Abstract
Although psychotherapy involves the interaction of client and therapist, mutual influence is not typically considered a source of variability in therapist adherence and competence in providing treatments assessed in clinical trials. We examined variability in adherence and competence in Motivational Enhancement Therapy (MET) both within and between therapist caseloads in a large multi-site clinical trial. Three-level multilevel models (repeated measures, nested within clients, nested with therapists) indicated significant variability both within and between therapists. There was as much and sometimes more variability in MET adherence and competence within therapist caseloads than between therapists. Variability in MET adherence and competence within caseloads was not consistently associated with client severity of addiction at baseline. However client motivation at the beginning of the session and days of use during treatment were consistent predictors of therapist adherence and competence. Results raise questions about the nature of therapist adherence and competence in providing treatment protocols in clinical trials. Accordingly, future analysis of clinical trials should consider the role of mutual influence in measures of therapist performance.
Keywords: Motivational Interviewing, Adherence, Competence, Multilevel Modeling
1.0 Introduction
There is a strong evidence base for the efficacy of Motivational interviewing (MI; Miller and Rollnick, 2002) and its implementation incorporating feedback, Motivational Enhancement Therapy (MET; Miller and Rollnick, 2009; Hettema, et al., 2005; Lundhal et al., 2010). Dozens of clinical trials (see Lundhal et al., 2010) have given way to studies of the process of effective MI. The majority of research examining the mechanisms of MI and MET has involved evaluations of therapist adherence to MI principles and the competence with which these interventions are delivered (Carroll et. al., 2000). There is a growing body of research indicating that the therapist impacts client behaviors in MET (see Miller and Rose, 2009 for a review). However, levels of therapist adherence and competence tend to be variable. More generally, across a variety of treatments and disorders, the relationships between therapist adherence, competence, and clinical outcomes tend to be small (see recent meta-analysis by Webb et al., 2010). As a result, the components of treatment responsible for change remain unclear (Carroll et al., 2006a).
One potential explanation for the lack of predicted relationships between therapist adherence and competence and treatment outcomes is research on the practice of MET is often uni-directional - focusing on how therapist behaviors influence clients. However, MI and MET are based on a theory of interpersonal behavior involving the mutual influence of clients and therapists on each other. Specifically, therapist confrontation and client resistance to change are considered complimentary behaviors that reinforce each other (Miller and Rollnick, 2002; Miller, 2005). Accordingly, a fundamental tenet of motivational interviewing is that client resistance is not merely a client factor, but a dyadic process that occurs “within the context of a relationship or a system” (Miller and Rollnick, 2002, p.46). MI and MET are designed to promote client motivation by training therapists to resist the tendency to respond to client resistance with confrontation by maintaining an empathic stance and strategically eliciting client statements in favor of change (Hartzler et al., 2009; Miller and Rose, 2009). The purpose of the current paper is to provide an initial test of the hypothesis that therapist adherence and competence in providing MET is partially determined by the mutual influence of therapists and clients on each other.
If therapists are influenced by client behaviors, there are two and opposite models for conceptualizing the direction of the effect. One hypothesis, suggests that therapist adherence and competence may be negatively impacted by more difficult clients. For example, clients with high psychiatric severity may negatively impact ratings of therapist adherence by decreasing the extent to which therapists can engage in motivational strategies such as making plans for change and pro/con lists. Similarly, the complexity of working with patients with more psychiatric problems may result in decreased ratings of therapist competence. It is also possible that clients who present as more resistant elicit MI-inconsistent behaviors from therapists such as confrontation (Francis et al. 2005). Alternatively, the second and rival hypothesis, consistent with the goals of training therapists in MI, posits that difficult or resistant behaviors on the part of clients should elicit greater use of MI strategies among therapists. A core goal of training in MI is to teach therapists to not reciprocate client resistance with confrontation (Miller and Rollnick, 2002). Analyses that examine how and to what extent therapists trained in MET might respond with behaviors consistent or inconsistent with MET by different clients may further clarify the mechanisms of action responsible for client change, as well as lead to improved training procedures related to working with challenging clients. The influence of clients on therapist adherence and competence may be particularly important for client outcomes, as certain client behaviors could encourage the very therapist behaviors that MET views as working against a goal of reduced substance use.
We are not aware of any research addressing the potential impact of clients on therapist MET competence. However, there is some evidence supporting the first hypothesis that client difficulty decreases therapist adherence in providing MET. Francis and colleagues (2005) found that therapists who provided treatment to highly resistant confederate clients were independently rated as more confrontational than those working with less resistant clients. However, these therapists had not yet been trained in MI or MET. Similarly, a sequential analysis of therapist and client utterances indicated that client change talk is more likely to be followed by MI-consistent responses from therapists (Moyers and Martin, 2006). Continued client substance use during treatment may also influence therapist use of MI. Thryian and colleagues (2007) found that clients who had stopped smoking were 3 times more likely to receive a higher quality MI session as compared to those who were daily smokers. In contrast and consistent with the second hypothesis that therapists will not be drawn into MET inconsistent behaviors by client resistance, an analysis of process data from Project MATCH (Carroll et al., 1998) and the multisite Marijuana Treatment Project (Gibbons et al., 2010) indicated that continued substance use during treatment was associated with greater use of MET techniques.
