Abstract
To determine CYP2C19 and CYP2C8 allele frequencies, 28 coding and/or functional variants were genotyped in 1250 African-American, Asian, Caucasian, Hispanic and Ashkenazi Jewish (AJ) individuals. The combined CYP2C19 variant allele frequencies ranged from ~0.30–0.41; however, the CYP2C8 frequencies were much lower (~0.04–0.13). After incorporating previously reported CYP2C9 genotyping results from these populations (36 total CYP2C variants), 16 multi-ethnic CYP2C haplotypes were inferred with frequencies >0.5%. Notably, the 2C19*17-2C9*1-2C8*2 haplotype was identified among African-Americans (8%) and Hispanics (2%), indicating that CYP2C19*17 does not always tag a CYP2C haplotype that encodes efficient CYP2C-substrate metabolism. The 2C19*1-2C9*2-2C8*3 haplotype was identified in all populations except African-Americans and additional novel haplotypes were identified in selected populations (e.g., 2C19*2-2C9*1-2C8*4, 2C19*4B-2C9*1-2C8*1), together indicating that both CYP2C19*17 and *2 can be linked with other CYP2C loss-of-function alleles. These results have important implications for pharmacogenomic association studies involving the CYP2C locus and are clinically relevant when administering CYP2C-substrate medications.
Keywords: CYP2C19, CYP2C8, CYP2C9, clinical pharmacogenetics, linkage disequilibrium, haplotype
INTRODUCTION
The hepatic cytochrome P450 (CYP450) superfamily of hemoproteins are the principal enzymes involved in human drug metabolism and bioactivation. Over 50 human CYP450 isozymes have been identified; however, members of the CYP2 and CYP3 families have significant importance as they contribute to the metabolism of the majority of drugs.1 The most relevant CYP2C subfamily enzymes are encoded by a cluster of polymorphic genes on chromosome 10q23.33, organized as Cen-CYP2C18-CYP2C19-CYP2C9-CYP2C8-Tel.2–4 Although the sequences of these four isoforms are greater than 80% identical, they can have distinct substrate specificities, and together are involved in the metabolism of ~20–30% of all medications.3
CYP2C19 contributes to the metabolism of a large number of clinically relevant drugs and drug classes such as antidepressants, benzodiazepines, mephenytoin, proton pump inhibitors, and the antiplatelet prodrug clopidogrel.5–7 CYP2C9 is involved in the metabolism of tolbutamide, phenytoin, S-warfarin, losartan, and numerous anti-inflammatory drugs such as ibuprofen.8–9 Some CYP2C9 substrates overlap with CYP2C8, including arachidonic acid, several non-steroidal anti-inflammatory drugs, and retinoic acid. CYP2C8 also plays a direct role in the metabolism of some important therapeutic drugs, including paclitaxel, amodiaquine, troglitazone, amiodarone, verapamil, cerivastatin, and fluvastatin.10 Although variant CYP2C18 alleles have been reported,11–12 CYP2C18 expression is not consistent with a major role in hepatic drug metabolism and specific CYP2C18-substrates have yet to be clearly identified.3 Both common and rare CYP2C19, CYP2C9, and CYP2C8 variant alleles have been identified in different populations, which are catalogued by the Human Cytochrome P450 (CYP) Allele Nomenclature Committee.13 Many of these variant alleles encode reduced or complete loss-of-function, and their frequencies can significantly differ between racial and ethnic populations.14–17 Importantly, the ~390 kb of sequence that encompasses the CYP2C cluster is in strong linkage disequilibrium (LD),18–19 indicating that there is a tendency to jointly inherit alleles that confer specific CYP2C19, CYP2C9, and CYP2C8 metabolic phenotypes. Previous studies interrogating selected CYP2C variants have identified LD between some CYP2C19, CYP2C9, and CYP2C8 alleles in specific ethnic subpopulations;20–24 however, the frequencies of many variant CYP2C alleles and relevant haplotypes remain unknown in most populations.
We previously reported the frequencies of important CYP2C9 alleles (*2, *3, *4, *5, *6, *8, *11, *13) in the African-American, Asian, Caucasian, Hispanic, and Ashkenazi Jewish (AJ) populations,16, 25 and recently identified the novel CYP2C19*4B allele in the AJ population that is defined by both gain-of-function [c.−806C>T (*17)] and loss-of-function [c.1A>G (*4)] alleles on the same haplotype.26 To determine the frequencies of additional CYP2C alleles in these populations, 28 variant CYP2C19 (*2 – *10, *12 – *17, *22) and CYP2C8 (*2 – *10, *12 – *14) alleles were genotyped in 250 DNA samples each from healthy African-American, Asian, Caucasian, Hispanic, and AJ individuals. These results were then combined with the previously reported CYP2C9 data to identify CYP2C haplotypes and their multi-ethnic frequencies. These results have important implications for pharmacogenetic association studies involving the CYP2C locus and are clinically relevant when administering CYP2C-substrate medications. In addition, given the recent interest in clinical CYP2C19 genetic testing for clopidogrel response,6, 27–31 we determined the ABCB1 c.3435C>T32–35 allele and genotype frequencies for all tested populations.
MATERIALS AND METHODS
Study Population
Peripheral blood samples from healthy donors who indicated their racial background and gave informed consent for the use of their DNA for research were obtained from the New York Blood Center with IRB approval as previously defined.16, 25 In addition, blood samples were obtained with informed consent from unrelated healthy 100% AJ individuals from the greater New York metropolitan area.26, 36–38 All personal identifiers were removed, and isolated DNA samples were tested anonymously. Genomic DNA was isolated using the Puregene® DNA Purification kit (Qiagen, Valencia, CA) according to the manufacturer's instructions. Two hundred and fifty samples were genotyped for each of the five tested populations (African-American, Asian, Caucasian, Hispanic, and AJ).
Genotyping
The designations of all CYP450 alleles refer to those defined by the Cytochrome P450 Allele Nomenclature Committee (http://www.cypalleles.ki.se/).13 Eleven variant CYP2C19 alleles (*2 – *10, *13, *17) were genotyped using the eSensor® 2C19 Test (GenMark Diagnostics, Carlsbad, CA) as per the manufacturer's instructions, and five additional variant CYP2C19 alleles (*12, *14 – *16, *22) and ABCB1 c.3435C>T were genotyped using a custom multiplexed SNaPshot® single base extension assay (Applied Biosystems, Carlsbad, CA) as previously described.26 Eight variant CYP2C9 alleles (*2 – *6, *8, *11, *13) were genotyped using the Tag-It™ Mutation Detection Kit (Luminex Molecular Diagnostics, Toronto, ON) and PCR-restriction fragment length polymorphism (PCR-RFLP) assays as previously reported.16
All 12 variant CYP2C8 alleles currently defined by the Cytochrome P450 Allele Nomenclature Committee (*2 – *10, *12 – *14) were genotyped using an additional custom multiplexed SNaPshot® single base extension assay (Applied Biosystems). Multiplexed PCR reactions were performed in 10 μl containing ~50 ng of DNA, 2× PCR buffer (Invitrogen, Carlsbad, CA), 1.5 mM MgCl2, 0.2 mM of each dNTP, forward and reverse primers (CYP2C8 exon 3: 0.8 μM; exons 4, 5, 7 and 9: 0.6 μM; exon 8: 0.4 μM; Supplemental Table S1), and 2.0 units of Platinum® Taq DNA Polymerase (Invitrogen). Amplification consisted of an initial denaturation step at 94°C for 5 min followed by 35 amplification cycles (94°C for 30 sec, 57°C for 30 sec, and 72°C for 1 min) and a final incubation at 72°C for 10 min. Amplicons were digested with 3.0 units of shrimp alkaline phosphatase (SAP) and 2.0 units of Exonuclease I (both from USB Corporation, Cleveland, OH). SNaPshot® primer extension reactions were performed in 10 μl containing 1× SNaPshot® Reaction Mix (Applied Biosystems), 0.2 μM of each allele-specific primer (Supplemental Table S1) and 3.0 μl of PCR product. Following the recommended thermal cycling, samples were treated with 1.0 unit of SAP, electrophoresed on an ABI Prism 3130 Genetic Analyzer, and analyzed using GeneMarker software v1.95 (SoftGenetics, State College, PA). Representative positive control samples for all identified CYP2C alleles were confirmed by bidirectional sequencing (Supplemental Figure S1), and wild-type (*1) CYP2C19, CYP2C9, and CYP2C8 alleles were assigned in the absence of other detectable variant alleles.
