as age, lifestyle habits, gender, and coping styles.
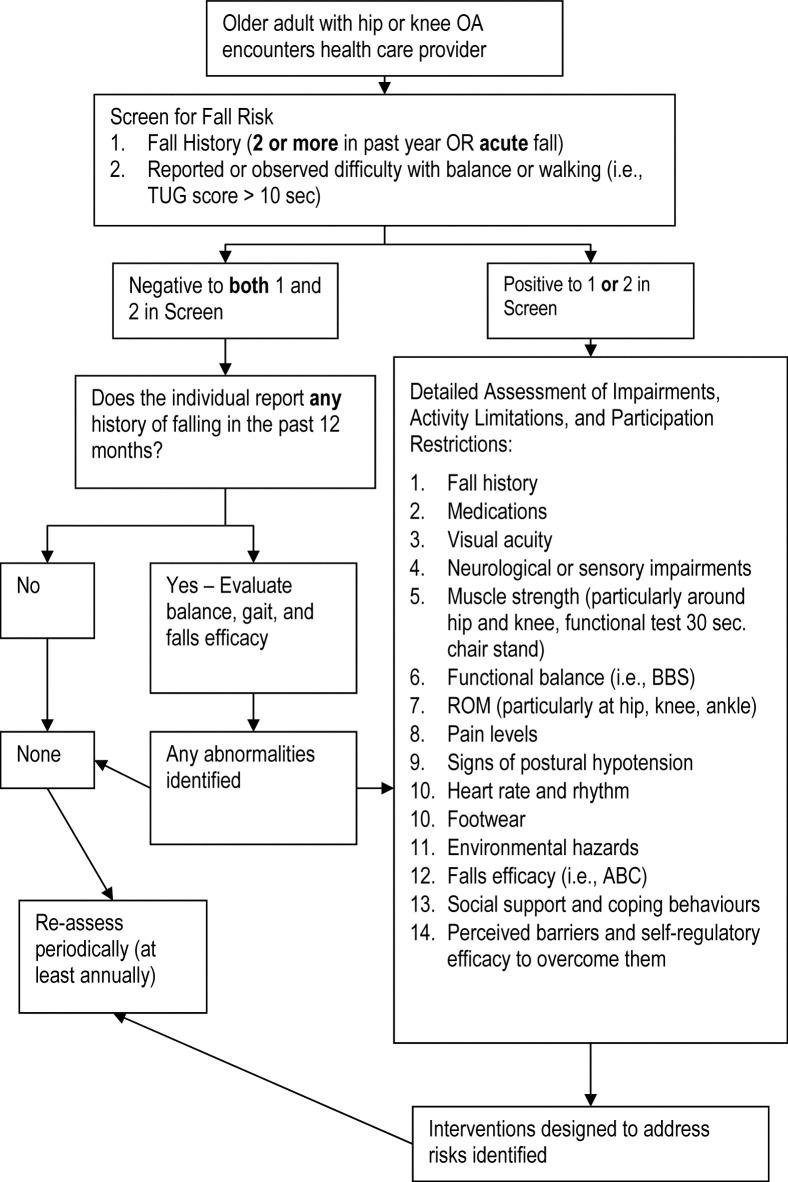
All parts and domains of the ICF classification may be negatively affected by hip or knee OA and may be affected by and/or lead to falls. Therefore, using the ICF classification as a guide in identifying multiple fall-risk factors among older adults with hip or knee OA may be helpful in determining whether additional factors will be needed in an adapted fall screening and assessment algorithm. The purpose of the present study was to identify factors contributing to increased fall risk among older adults with hip or knee OA and to integrate these factors into the most recent clinical guidelines and algorithm13 for fall-risk screening and assessment (see Figure 2). Adapting the algorithm may be advantageous to clinicians by providing a framework to direct future research and clinical practice in the area of hip and knee OA and fall risk.
Figure 2.
An algorithm for fall-risk screening and assessment of older adults with hip and knee osteoarthritis. Adapted from the Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. BBS: Berg Balance Scale; TUG: timed up-and-go Test; ABC: Activities-specific Balance Confidence.13
METHODS
A selective review of the literature was conducted by three researchers (the authors and a literature search assistant). Searches were performed in Medline, PubMed, and CINAHL using the following medical subject headings (MeSH) and keywords: osteoarthritis hip OR osteoarthritis knee AND any of: risk assessment, risk, risk factors AND any of: accidental falls, falls efficacy, falls self-efficacy, depression, social isolation, stability, postural control, gait, walking activity level, physical fitness, muscle strength, and activities of daily living. These keywords were used to capture the range of impairments, activity limitations, and participation restrictions that are associated with hip and knee OA and presumed to affect fall risk. We did not restrict our search to older adults only because it is not clear whether fall risk within certain higher risk populations may be higher throughout the adult and early older adult years (i.e., between 50 and 64 years) because of the nature of the health condition.
We focused our search on literature published within the years 2000–2010 to provide an overview of the most recently researched impairments, activity limitations, and participation restrictions involved in fall risk. Because of the limited number of articles published on this topic, however, some key studies before 2000 that related specifically to the association of falls and fracture to OA were also included. Our search retrieved a total of 122 titles, 101 of which were eliminated following a review of the abstracts because they were published in a language other than English, were not relevant to the topic, or were editors' views or commentary. A total of 21 articles fit the search criteria and were included in the review.6,7,9–12,16–30 Although all 21 studies included adults with OA or joint pain (including hip and knee), only 14 were specific to either hip or knee OA.10,11,12,16,19,20–23,25–29 We found few studies that addressed the relationship between personal and environmental contextual factors and fall risk specific to this population; we therefore added other studies known to us in order to supplement the relevant information related to fracture risk, older adults, falls, fall risk, and arthritis defined in more general terms. In particular, literature on physical activity, including key reviews and recent research, was selectively reviewed to illustrate potential application to assessment and intervention. Physical activity was a focus because, according to the ICF, it can be a participation restriction but can also be a recommended strategy to prevent falls for those at risk.
RESULTS AND DISCUSSION
The results and discussion are organized below under four main sections. The first section provides an overview of the literature that describes the association of OA to falls and fracture risk. The second section reviews our selected literature that fit under the ICF fall-risk headings (see Figure 1). This selected literature review was then used to inform the adaptation of the current clinical practice algorithm to an older adult population with hip or knee OA, which is described in the third section. Recommendations for screening, intervention, and future research for the older adult population with hip or knee OA conclude the paper (the fourth section).
Fall and fracture risk
Controversy exists in the literature as to whether the presence of OA increases, decreases, or has no effect on fall and fracture risk. Historically, the presence of OA has been assumed to increase bone density in the affected area as a result of increased proliferation of subchondral bone growth. The presence of OA would thus be expected to decrease the risk of fracture at the site. However, it is not clear whether or not an increase in bone density results in a stronger bone that is less likely to fracture.