In sum, theory and preliminary research suggests clients may influence therapist adherence and competence in providing MET. However, there are few studies in this area and the direction of effects remains unclear.
The social relations model (SRM; Kenny et al., 2006) provides a framework for partitioning sources of variability in interpersonal interactions such as therapist adherence and competence. The SRM posits that interpersonal behavior can differ as a result of three main components: 1) the actor, 2) the partner, and 3) the relationship. In psychotherapy, this translates to 1) client, 2) therapist, and 3) relationship or dyad components. Psychotherapy clinical trials are typically nested in structure wherein one therapist treats several different clients, but clients receive treatment from only one therapist. Nested designs allow the researcher to disentangle sources of variability in a target behavior (e.g., therapist adherence) into therapist components (i.e., between therapist differences) as well as patient and relationship components (i.e., differences between clients within therapist caseloads). The between therapist component is a measure of consensus – the similarity of ratings of adherence and competence for a given therapist. High levels of consensus indicate that some therapists were more adherent and competent than others across clients in their respective caseloads. The patient and relationship component is a measure of uniqueness – do clients experience different amounts of adherence and competence with their therapists? Differences between clients within a therapist’s caseload may be the result of characteristics unique to the client or the relationship of a given client with a therapist. Round robin designs, in which clients are treated by multiple therapists, are necessary to separate relationship effects from client effects, and are typically unfeasible in applied clinical studies. The structure of current data in which clients are nested or clustered within therapists allows for the partitioning of adherence and competence into between and within therapist components and provides an indication of the extent to which adherence and competence are determined by therapists as well as factors unique to either clients or their relationship with clients (see Marcus et al., 2009; Raudenbush and Bryk, 2002).
If therapist adherence and competence are the product mutual influence, then we would expect relatively high levels of variability in adherence and competence within a therapist's caseload. However, if a therapist's adherence and competence in providing MET is primarily driven by the therapist, variability in these measures within caseloads should be negligible.
In the current paper, we analyzed data from a large multi-site study of substance use treatment to examine if therapist adherence and competence in providing MET is variable within therapist caseloads and impacted by client behaviors. We hypothesized that adherence and competence in providing MET will vary within therapist caseloads (Hypothesis 1). Given mixed findings in prior literature, we further evaluated two rival hypotheses (2a and 2b) with respect to the relationships between client difficulty (e.g., substance use, motivation, other severity indicators), both at baseline and during treatment and ratings of therapist adherence to MET. Based on the interpersonal theory on which MET is based, 2a predicts that client difficulty will be associated with less adherence. However, consistent with the goals of MET training, 2b predicts that client resistance will be associated with greater adherence to MET protocols. Given the absence of prior research regarding the effects of clients on therapist competence, we regarded analyses of client indicators of resistance on therapist competence as exploratory.
2.0 Method
We analyzed data from a large multi-site randomized clinical trial that compared three sessions of MET to three sessions of counseling as usual for substance abuse (Ball et al., 2007). As the focus of the analysis dealt with adherence and competence to MET, only the MET condition was included in the analysis. Details regarding study design, exclusion and inclusion criteria, participant characteristics, and training of therapists are available in previous publications (Ball et al., 2002; Ball et al., 2007; Martino et al., 2008; Santa Ana et al., 2009).
2.1 Participants
The initial study included 461 randomized participants who reported mixed substance use problems (29% alcohol, 23% cocaine, 16% marijuana, 9% opiates, 4% methamphetamines, 11% alcohol and drug, and 8% other). Ratings of adherence and competence in providing MET were obtained on a randomly selected set of sessions from the clients who completed all three treatment sessions (see Martino et al., 2008, for description of sampling strategy and rating system). Additional tapes were rated in order to ensure that every therapist had a least one session rated. The data for the primary analyses included ratings of 194 session tapes for 79 clients and 12 therapists. There were an average of 2.46 (SD=0.78) sessions rated per client, 66% of clients had three sessions rated, 14% had two sessions rated, and 20% had only one session rated. These clients had a mean age of 34.5 (SD=10.5) years and were 73% male, 46% Caucasian, 39% African American, 10% Hispanic American, and 2% multiracial. Exact samples sizes varied across measures in large part because a competence rating (i.e., skill demonstrated when technique present) was made only when a specific technique was used.
Therapists were 12 clinicians who saw at least two clients (one therapist who saw only one client was excluded) at participating community treatment programs who were randomized to be trained and supervised in MET. The average number of clients treated by each therapist ranged from a low of 2 to a high of 13 (mean = 6.58, SD = 3.61). Most therapists reported no previous experience with MI or MET or use of therapy manuals (Ball et al., 2002).
2.2 Treatment
Therapists provided three study sessions of approximately 45–55 minutes. MET therapists followed a manual developed by Farentinos and Obert (2000) which was adapted from Miller et al.’s (1992) Project Match MET Manual, and received ongoing biweekly supervision from program supervisors after initial certification, based on review of their session tapes, rating-based feedback, and coaching. The manual encouraged therapists to use client-centered communication skills, suggested methods for handling resistance, and provided more strategic skills for eliciting and reinforcing client change talk.