CYP2C19*4B Confirmation
Confirmation of potential CYP2C19*4B carriers was performed by cloning and allele-specific sequencing of a 1.2 kb fragment encompassing CYP2C19*17 (c.−806C>T) and *4 (c.1A>G) as previously described.26 For each sample, six to ten colonies were propagated and bidirectionally sequenced using M13 and T7 vector-specific primers. All plasmid sequence data were analyzed using Mutation Surveyor software v3.30 (SoftGenetics).
Statistical Analyses and Haplotyping
Observed genotype frequencies were compared with those expected under Hardy-Weinberg equilibrium using the χ2 test for each racial and ethnic group. The χ2 test was also used to detect overall and pairwise differences in allele frequencies between all tested populations. Pairwise LD between tested variants was assessed using Lewontin's D' and the squared correlation coefficient between allele frequencies (r2) expressed as a function of D'. The expectation-maximization (EM) algorithm was implemented to calculate maximum likelihood estimates of haplotype frequencies assuming Hardy-Weinberg equilibrium. All analyses were conducted using SAS/Genetics software (SAS Institute, Inc., Cary, NC).
RESULTS
CYP2C19 Allele and Genotype Frequencies
The CYP2C19 allele and genotype frequencies are summarized in Tables 1 and 2. All alleles were in Hardy-Weinberg equilibrium (p>0.05) and no studied population carried the *4A, *5, *7, *10, *16, or *22 allele. The overall across-population difference in CYP2C19 allele frequencies was significant for five polymorphic variants (rs12248560 [*17], rs4244285 [*2], rs4986893 [*3], rs17882687 [*15], rs28399504 [*4]; p<0.02). The CYP2C19*4B allele was detected in both the Caucasian and Hispanic populations and confirmed by cloning and allele-specific sequencing as previously described.26 The combined frequencies of detected variant CYP2C19 alleles were 0.406 (African-American), 0.386 (Asian), 0.304 (Caucasian), 0.296 (Hispanic), and 0.368 (AJ).
TABLE 1.
CYP2C19 Allele Frequencies
| African-American (n = 500) |
Asian (n = 500) |
Caucasian (n = 500) |
Hispanic (n = 500) |
Ashkenazi Jewisha (n = 500) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CYP2C19 Allele | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI |
| *1 | 0.594 | 0.551–0.637 | 0.614 | 0.571–0.657 | 0.696 | 0.656–0.736 | 0.704 | 0.664–0.744 | 0.632 | 0.590–0.674 |
| *2 | 0.194 | 0.159–0.229 | 0.276 | 0.237–0.315 | 0.132 | 0.102–0.161 | 0.128 | 0.099–0.157 | 0.146 | 0.115–0.177 |
| *3 | 0.004 | 0.000–0.010 | 0.048 | 0.029–0.067 | 0.004 | 0.000-0.010 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *4A | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *4B | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.004 | 0.000–0.010 | 0.002 | 0.000–0.006 | 0.020 | 0.008–0.032 |
| *5 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *6 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.002 | 0.000–0.006 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *7 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *8 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.002 | 0.000–0.006 | 0.004 | 0.000–0.010 | 0.000 | 0.000–0.000 |
| *9 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.002 | 0.000–0.006 | 0.000 | 0.000–0.000 |
| *10 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *12 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *13 | 0.012 | 0.000–0.022 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.004 | 0.000–0.010 | 0.000 | 0.000–0.000 |
| *14 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *15 | 0.014 | 0.004–0.024 | 0.000 | 0.000–0.000 | 0.002 | 0.000–0.006 | 0.004 | 0.000–0.010 | 0.004 | 0.000–0.010 |
| *16 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *17 | 0.182 | 0.148–0.216 | 0.062 | 0.041–0.083 | 0.158 | 0.126–0.190 | 0.152 | 0.121–0.183 | 0.198 | 0.163–0.233 |
| *22 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
n: number of alleles; CI: confidence interval.
Data from Scott et al., 2011.26
TABLE 2.
CYP2C19 Genotype Frequencies
| Observed (expecteda) frequency (%) |
|||||
|---|---|---|---|---|---|
| Predicted CYP2C19 metabolizer phenotype/genotype | African-American (n = 250) | Asian (n = 250) | Caucasian (n = 250) | Hispanic(n = 250) | Ashkenazi Jewishb (n = 250) |
| Ultrarapid Metabolizer (UM) | |||||
| *17/*17 | 2.8 (3.3) | 1.6 (0.4) | 2.8 (2.5) | 2.4 (2.3) | 3.6 (3.9) |
| Extensive Metabolizer (EM) | |||||
| *1/*1 | 38.4 (35.3) | 36.4 (37.7) | 49.2 (48.4) | 50.4 (49.6) | 41.6 (39.9) |
| *1/*17c | 20.4 (21.6) | 5.6 (7.6) | 22.8 (22.0) | 20.4 (21.4) | 25.2 (25.0) |
|
|
|||||
| TOTAL: | 58.8 (56.9) | 42.0 (45.3) | 72.0 (70.4) | 70.8 (71.0) | 66.8 (65.0) |
| Intermediate Metabolizer (IM) | |||||
| *1/*2 | 18.4 (23.0) | 37.2 (33.9) | 16.4 (18.4) | 17.2 (18.0) | 16.0 (18.5) |
| *1/*3 | 0.4 (0.5) | 7.2 (5.9) | 0.4 (0.6) | 0.0 (0.0) | 0.0 (0.0) |
| *1/*4B | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.6) | 0.0 (0.3) | 2.0 (2.5) |
| *1/*6 | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.3) | 0.0 (0.0) | 0.0 (0.0) |
| *1/*8 | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.3) | 0.4 (0.6) | 0.0 (0.0) |
|
|
|||||
| TOTAL: | 18.8 (23.5) | 44.4 (39.8) | 17.6 (20.0) | 17.7 (18.9) | 18.0 (21.0) |
| Poor Metabolizer (PM) | |||||
| *2/*2 | 4.8 (3.8) | 6.4 (7.6) | 2.8 (1.7) | 2.0 (1.6) | 2.8 (2.1) |
| *2/*3 | 0.4 (0.2) | 1.6 (2.6) | 0.4 (0.1) | 0.0 (0.0) | 0.0 (0.0) |
| *2/*4B | 0.0 (0.0) | 0.0 (0.0) | 0.8 (0.1) | 0.0 (0.1) | 0.8 (0.6) |
| *3/*3 | 0.0 (0.0) | 0.4 (0.2) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
|
|
|||||
| TOTAL: | 5.2 (3.9) | 8.4 (10.5) | 4.0 (2.0) | 2.0 (1.8) | 3.6 (2.8) |
| Unknown | |||||
| *1/*9 | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.3) | 0.0 (0.0) |
| *1/*13 | 0.8 (1.4) | 0.0 (0.0) | 0.0 (0.0) | 0.8 (0.6) | 0.0 (0.0) |
| *1/*15 | 2.0 (1.7) | 0.0 (0.0) | 0.4 (0.3) | 0.8 (0.6) | 0.0 (0.0) |
| *2/*13 | 0.8 (0.5) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.1) | 0.0 (0.0) |
| *2/*15 | 0.4 (0.5) | 0.0 (0.0) | 0.0 (0.1) | 0.0 (0.1) | 0.4 (0.1) |
| *2/*17 | 9.2 (7.1) | 3.6 (3.4) | 3.2 (4.2) | 4.4 (3.9) | 6.4 (5.8) |
| *3/*17 | 0.0 (0.1) | 0.0 (0.6) | 0.0 (0.1) | 0.0 (0.0) | 0.0 (0.0) |
| *4B/*15 | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.0) |
| *4B/*17 | 0.0 (0.0) | 0.0 (0.0) | 0.0(0.1) | 0.4(0.1) | 0.8 (0.8) |
| *8/*17 | 0.4 (0.1) | 0.0 (0.0) | 0.0 (0.1) | 0.4 (0.1) | 0.0 (0.0) |
| *13/*17 | 0.8 (0.4) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.1) | 0.0 (0.0) |
| *15/*17 | 0.4 (0.5) | 0.0 (0.0) | 0.0 (0.1) | 0.0 (0.1) | 0.0 (0.2) |
|
|
|||||
| TOTAL: | 14.4 (12.3) | 3.6 (4.0) | 3.6 (4.9) | 7.2 (5.9) | 8.0 (7.4) |
Based on their observed genotypes, the African-American, Asian, Caucasian, Hispanic, and AJ predicted CYP2C19 metabolic phenotypes3, 5,7were distributed as ultrarapid (3%, 2%, 3%, 2%, 4%), extensive (59%, 42%, 72%, 71%, 67%), intermediate (19%, 44%, 18%, 18%, 18%), and poor (5%, 8%, 4%, 2%, 4%) metabolizers, respectively (Table 2). Some of the variant CYP2C19 alleles (*9, *10, *12 – *16, *22) in the expanded panel currently do not have clear phenotypic consequences, as do compound heterozygous genotypes that include both gain- and loss-of-function alleles (e.g., *2/*17). As such, the frequencies of individuals with unknown predicted metabolic phenotypes using this CYP2C19 genotyping panel in the African-American, Asian, Caucasian, Hispanic, and AJ were 14%, 4%, 4%, 7%, and 8%, respectively.