Two studies support the idea that the presence of OA is not protective against fragility fracture (defined as a fracture caused by injury that would be insufficient to fracture a normal bone, such as a fall from standing height or less) despite higher bone density.6–7,31 However, Vestergaard and colleagues32 found, in a case control study of 124,655 fracture cases, that the presence of OA at any joint was associated with a decreased risk of fracture. OA at the hip or knee was associated with a declining risk from the time of diagnosis. It is possible that this result may be partially due to the correlation between declining physical activity levels and an increasing severity of lower extremity OA, meaning less exposure to fall-related fracture risk. Functional status, fall risk, and physical activity levels were not measured in this study. The rationale for, or mechanism of, declining fracture risk is not entirely clear, and the findings contradict those of a previous study5 that reported an increased risk specific to joint location in the lower extremity. Arden and colleagues5 found a twofold increase in non-traumatic fracture risk for hip OA relative to controls, but did not find a similar increase at other OA joint sites (e.g., knee, spine, and wrist). One explanation may be that individuals with hip OA have a greater incidence or risk of falls and thus a higher fracture risk, regardless of bone density values. One study found an increased occurrence of falls in women who presented to their physician with hip pain, relative to matched case controls.16 A second study found a threefold increase in fall risk, as measured by the Physiologic Profile Assessment (PPA), in women who scored higher in function and pain disability (scored ≥50 on the Western Ontario and McMaster Universities Osteoarthritis Index [WOMAC]) related to their OA.24
Not all studies produced evidence of site-specific arthritis-related fall risk. The presence of any arthritis or joint pain was shown to be a risk factor for falls.9,17,30 Relative risk ratios are moderate with the presence of arthritis at any joint (RR=2.4, 95% CI, 1.9–2.9),8 signs of hip OA (RR=1.7, 95% CI, 0.99–3.0),33 and history of arthritis or presence of hip or knee pain on passive range of motion (RR=1.9, 95% CI, 1.3–3.7).30 It makes sense that the presence of arthritis in the lower limbs would have the greatest impact on fall risk, since lower limb weakness, balance reactions (primarily controlled by trunk and lower extremity neuromuscular control), and functional ability (e.g., gait, ability to rise from a chair) show direct associations with fall risk.8,18 In a study of 1,821 men and women (mean age 69 years), Jones and colleagues7 found significantly increased postural sway and quadriceps weakness for those with self-reported arthritis (location not defined). Sturnieks and colleagues19 found increased fall risk in older adults with lower extremity arthritis (hips, knees, ankles, or feet) relative to a sample of healthy older adults. Arden and colleagues5 studied 1,353 women aged 45–64 years with radiographic diagnosis of hip OA and found a significantly greater association with self-reported non-traumatic fracture relative to other OA sites (knees, spine, and hands); these women were also 2.4 times more likely than controls to have had a non-traumatic fracture in the past 10 years. In another study, Arden and colleagues6 found a significant decrease in fall risk for women with more severe radiographic changes resulting from hip OA (RR=0.7, 95% CI, 0.5–1.0) but an increased risk for those with self-reported hip OA (RR=1.4, 95% CI, 1.2–1.5). As Vestergaard and colleagues32 have proposed, such findings may suggest that those with more severe disease and thus more limited functional ability put themselves at less risk than those with milder OA. Vestergaard and colleagues conclude that although hip OA patients had higher bone density values, a reduced risk of falls or fracture was not evident.
In summary, limited evidence exists of a causal link between hip and/or knee OA and future risk of falling and fractures, and it is not known whether the presence of both hip and knee OA further raises the risk. However, the bulk of evidence supports the notion that hip/knee OA is not protective against fractures, and may be more likely to increase the risk of fragility fracture through increased risk of falling, particularly in the case of hip OA. Given the findings of Vestergaard and colleagues' large case-control study,32 further study is needed to determine how joint OA affects the density, area, and strength of adjoining bones and the association of these factors with fracture risk. Exploring the fall-risk factors that are also common impairments, activity limitations, and participation restrictions associated with hip or knee OA is an important second consideration, given the limited evidence of a direct causal link.
Impairments, activity limitations, and participation restrictions linked to fall risk
Impairments secondary to hip or knee OA, such as pain (associated with sensory function), muscle weakness, decreased mobility, and reduced falls efficacy, have direct effects on primary fall-risk factors (i.e., activity limitations) including balance, walking, and the ability to perform daily tasks safely.8,9,13,25 These impairments also restrict participation in societal functioning—recreation and leisure, physical activity, and community life—which compounds the disability of people with hip or knee OA and may further increase their fall risk.17 The complex association of impairments, activity limitations, and participation restrictions in relation to fall risk is reviewed below.
Relationship of muscle performance, mobility, and pain to balance and walking
When walking, an individual must bear 81% of his or her body weight on a single limb for 60% of the gait cycle, which equates to a loading force through the hip greater than four times the body weight.34 This force is counter-balanced by the hip abductor muscles. Adequately conditioned muscles and the ability to generate force quickly can attenuate impact loads.35 In comparison, muscle waste and loss of static and dynamic strength can greatly increase compressive forces on the hip. People with muscle weakness and/or hip or knee pain will often compensate by limping during gait and shifting the centre of body mass over the support limb to increase the efficiency of the abductor muscles, primarily the gluteus medius.34 This compensation results in an abnormal gait with the centre of gravity displaced toward the side of the painful hip or knee. Balance may then be jeopardized, and the risk of falling increased, particularly if abnormal gait is combined with environmental obstacles, poor visual cues, and/or decreased proprioception. In addition, buckling of the lower limb due to muscle weakness and pain can compound the risk of falling.9 This sequence of events is even further compounded by age-related changes in gait: slower speed, decreased stride length, increased double support, decreased plantar flexion propulsion, and decreased hip extension.35 Indeed, over 75% of falls reported in one study of people with hip OA were associated with a walking or stepping activity.10
Static and dynamic strength deficits of up to 60% in the lower extremity muscles have been observed in people with OA.36 Neuromuscular inhibition of the quadriceps is the most common muscle weakness associated with knee OA, but few studies have identified specific weakness deficits for hip OA. Quadriceps weakness has been associated with increased fall risk8 and is more prevalent in lower extremity arthritis.9 A recent study37 found that both concentric and eccentric quadriceps muscle strength was independently associated with functional performance and fall risk in a healthy older adult population. Muscle power may also be an important aspect of neuromuscular control related to fall risk, but has received little attention in the literature on either healthy older adults or older adults with arthritis.