2.3 Measures
2.3.1 Adherence and Competence
MET sessions were audiotaped. Fifteen independent raters were trained to code tapes. The coding protocol - the Independent Tape Rater Scale (ITRS: Martino et al 2008) was adapted from several instruments, including the Yale Adherence and Competence Rating System (Carroll, et al., 2000). Ten items asked about MI skills and resulted in two subscales: (a) fundamental, and (b) advanced (Martino et al., 2008) for both adherence and competence (7 point Likert scale; adherence, 1 = not present to 7 = extensively; competence; 1 = very poor to 7 = excellent). Raters were asked to code the frequency or extensiveness of particular interventions in the session and also the quality or skillfulness. The fundamental MET subscale included behaviors such as fostering collaboration, positive affirmations, and general motivational interviewing style. Advanced MET behaviors included problem discussion and feedback, enhancing motivation, and building a plan for change. In the current sample, the inter-rater reliability of these scales was quite high, ranging from .89 to .95. Fundamental and advanced MET adherence (frequency) ratings were highly correlated (r = .78) while fundamental and advanced competence (skillfulness) ratings were more modestly related (.39) (Martino et al., 2008).
An additional 10 items comprised a subscale that assessed the presence of therapist behaviors inconsistent or antithetical to MET (e.g., confrontation of denial, therapeutic authority) or typical of treatment approaches different from MET (e.g., skills training, psychodynamic). The adherence and competence of therapists provision of MET-inconsistent behaviors was rated in a similar manner to MET fundamental and advanced strategies.
2.3.2 Beginning of session motivation
Raters coded a client's stage of motivation at the beginning of each session on a 7-point scale. Each one point increment in the item rating was indicative of a relative change in the balance of client change talk and resistant statements such that a score of 1 indicated very little change talk and very strong resistance and a 7 represented strong motivation for change as evidenced by almost all change talk and very little resistance. Ratings were based on an independent rating of the first five minutes of each session (Martino et al. 2008).
2.3.3 Addiction Severity Index (ASI)
We used several subscales from a brief version of the ASI (McLellan et al., 1992) administered as baseline indicators of substance-related psychosocial problems. This structured interview has been used extensively in substance abuse treatment research with excellent psychometric support (Alterman et al., 1994, 2001). The brief version used in the CTN eliminated some questions which were collected elsewhere in the assessment battery and/or not used in the calculation of composite scores (Carroll et al, 2006b).
2.3.4 Days of any substance use during treatment
Client reported days of any substance use during each of the four weeks of treatment was measured using the Substance Use Calendar which is an interview of self-reported substance use based on the Time Line Follow-Back interview (Sobell and Sobell, 1992). Scores ranged from 0 to 28 and were positively skewed (50% of the sample with complete data reported 0 days of substance use during treatment).
2.4 Data Analysis
We tested hypothesis 1 and 2 using multilevel models that provided estimates of variability in adherence and competence in performing MET across 194 session tapes for 79 clients and 12 therapists (exact n’s varied across measures of adherence and competence). Multilevel models are appropriate when data are nested (e.g., students in classrooms or repeated measures in individuals) and can model individual change in the presence of missing data (Singer and Willet, 2003). The current data is nested in structure and, as analyzed, contains three levels: repeated measures (sessions 1, 2, or 3; level 1) nested within clients (level 2), and clients are further nested within therapists (level 3). Both clients and therapists were treated as random effects. Client variation within therapists is found at level 2 and variation between therapists is found at level 3 (Raudenbush and Bryk, 2002). Estimates of the difference between clients within therapists (level 2) are necessarily an amalgam of client and relationship or dyad variability. For ease of presentation we refer to variability at level 2 as ‘within therapist’ variability. Data was analyzed with Hierarchical Linear Modeling (HLM6) (Raudenbush et al., 2005).
As an initial test we examined the possibility of growth in adherence or competence over time by entering session number into the model at level 1. Session was not a significant predictor of any measure of adherence or competence, thus there was no evidence of linear change in use of MET over time. Accordingly, session number was dropped from all future models.
As a test of our initial hypothesis (hypothesis 1) that there would be within therapist variability in adherence and competence in providing MET, we constructed the first set of models which decomposed variation in MET adherence and competence into within and between therapist components. The equation was as follows:
where Yijz is the predicted adherence or competence rating at session i, for client j, treated by therapist z; β00 is the intercept; R0 is the within therapist variance ; U00 is the between-therapist variance ; and E is the variance in repeated measures . Coefficients inside the brackets are the random effects and coefficients outside the brackets are the fixed effects. Based on these variance components, we computed both the percentage of variation in repeated measures of adherence and competence that is within therapists and between therapists (see Raudenbush and Bryk, 2002).
Next, we tested our second set of hypotheses that client behavior at baseline, as measured by the ASI, and client behavior during treatment, as measured by client motivation at the beginning of the session and days of substance use during treatment, would predict adherence and competence in providing MET. Client motivation was rated at the beginning of every session and thus was entered into the model at level 1 (repeated measures). Baseline symptoms and days of use during treatment were client level variables that did not vary over the course of treatment. Accordingly, we entered these variables as predictors of adherence and competence at level 2 – the client level.
