Abstract
A prototype 1,310-nm wavelength spectral domain optical coherence tomography (SD-OCT) instrument was constructed and mounted onto a conventional slit lamp for imaging of the anterior segment. The device had an axial resolution of 8 µm and was able to acquire real-time two-dimensional images at 14 frames/second and full three-dimensional datasets in approximately 7 seconds. An SD-OCT dataset of 100 B-scans, each consisting of 512 A-scans, was acquired from the left eye of a patient who had undergone phacoemulsification with a clear corneal incision. The resulting dataset could be manipulated in three-dimensional space to analyze the geometry of the wound. Additionally, stromal edema and iris features were clearly imaged with the device. SD-OCT can be used to analyze clear corneal incisions to determine optimal wound construction technique and geometry as they relate to the prevention of complications such as postoperative wound leak, infection, and epithelial ingrowth.
INTRODUCTION
A clear corneal incision has become the preferred type of wound used in phacoemulsification cataract surgery.1 It provides for a bloodless surgical field and reduced postoperative recovery time, and is self-sealing if properly constructed. Since their inception in the early 1990s, it has been suggested that clear corneal incisions are responsible for the increased reported rates of postoperative endophthalmitis.2,3 Although there is no definitive evidence implicating a specific component of clear corneal incisions in the increased rate of postoperative endophthalmitis, wound features such as gaping, misalignment, and loss of coaptation have been identified as possible contributors to this sight-threatening problem.4
Optical coherence tomography (OCT) is the first type of imaging technology able to examine the cross-sectional architecture of clear corneal incisions. Recently, time domain OCT systems such as Visante (Carl Zeiss Meditec, Inc., Dublin, CA) have been used to image clear corneal incisions and assess wound integrity.4,5 These systems acquire a two-dimensional B-scan with an 18-µm axial resolution (Carl Zeiss Meditec, Inc., Visante product information).
Anterior segment spectral domain OCT (SD-OCT) has several advantages over commercially available time domain anterior segment OCT systems. 6–8 Although the axial resolution of the two technologies is comparable, anterior segment SD-OCT has a greater speed of image acquisition, allowing three-dimensional datasets to be acquired. Furthermore, anterior segment SD-OCT has an enhanced ability to visualize the cornea and other structures with low reflectivity.