Loss of hip extension and hip abduction strength may be the most important contributor to gait changes and, thus, to changes in postural control during dynamic activity. Hip abductor and extensor weakness reduces the ability to stabilize the limb and shifts the weight forward in the stance phase, resulting in slower gait and a more flexed posture. Loss of hip extension range and strength may be a biomechanical contributor to fall risk.26,27 Biomechanical studies also suggest that the ability to prevent a fall in the event of tripping depends on where the centre of gravity is located at the time of the trip. An anterior shift of the centre of gravity because of flexed posturing or loss of hip extension is associated with falling when a trip occurs. Buckling of the limb, which can occur as a result of pain or muscle weakness, is also associated with a greater risk of falling.28,29
In summary, the consequences of hip OA—pain, loss of mobility, impaired balance, and loss of strength—combined with deterioration in neuromuscular function associated with aging, may increase the risk of falling. In particular, loss of hip extension range and weakness of the hip abductors and extensors may cause abnormal gait patterns that alter the ability to successfully shift the centre of gravity (as in normal walking) and decrease the ability to react to perturbations in weight-bearing positions.
At present, there is no consensus on the best screening test for gait and walking difficulties related to fall risk. The timed up-and-go (TUG)38 is one of the more common, functional walking tests used; there is debate in the literature as to the most sensitive cutoff point to predict future fall risk.10,20 In an analysis of older adults with hip OA, we found that a cutoff point of ≥10 seconds was associated with higher levels of functional decline and history of near falls but was not associated with a history of falls.10 The TUG could be a useful tool for identifying general activity limitations associated with fall risk. In addition, new clinical practice guidelines suggest that simply questioning an individual about difficulty in walking and balance may be adequate to screen for individuals who require a more detailed assessment.13
Relationship of pain and falls-efficacy to balance and walking
Fear of falling is more prevalent in older populations with joint pain,39,40 but whether this fear reflects a more general state of anxiety not specific to falls is unclear. More recently, researchers have evaluated fear of falls in the context of self-efficacy theory.41 Falls efficacy is defined as one's belief in one's skill and ability to successfully perform a task without falling.42 In this context, fear of falling is conceptualized as low levels of perceived self-efficacy or little confidence in one's ability to avoid falls,43 referred to in the literature as both “falls efficacy”43 and “balance confidence.”44 Higher levels of falls efficacy relates to higher confidence in the ability to prevent a fall and, thus, less fear about performing day-to-day tasks.
Fear of falling is relevant to falls for several reasons. First, it is an independent predisposing factor in both reduced physical status (e.g., muscle performance, mobility, balance, and physical activity involvement)45–47 and negative psychosocial effects (e.g., social isolation and depression).42,44,45 With decreased mobility and increased social isolation, fall-risk factors accumulate. The evidence is clear that increased fear of falling restricts both daily functional activity and recreational activity.46,47 The presence of back, joint, or muscle pain has been found to increase the likelihood of fear of falling reports two to four times, almost double in comparison to the findings from healthy, community-dwelling older adults.18,45,48 Jamison and colleagues48 reported that the presence of more intense pain was significantly associated with increased fear of falling in adults with arthritis. The relationship of chronic pain to fall risk is a complex interaction of factors including sleep disturbances, decreased attention, social withdrawal, medication use, functional limitations, gait changes, presence of other chronic conditions, and limitation of activity.17
Our previous studies found an independent association between lower levels of falls efficacy and poorer performance on balance tests in older adults with hip OA—controlling for age, physical activity level, and other functional status measures.21 We also found that an intervention program designed to enhance falls efficacy through education combined with an aquatic exercise program, improved both physical performance and falls efficacy in comparison to aquatic exercise alone and a control group with no excercise.22 In addition, older adults with hip OA and lower levels of falls efficacy responded better (i.e., with better physical performance and increases in falls efficacy) than those with higher levels of falls efficacy when education was combined with exercise.23 Taken together, these findings suggest that older adults with hip OA are at an increased risk of falls as a result of combinations of physical and psychological fall-risk factors, and that interventions designed to address both types of factors should result in the greatest reduction of fall risk.
The relationship of balance and walking limitations to increased risk of tripping/falls
Cecchi and colleagues11 found standing balance to be impaired in older adults with hip pain but not in those with knee pain, which may be due to older adults' relying more on the use of a hip strategy to balance as opposed to the ankle strategy more commonly observed in younger adults.49 Hip pain may result in reflex inhibition of the thigh and gluteal muscles. Hip pain has been associated with loss of hip extension, an anterior shift of the centre of gravity,27 and increased incidence of near falls.13 In fact, up to 30% of older adults with hip OA reported one or more near falls per week, while 45% had experienced one or more falls in the past year.10
Foley and colleagues24 found that self-reported functional ability and pain related to hip or knee OA were associated with reaction time, balance, proprioception, knee extension strength, and edge-contrast sensitivity. Other studies found balance impairment in older adults with hip or knee OA.10,25 Jadelis and colleagues50 also found obesity to be a contributing factor in greater balance impairment in those with knee pain. Presence of obesity is also linked to a reduced ability to perform functional activities, such as getting up and down from the floor and ascending and descending stairs.51
Obstacle clearance requires a fine balance of controlled kinematics of the trailing foot while maintaining body balance on the stance leg. Older adults with hip and knee OA may be at greater risk of falling when navigating obstacles because of the demanding requirements for both lower limbs. Pandya and colleagues52 reported a 37% lower obstacle avoidance success rate and a 54% reduction in single limb stance time in older adults with knee OA using virtual obstacles displayed at random intervals while participants walked down a 9.5 m walkway. There was a linear association between higher levels of self-reported pain and decreases in obstacle avoidance success and stance phase time, although it is unclear whether virtual obstacle navigation can be transferred to everyday experiences. Intra-articular injections, which decreased pain, improved success rates,53 but obstacle avoidance success still remained 20% lower than for healthy controls. It appears that other factors, such as muscle strength, joint motion, neuromuscular control, and proprioceptive changes associated with lower extremity OA, played a role beyond pain in increasing the risk of tripping in this population. Indeed, Chen and colleagues54 found that older adults with bilateral knee OA demonstrated different kinematics and kinetics when crossing an obstacle. In the OA group, greater hip-abduction moments were produced on the stance limb, likely to support the higher clearance observed for the swing or crossing limb relative to healthy controls, and an increased anterior pelvic tilt and greater knee-extensor moments were observed on the stance limb. It appears that both hip and knee strength are important for controlling the motion necessary to prevent a fall when stepping over an obstacle. The impact on fall risk of the use of walking aids, in combination with other fall-risk factors affecting walking and balance in hip and knee OA, is unknown.