3.0 Results
3.1 Within and Between Therapist Effects
Table 1 provides the means across sessions on each measure of MET adherence and competence. Table 2 provides the fixed and random effects for each measure of MET frequency and competence. The between therapist variance components in Table 2 test if therapists were a source of variability in adherence and competence (i.e., there were differences between therapists) and the within therapist variance components test if clients and/or dyads were a source of variability in adherence and competence (i.e., there were differences in adherence and competence between clients within a therapists caseload). The between therapist variance components (τc00) for fundamental and advanced adherence, as well as advanced competence and MET-inconsistent adherence were significantly different from zero. In addition, the within therapist variance components (τb00) for fundamental adherence as well as fundamental, advanced, and MET-inconsistent competence were significantly different from zero (see Table 2). Generally, this provides support for hypothesis 1. Hence, there was significant variation in adherence and competence both within and between therapists. The variance in repeated measures accounted for within therapists ranged from 3 to 25% (m = 14% across measures). The variance accounted for between therapists also varied widely from 3 to 32% (m = 13% across measures).
Table 1.
Means, standard deviations, and samples sizes for each measure of adherence and competence.
| Mean (sd) | ||
|---|---|---|
| Fundamental MET Skills | ||
| Adherence | 4.37 (0.98) | |
| N=190 | ||
| Competence | 4.85 (0.79) | |
| N=194 | ||
| Advanced MET Skills | ||
| Adherence | 2.64 (0.83) | |
| N=192 | ||
| Competence | 4.78 (0.67) | |
| N=188 | ||
| MET Inconsistent Strategies | ||
| Adherence | 1.63 (0.84) | |
| N=192 | ||
| Competence | 4.38 (0.63) | |
| N=108 | ||
Table 2.
Fixed and Random effects for 3-level model partitioning variability in adherence and competence.
| Fixed Effects | Random Effects | ||||||
|---|---|---|---|---|---|---|---|
| Intercept β00 | Residual | Within Therapist τb00 |
Between Therapist τc00 |
Within Therapist % |
Between Therapist % |
||
| Fundamental MET | |||||||
| Adherence (n=190) | 4.34*** | 0.75 | 0.12** | 0.10** | 0.14 | 0.12 | |
| Competence (n=194) | 4.83*** | 0.44 | 0.15*** | 0.01 | 0.25 | 0.02 | |
| Advanced MET | |||||||
| Adherence (n=192) | 2.58*** | 0.57 | 0.02 | 0.08*** | 0.03 | 0.13 | |
| Competence (n=188) | 4.72*** | 0.34 | 0.04* | 0.06*** | 0.11 | 0.17 | |
| MET Inconsistent Strategies | |||||||
| Adherence (n-192) | 1.71*** | 0.47 | 0.05 | 0.22*** | 0.09 | 0.32 | |
| Competence (n=108) | 4.36*** | 0.29 | 0.07* | 0.01 | 0.19 | 0.03 | |
Note. The sample sizes mostly varied because competence is not rated if items comprising competence scores did not occur. The sample sizes ranged from a minimum of 108 for advanced MET competence and a maximum of 194;
<.05;
<.01;
<.001.
Within therapist % denotes the percentage of variability in a given outcome at the client level or within therapists. Between therapist % denotes the percentage of variability in a given outcome at the therapist level or between therapists.
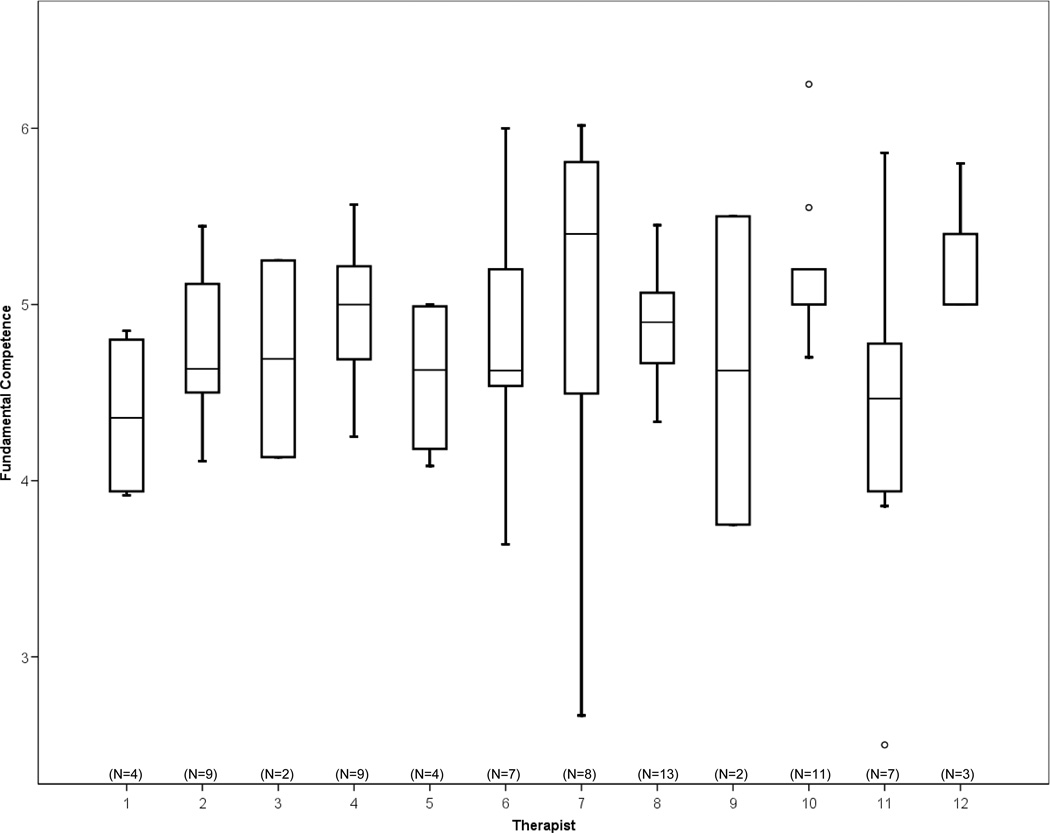
Some differences in percent of variance accounted for between and within therapists were notable. Twenty-five and 19% of the variability in fundamental and MET-inconsistent competence was within therapists, while therapists accounted for 2–3% that was not significantly different from zero. As an illustration, Figure 1 provides box plots of the variability in fundamental competence within each therapist’s caseload. An inspection of Figure 1 indicates relatively little difference between therapists in the average levels of competence, but notable variability within some therapist’s caseloads. In contrast, thirty-two percent of the variability in therapist use of MET-inconsistent strategies was attributable to therapists, while only 9% was within therapists.
