Patients' comfort with and desire to discuss cancer costs exceed those of oncologists, suggesting a need to educate oncologists on this important topic.
Abstract
Purpose:
Recent publications have promoted physician-patient communication on cost as a means of decreasing overall spending and minimizing patients' financial burden in oncology. No study has assessed patients' perspectives on cost communication in oncology. We sought to describe oncology patients' attitudes toward cost communication, explore potential predictors for patients' communication preferences, and assess how patients with cancer consider cost when making management decisions.
Methods:
A 31-item questionnaire was developed to measure oncology patients' communication preferences regarding the cost of cancer care, focusing on out-of-pocket costs. Items were adapted from other instruments when possible. After piloting, patients were recruited from an academic ambulatory oncology practice. Basic descriptive statistics were applied.
Results:
Of the 771 patients approached, 256 responded (response rate, 33%). Most (68%) preferred to know about out-of-pocket costs before treatment. A majority (59%) wanted their physician to discuss these costs with them. Although 76% reported feeling comfortable discussing cost with their physician, 74% were amenable to discussing cost with someone other than their physician. Most patients did not consider out-of-pocket costs (57%) or the health care costs of the country (61%) in their decision making, nor did they believe their physician should (55%). Patients receiving active chemotherapy were less likely to want to discuss out-of-pocket costs with their physician (P = .035).
Conclusion:
Patients' comfort with and desire to discuss cancer costs exceed that of oncologists, suggesting a need to educate oncologists on this important topic. A patient's desire to understand treatment-associated cost does not equate with a desire for cost to influence medical decision making.
Introduction
Technologic advances have led to substantial progress in cancer detection, prevention, and treatment, resulting in reduced cancer-specific mortality. These advancements, however, have also contributed significantly to the rapidly rising health care costs that affect both individual patients and society at large. Cancer care accounted for an estimated $104.1 billion in medical expenditures in the United States in 20061 and increased to $124.6 billion in 2010.2 In 2007, 40% of Medicare drug spending was attributed to drugs prescribed by oncologists,3 and by 2020, the National Institutes of Health estimate that cancer costs will total more than $200 billion.4 As the US population ages, these costs are predicted to increase substantially.
Recent publications, including the 2009 American Society of Clinical Oncology cost of cancer care guidance statement,5 have promoted physician-patient communication on cost as a means of decreasing overall spending and minimizing patients' financial burden. Financial discussions between patients and their oncologists have the potential to affect not only the cost of care but also cancer outcomes and patient satisfaction. Patient preferences regarding cost communication are currently unknown. Thus evidence to guide oncologists' approach to such discussions is needed.
Studies show that most oncologists feel uncomfortable and ill equipped to lead cost discussions.6,7 A substantial minority of oncologists argue further that cost discussions may complicate and even compromise the physician-patient relationship.6,8 Research involving primary care patients suggests that a majority of patients want to discuss out-of-pocket costs with their internists.9 However, this finding may not extend to patients with cancer. In fact, studies suggest that some patients with cancer place greater value on treatments than do the general public and their health care providers.10–12 They may also prefer to discuss sensitive topics with someone other than their oncologist.13
To date, no data exist on preferences of patients with cancer regarding cost communication. In this study, we sought to describe patients' attitudes toward discussing cancer costs with their oncologist, assess how patients consider cost when making management decisions in oncology, and explore possible associations between patient characteristics and their communication preferences.
Methods
Survey Development
This cross-sectional descriptive pilot study was designed to assess communication preferences among a cohort of outpatient oncology patients diagnosed with solid tumor malignancies using a unique self-administered questionnaire. When possible, items were adapted from relevant, previously validated instruments.6,9,14 The survey instrument consisted of 31 items covering several domains, including: patient demographics, socioeconomic status, cancer diagnosis, health insurance coverage, personal experience with cancer treatment, communication preference, extent of cost burden related to cancer care, and influence of cost on medical decision making. A majority of questions regarding cost communication focused specifically on out-of-pocket costs. Respondents were also invited to provide optional written comments. The survey was piloted by six oncology nurses, 10 oncology physicians, and 17 oncology patients and adapted based on their feedback. Approval to administer the survey was obtained from the hospital internal review board.