Assessment of activity limitations should address the relationship of impairments to functional activities and balance. Assessment of postural control should incorporate both confidence and physical performance, since the two parameters are closely connected. The variety of functional balance and balance confidence measures that could be used to assess these risk factors are beyond the scope of this paper. In our experience, these tools, such as the Berg Balance Scale,55 consist of functional balance tasks that measure several of the common activities with which individuals with hip and knee OA may have difficulties—sit to stand, stepping, reaching, and turning. Falls efficacy tools such as the Activities-specific Balance Confidence (ABC) Scale44 can identify individuals with lower confidence levels. We found that lower levels of falls efficacy were associated with lower balance performance and that older adults with hip OA who had lower levels of falls efficacy (i.e., ABC scores <70) were more likely to benefit from interventions that incorporated more intensive strategies to educate and build on self-efficacy.22
Physical activity: Restrictions on participation, strategies to prevent falls and improve health
It is recommended that older adults engage in at least 150 minutes of moderate physical activity per week to manage their arthritis and obtain health benefits.56,57 Moderate activity is defined as activity that increases one's heart rate and breathing rate while still allowing one to talk but not sing.58 Unfortunately, up to 80% of adults with arthritis do not adhere to these recommendations.57,59,60 Low rates of adherence illustrate the restrictions on physical activity participation that exist among people with arthritis. Yet physical activity adherence among adults with various types of arthritis, including OA, has been shown to reduce pain, increase physical function, and improve falls efficacy. 61–64 Further, these community-deliverable activity programs deliver their beneficial effects regardless of individuals' age, the type of physical activity training, whether the physical activity is supervised or not, the length of the program, and the type of arthritis.64 Investigating processes important for regular participation in physical activity is therefore crucial for understanding how to improve poor adherence among all adults with arthritis.59,60
Ideally, such research should be theory driven in order, first, to identify reliable determinants of adherence and, second, to use theory as the guiding framework from which intervention strategies can be designed and implemented to positively affect determinants of adherence.64–66 Although not extensive, there is evidence from research reviews and studies that both environmental contextual and personal contextual factors (i.e., ICF factors; see Figure 1) are associated with physical activity adherence in people with arthritis.67–71 Environmental factors for which there is evidence of a positive relationship with adherence include increased social support (including physical activity advice from health care providers) and decreased work/family responsibilities. Personal contextual factors for which there is evidence of a positive association with adherence include lower pain, higher perceived well-being, no evidence of depression, fewer barriers, and increased self-regulatory efficacy (which revolves around confidence beliefs important for performing regular activity, such as scheduling/planning, coping with barriers, and goal setting). Despite these positive associations, and similar to behavioural medicine research,72 this research is largely atheoretical, which is problematic in the eventual design of effective interventions because strategies to change determinants are not known.
To address this issue, research based in social cognitive theory41,73 has been used to examine factors associated with physical activity adherence in adults with arthritis. Overall, findings have illustrated that physical activity adherence may be affected by activity-specific and disease-specific personal contextual factors. For example, adults reported both general barriers, common across symptomatic and asymptomatic populations (e.g., lack of motivation, lack of time), and arthritis-specific barriers (e.g., pain, joint stiffness). However, the extent to which barriers were perceived to limit activity had a stronger association with participation than the actual experience or frequency of barriers.67 Further, self-regulatory efficacy in using strategies to cope with barriers (i.e., an activity-specific factor) appears to mitigate the impact of limiting barriers and is associated with more physical activity. For example, two people may frequently experience a lack of time as a barrier to being active, but one who is confident in using strategies to successfully cope with that barrier (e.g., through scheduling activities, having plans to be active with friends) will report that it does not limit activity, while a less efficacious individual would report lack of time as being very limiting to activity.
Recent research has illustrated that pain acceptance, a disease-specific factor, may also be important for adherence to physical activity. Pain acceptance involves a willingness to experience pain without attempting to control it, and an engagement in valued life activities, such as physical activity.74,75 Gyurcsik and colleagues76 found that women with arthritis who reported more pain acceptance also had higher self-regulatory efficacy beliefs to cope with arthritis-specific barriers, expected more positive arthritis-related outcomes from activity (e.g., less pain, soreness, and stiffness), had lower pain intensity, and engaged in more physical activity than their counterparts with lower pain acceptance.
The relationship of personal and environmental contextual factors to engagement in physical activity
Theory-based investigations have begun to identify relationships between disease-specific personal contextual factors (e.g., pain acceptance and intensity) and activity-specific personal contextual factors important for physical activity adherence (e.g., barrier limitation, self-regulatory efficacy). Understanding the potentially complex interplay between such factors is a necessary step toward improving adherence to physical activity as a strategy for better disease management, including falls prevention.77,78 People with arthritis who attempt to adhere to activity must interpret their disease symptoms and outcomes and must also have the necessary activity-specific personal factors important for adherence in all populations (e.g., the self-regulatory efficacy to identify and use effective strategies to cope with limiting barriers). To date, very little research has examined this potential interplay of factors.
Future physical-activity research among individuals with arthritis should be driven by the use of compatible theories that, taken together, address activity-specific and disease-specific personal and environmental contextual factors. For example, social cognitive theory, which focuses on activity-specific factors as well as environmental factors,41,73 and the common sense model, which focuses on people's perceptions and beliefs about their chronic disease (e.g., timeline and consequences of the disease),79,80 may be used in a complementary fashion to study determinants of adherence among individuals with arthritis. Understanding how individuals with arthritis who adhere to physical activity at the recommended dose differ in their contextual factors from those who struggle with adherence may also be a fruitful avenue to investigate. Learning the contextual profile of people who adhere to physical activity in the context of their chronic disease could provide avenues for intervention among those who are less adherent so as to improve their disease management and health outcomes, including improvements in fall-risk factors such as pain, muscle weakness, and balance as well as reductions in fall incidence.81,82
Linking risk factors to clinical practice guidelines for falls screening and assessment: An adapted algorithm
Using the ICF, we have integrated knowledge of fall risk in older adults with knee or hip OA into an algorithm for the purposes of screening and assessment as well as to guide future research in this area (see Figure 2). This algorithm is based on the newly revised clinical practice guidelines for fall prevention in community-dwelling older adults.13 Our literature review suggests that a slightly modified algorithm is required to consider the unique presentation of impairments, activity limitations, and participation restrictions associated with hip or knee OA. The adapted algorithm is not meant to replace the evidence-based guidelines established by the American Geriatric Society and British Geriatric Society panel, but is meant to supplement other factors, which have less evidence in the literature, that may be important to explore in future research and use of the algorithm. For example, pain assessment, specific tests for joint range of motion, falls efficacy, and social aspects of coping behaviour (factors specific to older adults with chronic pain conditions such as OA) are included in this adapted algorithm, but not in the published guidelines. These adaptations (see Figure 2) are not meant to be exhaustive, but are based on the selected review outlined above.
Recommendations for falls screening and assessment for hip and knee OA
The presence of walking and balance difficulties should be a first-line screen for older adults with hip or knee OA. Standard functional mobility measures such as the TUG can assist in identifying higher risk individuals. As recommended by the American Geriatric Society and British Geriatric Societys guidelines, in instances where the initial screening is positive for a recent fall or a history of two or more falls in the past year and/or difficulty with balance or walking, then a detailed assessment of impairments, activity limitations, and participation restrictions should occur. If the screen is negative, but the individual reports any history of a fall in the past year, further evaluation of balance, gait, and falls efficacy is recommended. If no signs of fall risk exist at the time of screening, periodic re-evaluation should occur at least annually.