Figure 1.
Box plots for each therapist illustrating the variability in fundamental competence within and between each therapist’s caseload.
3.2 Effects of Baseline ASI
To test our second set of hypotheses, we entered baseline ASI medical, family/social, employment, alcohol, drug, legal, and psychiatric composite scores as predictors of adherence and competence at the client level (level 2). There were few significant correlations. However, consistent with hypothesis 2a, the psychiatric composite was a significant predictor of advanced adherence, β01 = −0.64, p = .02, indicating that as psychiatric severity increased at pre-treatment therapists provided MET advanced skills less frequently. In addition, the family/social composite was a negative predictor of fundamental adherence, β01 = −0.54, p = .04, and advanced competence, β01 = −0.54, p = .04, indicating that as family/social problems increased therapist provided less fundamental MET skills and were rated as performing advanced skills less competently. Finally, and consistent with hypothesis 2b, the pre-treatment legal composite was a positive predictor of fundamental adherence, β01 = 1.12, p = .01, indicating that as legal involvement increased, therapist use of fundamental MET skills increased. No other ASI variable was a significant predictor of any other adherence or competence rating.
3.3 Effects of Motivation at the Beginning of Session and Days of Use during Treatment
Regarding the effect of client behavior during treatment, we entered motivation and days of use as predictors of adherence and competence. Beginning of session motivation was a significant predictor of three of the four measures that demonstrated significant variability within therapists. Consistent with hypothesis 2b, motivation at the beginning of the session was a negative predictor of fundamental and advanced adherence, indicating that when a client’s motivation at the beginning of the session was lower, counselor adherence to MET during the session was higher. In addition, motivation at the beginning of the session was a positive predictor of MET-inconsistent competence, suggesting that as client motivation increased therapists were rated as more skilled at the MET-inconsistent interventions that they used (see Table 3).
Table 3.
The effect of beginning of session motivation on adherence and competence.
| Fixed Effects | Random Effects | |||||||
|---|---|---|---|---|---|---|---|---|
| Intercept β00 | Beginning of Session Motivation β01 |
Residual | Within Therapist τb00 |
Between Therapist τc00 |
Within Therapist % |
Between Therapist % |
||
| Fundamental MET | ||||||||
| Adherence (n=190) | 4.95*** | −0.14* | 0.75 | 0.10* | 0.10** | 0.12 | 0.12 | |
| Competence (n=194) | 4.59*** | 0.05 | 0.44 | 0.15*** | 0.01 | 0.25 | 0.02 | |
| Advanced MET | ||||||||
| Adherence (n=192) | 3.23*** | −0.14** | 0.57 | 0.006 | 0.09*** | 0.01 | 0.14 | |
| Competence (n=188) | 4.34 | 0.09 | 0.34 | 0.04 | 0.06*** | 0.11 | 0.15 | |
| MET Inconsistent Strategies | ||||||||
| Adherence (n-192) | 2.01*** | −0.07 | 0.46 | 0.04 | 0.23*** | 0.08 | 0.33 | |
| Competence (n=108) | 3.70*** | 0.15* | 0.31 | 0.05 | 0.01 | 0.14 | 0.03 | |
Note. The sample sizes mostly varied because competence is not rated if items comprising competence scores did not occur. The sample sizes ranged from a minimum of 108 for advanced MET competence and a maximum of 194;
<.05;
<.01;
<.001.
Within therapist % denotes the percentage of variability in a given outcome at the client level or within therapists. Between therapist % denotes the percentage of variability in a given outcome at the therapist level or between therapists.
Finally, we tested the effect of days of any substance use during treatment on therapist adherence and competence. Consistent with hypothesis 2a, the effect of days of use was negative and significant for fundamental adherence, β01 = −0.03, p = .004, and competence, β01 = −0.02, p = .009, as well as advanced adherence, β01 = −0.03, p = .003, and MET-inconsistent competence, β01 = −0.02, p = .024. The effect of days of any substance use on advanced competence and MET-inconsistent adherence were not significant. Given the skewed distribution of days of any use during treatment variable and the presence of several extreme observations (i.e., 50% of the sample report no substance use during treatment, but 5 patients reported using substances every day or nearly every day), we repeated this analyses with these extreme observations removed from the analysis. When these individuals were removed there were no significant effects of days of use on any measure of adherence or competence.