Survey Administration
All patients scheduled to see a medical oncologist specializing in solid tumor malignancies at Beth Israel Deaconess Medical Center in Boston, Massachusetts, during February 2010 were asked to participate. When checking in for their appointment, patients were provided with a cover letter inviting their participation and explaining the goals of the study. Those who agreed to participate were then asked to complete the questionnaire during the visit and return it to a locked collection box in the clinic waiting room. Participants were asked to complete the questionnaire only once.
Participants were also asked to provide optional written informed consent for a limited medical record review. If permission was granted, the investigators reviewed the medical record for accurate cancer staging information and treatment history.
Analytic Strategies
Primary and secondary end points.
The primary objective was to obtain descriptive data regarding patients' attitudes toward communication about cost of cancer care. The secondary objective was to explore predictors of patients' communication preferences with regard to out-of-pocket costs.
Sample size and power.
We aimed to enroll a convenience sample of 250 participants to capture a broad range of tumor diagnoses as well as time since diagnosis, thereby providing a representative sample of patients with cancer in our academic oncology practice. Statistical analysis further supported an accrual goal of 250 patients. On the basis of a review of monthly clinical activity, the estimated eligible patient population was approximately 2,000 patients over a 2-month period. Subsequent sample size calculations revealed that between 235 and 322 patients would be required to demonstrate 5% to 6% CIs with 95% certainty. Assuming a recruitment rate of 10% to 15%, we anticipated accrual of 250 participants within an 8-week period.
Statistical Considerations
The primary aim of the study was to present descriptive data regarding oncology patients' preferences for discussing cancer costs, with a majority of questions focusing on out-of-pocket costs. Basic descriptive statistics were applied, including frequencies, medians, and proportions. We evaluated associations between responses using simple frequencies and evaluated the bivariate relationships between survey items using cross tabulations. Given that the primary outcome of interest was descriptive cross-sectional data, missing data were censored.
The secondary aim of the study was to explore associations between patients' communication preferences regarding out-of-pocket costs and other measured factors including demographics, experience with cancer, and cost burden. A single Likert scale item served as the dependent variable: “I would like my doctor to talk with me about my out-of-pocket costs when he/she recommends a cancer test or treatment.” Independent variables were represented by the remaining items in the survey. Bivariate analyses were performed using the Fisher's exact test statistic to identify factors associated with patients' preferences for cost communication. The P value was set at less than .05.
Results
Study Population
Of 771 patients approached for study participation in the outpatient oncology unit at Beth Israel Deaconess Medical Center, 256 returned questionnaires, for a response rate of 33%. Recruitment, which was planned for 8 weeks, was stopped after 3 weeks because the targeted sample size had been obtained. Respondent demographics are listed in Table 1. Consent for the limited medical record review was provided by 171 participants (64%).
Table 1.