In contrast, if the initial screen is positive, the algorithm includes recommendations for a more detailed assessment (see Figure 2). Specifically for older adults with hip and knee OA this assessment should address the following issues:
Pain contributes to increased reporting of functional loss and decreased neuromuscular control of large muscles contributing to postural stability; the emotional stress of pain also leads to decreased ability to engage in both social and physical activity. Assessing pain levels and the impact of pain on daily living is important to establish a baseline. Interventions should address pain management, including a focus on actively coping with pain and on pain acceptance.
Detailed clinical assessment of lower extremity strength, range of motion, and balance is important. In particular, the therapist should pay close attention to loss of range and strength in hip extension and loss of strength in hip abduction and knee extension. Standard measures of balance, such as the Berg Balance Scale, can identify functional balance limitations. Physical activity interventions should focus on both improving strength of key muscle groups (hip abductors, extensors, knee extensors) and challenging balance.
Because of the increased risk of tripping in this population, as well as difficulty with activities such as ascending and descending stairs, stepping ability may be another important functional task to evaluate. Interventions should address practice of navigating obstacles, strengthening of hip flexors, ankle dorsiflexion range and strength to clear the toe, and climbing stairs.
In addition to physical screening tests, falls efficacy appears to be an important factor to consider for fall-risk screening in this population. Easy to administer questionnaires such as the ABC Scale could be useful in identifying those individuals with lower falls efficacy who may benefit more from interventions incorporating self-efficacy enhancement and education on fall risk. Understanding the underlying mechanisms of lower falls efficacy would add further insight into how to prevent falls efficacy from spiralling into a collective impact of social isolation and decreased physical activity, which further leads to an increase in risk of falls. Interventions should integrate the physical practice of daily living tasks and/or physical activity sessions along with building confidence in movement during these tasks. Confidence building should be theory-driven, addressing the individual's ability to self-regulate and overcome barriers to physical activity.
Detailed history taking and assessment of social, personal, and environmental contextual factors (e.g., environmental hazards, social support, barriers to physical activity and self-regulatory efficacy to cope with barriers) are important to identify the need for other professional referrals and changes to such factors.
Screening, assessment, and treatment planning should be theory-based, when possible. For example, using complementary theories related to physical activity adherence that contain activity-specific and disease-specific factors would be advantageous for identifying the range of factors contributing to adherence, potentially reducing fall risk and incidence.
Future research recommendations
Identify the key fall-risk factors in older adults with hip or knee OA to design effective screening and intervention strategies.
Determine pre-operative and post-operative fall-risk status for individuals undergoing total hip and knee arthroplasty, including long-term follow-up for at least one year.
Examine the impact of hip and knee OA on gait biomechanics related to falling and determine the impact of use of walking aids on fall risk in this population.
Evaluate the relationships of psychosocial and physical fall-risk factors and how these complex interactions influence ability to engage in physical activity.
Identify theory-based personal and environmental activity- and disease-specific contextual factors that influence physical activity adherence and the ability to engage in fall prevention strategies.
Determine whether the screening algorithm proposed applies to all older adults (i.e., aged 50 years and over).
Limitations
We recognize that the lack of a systematic literature review and of a selection process based on internal validity ratings is a limitation of our study. However, the lack of research specific to this population warrants the development of an adapted algorithm that can guide future research, leading to a systematic review with effect sizes.
CONCLUSION
Research evidence illustrates that older adults with hip or knee OA have an increased risk of falling, which may increase their fracture risk. Based on the literature reviewed above, we recommend that health professionals regularly screen their clients with hip and knee OA for fall risk, which will identify a broad range of impairments, activity limitations, and participation restrictions, as well as personal and environmental contextual factors associated with fall risk, in order to best prescribe appropriate interventions. Further research related to fall rates and risk as well as the inter-relationship of risk factors is needed in this population.
KEY MESSAGES
What is already known on this topic
Older adults with hip and knee OA have a collection of impairments, activity limitations, and participation restrictions that put them at a higher risk of falls. The presence of OA at a joint does not appear to have a protective effect against fracture; in fact, this population may be at an even higher risk of fall and fracture than the healthy community-dwelling older adult population. Identifying the risk factors and incorporating a theoretical framework based on research to screen, assess, and provide effective intervention for higher-risk populations is important to direct health care initiatives and future research.
What this study adds
This selected review of literature and proposal of an integrated framework for screening and assessing older adults with hip and knee OA for fall risk can assist in developing more effective strategies for prevention and treatment of fall risk. The model proposed here, which applies the ICF framework and established fall-risk assessment guidelines to a high-risk target population, can be used with other high-risk populations. A theoretical model is also helpful in generating future research on this topic.
Physiotherapy Canada 2012; 64(3);302–314; doi:10.3138/ptc.2011-12BH
References
- 1.Arthritis Society of Canada. Osteoarthritis [Internet] [cited 2011 Jan 23]. Available from: http://www.arthritis.ca/types%20of%20arthritis/default.asp?s=1&province=ca.
- 2.Canadian Institute of Health Research. Arthritis [internet] [Cited 2011 January 25]. Available from: http://www.cihr-irsc.gc.ca/e/11196.html.
- 3.Gupta S, Hawker GA, Laporte A, et al. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology (Oxford) 2005;44(12):1531–7. doi: 10.1093/rheumatology/kei049. http://dx.doi.org/10.1093/rheumatology/kei049. Medline:16091394. [DOI] [PubMed] [Google Scholar]
- 4.Health Canada. Wait times in Canada [Internet] [cited 2011 Jan 25]. Available from: http://www.hc-sc.gc.ca/hcs-sss/qual/acces/wait-attente/index-eng.php.