ABCB1 Allele and Genotype Frequencies
Some studies have found that clopidogrel-treated patients with cardiovascular disease who are homozygous carriers of the synonymous ABCB1 c.3435C>T (p.I1145I) variant have higher rates of adverse cardiovascular events than c.3435C carriers during therapy, which was independent from and compounded by CYP2C19 loss-of-function alleles.32–34 However, conflicting data have been reported regarding which allele (c.3435C or c.3435T) was associated with the increased risk.35Supplemental Tables S2 and S3 summarize the identified ABCB1 c.3435C>T allele and genotype frequencies, which were statistically different between all tested populations (p<0.0001). Of note, the c.3435T/T genotype frequencies in the African-American, Asian, Caucasian, Hispanic, and AJ were 6%, 20%, 29%, 24%, and 8%, respectively. In addition, categorizing the tested subjects based on CYP2C19 loss-of-function allele carrier status and ABCB1 c.3435T/T genotype34 indicated that 34 – 66% of all tested multi-ethnic individuals carried CYP2C19 and ABCB1 genotypes that conferred an increased risk for clopidogrel nonresponsiveness and/or adverse effects (Supplemental Table S4 and Supplemental Figure S2).
CYP2C8 Allele and Genotype Frequencies
The CYP2C8 allele and genotype frequencies are summarized in Tables 3 and 4. All alleles were in Hardy-Weinberg equilibrium (p>0.05) and no studied population carried the *5 – *10, *12, or *13 allele. The overall across-population difference in CYP2C8 allele frequencies was highly significant for three polymorphic variants (rs11572080 [*3], rs11572103 [*2], rs10509681 [*3]; p<0.0001). The combined frequencies of detected variant CYP2C8 alleles were 0.122 (African-American), 0.038 (Asian), 0.130 (Caucasian), 0.116 (Hispanic), and 0.100 (AJ). The African-American, Asian, Caucasian, Hispanic, and AJ CYP2C8 genotype frequencies were distributed as homozygous wild-type (77%, 92%, 77%, 79%, 80%), heterozygous (22%, 8%, 20%, 20%, 20%), and homozygous variant/compound heterozygous (0.4%, 0%, 3%, 1%, 0%), respectively.
TABLE 3.
CYP2C8 Allele Frequencies
| African-American (n = 500) |
Asian (n = 500) |
Caucasian (n = 500) |
Hispanic (n = 500) |
Ashkenazi Jewish (n = 500) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CYP2C8 Allele | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI | Freq. | 95% CI |
| *1 | 0.878 | 0.849–0.907 | 0.962 | 0.945–0.979 | 0.870 | 0.841–0.899 | 0.884 | 0.856–0.912 | 0.900 | 0.874–0.926 |
| *2 | 0.100 | 0.074–0.126 | 0.004 | 0.000–0.010 | 0.002 | 0.000–0.006 | 0.022 | 0.009–0.035 | 0.004 | 0.000–0.010 |
| *3 | 0.010 | 0.001–0.019 | 0.022 | 0.009–0.035 | 0.094 | 0.068–0.120 | 0.076 | 0.053–0.099 | 0.076 | 0.053–0.099 |
| *4 | 0.012 | 0.002–0.022 | 0.012 | 0.002–0.022 | 0.032 | 0.017–0.047 | 0.018 | 0.006–0.030 | 0.020 | 0.008–0.032 |
| *5 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *6 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *7 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *8 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *9 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *10 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *12 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *13 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
| *14 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 | 0.002 | 0.000–0.006 | 0.000 | 0.000–0.000 | 0.000 | 0.000–0.000 |
n: number of alleles; CI: confidence interval.
TABLE 4.
CYP2C8 Genotype Frequencies
| CYP2C8 Genotype | Observed (expecteda) frequency (%) |
||||
|---|---|---|---|---|---|
| African-American (n = 248) | Asian (n = 249) | Caucasian (n = 248) | Hispanic (n = 248) | Ashkenazi Jewish (n = 249) | |
| Wild-type | |||||
| *1/*1 | 76.6 (76.9) | 92.0 (92.5) | 77.2 (75.7) | 78.6 (78.3) | 80.0 (81.0) |
| Heterozygous | |||||
| *1/*2 | 18.1 (17.7) | 0.8 (0.8) | 0.4 (0.3) | 4.0 (3.9) | 0.8 (0.7) |
| *1/*3 | 2.0 (1.8) | 4.4 (4.3) | 14.8 (16.4) | 12.9 (13.6) | 15.2 (13.7) |
| *1/*4 | 2.0 (2.1) | 2.4 (2.3) | 4.4 (5.6) | 2.8 (2.9) | 4.0 (3.6) |
| *1/*14 | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.3) | 0.0 (0.3) | 0.0 (0.0) |
|
|
|||||
| TOTAL: | 22.2 (21.6) | 7.6 (7.4) | 20.0 (22.6) | 19.8 (20.3) | 20.0 (18.0) |
| Homozygous Variant/Compound Heterozygous | |||||
| *2/*2 | 0.8 (1.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| *2/*3 | 0.0 (0.2) | 0.0 (0.0) | 0.0 (0.0) | 0.4 (0.3) | 0.0 (0.1) |
| *2/*4 | 0.4 (0.2) | 0.0 (0.0) | 0.0 (0.0) | 0.0(0.1) | 0.0 (0.0) |
| *3/*3 | 0.0 (0.0) | 0.0 (0.0) | 0.8 (0.9) | 0.8 (0.6) | 0.0 (0.6) |
| *3/*4 | 0.0 (0.0) | 0.0 (0.1) | 2.0 (0.6) | 0.4 (0.3) | 0.0 (0.3) |
|
|
|||||
| TOTAL: | 0.4 (0.3) | 0.0 (0.1) | 2.8 (1.5) | 1.2 (0.9) | 0.0 (0.9) |
n: number of subjects.
Predicted Hardy-Weinberg frequencies.