REPORT
A prototype anterior segment SD-OCT device using a superluminescent diode laser with a 75-nm bandwidth centered at 1,310 nm was constructed. The spectrometer was custom developed by Bioptigen (Durham, NC) and was connected with a telecentric light delivery probe. The device was then mounted on a conventional slit lamp for conducting examinations of eyes with postoperative clear corneal incisions. The device had an axial resolution of 8 µm in tissue and had an acquisition speed of approximately 7,000 A-scans/second. It was able to acquire real-time two-dimensional B-scans, each consisting of 512 A-scans, at 14 frames/second and full three-dimensional datasets in approximately 7 seconds. Images were acquired using a 6 × 6 × 3 mm rectangular scan pattern through the cornea centered on the clear corneal incision. The imaging of patients using this instrument occurred after informed consent was obtained and was approved by the University of Miami Miller School of Medicine Medical Sciences Subcommittee for the Protection of Human Subjects and the Institutional Review Board.
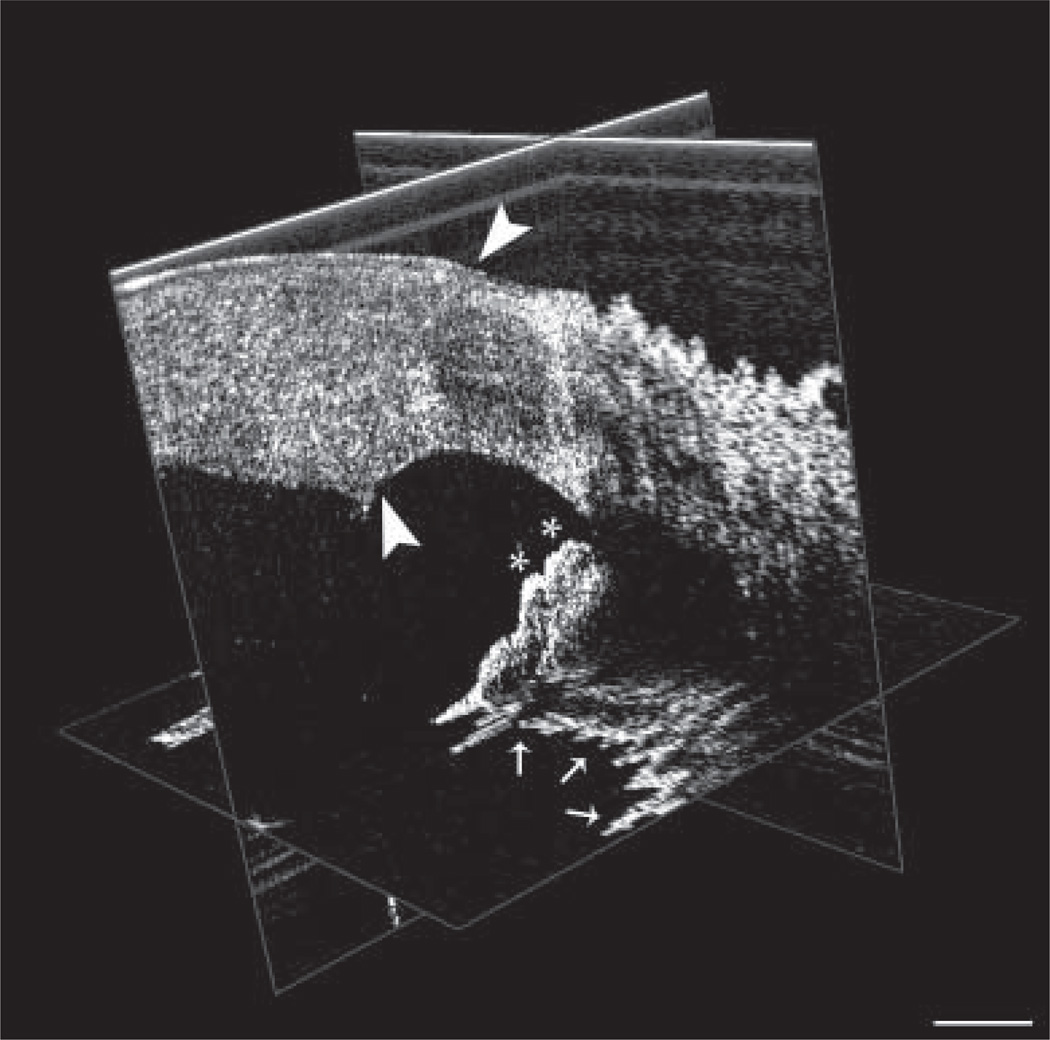
An anterior segment SD-OCT three-dimensional dataset of 100 B-scans, each consisting of 512 A-scans, was acquired on postoperative day 1 from a clear corneal incision created with a 3.0-mm keratome blade from an 80-year-old man who underwent uncomplicated cataract extraction by phacoemulsification and posterior chamber intraocular lens implantation. The scan dataset consisted of 100 B-scans, which allowed for the reconstruction of an en face image of the temporal limbus using proprietary software (Fig. 1). Additionally, a three-dimensional cube was generated that could be manipulated in space to fully analyze the geometry of the wound (Fig. 2). This data cube could be rotated in three-dimensional space and individual B-scans (actual and reconstructed) could be viewed in all three axes to analyze the anatomy of the clear corneal incision, the anatomic angle, and the iris.
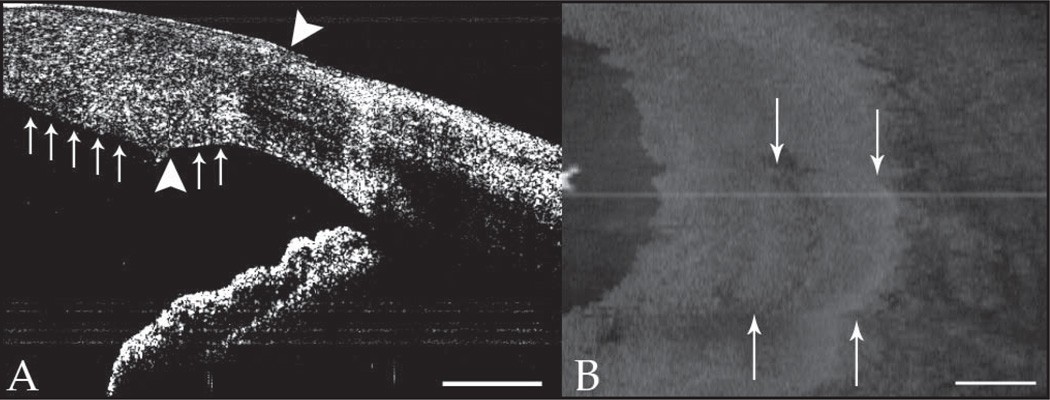
Figure 1.
Spectral domain optical coherence tomography two-dimensional B-scan (A) and reconstructed en face image (B) of the temporal limbus. The en face image demonstrates the location of the clear corneal incision (arrows). The geometry of the clear corneal incision is distinctly visible in the two-dimensional Bscan (between arrowheads). Additionally, an area of stromal edema (arrows) is visible. Scale bars are 1 mm.