- 5.Arden NK, Griffiths GO, Hart DJ, et al. The association between osteoarthritis and osteoporotic fracture: the Chingford Study. Br J Rheumatol. 1996;35(12):1299–304. doi: 10.1093/rheumatology/35.12.1299. http://dx.doi.org/10.1093/rheumatology/35.12.1299. Medline:9010060. [DOI] [PubMed] [Google Scholar]
- 6.Arden NK, Nevitt MC, Lane NE, et al. Study of Osteoporotic Fractures Research Group. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Arthritis Rheum. 1999;42(7):1378–85. doi: 10.1002/1529-0131(199907)42:7<1378::AID-ANR11>3.0.CO;2-I. http://dx.doi.org/10.1002/1529-0131(199907)42:7<1378::AID-ANR11>3.0.CO;2-I. Medline:10403265. [DOI] [PubMed] [Google Scholar]
- 7.Jones G, Nguyen T, Sambrook PN, et al. Osteoarthritis, bone density, postural stability, and osteoporotic fractures: a population based study. J Rheumatol. 1995;22(5):921–5. Medline:8587083. [PubMed] [Google Scholar]
- 8.American Geriatrics Society; British Geriatrics Society; American Academy of Orthopedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–72. http://dx.doi.org/10.1046/j.1532-5415.2001.49115.x. Medline:11380764. [PubMed] [Google Scholar]
- 9.Leveille SG, Bean J, Bandeen-Roche K, et al. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50(4):671–8. doi: 10.1046/j.1532-5415.2002.50161.x. http://dx.doi.org/10.1046/j.1532-5415.2002.50161.x. Medline:11982667. [DOI] [PubMed] [Google Scholar]
- 10.Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;7(17) doi: 10.1186/1471-2318-7-17. Available from: http://www.biomedcentral.com/1471-2318/7/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cecchi F, Molino-Lova R, Di Iorio A, et al. Measures of physical performance capture the excess disability associated with hip pain or knee pain in older persons. J Gerontol A Biol Sci Med Sci. 2009;64(12):1316–24. doi: 10.1093/gerona/glp125. http://dx.doi.org/10.1093/gerona/glp125. Medline:19797345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swinkels A, Newman JH, Allain TJ. A prospective observational study of falling before and after knee replacement surgery. Age Ageing. 2009;38(2):175–81. doi: 10.1093/ageing/afn229. http://dx.doi.org/10.1093/ageing/afn229. Medline:19029071. [DOI] [PubMed] [Google Scholar]
- 13.Panel on Prevention of Falls in Older Persons; American Geriatrics Society; British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148, 57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization [Internet] Geneva: International Classification of Functioning, Disability and Health; 2007. [cited 2011 Jan 25]. Available from: http://www.who.int/classifications/icf/en/ [Google Scholar]
- 15.World Health Organization. ICF Checklist [Internet] Geneva: The Organization; 2003. [cited 2011 Jan 26]. Available from: http://www.who.int/classifications/icf/training/icfchecklist.pdf. [Google Scholar]
- 16.Nahit ES, Silman AJ, Macfarlane GJ. The occurrence of falls among patients with a new episode of hip pain. Ann Rheum Dis. 1998;57(3):166–8. doi: 10.1136/ard.57.3.166. http://dx.doi.org/10.1136/ard.57.3.166. Medline:9640133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Varela-Burstein E, Miller PA. Is chronic pain a risk factor for falls among community dwelling elders? Top Geriatr Rehabil. 2003;19(2):145–59. [Google Scholar]
- 18.Studenski S, Duncan PW, Chandler J, et al. Predicting falls: the role of mobility and nonphysical factors. J Am Geriatr Soc. 1994;42(3):297–302. doi: 10.1111/j.1532-5415.1994.tb01755.x. Medline:8120315. [DOI] [PubMed] [Google Scholar]
- 19.Sturnieks DL, Tiedemann A, Chapman K, et al. Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol. 2004;31(11):2272–9. Medline:15517643. [PubMed] [Google Scholar]
- 20.Kristensen MT, Foss NB, Kehlet H. Timed “up & go” test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther. 2007;87(1):24–30. doi: 10.2522/ptj.20050271. http://dx.doi.org/10.2522/ptj.20050271. Medline:17142643. [DOI] [PubMed] [Google Scholar]
- 21.Arnold CM, Faulkner RA. Does falls-efficacy predict balance performance in older adults with hip osteoarthritis? J Gerontol Nurs. 2009;35(1):45–52. doi: 10.3928/00989134-20090101-01. http://dx.doi.org/10.3928/00989134-20090101-01. Medline:19227102. [DOI] [PubMed] [Google Scholar]
- 22.Arnold CM, Faulkner RA. The effect of aquatic exercise and education on lowering fall risk in older adults with hip osteoarthritis. J Aging Phys Act. 2010;18(3):245–60. doi: 10.1123/japa.18.3.245. Medline:20651413. [DOI] [PubMed] [Google Scholar]
- 23.Arnold CM, Faulkner R, Gyurcsik NC. The relationship of falls-efficacy to improvement in fall risk factors following an exercise plus educational intervention for older adults with hip osteoarthritis. Physiother Can. 2011;63(4):410–20. doi: 10.3138/ptc.2010-29. http://dx.doi.org/10.3138/ptc.2010-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foley SJ, Lord SR, Srikanth V, et al. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthritis Cartilage. 2006;14(6):533–9. doi: 10.1016/j.joca.2005.12.007. http://dx.doi.org/10.1016/j.joca.2005.12.007. Medline:16460970. [DOI] [PubMed] [Google Scholar]
- 25.Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther. 1997;25(1):13–8. doi: 10.2519/jospt.1997.25.1.13. Medline:8979171. [DOI] [PubMed] [Google Scholar]
- 26.Chang SJ, Mercer VS. Relationship between hip abductor rate of force development and medial-lateral stability in older adults. J Geriatr Phys Ther. 2003;26(3):47–8. [Google Scholar]
- 27.Kerrigan DC, Lee LW, Collins JJ, et al. Reduced hip extension during walking: healthy elderly and fallers versus young adults. Arch Phys Med Rehabil. 2001;82(1):26–30. doi: 10.1053/apmr.2001.18584. http://dx.doi.org/10.1053/apmr.2001.18584. Medline:11239282. [DOI] [PubMed] [Google Scholar]
- 28.Pavol MJ, Owings TM, Foley KT, et al. Mechanisms leading to a fall from an induced trip in healthy older adults. J Gerontol A Biol Sci Med Sci. 2001;56(7):M428–37. doi: 10.1093/gerona/56.7.m428. http://dx.doi.org/10.1093/gerona/56.7.M428. Medline:11445602. [DOI] [PubMed] [Google Scholar]
- 29.Pavol MJ, Owings TM, Foley KT, et al. Influence of lower extremity strength of healthy older adults on the outcome of an induced trip. J Am Geriatr Soc. 2002;50(2):256–62. doi: 10.1046/j.1532-5415.2002.50056.x. http://dx.doi.org/10.1046/j.1532-5415.2002.50056.x. Medline:12028206. [DOI] [PubMed] [Google Scholar]
- 30.Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261(18):2663–8. http://dx.doi.org/10.1001/jama.1989.03420180087036. Medline:2709546. [PubMed] [Google Scholar]
- 31.World Health Organization. Guidelines for preclinical evaluation and clinical trials in osteoporosis [Internet] Geneva: The Organization; 1998. [cited 2011 Jan 26]. Available from: http://whqlibdoc.who.int/publications/1998/9241545224_eng.pdf. [Google Scholar]
- 32.Vestergaard P, Rejnmark L, Mosekilde L. Osteoarthritis and risk of fractures. Calcif Tissue Int. 2009;84(4):249–56. doi: 10.1007/s00223-009-9224-z. http://dx.doi.org/10.1007/s00223-009-9224-z. Medline:19234808. [DOI] [PubMed] [Google Scholar]
- 33.Campbell AJ, Borrie MJ, Spears GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. 1989;44(4):M112–7. doi: 10.1093/geronj/44.4.m112. Medline:2738307. [DOI] [PubMed] [Google Scholar]
- 34.Maquet P. Biomechanics of the hip. Berlin: Springer-Verlag; 1985. [Google Scholar]
- 35.Brandt K, Doherty M, Lohmander L. Osteoarthritis. 2nd ed. New York: Oxford University Press; 2003. [Google Scholar]
- 36.Barak Y, Wagenaar RC, Holt KG. Gait characteristics of elderly people with a history of falls: a dynamic approach. Phys Ther. 2006;86(11):1501–10. doi: 10.2522/ptj.20050387. http://dx.doi.org/10.2522/ptj.20050387. Medline:17079750. [DOI] [PubMed] [Google Scholar]
- 37.Crockett K, Schmyr A, Hermanson M, et al. Association of muscle power and strength to the kinematics and performance of sit to stand. Forthcoming.