Patient Demographic and Clinical Characteristics
| Characteristic | % of Patients |
|---|---|
| Age, years | |
| Median | 59 |
| Range | 22-84 |
| Sex | |
| Female | 63 |
| Male | 37 |
| Time since diagnosis | |
| < 3 months | 5 |
| 3-6 months | 12 |
| 6-12 months | 12 |
| 1-2 years | 17 |
| 2-5 years | 24 |
| > 5 years | 29 |
| Cancer type | |
| Breast | 36 |
| GI | 15 |
| Genitourinary | 16 |
| Lung | 10 |
| Gynecologic | 9 |
| Other (lymphoma, melanoma, sarcoma) | 13 |
| Currently undergoing chemotherapy | |
| Yes | 42 |
| No | 58 |
| Ethnicity | |
| White | 87 |
| Black/African American | 6 |
| Asian | 2.5 |
| Other | 4.5 |
| Education | |
| Some high school or less | 2 |
| High school diploma or GED | 18 |
| Vocational degree or some college | 18 |
| College degree | 27 |
| Professional or graduate degree | 35 |
| Annual income, $ | |
| < 24,999 | 12 |
| 25,000-49,999 | 13 |
| 50,000-74,999 | 17 |
| 75,000-99,999 | 12 |
| 100,000-249,999 | 23 |
| > 250,000 | 9 |
| Employment status | |
| Full time | 34 |
| Part time | 15 |
| Unemployed | 10 |
| Retired | 26 |
| Disabled | 9 |
| Medical leave of absence | 4 |
| Respondent has left job since diagnosis | |
| Yes | 30 |
| No | 70 |
| Family member has left job since diagnosis | |
| Yes | 10 |
| No | 90 |
| Respondent is primary wage earner in household | |
| Yes | 46 |
| No | 50 |
| Insurance coverage | |
| Medicare only | 2 |
| Medicare with supplemental | 24 |
| Private or employer based | 65 |
| Medicaid or Mass Health | 6 |
| Uninsured | 2 |
| Prescription drug coverage | |
| Yes | 87 |
| No | 11 |
| Stage at survey* | |
| Surveillance without active disease | 34 |
| Undergoing treatment for localized disease | 14 |
| Metastatic or recurrent disease | 52 |
Abbreviation: GED, general equivalency diploma.
Based on the 171 patients who allowed medical record review.
Communication Preferences
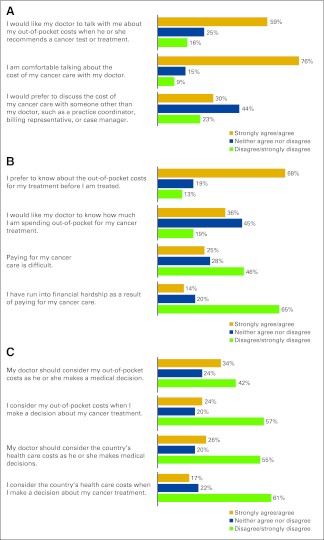
Responses regarding communication preferences are shown in Figure 1A. A majority of respondents (59%) wanted to discuss out-of-pocket costs with their physician, and an even greater majority (76%) was comfortable discussing cancer costs with their physician. A substantial minority of respondents (30%) preferred to discuss costs with someone other than their physician. Of those who did not wish to discuss cost with their physician, 50% expressed a preference to do so with someone other than their physician (P = .039).
Figure 1.
Responses regarding (A) communication preference, (B) cost burden, and (C) influence of cost on medical decision making.
Cost Burden
One fourth of respondents agreed that paying for their cancer care was difficult, and 14% reported financial hardship as a result (Fig 1B). Twenty-nine percent reported having to make sacrifices as a result of paying for their cancer care. Examples included: forgoing vacations, paying bills late, missing mortgage or college tuition payments, not taking medications as prescribed, and omitting alternative therapies. Reporting financial hardship or burden did not influence out-of-pocket communication preferences.
Influence of Cost on Decision Making
Participants' preferences regarding how cost should influence decision making are shown in Figure 1C. Most (57%) did not consider out-of-pocket costs in their decision making, and nearly half (42%) did not wish for their physician to consider such costs. However, respondents were more likely to agree that their physician, as opposed to themselves, should consider out-of-pocket costs when making decisions about cancer care (34% v 24%; P < .001). Among those who considered their out-of-pocket costs, 70% also agreed that their physician should consider out-of-pocket costs when making medical decisions.
Similarly, a majority of respondents disagreed with having the health care costs of the country influence individual cancer management decisions. Among the sizable minority in favor of considering national costs, a greater number of respondents agreed that cost consideration should be the physician's responsibility rather than the patient's (26% v 17%, P < .001).