4.0 Discussion
We used multilevel modeling techniques to examine the mutual influence of clients and therapists in MET adherence and competence over three sessions in a multi-site trial of community-based substance abuse treatment. As has been demonstrated in previous studies (Carroll et al., 2006), therapists differed in the extent to which they were rated as adherent and competent. In addition, the extent to which therapists were adherent to and competent in providing MET varied across clients within their caseloads. For example, the data showed that some therapists used strategies to build motivation for change with more competence than others, but therapists’ competence in using these strategies also varied among the clients they had seen.
Estimates of variability differed widely between and within therapists in adherence (e.g., fundamental [14 vs. 12%], advanced [3 vs. 13%], and MET-inconsistent [9 vs. 32%]) and competence (e.g., fundamental [26 vs. 2%], advanced [11 vs. 17%], and MET-inconsistent [19 vs. 3%]). This suggests that while some observer rated measures of therapist behavior may be highly variable across clients within a caseload, others may be relatively stable. Indicators with large between therapist components such as MET-inconsistent adherence may be important targets for supervision - it appears that some therapists consistently used these skills more than others. Yet it also appears that many observer rated measures of adherence and competence are as much a state that is influenced by the clients whom they are treating as they are a stable therapist trait.
For example, ratings of therapist competence varied significantly within therapist caseloads, most notably for competence in fundamental MI skills. This indicates that the skill with which a therapist maintained a motivational interviewing style may depend on certain client or client/therapist dyad factors. It may be that all therapists would perform poorly with a given client who is extremely difficult, whereas other clients may elicit poor performance with only certain therapists. In contrast, there appeared to be large differences between MET therapists in the extent to which they utilized MET-inconsistent strategies, and the use of these strategies varied little within therapist caseloads. Consistent with studies of training MI skills (Miller et al, 2004; Baer et al, 2009), our data suggest that MI training may have been relatively less successful in reducing the degree to which some therapists utilize MI-inconsistent interventions.
We sought to account for within therapist variability in adherence and competence with measures reflecting individual differences in clients' motivation and addiction severity. Results provided mixed support for both hypothesis 2a and 2b. Lower client motivation for change at the beginning of the session predicted increased use of MET fundamental and advanced skills, but increased competence in the use of MET-inconsistent skills. This finding is consistent with the goals of MET in that it may be that therapists respond appropriately to clients who have lower motivation by increasing their use of MET strategies such as listening reflectively and using open questions. Similarly, clients with more motivation may influence therapists to move on to other, non-MET strategies. This interpretation, then, is encouraging as a measure of MET proficiency, as the explicit goal of MET is to provide therapists with a framework for responding to clients who are poorly motivated to reduce substance use. Clients with more motivation may need less frequent use of MET strategies that are intended to improve motivation.
Consistent with hypothesis 2a, we found that increased days of any substance use during treatment was related to lower MET adherence and competence. Caution is warranted in interpreting these results because the effects appeared to be due to influential observations of several clients who used almost daily during the trial, and the substance use variable in this analysis was not connected to a particular session. Thus, use during treatment was related to poorer therapist adherence and competence, but it is not possible to determine if therapist adherence or competence affected client substance use, or the reverse.
Baseline measures of client functioning did not consistently predict adherence or competence in providing MET. Increased client psychiatric severity was associated with decreased therapist advanced adherence to MET, indicating that providers may be less able to systematically elicit clients’ motivation or develop plans for change with clients with higher psychiatric symptom severity. However, this was one of few statistically significant predictors in a large analysis, so this result should be viewed cautiously. This may indicate that a client’s baseline addiction severity has less of an impact on therapist behavior than a client’s more recent use during treatment in that substance use during treatment is more proximal to how therapists respond to their clients. We expected that variables measuring addiction severity, in particular measures of associated psychosocial problems (e.g., legal problems) would predict frequency of MET strategies. We found only scant evidence for our hypothesis that clients with significant problems in associated life domains would present challenges for therapist delivery of MET. However, there may have been unmeasured variables such as client personality or interpersonal functioning that would predict therapist behaviors.
A general limitation of our analysis is the restriction of the sample to clients who completed all three treatment sessions. This restriction seemed logical given that the primary research question was to determine the effect of therapist behaviors on outcomes, and it would be difficult to examine the impact of therapist behavior on a client if the client had only marginal contact with the provider. However, this restriction may also have reduced our ability to detect associations between MET and other variables because only clients who were motivated enough to attend all three sessions were included. It is also important to note that our analysis included therapists who were trained and monitored in their provision of MET. Accordingly, one might expect more variability both within and between therapists in community treatment programs with less training or supervision. Another limitation is that raters simultaneously rated the therapists’ MET adherence and competence and client motivation in the same sessions. Bias is possible in that the actions of the therapist in the early portion of the session could have influenced ratings of the client. However, raters were told to rate adherence and competence without considering client response. In addition, an advantage of using client motivation at the beginning of the session as a predictor of therapist use of MET is that ratings are not as confounded by therapist behaviors during the remaining part of the session. Future analyses may be complimented by self-report or observer ratings of client motivation taken before the first meeting with the therapist, or by moment by moment sequential analysis of verbal interactions (c.f., Moyers et al, 2009).