- 38.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. Medline:1991946. [DOI] [PubMed] [Google Scholar]
- 39.Evitt CP, Quigley PA. Fear of falling in older adults: a guide to its prevalence, risk factors, and consequences. Rehabil Nurs. 2004;29(6):207–10. Medline:15597999. [PubMed] [Google Scholar]
- 40.Murphy SL, Dubin JA, Gill TM. The development of fear of falling among community-living older women: predisposing factors and subsequent fall events. J Gerontol A Biol Sci Med Sci. 2003;58(10):M943–7. doi: 10.1093/gerona/58.10.m943. http://dx.doi.org/10.1093/gerona/58.10.M943. Medline:14570863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bandura A. Self-efficacy: the exercise of control. New York: Freeman and Company; 1997. [Google Scholar]
- 42.Marks R. Efficacy theory and its utility in arthritis rehabilitation: review and recommendations. Disabil Rehabil. 2001;23(7):271–80. doi: 10.1080/09638280010004162. http://dx.doi.org/10.1080/09638280010004162. Medline:11354579. [DOI] [PubMed] [Google Scholar]
- 43.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):239–43. doi: 10.1093/geronj/45.6.p239. Medline:2229948. [DOI] [PubMed] [Google Scholar]
- 44.Myers AM, Powell LE, Maki BE, et al. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51(1):M37–43. doi: 10.1093/gerona/51a.1.m37. http://dx.doi.org/10.1093/gerona/51A.1.M37. Medline:8548512. [DOI] [PubMed] [Google Scholar]
- 45.Kressig RW, Wolf SL, Sattin RW, et al. Associations of demographic, functional, and behavioral characteristics with activity-related fear of falling among older adults transitioning to frailty. J Am Geriatr Soc. 2001;49(11):1456–62. doi: 10.1046/j.1532-5415.2001.4911237.x. http://dx.doi.org/10.1046/j.1532-5415.2001.4911237.x. Medline:11890583. [DOI] [PubMed] [Google Scholar]
- 46.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33(3):273–9. doi: 10.1093/ageing/afh077. http://dx.doi.org/10.1093/ageing/afh077. Medline:15082433. [DOI] [PubMed] [Google Scholar]
- 47.Bruce DG, Devine A, Prince RL. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50(1):84–9. doi: 10.1046/j.1532-5415.2002.50012.x. http://dx.doi.org/10.1046/j.1532-5415.2002.50012.x. Medline:12028251. [DOI] [PubMed] [Google Scholar]
- 48.Jamison M, Neuberger GB, Miller PA. Correlates of falls and fear of falling among adults with rheumatoid arthritis. Arthritis Rheum. 2003;49(5):673–80. doi: 10.1002/art.11383. http://dx.doi.org/10.1002/art.11383. Medline:14558053. [DOI] [PubMed] [Google Scholar]
- 49.Shumway-Cook A, Woollacott MH. Motor control: translating research into clinical practice. Philadelphia: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 50.Jadelis K, Miller ME, Ettinger WH, Jr, et al. Strength, balance, and the modifying effects of obesity and knee pain: results from the Observational Arthritis Study in Seniors (oasis) J Am Geriatr Soc. 2001;49(7):884–91. doi: 10.1046/j.1532-5415.2001.49178.x. http://dx.doi.org/10.1046/j.1532-5415.2001.49178.x. Medline:11527479. [DOI] [PubMed] [Google Scholar]
- 51.Topp R, Woolley S, Khuder S, et al. Predictors of four functional tasks in patients with osteoarthritis of the knee. Orthop Nurs. 2000;19(5):49–58. doi: 10.1097/00006416-200019050-00009. http://dx.doi.org/10.1097/00006416-200019050-00009. Medline:11153386. [DOI] [PubMed] [Google Scholar]
- 52.Pandya NK, Draganich LF, Mauer A, et al. Osteoarthritis of the knees increases the propensity to trip on an obstacle. Clin Orthop Relat Res. 2005;431:150–6. doi: 10.1097/01.blo.0000150316.97009.f2. http://dx.doi.org/10.1097/01.blo.0000150316.97009.f2. Medline:15685069. [DOI] [PubMed] [Google Scholar]
- 53.Pandya NK, Piotrowski GA, Pottenger L, et al. Pain relief in knee osteoarthritis reduces the propensity to trip on an obstacle. Gait Posture. 2007;25(1):106–11. doi: 10.1016/j.gaitpost.2006.02.001. http://dx.doi.org/10.1016/j.gaitpost.2006.02.001. Medline:16529934. [DOI] [PubMed] [Google Scholar]
- 54.Chen HL, Lu TW, Wang TM, et al. Biomechanical strategies for successful obstacle crossing with the trailing limb in older adults with medial compartment knee osteoarthritis. J Biomech. 2008;41(4):753–61. doi: 10.1016/j.jbiomech.2007.11.017. http://dx.doi.org/10.1016/j.jbiomech.2007.11.017. Medline:18177877. [DOI] [PubMed] [Google Scholar]
- 55.Berg K, Wood-Dauphinee S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304, 11. [Google Scholar]
- 56.Public Health Agency of Canada; Centre for Chronic Disease Prevention and Control, Chronic Disease Surveillance Division. Life with arthritis in Canada: a personal and public health challenge [Internet] [cited 2011 Feb 4]. [updated 2010]. Available from: http://www.phac-aspc.gc.ca/cd-mc/arthritis-arthrite/lwaic-vaaac-10/pdf/arthritis-2010-eng.pdf.