Figure 2.
Spectral domain optical coherence tomography three-dimensional data cube with one frame selected in each of three axes. This dataset can be rotated in all three axes. Additionally, each viewing plane can be scanned through to localize specific points in the three-dimensional cube of data, which can then be viewed from any angle. In the configuration shown, peripheral rolls of iris (asterisks) and the pupillary margin (arrows) are visible. Additionally, the geometry of the clear corneal incision is visible (between arrowheads). Scale bar is 1 mm.
DISCUSSION
Anterior segment SD-OCT is a powerful new technology that is able to acquire volumetric data that can be rendered and manipulated three-dimensionally and provides increased utility compared to the cross-sectional data gathered from commercially available anterior segment time domain OCT instruments. Individual slices from the three-dimensional anterior segment SD-OCT dataset consist of individual B-scans that contain the postoperative clear corneal incision. The three-dimensional architecture of the wound and specific features of the wound, such as areas of stromal edema, could be determined by software analysis of the wound on each consecutive B-scan. Volumetric data have a distinct advantage over a single time domain B-scan in that the full three-dimensional architecture of a clear corneal incision can be rendered.
Anterior segment SD-OCT of the cornea has been described previously using an 830-nm device.8 The longer wavelength of 1,310-nm SD-OCT is advantageous because it allows for deeper tissue penetration. Thus, full-thickness cornea, sclera, and iris can be imaged, providing a full assessment of anterior segment anatomy and pathology. This article serves as a proof of concept that 1,310-nm anterior segment SD-OCT can obtain volumetric data of a clear corneal incision. Currently, the axial resolution of the device is 8 µm and the instrument has a 7-second three-dimensional acquisition time and consequently is subject to motion artifact. However, inevitable improvements in the light source and acquisition speed will improve axial resolution and minimize motion artifact.
We have demonstrated an anterior segment SD-OCT system that can acquire three-dimensional data of the anterior segment and can be used to assess clear corneal incisions. Ultimately, this technology will allow consecutive B-scans to be segmented to reveal the three-dimensional architecture of clear corneal incisions, thus providing an anatomic characterization of the optimal surgical wound.
Acknowledgments
Supported by research grants from NEI (R03 EY016420), NEI core center grant P30 EY014801 to the University of Miami, and Research to Prevent Blindness, Inc., New York, New York
REFERENCES
- 1.Duffey RJ, Leaming DV. Trends in refractive surgery in the United States. J Cataract Refract Surg. 2004;30:1781–1785. doi: 10.1016/j.jcrs.2004.05.038. [DOI] [PubMed] [Google Scholar]
- 2.Masket S. Is there a relationship between clear corneal cataract incisions and endophthalmitis? J Cataract Refract Surg. 2005;31:643–645. doi: 10.1016/j.jcrs.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 3.Miller JJ, Scott IU, Flynn HW, Jr, Smiddy WE, Newton J, Miller D. Acute-onset endophthalmitis after cataract surgery (2000–2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol. 2005;139:983–987. doi: 10.1016/j.ajo.2005.01.025. [DOI] [PubMed] [Google Scholar]
- 4.Calladine D, Packard R. Clear corneal incision architecture in the immediate postoperative period evaluated using optical coherence tomography. J Cataract Refract Surg. 2007;33:1429–1435. doi: 10.1016/j.jcrs.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Fine IH, Hoffman RS, Packer M. Profile of clear corneal cataract incisions demonstrated by optical coherence tomography. J Cataract Refract Surg. 2007;33:94–97. doi: 10.1016/j.jcrs.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Wojtkowski M, Bajraszewski T, Targowski P, Kowalczyk A. Real-time in vivo imaging by high-speed spectral optical coherence tomography. Opt Lett. 2003;28:1745–1747. doi: 10.1364/ol.28.001745. [DOI] [PubMed] [Google Scholar]
- 7.Nassif N, Cense B, Park BH, et al. In vivo human retinal imaging by ultrahigh-speed spectral domain optical coherence tomography. Opt Lett. 2004;29:480–482. doi: 10.1364/ol.29.000480. [DOI] [PubMed] [Google Scholar]
- 8.Kaluzny BJ, Kaluzny JJ, Szkulmowska A, et al. Spectral optical coherence tomography: a novel technique for cornea imaging. Cornea. 2006;25:960–965. doi: 10.1097/01.ico.0000224644.81719.59. Erratum in: Cornea. 2007;26:646. [DOI] [PubMed] [Google Scholar]