Associations With Communication Preferences Regarding Out-of-Pocket Costs
The only factor significantly associated with a desire to discuss out-of-pocket costs was current chemotherapy use (Appendix Table A1, online only). Participants actively being treated with chemotherapy at the time of survey administration were twice as likely to disagree with the statement, “I would like my doctor to talk with me about my out-of-pocket costs when he/she recommends a cancer test or treatment,” as compared with those not actively undergoing chemotherapy (12% v 23%; P = .035). No other demographic factors were significantly associated with a communication preference, including: sex, ethnicity, education, income, employment status, and insurance status.
Cancer-specific factors, including cancer type and stage, were also investigated. Of the 256 respondents, 171 agreed to a review of their medical record for disease staging and treatment information. Given the broad range of disease types within our sample and potentially conflicting treatment and survival implications of traditional TNM staging among different cancer types, we opted to categorize cancer stage as: localized disease, no evidence of disease, or metastatic/recurrent disease. Defined in this way, staging was not significantly associated with a communication preference about out-of-pocket costs. Patients' perceptions about therapeutic goals, curative versus palliative, and their relation to out-of-pocket cost communication preferences were also investigated, and again no significant differences were identified.
Qualitative Responses
In the qualitative portion of the study, participants were asked to provide additional comments. Representative examples are presented in Table 2. Those in favor of cost discussions highlight a desire for transparency and patient involvement. Those opposed to cost discussions expressed trust in their physician and a desire not to burden the physician.
Table 2.
Qualitative Responses
| Patients Who Do Want to Discuss Cost | Patients Who Do Not Want to Discuss Cost |
|---|---|
| “If/when physicians present options, they should recommend choices 1,2, and 3 based on best care first. Then compare costs with the patient and the risks/benefits of the differences. I may choose my grandchild's education or daughter's health over mine due to cost, but that is my choice.” | “I don't think doctors have to be burdened with discussing health care costs with patients. All I want to discuss with my doctors is my health.” |
| “I underwent IL-2 treatment and was shocked to learn of the cost from a nurse. I think more openness on these costs is important, not only from the point of view of containing health care costs, but also eliminating the stigma of secrecy on costs … . I believe the cost/benefit analysis must include the patient.” | “Doctors should focus on care not cost. Single payer!” |
| “I often wonder about the costs of the tests, exams, etc. Sometimes I feel that tests are given that I don't really need. There may be places to save on health care costs. On the other hand, I am grateful for receiving good care … . I wouldn't mind discussing the costs with my physician and how best to save money.” | “I trust my doctor's judgment and recommendation for treatment. I don't think certain tests or treatments would be ordered unless necessary, so I don't feel the system is abused.” |
| “Knowing the cost of treatment is important, even if the insurance pays for most of it.” | “Money should not dictate treatment.” |
| “Hospitals should voluntarily know and disclose costs, even if all procedures are insured. Patients should control costs by being selective.” | “I do not think it should be the doctor's responsibility to discuss care cost. That is asking too much from a physician. They can inform patients of relative cost, but more specifics should be handled separately.” |
| “I feel people should know the cost of their treatment when they carry employer-based health insurance so that they are not so cavalier about costs to the health care system. Because we don't know, we are not active consumers. We do not pick and choose based on the pros and cons.” |
Abbreviation: IL-2, interleukin-2.
Discussion
Despite recommendations for oncologists to engage their patients in cost discussions, no data exist regarding patient perspectives on cost communication in oncology. Understanding patient attitudes toward cost communication is critical for guiding conversations on this potentially charged topic. In a sample of patients with cancer seen at an academic oncology practice in Massachusetts, we found that a majority felt comfortable discussing out-of-pocket costs with their physician and would welcome financial discussions at the time of diagnosis and treatment recommendations. Patients in our sample demonstrated attitudes similar to those of primary care patients,9 and our data indicate that patients' comfort with this topic far exceeds that of oncologists. As recent surveys show, only a minority of oncologists (37%) report feeling comfortable having cost discussions with their patients.6 Our results should encourage oncologists to engage their patients in cost discussions, recognizing that a majority of patients would likely welcome out-of-pocket cost communication and would willingly participate.