Linkage Disequilibrium and CYP2C Haplotypes
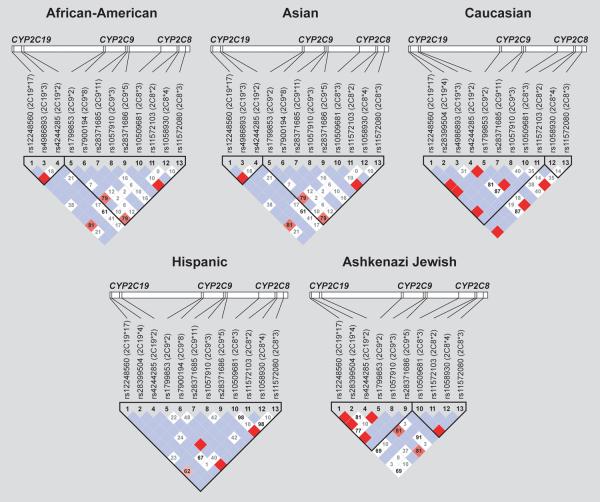
After combining the CYP2C19 and CYP2C8 genotyping results with the previously reported CYP2C9 data, pairwise LD was calculated and visualized using Haploview version 4.1 for each racial and ethnic group (Figure 1). Using 13 polymorphic alleles [CYP2C19*2, *3, *4, *17; CYP2C9*2, *3, *5, *8, *11; CYP2C8*2, *3 (p.R139K), *3 (p.K399R), *4], 33, 18, 19, 22, and 23 non-redundant CYP2C haplotypes were inferred in the African-American, Asian, Caucasian, Hispanic, and AJ populations, respectively. However, only 16 of all identified haplotypes had frequencies greater than 0.5% in at least one population and together accounted for ~96 – 99% of the overall CYP2C cluster haplotypic diversity in these populations (Table 5).
FIGURE 1.
Linkage disequilibrium (LD) across the CYP2C locus (10q23.33) in each tested population using 13 polymorphic SNPs. Pairwise LD between polymorphisms is expressed as D'. Significant linkage (logarithm of the odds, LOD≥2) is illustrated by red shading depending on the magnitude of D' (from pink to bright red), and insignificant linkage (LOD<2) is illustrated by blue (if D'=1) or white (if D'<1) shading. Haplotype blocks were inferred using the `Four gamete of LD' method (Haploview).
TABLE 5.
CYP2C Haplotype Frequencies
| Haplotypesa | rs12248560 (C>T; 2C19*17) |
rs28399504 (A>G; 2C19*4) |
rs4986893 (G>A; 2C19*3) |
rs4244285 (G>A; 2C19*2) |
rs1799853 (C>%T; 2C9*2) |
rs7900194 (G>%A; 2C9*8) |
rs28371685 (C>%T; 2C9*11) |
rs1057910 (A>%C; 2C9*3) |
rs28371686 (C>%G; 2C9*5) |
rs10509681 (A>;G; 2C8*3) |
rs11572103 (A>%T; 2C8*2) |
rs1058930 (C>%G; 2C8*4) |
rs11572080 (G>%A; 2C8*3) |
Frequency (95% CI) |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| African-American | Asian | Caucasian | Hispanic | Ashkenazi Jewish |
||||||||||||||
| 2C19-2C9-2C8 | ||||||||||||||||||
| *1-*1-*1 | C | A | G | G | C | G | C | A | C | A | A | C | G | 0.513 (0.473–0.554) |
0.545 (0.505–0.585) |
0.474 (0.435–0.513) |
0.534 (0. 494–0.573) |
0.406 (0.367–0.446) |
| *2-*1-*1 | C | A | G | A | C | G | C | A | C | A | A | C | G | 0.173 (0.142–0.204) |
0.272 (0.236–0.308) |
0.120 (0.094–0.145) |
0.125 (0.099–0.151) |
0.132 (0.105–0.160) |
| *2-*1-*4 | C | A | G | A | C | G | C | A | C | A | A | G | G | 0.005 (0.000–0.011) |
- | - | - | 0.006 (0.000–0.012) |
| *3-*1-*1 | C | A | A | G | C | G | C | A | C | A | A | C | G | - | 0.048 (0.031–0.065) |
- | - | - |
| *4B-*1-*1 | T | G | G | G | C | G | C | A | C | A | A | C | G | - | - | - | - | 0.016 (0.006–0.026) |
| *17-*1-*1 | T | A | G | G | C | G | C | A | C | A | A | C | G | 0.091 (0.068–0.115) |
0.056 (0.037–0.074) |
0.152 (0.124–0.180) |
0.134 (0.107–0.161) |
0.188 (0.156–0.219) |
| *17-*1-*2 | T | A | G | G | C | G | C | A | C | A | T | C | G | 0.075 (0.054–0.097) |
- | - | 0.017 (0.007–0.028) |
- |
| *1-*2-*1 | C | A | G | G | T | G | C | A | C | A | A | C | G | 0.012 (0.003–0.021) |
0.014 (0.005–0.024) |
0.059 (0.041–0.078) |
0.006 (0.000–0.013) |
0.067 (0.047–0.087) |
| *1-*2-*3 | C | A | G | G | T | G | C | A | C | G | A | C | A | - | 0.012 (0.003–0.021) |
0.089 (0.067–0.112) |
0.070 (0.050–0.090) |
0.067 (0.047–0.088) |
| *1-*3-*1 | C | A | G | G | C | G | C | C | C | A | A | C | G | 0.018 (0.007–0.028) |
0.021 (0.009–0.032) |
0.054 (0.036–0.072) |
0.049 (0.032–0.066) |
0.080 (0.058–0.102) |
| *1-*3-*3 | C | A | G | G | C | G | C | C | C | G | A | G | A | - | 0.007 (0.000–0.014) |
- | - | 0.006 (0.000–0.013) |
| *1-*5-*1 | C | A | G | G | C | G | C | A | G | A | A | C | G | 0.012 (0.003–0.021) |
- | - | 0.011 (0.003–0.019) |
- |
| *1-*8-*1 | C | A | G | G | C | A | C | A | C | A | A | C | G | 0.039 (0.023–0.055) |
- | - | 0.010 (0.002–0.018) |
- |
| *1-*11-*1 | C | A | G | G | C | G | T | A | C | A | A | C | G | 0.015 (0.005–0.025) |
- | - | 0.005 (0.000–0.011) |
- |
| *1-*1-*2 | C | A | G | G | C | G | C | A | C | A | T | C | G | 0.008 (0.001–0.015) |
- | - | 0.008 (0.001–0.015) |
- |
| *1-*1-*4 | C | A | G | G | C | G | C | A | C | A | A | G | G | - | 0.010 (0.002–0.019) |
0.022 (0.010–0.033) |
0.009 (0.001–0.016) |
0.008 (0.001–0.015) |
n: number of subjects; CI: confidence interval.
Shaded boxes represent variant nucleotides.
Estimated haplotype frequencies showed considerable variation across the five populations and some of the commonly studied CYP2C19, CYP2C9 and CYP2C8 functional variants were found to exist in more than one haplotype. The two most common variant allele-containing haplotypes were 2C19*2-2C9*1-2C8*1 (12 – 27%) and 2C19*17-2C9*1-2C8*1 (6 – 19%). Importantly, a 2C19*17-2C9*1-2C8*2 haplotype was also identified among African-Americans (7.5%) and Hispanics (1.7%), indicating that CYP2C19*17 does not always tag a CYP2C haplotype that encodes efficient CYP2C-substrate metabolism as previously reported in Nordic populations.22 The estimated D' and r2 between 2C19*17 and 2C8*2 were 0.813 and 0.325 among African-Americans, and 0.626 and 0.057 among Hispanics, respectively (Table 6). In addition, a haplotype containing two CYP2C loss-of-function alleles (2C19*1-2C9*2-2C8*3) was identified in all populations (1.2 – 8.9%) except African-Americans. Unique ethnic-specific and/or rare haplotypes were also detected at frequencies of 0.5 – 4.8%, including 2C19*3-2C9*1-2C8*1 (Asians), 2C19*4B-2C9*1-2C8*1 (AJs), 2C19*2-2C9*1-2C8*4 (African-Americans and AJs), and 2C19*1-2C9*3-2C8*3 (Asians and AJs).