An important topic for future research is to determine if therapist variability in adherence within their caseload is intentional or unintentional (it seems unlikely that therapists would intentionally perform less competently). Specifically, variability in adherence within caseloads may be an example of therapist responsivity to a given client presentation. However, it may also represent therapists’ lack of ability or knowledge regarding how to apply MET with more (or less) challenging clients. There is also the potential for more subtle forms of client influence wherein therapists respond to client behavior less strategically. For example, a client with a certain interpersonal style may elicit behaviors inconsistent with MET despite a therapist’s intention to maintain adherence. This perspective would be consistent with the finding that therapists respond more confrontationally to confederate clients who are intentionally presenting as more resistant (Francis et al., 2005). Alternatively, there is evidence that the relationship between adherence to specific drug counseling interventions and treatment outcome is curvilinear, indicating that moderate levels of adherence to specified behaviors is most beneficial to clients (Barber et al., 2006). Further study is needed to determine how this process unfolds in therapy and the degree to which therapist flexibility is beneficial to clients.
The current study provides further evidence to suggest that therapists' use of MET happens in a complex interpersonal interaction and that therapists often do not apply the same set of skills uniformly across clients. This finding has important implications for the future of process and outcome studies. For example, previous research indicates that the strength of client commitment predicts subsequent substance use (Amrhein et al., 2003; Aharonovich et al., 2008). However, the current findings indicate the potential for a negative feedback loop wherein increased client motivation could result in less counselor use of MET strategies. Accordingly, the simple correlation between therapist adherence and client motivation may be a poor indicator of their true relationship. This phenomenon may be one explanation for the lack of consistent correlations between adherence, competence and treatment outcome in MET (Martino et al, 2008) and perhaps psychotherapy generally (Webb et al., 2010). Ratings of therapist adherence may need to be conceptualized or defined to include more dyadic components, for example, use of strategies that are relevant to clients’ needs. Future analyses of the relationship between therapist behavior and clinical outcomes will also likely be improved by the use of multilevel modeling approaches that can disentangle multiple sources of variability (see Baldwin et al., 2007; Crits-Christoph et al., 2009).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aharonovich E, Amrhein PC, Bisaga A, Nunes EV, Hasin DS. Cognition, commitment language, and behavioral change among cocaine-dependent patients. Psychol. Addict. Behav. 2008;22:557–562. doi: 10.1037/a0012971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Brown LS, Zaballero A, McKay JR. Interviewer severity ratings and composite scores of the ASI: a further look. Drug Alcohol Depend. 1994;34:201–209. doi: 10.1016/0376-8716(94)90157-0. [DOI] [PubMed] [Google Scholar]
- Alterman AI, Bovasso GB, Cacciola JS, McDermott PA. A comparison of the predictive validity of four sets of baseline ASI summary indices. Psychol. Addict. Behav. 2001;15:159–162. doi: 10.1037//0893-164x.15.2.159. [DOI] [PubMed] [Google Scholar]
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J. Consult. Clin. Psychol. 2003;71:862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Wampold BE, Imel ZE. Untangling the alliance-outcome correlation: exploring the relative importance of therapist and patient variability in the alliance. J. Consult. Clin. Psychol. 2007;75:842–852. doi: 10.1037/0022-006X.75.6.842. [DOI] [PubMed] [Google Scholar]
- Ball SA, Martino S, Nich C, Frankfort TL, Van Horn D, Crits-Christoph P, Woody GE, Obert JL, Farentinos C, Carroll KM. Site matters: multisite randomized trial of motivational enhancement therapy in community drug abuse clinics. J. Consult. Clin. Psychol. 2007;75:556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber JP, Gallop R, Crits-Christoph P, Frank A, Thase ME, Weiss RD, Connolly Gibbons MB. The role of therapist adherence, therapist competence, and the alliance in predicting outcome of individual drug counseling: results from the NIDA Collaborative Cocaine Treatment Study. Psychother. Res. 2006;16:229–240. [Google Scholar]
- Crits-Christoph P, Gallop R, Temes CM, Woody G, Ball SA, Martino S, Carroll KM. The alliance in motivational enhancement therapy and counseling as usual for substance use problems. J. Consult. Clin. Psychol. 2009;77:1125–1135. doi: 10.1037/a0017045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry R, Frankforter T, Nuro KF, Ball SA, Fenton LR, Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Farentinos C, Ball SA, Crits-Christoph P, Libby B, Morgenstern J, Obert JL, Polcin D, Woody GE. MET meets the real world: design issues and clinical strategies in the Clinical Trials Network. J. Subst. Abuse Treat. 2002;23:73–80. doi: 10.1016/s0740-5472(02)00255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Kadden RR, Longabaugh RL, Rounsaville BJ, Wirtz PW, Zweben A. Internal validity of Project MATCH treatments: discriminability and integrity. J. Consult. Clin. Psychol. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel LE, Mikulich-Gilbertson SK, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE National Institute on Drug Abuse Clinical Trials Network. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug Alcohol Depend. 2006;81:301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farentinos C, Obert JL. CTN Motivational Enhancement Treatment Manual. 2000. Unpublished manuscript. [Google Scholar]