Our data may also provide insight into patients' motivation for discussing cost. Most patients wanted to know about out-of-pocket costs at the time of treatment, but few acknowledged that cost would influence their personal medical decisions or wished for cost to influence their physician's decisions. Even in an environment of mandated health insurance in Massachusetts, one in four patients among our sample reported difficulty in paying for their cancer care, and nearly one in seven had fallen into financial hardship. Despite substantial financial hardship, a majority of patients in our sample did not want cost to influence medical decision making. Instead, patients' motivation for discussing cost likely arises from a desire to be informed. Our data suggest that a patient's desire to understand treatment-associated out-of-pocket costs does not equate to a desire for cost to influence medical decisions, and most patients do not regard cost communication as an avenue for reducing health care spending.
In our study, most patients reported that their out-of-pocket expenses would not influence their decision making. However, a recently published survey of medical oncologists found that 84% make recommendations that are influenced by their patients' out-of-pocket costs,7 highlighting the discrepancies in how physicians and patients approach cost consideration and communication. Interestingly, our study found that those patients who agreed that cost should be considered in decision making were more likely to agree that the physician, as opposed to the patient, should consider such cost. This includes both out-of-pocket costs and costs to society. These data raise important questions about who should bear the burden of cost consideration in oncologic decisions. It is clear that some patients prefer to play a more passive role in medical decision making, and this may include financial considerations as well.15
Our data demonstrate that most patients want to discuss out-of-pocket costs with their oncologist. This, combined with the known financial burden encountered by many when paying for cancer care,16 underscores the importance of this topic and the critical need to address barriers to cost communication. Lack of time and knowledge present two major barriers to effective cost communication between physicians and patients.6,9,17 Results from this study should motivate oncologists to educate themselves about cancer care costs and encourage oncology organizations, such as the American Society of Clinical Oncology, to advance educational efforts in cost communication for their members.18,19 Conceptualizing the discussion about cost as a discussion about financial toxicity may help guide some physicians, who are already skilled at counseling their patients on other potential treatment-related toxicities.
Most patients in our sample were amenable to discussing cost with a nonphysician member of the oncology team. Even among those patients who wanted to discuss their out-of-pocket costs with their physician, a full third preferred to hold such discussions with someone other than their physician. Such a financial expert could provide information on out-of-pocket expenses and potentially help patients and families identify resources for mitigating financial burden. This team member may be less threatening for the minority of patients who were opposed to discussing cost with their oncologist and may improve workflow in a busy clinical practice.
Discussions of cost, however, are intricately tied to discussions of prognosis and the perceived value of diagnostic and treatment modalities. Data have shown that patients' willingness to pay may reflect their perceived benefit of a treatment.20 Ultimately, it is the oncologists' responsibility to educate patients on whether the intent of treatment is curative or palliative and the likelihood of attaining the stated goal. A substantial proportion of patients, however, may not recognize the gravity of their prognosis, and this can lead them to make different, often more costly, choices about treatment. In a recently published study of patients with metastatic non–small-cell lung cancer, most patients misunderstood that the intent of therapy was palliative, not curative.14 However, patients who held an accurate perception of their prognosis were less likely to receive intravenous chemotherapy near the end of life. Only in the context of honest communication about prognosis and the ability of a proposed treatment to provide benefit can patients make an informed decision about the value of a treatment and their own willingness to bear the expense.