TABLE 6.
Linkage disequilibrium between CYP2C19*17 and CYP2C8*2
| Population | CYP2C19*17 (rs12248560) Frequency | CYP2C8*2 (rs11572103) Frequency | D' | r2 | 2C19*17-2C9*1-2C8*2 Frequency |
|---|---|---|---|---|---|
| African-American | 0.182 | 0.100 | 0.813 | 0.325 | 0.075 |
| Asian | 0.062 | 0.004 | 0.471 | 0.018 | ND |
| Caucasian | 0.158 | 0.002 | 1.000 | 0.028 | ND |
| Hispanic | 0.152 | 0.022 | 0.626 | 0.057 | 0.017 |
| Ashkenazi Jewish | 0.198 | 0.004 | 1.000 | 0.017 | ND |
ND: not detected.
DISCUSSION
The paucity of frequency data for variant CYP2C19 and CYP2C8 alleles beyond those commonly tested (e.g., *2 and *3) prompted our genotyping of 28 functional and/or coding region variants (CYP2C19*2 – *10, *12 – *17, *22; CYP2C8*2 – *10, *12 – *14) in the African-American, Asian, Caucasian, Hispanic, and AJ populations. Although not all alleles were detected, the combined variant CYP2C19 allele frequencies ranged from ~0.30 – 0.41 in the tested populations; however, the combined CYP2C8 frequencies were much lower (~0.04 – 0.13). After combining these results with our previously reported CYP2C9 data (36 total variants),16 16 unique CYP2C haplotypes were inferred in the tested populations with frequencies greater than 0.5%. Our haplotype data indicate that CYP2C19*17 does not always tag a CYP2C haplotype encoding efficient CYP2C-substrate metabolism as previously reported in Nordic populations22 and highlight that, despite largely acting as independent loci, CYP2C19*17 and *2 can also be found in LD with other variant CYP2C alleles that influence the metabolizer phenotypes.
The first CYP2C19 loss-of-function allele discovered based on its role in impaired mephenytoin metabolism was *2 (c.681G>A),39 and since then a number of additional variants have been identified in different populations. Some have known effects on CYP2C19 enzyme activity, whereas others do not have clear phenotypic effects.7, 13 Consequently, our study using an expanded panel of 16 CYP2C19 variant alleles identified individuals with certain genotypes (e.g., *1/*15, *2/*17) that have unknown consequences on CYP2C19-mediated drug metabolism. The identified frequencies of individuals with unknown predicted metabolizer phenotypes ranged from 4 – 14% in the tested populations (highest in African-Americans), suggesting that further in vivo and/or in vitro phenotyping studies with these specific variant alleles are warranted prior to their inclusion in clinical genotyping panels. CYP2C19 poor metabolizers typically carry two loss-of-function alleles and the frequencies of these genotypes ranged from ~2 – 8% in the tested populations, which was highest in Asians due to their higher frequencies of both *2 and *3.
CYP2C19 has recently received considerable attention due to its principal role in the bioactivation of the antiplatelet agent clopidogrel. Importantly, CYP2C19 loss-of-function alleles have been associated with lower active metabolite exposure,40–41 decreased platelet responsiveness ex vivo among clopidogrel-treated subjects,42–45 and increased adverse cardiovascular event rates among clopidogrel-treated patients with acute coronary syndromes and/or those undergoing percutaneous coronary intervention.33–34, 44–48 The increased risk among CYP2C19 loss-of-function allele carriers, particularly for poor metabolizers, prompted product insert label revision by the U.S. Food and Drug Administration (FDA) and additional interest in implementing CYP2C19 clinical testing to guide antiplatelet therapy for some cardiovascular patient populations.28, 30, 49–52 Recently, the CYP2C19*4B allele was discovered in the AJ population which has important implications for clinical CYP2C19 testing as the allele harbors both gain-of-function [c.−806C>T (*17)] and loss-of-function [c.1A>G (*4)] variants on the same haplotype.26 In the current study, CYP2C19*4B was also identified in both the Caucasian and Hispanic populations at lower frequencies (≤1%); however, no carriers of the *4A allele (c.1A>G without c.−806C>T) were detected in any of the tested populations. Importantly, we previously identified CYP2C19*4A in the Sephardic Jewish population,26 which confirms the independent existence of these two sub-alleles.
Although more controversial than CYP2C19, some studies have found that carriers of the ABCB1 (P-glycoprotein) c.3435C>T synonymous variant have higher rates of adverse cardiovascular events during clopidogrel therapy,32–35, 53 suggesting that ABCB1 might influence clopidogrel efflux and drug bioavailability. However, conflicting data have been reported regarding both the relationship between c.3435C>T and P-glycoprotein expression54–56 and which allele (c.3435C or c.3435T) is associated with the increased cardiovascular risk.35 Despite this discrepancy, large clinical studies found that c.3435T/T patients had a higher rate of adverse cardiovascular events than c.3435C homozygotes during clopidogrel therapy, which was independent from and compounded by CYP2C19 loss-of-function alleles.33–34 Our study identified a high frequency of c.3435T/T homozygotes in the tested populations (6 – 30%), and when combined with the CYP2C19 variant frequencies, 34 – 66% of tested individuals harbored a CYP2C19 loss-of-function allele and/or ABCB1 c.3435T/T, which could influence their response to clopidogrel.
CYP2C8 is involved in the metabolism of a number of drugs and xenobiotics including arachidonic acid, repaglinide, and the anticancer agent paclitaxel.57–59 Although early in vitro data suggested that CYP2C8*2 and *3 resulted in impaired activity and decreased metabolism of CYP2C8 substrates, some in vivo data on the phenotypic consequences of these alleles have yielded contradictory results.58–60 Moreover, the effects of the known variant CYP2C8 alleles on activity may be substrate specific.60 We genotyped all 12 currently defined variant CYP2C8 alleles (*2 – *10, *12 – *14) and only detected *2, *3, *4 and *14 in the tested populations. All other alleles were originally discovered at low frequencies in Japanese individuals,61–64 which may have been an underrepresented ethnicity in our heterogeneous Asian population. Together, these results suggest that future CYP2C8 pharmacogenetic studies could benefit from additional genotype-phenotype correlation data, and further CYP2C8 sequencing of phenotype outliers in different racial and ethnic populations.
The CYP2C9*2 (p.R144C) reduced function allele previously was found linked with CYP2C8*3 in the Swedish population,20 underscoring the strong LD across the CYP2C region.18–19 This finding highlighted the possibility of jointly inheriting multiple CYP2C reduced function alleles on individual haplotypes, which has important implications for the metabolism of common CYP2C9 and CYP2C8 substrates (e.g., arachidonic acid, nonsteroidal anti-inflammatory drugs, etc.). Global variation in CYP2C9-CYP2C8 haplotype frequencies, including the 2C9*2-2C8*3 haplotype, has been reported in other worldwide populations,21 and very recent reports have extended these haplotype studies to include CYP2C19 in selected populations.22–24 For example, in Nordic populations, the CYP2C19*17 gain-of-function allele was found almost exclusively with wild-type CYP2C9*1 and CYP2C8*1.22 However, CYP2C19*17 subsequently was reported in LD with CYP2C8*2 among Brazilian individuals of African descent, prompting these authors to conclude that further multi-ethnic CYP2C haplotype studies including CYP2C19*17 were warranted.24
Interrogating 36 variant CYP2C alleles in five major racial and ethnic populations resulted in 16 inferred CYP2C haplotypes with frequencies greater than 0.5% in our study. Of note, the 2C19*1-2C9*2-2C8*3 haplotype was identified in all racial and ethnic groups except African-Americans. In contrast, the aforementioned 2C19*17-2C9*1-2C8*2 haplotype reported among Brazilians of African descent24 was identified in both our African-American (8%) and Hispanic (2%) populations. As Hispanics can be three-way admixtures of Native American, European and West African populations,65 our data underscore that CYP2C19*17 should not be used as a sole determinant for extensive CYP2C substrate metabolism in populations with African descent.24 However, 2C19*17-2C9*1-2C8*1 was the more common CYP2C19*17-containing haplotype among all carriers of this variant allele (African-American: 9%; Asian: 6%; Caucasian: 15%; Hispanic: 13%; AJ: 19%). Notably, despite the identification of the 2C19*17-2C9*1-2C8*2 haplotype, CYP2C19*17 still appears to be a marker of extensive CYP2C9 metabolism, which may be more clinically relevant than CYP2C8-mediated drug metabolism.