- 57.Canadian Society of Exercise Physiology. Canadian Physical Activity Guidelines [Internet] The Society; 2011. Jan, [cited 2011 Feb 10]. Available from: http://www.csep.ca/english/view.asp?x=804. [Google Scholar]
- 58.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–45. doi: 10.1249/mss.0b013e3180616aa2. http://dx.doi.org/10.1249/mss.0b013e3180616aa2. Medline:17762378. [DOI] [PubMed] [Google Scholar]
- 59.Marks R, Allegrante JP. Chronic osteoarthritis and adherence to exercise: a review of the literature. J Aging Phys Act. 2005;13(4):434–60. doi: 10.1123/japa.13.4.434. Medline:16301755. [DOI] [PubMed] [Google Scholar]
- 60.Pisters MF, Veenhof C, Schellevis FG, et al. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res (Hoboken) 2010;62(8):1087–94. doi: 10.1002/acr.20182. http://dx.doi.org/10.1002/acr.20182. Medline:20235201. [DOI] [PubMed] [Google Scholar]
- 61.Busch AJ, Schachter CL, Overend TJ, et al. Exercise for fibromyalgia: a systematic review. J Rheumatol. 2008;35(6):1130–44. Medline:18464301. [PubMed] [Google Scholar]
- 62.Conn VS, Hafdahl AR, Minor MA, et al. Physical activity interventions among adults with arthritis: meta-analysis of outcomes. Semin Arthritis Rheum. 2008;37(5):307–16. doi: 10.1016/j.semarthrit.2007.07.006. http://dx.doi.org/10.1016/j.semarthrit.2007.07.006. Medline:17888500. [DOI] [PubMed] [Google Scholar]
- 63.Hurkmans E, van der Giesen FJ, Vliet Vlieland TP, et al. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009;(4):CD006853. doi: 10.1002/14651858.CD006853.pub2. Medline:19821388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kelley GA, Kelley KS, Hootman JM, et al. Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res (Hoboken) 2011;63(1):79–93. doi: 10.1002/acr.20347. http://dx.doi.org/10.1002/acr.20347. Medline:20824798. [DOI] [PubMed] [Google Scholar]
- 65.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;15(4):266–97. doi: 10.1016/s0749-3797(98)00080-4. http://dx.doi.org/10.1016/S0749-3797(98)00080-4. Medline:9838973. [DOI] [PubMed] [Google Scholar]
- 66.Brawley LR. The practicality of using social psychological theories for exercise and health research and intervention. J Appl Sport Psychol. 1993;5(2):99–115. http://dx.doi.org/10.1080/10413209308411309. [Google Scholar]
- 67.Brittain DR, Gyurcsik NC, McElroy M, et al. General and arthritis-specific barriers to moderate physical activity in women with arthritis. Womens Health Issues. 2011;21(1):57–63. doi: 10.1016/j.whi.2010.07.010. http://dx.doi.org/10.1016/j.whi.2010.07.010. Medline:20833069. [DOI] [PubMed] [Google Scholar]
- 68.Der Ananian C, Wilcox S, Saunders R, et al. Factors that influence exercise among adults with arthritis in three activity levels. Prev Chron Dis. 2006;3:1–16. http://www.cdc.gov/pcd/issues/2006/jul/05_0220.htm. [PMC free article] [PubMed] [Google Scholar]
- 69.Eyler AA. Correlates of physical activity: who's active and who's not? Arthritis Rheum. 2003;49(1):136–40. doi: 10.1002/art.10910. http://dx.doi.org/10.1002/art.10910. Medline:12579605. [DOI] [PubMed] [Google Scholar]
- 70.Wilcox S, Der Ananian C, Abbott J, et al. Perceived exercise barriers, enablers, and benefits among exercising and nonexercising adults with arthritis: results from a qualitative study. Arthritis Rheum. 2006;55(4):616–27. doi: 10.1002/art.22098. http://dx.doi.org/10.1002/art.22098. Medline:16874785. [DOI] [PubMed] [Google Scholar]
- 71.Wilcox SA, Der Ananian C, Sharpe PA, et al. Correlates of physical activity in persons with arthritis: Review and recommendations. J Phys Act Health. 2005;2:230–52. [Google Scholar]
- 72.Painter JE, Borba CPC, Hynes M, et al. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35(3):358–62. doi: 10.1007/s12160-008-9042-y. http://dx.doi.org/10.1007/s12160-008-9042-y. Medline:18633685. [DOI] [PubMed] [Google Scholar]
- 73.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 74.McCracken LM, Vowles KE. Acceptance of chronic pain. Curr Pain Headache Rep. 2006;10(2):90–4. doi: 10.1007/s11916-006-0018-y. http://dx.doi.org/10.1007/s11916-006-0018-y. Medline:16539860. [DOI] [PubMed] [Google Scholar]
- 75.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107(1-2):159–66. doi: 10.1016/j.pain.2003.10.012. http://dx.doi.org/10.1016/j.pain.2003.10.012. Medline:14715402. [DOI] [PubMed] [Google Scholar]
- 76.Gyurcsik NC, Brawley LR, Spink KS, et al. Is level of pain acceptance differentially related to social cognitions and behavior? The case of active women with arthritis. J Health Psychol. 2011;16(3):530–9. doi: 10.1177/1359105310394229. http://dx.doi.org/10.1177/1359105310394229. Medline:21224336. [DOI] [PubMed] [Google Scholar]
- 77.Leventhal H, Brissette I, Leventhal E. The common-sense model of self-regulation of health and illness. In: Cameron L, Leventhal H, editors. The self-regulation of health and illness behaviour. New York, NY: Routledge; 2003. pp. 42–65. [Google Scholar]
- 78.Rejeski WJ, Brawley LR, Jung ME. Self-management of health behavior in geriatric medicine. In: Halter JB, Ouslander JG, Tinetti ME, et al., editors. Hazard's Geriatric Medicine and Gerontology. New York: McGraw Hill Medical; 2008. pp. 325–42. [Google Scholar]
- 79.Leventhal H, Mora PA. Is there a science of the processes underlying health and illness behaviors? A comment on Maes and Karoly. Appl Psychol-Int Rev. 2005;54:255–66. [Google Scholar]
- 80.Leventhal H, Weinman J, Leventhal EA, et al. Health psychology: the search for pathways between behavior and health. Annu Rev Psychol. 2008;59(1):477–505. doi: 10.1146/annurev.psych.59.103006.093643. http://dx.doi.org/10.1146/annurev.psych.59.103006.093643. Medline:17937604. [DOI] [PubMed] [Google Scholar]
- 81.Bryan AD, Magnan RE, Nilsson R, et al. The big picture of individual differences in physical activity behavior change: a transdisciplinary approach. Psychol Sport Exerc. 2011;12(1):20–6. doi: 10.1016/j.psychsport.2010.05.002. http://dx.doi.org/10.1016/j.psychsport.2010.05.002. Medline:21278837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64. doi: 10.1177/1090198104263660. http://dx.doi.org/10.1177/1090198104263660. Medline:15090118. [DOI] [PubMed] [Google Scholar]