One of the purported goals of advocating cost communication in oncology is to control health care spending. Interestingly, we found that the subset of patients who were likely to be driving health care costs up and facing the greatest expenses were less likely to want to discuss cost with their physician. Patients actively being treated with chemotherapy were less likely to want to speak with their physician about cost as compared with those not receiving chemotherapy. One could theorize that patients who are actively being treated for their cancer may fear they will not receive the most effective therapies if they admit to having financial concerns. They may also place higher value on their treatment and prioritize this over other financial considerations.21 Alternatively, patients being treated with chemotherapy may instead prioritize treatment response and symptom management over financial concerns during their physician visit.
To our knowledge, this study was the first of its kind to examine patients' attitudes toward cost communication in oncology. We recognize, however, that our study has several limitations. The study population was self-selected, and results may not reflect the attitudes of nonresponders. Because this was a self-administered questionnaire, there may have been varying interpretations of survey questions. Responses were collected in only 3 weeks and may have been influenced by the political and economic environment at that time, because the study was conducted during vigorous debate regarding the Affordable Care Act of 2010. In addition, the majority of questions on the survey instrument inquired specifically about out-of-pocket costs. Thus, our results may not reflect patients' attitudes toward discussing overall cost of cancer care, which might include market cost of a given chemotherapy agent or costs covered by insurance.
The most important limitation of our study is that our results may not be generalizable to a broad population of patients with cancer. The survey was conducted at an academic medical center in the state of Massachusetts, where health insurance is mandated. Our sample was composed of a relatively affluent, highly educated, and predominantly female population, with more than one third of patients being treated for breast cancer. Nearly 30% of participants were more than 5 years out from their original diagnosis. In contrast, data from the US Census Bureau show the median US household income to be approximately $50,303, with only 28% of Americans holding a college degree or higher.22 Men comprise 52% of all cancer diagnoses in the United States, with breast cancer representing 14% of all cancer diagnoses.23 Although the 5-year relative survival rate for all cancer types reaches 68%, individual survival rates are heavily affected by both type of cancer and stage at diagnosis.23 Thus, our sample likely differs from the overall US population of patients with cancer in important ways. Although we did not identify these demographic or cancer-specific factors to be associated with out-of-pocket cost communication preferences, it will be important to confirm our findings in different sample populations over more lengthy time periods.
In conclusion, we found that the majority of oncology patients within our sample felt comfortable with and wanted to discuss out-of-pocket costs related to cancer care with their physicians. Thus, further education and resources are needed to enable physicians to include cost communication in their oncology practice. Additionally, we found that a majority of oncology patients did not want cost to influence medical decision making, whereas the literature suggests that many oncologists do consider cost when making treatment recommendations. Given this divergence in viewpoints, further research is needed to evaluate how physician-patient communication about cost and the value of cancer care affect not only the overall cost of cancer care but also patient satisfaction and cancer outcomes.
Acknowledgment
We thank G. Caleb Alexander, MD, MS, Deborah Schrag, MD, MPH, and Reed Drews, MD, for their helpful comments and assistance with this study. Supported by Beth Israel Deaconess Medical Center Hematology/Oncology Fellowship Funds. A.J.B. and E.W.H. contributed equally to this work. Presented in poster format at the 47th Annual Meeting of the American Society of Clinical Oncology, June 3-7, 2011, Chicago, IL.
Appendix
Table A1.
Distribution for Participants Responding to Statement: “I Would Like My Doctor to Talk With Me About My Out-of-Pocket Expenses When He or She Recommends a Cancer Test or Treatment.”