Other novel haplotypes with multiple variants included 2C19*2-2C9*1-2C8*4 in the African-American and AJ populations, and 2C19*1-2C9*3-2C8*3 in the Asian and AJ populations. In addition, the 2C19*3-2C9*1-2C8*1 and 2C19*4B-2C9*1-2C8*1 haplotypes were found exclusively in the Asian and AJ populations, respectively. Together, these haplotype results are consistent with those previously reported in selected ethnic populations using fewer alleles and extend their findings by identifying both known and novel rare CYP2C haplotypes in other major racial and ethnic groups. Given the vast ethnic diversity prevalent among the Asian racial group, future CYP2C haplotype studies that include additional and more clearly defined ethnic Asian subpopulations are warranted.
In addition, future haplotype studies are warranted as novel CYP2C variants with clinical relevance are identified. For example, an intronic CYP2C9 polymorphism (rs7089580) was recently associated with warfarin dose variability in the African-American population; however, it is currently unclear if it is a functional non-coding variant with a role in gene transcription or if it is in LD with another functional CYP2C9 variant.66 As future studies establish which sequence variant of this potentially novel CYP2C9 allele is functionally relevant, it will be important to include it in CYP2C haplotype studies of the African-American and other populations. These studies could be instructive for the warfarin pharmacogenetics field as CYP2C haplotypes with loss-of-function variants in both CYP2C9 and CYP2C19 could influence dosing variability by affecting S- and R-warfarin pharmacokinetics, respectively. Although the relationship between CYP2C9 loss-of-function alleles and impaired S-warfarin metabolism is well established, a very recent study has reported an association between a CYP2C19 promoter variant (rs3814637) and R-warfarin clearance.67
In conclusion, our study determined the frequencies of 28 variant CYP2C19 and CYP2C8 alleles in the African-American, Asian, Caucasian, Hispanic and AJ populations, which highlight the polymorphic nature of CYP2C19 compared to CYP2C8 in all tested populations. Additionally, the recently described CYP2C19*4B allele, originally discovered in the AJ population, was identified in the Caucasian and Hispanic populations. Combining all genotyping results with our previous CYP2C9 data allowed for CYP2C haplotype structure analyses on all populations, which identified both previously reported and novel haplotypes. Taken together, these results have important implications for pharmacogenomic association studies involving the CYP2C locus and are clinically relevant when administering CYP2C-substrate medications.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported in part by grant KL2 RR029885 (S.A.S.) from the National Institutes of Health. The eSensor® 2C19 Test reagents used in this study were generously provided by GenMark Diagnostics (Carlsbad, CA).
J.-S.H. has received research grant support from Fondation de France, INSERM, Fédération Francaise de Cardiologie, Biotronik, and Medco Research Institute; consulting fees from Biotronik and Medco Health Solutions; and lecture fees from Daiichi Sankyo, Eli Lilly, and Bristol-Myers Squibb. S.A.S. has been a consultant to USDS, Inc.
SOURCES OF SUPPORT: This research was supported in part by grant KL2 RR029885 (S.A.S.) from the National Institutes of Health. eSensor® 2C19 Test reagents for this study were supplied by GenMark Diagnostics (Carlsbad, CA).
Footnotes
CONFLICT OF INTEREST All other authors declare no conflict of interest.
REFERENCES
- 1.Daly AK. Pharmacogenetics of the cytochromes P450. Curr Top Med Chem. 2004;4(16):1733–1744. doi: 10.2174/1568026043387070. [DOI] [PubMed] [Google Scholar]
- 2.Gray IC, Nobile C, Muresu R, Ford S, Spurr NK. A 2.4-megabase physical map spanning the CYP2C gene cluster on chromosome 10q24. Genomics. 1995;28(2):328–332. doi: 10.1006/geno.1995.1149. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein JA. Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol. 2001;52(4):349–355. doi: 10.1046/j.0306-5251.2001.01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y, Goldstein JA. The transcriptional regulation of the human CYP2C genes. Curr Drug Metab. 2009;10(6):567–578. doi: 10.2174/138920009789375397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desta Z, Zhao X, Shin JG, Flockhart DA. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet. 2002;41(12):913–958. doi: 10.2165/00003088-200241120-00002. [DOI] [PubMed] [Google Scholar]
- 6.Price MJ, Tantry US, Gurbel PA. The influence of CYP2C19 polymorphisms on the pharmacokinetics, pharmacodynamics, and clinical effectiveness of P2Y(12) inhibitors. Rev Cardiovasc Med. 2011;12(1):1–12. doi: 10.3909/ricm0590. [DOI] [PubMed] [Google Scholar]
- 7.Scott SA, Sangkuhl K, Shuldiner AR, Hulot JS, Thorn CF, Altman RB, et al. PharmGKB summary: very important pharmacogene information for cytochrome P450, family 2, subfamily C, polypeptide 19. Pharmacogenet Genomics. 2011 doi: 10.1097/FPC.0b013e32834d4962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miners JO, Birkett DJ. Cytochrome P4502C9: an enzyme of major importance in human drug metabolism. Br J Clin Pharmacol. 1998;45(6):525–538. doi: 10.1046/j.1365-2125.1998.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Booven D, Marsh S, McLeod H, Carrillo MW, Sangkuhl K, Klein TE, et al. Cytochrome P450 2C9-CYP2C9. Pharmacogenet Genomics. 2010;20(4):277–281. doi: 10.1097/FPC.0b013e3283349e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai XS, Yang LP, Li XT, Liu JP, Zhou ZW, Zhou SF. Human CYP2C8: structure, substrate specificity, inhibitor selectivity, inducers and polymorphisms. Curr Drug Metab. 2009;10(9):1009–1047. doi: 10.2174/138920009790711832. [DOI] [PubMed] [Google Scholar]
- 11.Tsuneoka Y, Matsuo Y, Okuyama E, Watanabe Y, Ichikawa Y. Genetic analysis of the cytochrome P-45OIIC18 (CYP2C18) gene and a novel member of the CYP2C subfamily. FEBS Lett. 1996;384(3):281–284. doi: 10.1016/0014-5793(96)00329-8. [DOI] [PubMed] [Google Scholar]
- 12.Komai K, Sumida K, Kaneko H, Nakatsuka I. Identification of a new non-functional CYP2C18 allele in Japanese: substitution of T204 to A in exon2 generates a premature stop codon. Pharmacogenetics. 1996;6(1):117–119. doi: 10.1097/00008571-199602000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Sim SC, Ingelman-Sundberg M. The Human Cytochrome P450 (CYP) Allele Nomenclature website: a peer-reviewed database of CYP variants and their associated effects. Hum Genomics. 2010;4(4):278–281. doi: 10.1186/1479-7364-4-4-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie HG, Prasad HC, Kim RB, Stein CM. CYP2C9 allelic variants: ethnic distribution and functional significance. Adv Drug Deliv Rev. 2002;54(10):1257–1270. doi: 10.1016/s0169-409x(02)00076-5. [DOI] [PubMed] [Google Scholar]
- 15.Ross KA, Bigham AW, Edwards M, Gozdzik A, Suarez-Kurtz G, Parra EJ. Worldwide allele frequency distribution of four polymorphisms associated with warfarin dose requirements. J Hum Genet. 2010;55(9):582–589. doi: 10.1038/jhg.2010.73. [DOI] [PubMed] [Google Scholar]