- Francis N, Rollnick S, McCambridge J, Butler C, Lane C, Hood K. When smokers are resistant to change: experimental analysis of the effect of patient resistance on practitioner behaviour. Addiction. 2005;100:1175–1182. doi: 10.1111/j.1360-0443.2005.01124.x. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Faouzi M, Daeppen JB. Counselor skill influences outcomes of brief motivational interventions. J. Subst. Abuse Treat. 2009;37:151–159. doi: 10.1016/j.jsat.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Faouzi M, Daeppen JB. Counsellor behaviours and patient language during brief motivational interventions: a sequential analysis of speech. Addiction. 2008;103:1793–1800. doi: 10.1111/j.1360-0443.2008.02337.x. [DOI] [PubMed] [Google Scholar]
- Gibbons CJ, Steinberg K, Nich C, Roffman RA, Kadden RM, Corvino J, Babor TF, Carroll KM. Treatment process, alliance and outcome in brief versus extended treatments for marijuana dependence. Addiction. 2010;105:1799–1808. doi: 10.1111/j.1360-0443.2010.03047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartzler B, Rosengren DB, Baer JS. Motivational interviewing. In: Cohen LM, Collins FL, Young AM, McChargue DE, Leffingwell TR, editors. The Pharmacology and Treatment of Substance Abuse: Evidence and Outcomes Based Perspectives. Washington DC: Routledge Taylor & Francis; 2009. [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annu. Rev. Clin. Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke B. Meta-analysis of motivational interviewing: Twenty Five years of empirical studies. Res Soc. Work Prac. 2010;20:137–160. [Google Scholar]
- Marcus DK, Kashy DA, Baldwin SA. Studying psychotherapy using the one-with-many design: The therapeutic alliance as an exemplar. J. Couns. Psychol. 2009;56:537–548. [Google Scholar]
- Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community program therapist adherence and competence in motivational enhancement. Drug Alcohol Depend. 2008;96:37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Confrontation and resistance as chicken and egg: comment on Francis et al. (2005) Addiction. 2006;101:137. doi: 10.1111/j.1360-0443.2006.01333.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Project MATCH Monograph Series. vol. 2. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. Motivational Enhancement Therapy Manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford Press; 2002. [Google Scholar]
- Miller WS, Rose GS. Towards a theory of motivational interviewing. Am. Psychol. 2009;64:527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Wilbourne PL, Hettema JE. What works? A summary of alcohol treatment outcome research. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 3rd ed. Boston, MA: Allyn & Bacon; 2003. pp. 13–63. [Google Scholar]
- Miller WR, Moyers T, Ernst D, Amrhein P. Manual for the Motivational Interviewing Skills Code, MISC v. 2.0. 2003. [Accessed on September, 20, 2009]. from http://casaa.unm.edu/codinginst.html. [Google Scholar]
- Miller WR, Yahne CE, Moyers TE, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J. Consult. Clin. Psychol. 2004;72:1050–1062. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Catley D, Harris KJ, Ahluwalia JS. Assessing the integrity of motivational interviewing interventions: reliability of the motivational interviewing skills code. Behav. Cogn. Psychother. 2003;31:177–184. [Google Scholar]
- Moyers TB, Miller WR, Hendrickson SM. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. J. Consult. Clin. Psychol. 2005;73:590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions: support for a potential causal mechanism. J. Subst. Abuse Treat. 2006;30:245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Catley D, Harris KJ, Ahluwalia JS. Assessing the integrity of motivational interviewing interventions: reliability of the motivational interviewing skills code. Behav. Cogn. Psychother. 2003;31:177–184. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SL, Miller WR. Assessing competence in the use of motivational interviewing. J. Subst. Abuse Treat. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: a causal chain for motivational interviewing. J. Consult. Clin. Psychol. 2009;77:1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM: Hierarchical Linear and Nonlinear Modeling. HLM Software; 2005. [Google Scholar]
- Santa Ana EJ, Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. What is usual about "treatment as usual"? Data from two multisite effectiveness trials. J. Subst. Abuse Treat. 2008;35:369–379. doi: 10.1016/j.jsat.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santa Ana EJ, Carroll KM, Añez L, Paris M, Ball SA, Nich C, Frankforter TL, Suarez-Martinez L, Szapocznik J, Martino S. Evaluating motivational interviewing adherence and competence among Spanish-speaking therapists. Drug Alcohol Depend. 2009;103:44–51. doi: 10.1016/j.drugalcdep.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer J, Willet JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana; 1992. pp. 41–72. [Google Scholar]
- Thyrian JR, Freyer-Adam J, Hannöver W, Röske K, Mentzel F, Kufeld C, Bischof G, Rumpf HJ, John U, Hapke U. Adherence to the principles of Motivational Interviewing, clients' characteristics and behavior outcome in a smoking cessation and relapse prevention trial in women postpartum. Addict. Behav. 2007;32:2297–2303. doi: 10.1016/j.addbeh.2007.01.024. [DOI] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Barber J. Therapist adherence/competence and treatment outcome: a meta-analytic review. J. Consult. Clin. Psychol. 2010;78:200–211. doi: 10.1037/a0018912. [DOI] [PMC free article] [PubMed] [Google Scholar]