| Characteristic | Agree/Neutral (%) | Disagree (%) | P* |
|---|---|---|---|
| Sex | 1.00 | ||
| Female | 84 | 16 | |
| Male | 83 | 17 | |
| Time since diagnosis | .196 | ||
| < 3 months | 83 | 16 | |
| 3-6 months | 80 | 20 | |
| 6-12 months | 80 | 20 | |
| 1-2 years | 74 | 26 | |
| 2-5 years | 85 | 15 | |
| > 5 years | 91 | 9 | |
| Currently undergoing chemotherapy | .035 | ||
| Yes | 77 | 23 | |
| No | 88 | 12 | |
| Ethnicity | .073 | ||
| White | 85 | 15 | |
| Black/African American | 80 | 20 | |
| Asian | 100 | 0 | |
| Education | .270 | ||
| Some high school or less | 60 | 40 | |
| High school diploma or GED | 88 | 12 | |
| Vocational degree or some college | 77 | 23 | |
| College degree | 88 | 12 | |
| Professional or graduate degree | 85 | 15 | |
| Annual income, $ | .544 | ||
| < 24,999 | 83 | 17 | |
| 25,000-49,999 | 81 | 19 | |
| 50,000-74,999 | 86 | 14 | |
| 75,000-99,999 | 80 | 20 | |
| 100,000-249,999 | 91 | 9 | |
| > 250,000 | 77 | 23 | |
| Rather not say | 92 | 8 | |
| Employment status | .586 | ||
| Full time | 83 | 17 | |
| Part time | 87 | 13 | |
| Unemployed | 76 | 24 | |
| Retired | 89 | 11 | |
| Disabled | 77 | 23 | |
| Medical leave of absence | 80 | 20 | |
| Respondent has left job since diagnosis | .338 | ||
| Yes | 81 | 19 | |
| No | 86 | 14 | |
| Family member has left job since diagnosis | .776 | ||
| Yes | 87.5 | 12.5 | |
| No | 84 | 16 | |
| Respondent is primary wage earner in household | 1.00 | ||
| Yes | 84 | 16 | |
| No | 84 | 16 | |
| Insurance coverage | .405 | ||
| Medicare only | 80 | 20 | |
| Medicare with supplemental | 86 | 14 | |
| Private or employer based | 84 | 16 | |
| Medicaid or Mass Health | 87 | 13 | |
| Uninsured | 50 | 50 | |
| Prescription drug coverage | .401 | ||
| Yes | 85 | 15 | |
| No | 78 | 22 | |
| Stage at survey† | .059 | ||
| No active disease | 91 | 9 | |
| Localized disease | 68 | 32 | |
| Metastatic or recurrent disease | 84 | 16 | |
| Cancer type | .271 | ||
| Breast | 89 | 11 | |
| Colon/rectal | 76 | 24 | |
| Esophageal/stomach | 60 | 40 | |
| Kidney | 80 | 20 | |
| Liver/gallbladder | 100 | 0 | |
| Lung | 72 | 28 | |
| Lymphoma | 67 | 33 |
Abbreviation: GED, general equivalency diploma.
Fisher's exact test.
Based on the 171 patients who allowed medical record review.
Authors' Disclosures of Potential Conflicts of Interest
The author(s) indicated no potential conflicts of interest.
Author Contributions
Conception and design: Andrea J. Bullock, Erin W. Hofstatter, Mary K. Buss
Administrative support: Andrea J. Bullock, Erin W. Hofstatter, Mary K. Buss
Provision of study materials or patients: Andrea J. Bullock, Erin W. Hofstatter, Mary K. Buss
Collection and assembly of data: All authors
Data analysis and interpretation: Andrea J. Bullock, Erin W. Hofstatter, Mary K. Buss
Manuscript writing: Andrea J. Bullock, Erin W. Hofstatter, Mary K. Buss
Final approval of manuscript: All authors
References
- 1.National Cancer Institute. Cancer Trends Progress Report 2009/2010—Costs of Cancer Care. http://progressreport.cancer.gov.
- 2.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meropol NJ, Schulman KA. Cost of cancer care: Issues and implications. J Clin Oncol. 2007;25:180–186. doi: 10.1200/JCO.2006.09.6081. [DOI] [PubMed] [Google Scholar]
- 4.National Cancer Institute. Cancer Prevalence and Cost of Care Projections. http://costprojections.cancer.gov/expenditures.html.