- 16.Scott SA, Khasawneh R, Peter I, Kornreich R, Desnick RJ. Combined CYP2C9, VKORC1 and CYP4F2 frequencies among racial and ethnic groups. Pharmacogenomics. 2010;11(6):781–791. doi: 10.2217/pgs.10.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Georgitsi M, Viennas E, Gkantouna V, Christodoulopoulou E, Zagoriti Z, Tafrali C, et al. Population-specific documentation of pharmacogenomic markers and their allelic frequencies in FINDbase. Pharmacogenomics. 2011;12(1):49–58. doi: 10.2217/pgs.10.169. [DOI] [PubMed] [Google Scholar]
- 18.Ahmadi KR, Weale ME, Xue ZY, Soranzo N, Yarnall DP, Briley JD, et al. A single-nucleotide polymorphism tagging set for human drug metabolism and transport. Nat Genet. 2005;37(1):84–89. doi: 10.1038/ng1488. [DOI] [PubMed] [Google Scholar]
- 19.Walton R, Kimber M, Rockett K, Trafford C, Kwiatkowski D, Sirugo G. Haplotype block structure of the cytochrome P450 CYP2C gene cluster on chromosome 10. Nat Genet. 2005;37(9):915–916. doi: 10.1038/ng0905-915. author reply 916. [DOI] [PubMed] [Google Scholar]
- 20.Yasar U, Lundgren S, Eliasson E, Bennet A, Wiman B, de Faire U, et al. Linkage between the CYP2C8 and CYP2C9 genetic polymorphisms. Biochem Biophys Res Commun. 2002;299(1):25–28. doi: 10.1016/s0006-291x(02)02592-5. [DOI] [PubMed] [Google Scholar]
- 21.Speed WC, Kang SP, Tuck DP, Harris LN, Kidd KK. Global variation in CYP2C8-CYP2C9 functional haplotypes. Pharmacogenomics J. 2009;9(4):283–290. doi: 10.1038/tpj.2009.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pedersen RS, Brasch-Andersen C, Sim SC, Bergmann TK, Halling J, Petersen MS, et al. Linkage disequilibrium between the CYP2C19*17 allele and wildtype CYP2C8 and CYP2C9 alleles: identification of CYP2C haplotypes in healthy Nordic populations. Eur J Clin Pharmacol. 2010;66(12):1199–1205. doi: 10.1007/s00228-010-0864-8. [DOI] [PubMed] [Google Scholar]
- 23.Suarez-Kurtz G, Genro JP, de Moraes MO, Ojopi EB, Pena SD, Perini JA, et al. Global pharmacogenomics: Impact of population diversity on the distribution of polymorphisms in the CYP2C cluster among Brazilians. Pharmacogenomics J. 2010 doi: 10.1038/tpj.2010.89. [DOI] [PubMed] [Google Scholar]
- 24.Suarez-Kurtz G. Linkage disequilibrium between the CYP2C19*17 and CYP2C8*2 alleles in populations of African descent. Eur J Clin Pharmacol. 2011;67(2):211–212. doi: 10.1007/s00228-010-0910-6. [DOI] [PubMed] [Google Scholar]
- 25.Scott SA, Jaremko M, Lubitz SA, Kornreich R, Halperin JL, Desnick RJ. CYP2C9*8 is prevalent among African-Americans: implications for pharmacogenetic dosing. Pharmacogenomics. 2009;10(8):1243–1255. doi: 10.2217/pgs.09.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scott SA, Martis S, Peter I, Kasai Y, Kornreich R, Desnick RJ. Identification of CYP2C19*4B: pharmacogenetic implications for drug metabolism including clopidogrel responsiveness. Pharmacogenomics J. 2011 doi: 10.1038/tpj.2011.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gurbel PA, Tantry US, Shuldiner AR, Kereiakes DJ. Genotyping: one piece of the puzzle to personalize antiplatelet therapy. J Am Coll Cardiol. 2010;56(2):112–116. doi: 10.1016/j.jacc.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Holmes DR, Jr., Dehmer GJ, Kaul S, Leifer D, O'Gara PT, Stein CM. ACCF/AHA clopidogrel clinical alert: approaches to the FDA “boxed warning”: a report of the American College of Cardiology Foundation Task Force on clinical expert consensus documents and the American Heart Association endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2010;56(4):321–341. doi: 10.1016/j.jacc.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Beitelshees AL, Horenstein RB, Vesely MR, Mehra MR, Shuldiner AR. Pharmacogenetics and clopidogrel response in patients undergoing percutaneous coronary interventions. Clin Pharmacol Ther. 2011;89(3):455–459. doi: 10.1038/clpt.2010.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scott SA, Sangkuhl K, Gardner EE, Stein CM, Hulot JS, Johnson JA, et al. Clinical Pharmacogenetics Implementation Consortium Guidelines for Cytochrome P450-2C19 (CYP2C19) Genotype and Clopidogrel Therapy. Clin Pharmacol Ther. 2011;90(2):328–332. doi: 10.1038/clpt.2011.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, et al. Pharmacogenetics: from bench to byte--an update of guidelines. Clin Pharmacol Ther. 2011;89(5):662–673. doi: 10.1038/clpt.2011.34. [DOI] [PubMed] [Google Scholar]
- 32.Taubert D, von Beckerath N, Grimberg G, Lazar A, Jung N, Goeser T, et al. Impact of P-glycoprotein on clopidogrel absorption. Clin Pharmacol Ther. 2006;80(5):486–501. doi: 10.1016/j.clpt.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Meneveau N, et al. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009;360(4):363–375. doi: 10.1056/NEJMoa0808227. [DOI] [PubMed] [Google Scholar]
- 34.Mega JL, Close SL, Wiviott SD, Shen L, Walker JR, Simon T, et al. Genetic variants in ABCB1 and CYP2C19 and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial: a pharmacogenetic analysis. Lancet. 2010;376(9749):1312–1319. doi: 10.1016/S0140-6736(10)61273-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wallentin L, James S, Storey RF, Armstrong M, Barratt BJ, Horrow J, et al. Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelor versus clopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trial. Lancet. 2010;376(9749):1320–1328. doi: 10.1016/S0140-6736(10)61274-3. [DOI] [PubMed] [Google Scholar]
- 36.Scott SA, Edelmann L, Kornreich R, Erazo M, Desnick RJ. CYP2C9, CYP2C19 and CYP2D6 allele frequencies in the Ashkenazi Jewish population. Pharmacogenomics. 2007;8(7):721–730. doi: 10.2217/14622416.8.7.721. [DOI] [PubMed] [Google Scholar]
- 37.Scott SA, Edelmann L, Kornreich R, Desnick RJ. Warfarin pharmacogenetics: CYP2C9 and VKORC1 genotypes predict different sensitivity and resistance frequencies in the Ashkenazi and Sephardi Jewish populations. Am J Hum Genet. 2008;82(2):495–500. doi: 10.1016/j.ajhg.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scott SA, Edelmann L, Liu L, Luo M, Desnick RJ, Kornreich R. Experience with carrier screening and prenatal diagnosis for 16 Ashkenazi Jewish genetic diseases. Hum Mutat. 2010;31(11):1240–1250. doi: 10.1002/humu.21327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA. The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem. 1994;269(22):15419–15422. [PubMed] [Google Scholar]
- 40.Brandt JT, Close SL, Iturria SJ, Payne CD, Farid NA, Ernest CS, 2nd, et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost. 2007;5(12):2429–2436. doi: 10.1111/j.1538-7836.2007.02775.x. [DOI] [PubMed] [Google Scholar]
- 41.Collet JP, Hulot JS, Anzaha G, Pena A, Chastre T, Caron C, et al. High doses of clopidogrel to overcome genetic resistance: the randomized crossover CLOVIS-2 (Clopidogrel and Response Variability Investigation Study 2) JACC Cardiovasc Interv. 2011;4(4):392–402. doi: 10.1016/j.jcin.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Hulot JS, Bura A, Villard E, Azizi M, Remones V, Goyenvalle C, et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood. 2006;108(7):2244–2247. doi: 10.1182/blood-2006-04-013052. [DOI] [PubMed] [Google Scholar]