- 5.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: The cost of cancer care. J Clin Oncol. 2009;27:3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 6.Schrag D, Hanger M. Medical oncologists' views on communicating with patients about chemotherapy costs: A pilot survey. J Clin Oncol. 2007;25:233–237. doi: 10.1200/JCO.2006.09.2437. [DOI] [PubMed] [Google Scholar]
- 7.Neumann PJ, Palmer JA, Nadler E, et al. Cancer therapy costs influence treatment: A national survey of oncologists. Health Aff (Millwood) 2010;29:196–202. doi: 10.1377/hlthaff.2009.0077. [DOI] [PubMed] [Google Scholar]
- 8.Schrag D. The price tag on progress: Chemotherapy for colorectal cancer. N Engl J Med. 2004;351:317–319. doi: 10.1056/NEJMp048143. [DOI] [PubMed] [Google Scholar]
- 9.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290:953–958. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 10.Aristides M, Chen J, Schulz M, et al. Conjoint analysis of a new Chemotherapy: Willingness to pay and preference for the features of raltitrexed versus standard therapy in advanced colorectal cancer. Pharmacoeconomics. 2002;20:775–784. doi: 10.2165/00019053-200220110-00006. [DOI] [PubMed] [Google Scholar]
- 11.Agrawal M, Grady C, Fairclough DL, et al. Patients' decision-making process regarding participation in phase I oncology research. J Clin Oncol. 2006;24:4479–4484. doi: 10.1200/JCO.2006.06.0269. [DOI] [PubMed] [Google Scholar]
- 12.Weinfurt KP, Castel LD, Li Y, et al. The correlation between patient characteristics and expectations of benefit from phase I clinical trials. Cancer. 2003;98:166–175. doi: 10.1002/cncr.11483. [DOI] [PubMed] [Google Scholar]
- 13.Lamont EB, Siegler M. Paradoxes in cancer patients' advance care planning. J Palliat Med. 2000;3:27–35. doi: 10.1089/jpm.2000.3.27. [DOI] [PubMed] [Google Scholar]
- 14.Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non–small-cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol. 2011;29:2319–2326. doi: 10.1200/JCO.2010.32.4459. [DOI] [PubMed] [Google Scholar]
- 15.Elkin EB, Kim SH, Casper ES, et al. Desire for information and involvement in treatment decisions: Elderly cancer patients' preferences and their physicians' perceptions. J Clin Oncol. 2007;25:5275–5280. doi: 10.1200/JCO.2007.11.1922. [DOI] [PubMed] [Google Scholar]
- 16.Zafar Y, Goetzinger AM, Fowler R, et al. Impact of out-of-pocket expenses on cancer care. J Clin Oncol. 2011;29(suppl):385s. abstr 6006. [Google Scholar]
- 17.Hofstatter EW. Understanding patient perspectives on communication about the cost of cancer care: A review of the literature. J Oncol Pract. 2010;6:188–192. doi: 10.1200/JOP.777002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baile WF, Buckman R, Lenzi R, et al. SPIKES: A six-step protocol for delivering bad news—Application to the patient with cancer. Oncologist. 2000;5:302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 19.McFarlane J, Riggins J, Smith TJ. SPIKE$: A six-step protocol for delivering bad news about the cost of medical care. J Clin Oncol. 2008;26:4200–4204. doi: 10.1200/JCO.2007.15.6208. [DOI] [PubMed] [Google Scholar]
- 20.Wong YN, Hamilton O, Egleston B, et al. Understanding how out-of-pocket expenses, treatment value, and patient characteristics influence treatment choices. Oncologist. 2010;15:566–576. doi: 10.1634/theoncologist.2009-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364:2060–2065. doi: 10.1056/NEJMsb1013826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Census Bureau. The 2011 Statistical Abstract. http://www.census.gov/compendia/statab.
- 23.American Cancer Society. Atlanta, GA: American Cancer Society; 2011. Cancer Facts and Figures 2011. [Google Scholar]