- 43.Giusti B, Gori AM, Marcucci R, Saracini C, Sestini I, Paniccia R, et al. Cytochrome P450 2C19 loss-of-function polymorphism, but not CYP3A4 IVS10 + 12G/A and P2Y12 T744C polymorphisms, is associated with response variability to dual antiplatelet treatment in high-risk vascular patients. Pharmacogenet Genomics. 2007;17(12):1057–1064. doi: 10.1097/FPC.0b013e3282f1b2be. [DOI] [PubMed] [Google Scholar]
- 44.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360(4):354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 45.Shuldiner AR, O'Connell JR, Bliden KP, Gandhi A, Ryan K, Horenstein RB, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA. 2009;302(8):849–857. doi: 10.1001/jama.2009.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J, et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet. 2009;373(9660):309–317. doi: 10.1016/S0140-6736(08)61845-0. [DOI] [PubMed] [Google Scholar]
- 47.Hulot JS, Collet JP, Silvain J, Pena A, Bellemain-Appaix A, Barthelemy O, et al. Cardiovascular risk in clopidogrel-treated patients according to cytochrome P450 2C19*2 loss-of-function allele or proton pump inhibitor coadministration: a systematic meta-analysis. J Am Coll Cardiol. 2010;56(2):134–143. doi: 10.1016/j.jacc.2009.12.071. [DOI] [PubMed] [Google Scholar]
- 48.Mega JL, Simon T, Collet JP, Anderson JL, Antman EM, Bliden K, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA. 2010;304(16):1821–1830. doi: 10.1001/jama.2010.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gladding P, Panattoni L, Webster M, Cho L, Ellis S. Clopidogrel pharmacogenomics: next steps: a clinical algorithm, gene-gene interactions, and an elusive outcomes trial. JACC Cardiovasc Interv. 2010;3(10):995–1000. doi: 10.1016/j.jcin.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 50.Roden DM, Shuldiner AR. Responding to the clopidogrel warning by the US food and drug administration: real life is complicated. Circulation. 2010;122(5):445–448. doi: 10.1161/CIRCULATIONAHA.110.973362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ned Mmsc RM., Phd Genetic testing for CYP450 polymorphisms to predict response to clopidogrel: current evidence and test availability. Application: pharmacogenomics. PLoS Curr. 2010;2 doi: 10.1371/currents.RRN1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee CC, McMillin GA, Babic N, Melis R, Yeo KT. Evaluation of a CYP2C19 genotype panel on the GenMark eSensor(R) platform and the comparison to the Autogenomics Infiniti and Luminex CYP2C19 panels. Clin Chim Acta. 2011;412(11–12):1133–1137. doi: 10.1016/j.cca.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 53.Cayla G, Hulot JS, O'Connor SA, Pathak A, Scott SA, Gruel Y, et al. Clinical, angiographic, and genetic factors associated with early coronary stent thrombosis. JAMA. 2011;306(16):1765–1774. doi: 10.1001/jama.2011.1529. [DOI] [PubMed] [Google Scholar]
- 54.Hoffmeyer S, Burk O, von Richter O, Arnold HP, Brockmoller J, Johne A, et al. Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci U S A. 2000;97(7):3473–3478. doi: 10.1073/pnas.050585397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakamura T, Sakaeda T, Horinouchi M, Tamura T, Aoyama N, Shirakawa T, et al. Effect of the mutation (C3435T) at exon 26 of the MDR1 gene on expression level of MDR1 messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clin Pharmacol Ther. 2002;71(4):297–303. doi: 10.1067/mcp.2002.122055. [DOI] [PubMed] [Google Scholar]
- 56.Owen A, Goldring C, Morgan P, Chadwick D, Park BK, Pirmohamed M. Relationship between the C3435T and G2677T(A) polymorphisms in the ABCB1 gene and P-glycoprotein expression in human liver. Br J Clin Pharmacol. 2005;59(3):365–370. doi: 10.1111/j.1365-2125.2005.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rahman A, Korzekwa KR, Grogan J, Gonzalez FJ, Harris JW. Selective biotransformation of taxol to 6 alpha-hydroxytaxol by human cytochrome P450 2C8. Cancer Res. 1994;54(21):5543–5546. [PubMed] [Google Scholar]
- 58.Dai D, Zeldin DC, Blaisdell JA, Chanas B, Coulter SJ, Ghanayem BI, et al. Polymorphisms in human CYP2C8 decrease metabolism of the anticancer drug paclitaxel and arachidonic acid. Pharmacogenetics. 2001;11(7):597–607. doi: 10.1097/00008571-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Totah RA, Rettie AE. Cytochrome P450 2C8: substrates, inhibitors, pharmacogenetics, and clinical relevance. Clin Pharmacol Ther. 2005;77(5):341–352. doi: 10.1016/j.clpt.2004.12.267. [DOI] [PubMed] [Google Scholar]
- 60.Daily EB, Aquilante CL. Cytochrome P450 2C8 pharmacogenetics: a review of clinical studies. Pharmacogenomics. 2009;10(9):1489–1510. doi: 10.2217/pgs.09.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soyama A, Saito Y, Komamura K, Ueno K, Kamakura S, Ozawa S, et al. Five novel single nucleotide polymorphisms in the CYP2C8 gene, one of which induces a frame-shift. Drug Metab Pharmacokinet. 2002;17(4):374–377. doi: 10.2133/dmpk.17.374. [DOI] [PubMed] [Google Scholar]
- 62.Hichiya H, Tanaka-Kagawa T, Soyama A, Jinno H, Koyano S, Katori N, et al. Functional characterization of five novel CYP2C8 variants, G171S, R186X, R186G, K247R, and K383N, found in a Japanese population. Drug Metab Dispos. 2005;33(5):630–636. doi: 10.1124/dmd.105.003830. [DOI] [PubMed] [Google Scholar]
- 63.Nakajima Y, Yoshitani T, Fukushima-Uesaka H, Saito Y, Kaniwa N, Kurose K, et al. Impact of the haplotype CYP3A4*16B harboring the Thr185Ser substitution on paclitaxel metabolism in Japanese patients with cancer. Clin Pharmacol Ther. 2006;80(2):179–191. doi: 10.1016/j.clpt.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 64.Saito Y, Katori N, Soyama A, Nakajima Y, Yoshitani T, Kim SR, et al. CYP2C8 haplotype structures and their influence on pharmacokinetics of paclitaxel in a Japanese population. Pharmacogenet Genomics. 2007;17(7):461–471. doi: 10.1097/FPC.0b013e32805b72c1. [DOI] [PubMed] [Google Scholar]
- 65.Mao X, Bigham AW, Mei R, Gutierrez G, Weiss KM, Brutsaert TD, et al. genomewide admixture mapping panel for Hispanic/Latino populations. Am J Hum Genet. 2007;80(6):1171–1178. doi: 10.1086/518564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Perera MA, Gamazon E, Cavallari LH, Patel SR, Poindexter S, Kittles RA, et al. The missing association: sequencing-based discovery of novel SNPs in VKORC1 and CYP2C9 that affect warfarin dose in African Americans. Clin Pharmacol Ther. 2011;89(3):408–415. doi: 10.1038/clpt.2010.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lane S, Al-Zubiedi S, Hatch E, Matthews I, Jorgensen AL, Deloukas P, et al. population pharmacokinetics of R- and S-warfarin: effect of genetic and clinical factors. Br J Clin Pharmacol. 2012;73(1):66–76. doi: 10.1111/j.1365-2125.2011.04051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li-Wan-Po A, Girard T, Farndon P, Cooley C, Lithgow J. Pharmacogenetics of CYP2C19: functional and clinical implications of a new variant CYP2C19*17. Br J Clin Pharmacol. 2010;69(3):222–230. doi: 10.1111/j.1365-2125.2009.03578.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.