Abstract
Breast Surgery is now a recognized subspecialty of General Surgery abroad with structured training for designated ‘Oncoplastic Breast Surgeons’. Oncoplastic Breast surgery is probably one of the most interesting and challenging new developments over the past 20 years. The aims of Oncoplastic surgery are wide local excision of the cancer coupled with partial reconstruction of the defect to achieve a cosmetically acceptable result. Avoidance of mastectomy and consequent reduction of psychological morbidity are the principal goals in the development of various oncoplastic techniques. The use of plastic surgical techniques not only ensures good cosmetic outcome, but also allows the cancer surgeon to remove the tumour with greater volume of surrounding tissue, thus extending the boundaries of breast conserving surgery. Proper patient selection and careful planning after proper radiological and clinical assessment are the two essential prerequisites before undertaking oncoplastic breast surgery. Oncoplastic surgery involves both volume displacement and volume replacement techniques. Some commonly used volume displacement procedures are described in the article. The need for adjustment of contralateral breast should also be anticipated at the time of planning breast conserving surgery, which can be done either at the same time as breast cancer surgery or as a delayed setting.
Introduction
Breast Surgery is now a recognized subspecialty of General Surgery with structured training for designated ‘Breast Surgeons’. Over the recent years, Breast cancer care has been enhanced by the emergence of Specialist Breast Surgeon with training in Oncoplastic Surgical skills – Oncoplastic Breast Surgeon [1–3].
Oncoplastic Breast surgery is probably one of the most interesting and challenging new developments of the last 20 years. The aims of Oncoplastic surgery are wide local excision of the cancer coupled with partial reconstruction of the defect to achieve a cosmetically acceptable result. Avoidance of mastectomy and consequent reduction of psychological morbidity are the principal goals in the development of various oncoplastic techniques. The focus of this chapter would be to highlight the principles governing the art and science of Oncoplastic beast conserving Surgery.
Key Points 1 and 2
Over the recent years, Breast cancer care has been enhanced by the emergence of Specialist Breast Surgeon with training in Oncoplastic Surgical skills – Oncoplastic Breast Surgeon.
The aims of Oncoplastic surgery are wide local excision of the cancer coupled with partial reconstruction of the defect to achieve a cosmetically good result. Avoidance of mastectomy and consequent reduction of psychological morbidity are the principal goals in the development of various oncoplastic techniques.
The Basics
Randomized controlled trials (RCTs) over the past two decades have now established that mastectomy and breast conserving surgery are equivalent in terms of survival [4, 5] provided local recurrence rates after breast conservation surgery are kept at about 1 % per annum [6].
Oncoplastic surgery should not be either identified or confused with breast reconstructive surgery after mastectomy. Whereas it is possible for a Breast surgeon to perform a mastectomy and then allow the Plastic surgeon to carry out the reconstruction, this is not feasible in oncoplastic breast conservative surgery, as it requires knowledge both of oncological and plastic surgery combined in one person for a good oncological and cosmetic outcome.
The concept of the Oncoplastic Breast surgeon is a new one for which formal training is still not fully developed. The difficulty lays in the fact that it requires the combination of knowledge in thee different specialties: Surgical oncology, Plastic surgery and Breast radiology.
An Oncoplastic Breast Surgeon has to address three questions before undertaking oncoplastic breast conserving surgery
Can the cancer be removed with a simple wide local excision with a good cosmetic result?
If not, would an oncoplastic technique either at the outset or after neoadjuvant systemic treatment reduce the risk of positive margins requiring a subsequent mastectomy?
Are the chances of achieving clear margins so small that breast conservation might not be advisable (although the patient might be willing to take a small chance)?
The answer to these questions is often not easy and requires considerable knowledge and experience not only in oncological and oncoplastic surgery, but also more importantly, in radiological assessment of the breast. A careful evaluation of mammographic, ultrasound and sometimes MRI extent of the disease, its nearness to the nipple and the distribution of the cancer in either radial or circumferential manner are all essential to the planning and the eventual success of the procedure.
Contrary to popular belief a few years ago, we now know that in some cases ipsilateral breast cancer local recurrence can be a determinant cause of death from the disease and therefore every attempt must be made to reduce the risk of local recurrence [6].
The oncoplastic surgical techniques described below avoids a mastectomy in carefully selected patients, achieves wider margins of excision and therefore, reduce the risk of local recurrence and consequently produces good cosmetic results.
Key Point 3
Oncoplastic surgery should not be confused with breast reconstructive surgery after mastectomy. Oncoplastic Breast Surgeon requires the combination of knowledge in thee different specialties: Surgical oncology, Plastic surgery and Breast radiology.
Criteria for Breast Conserving Surgery
The criteria for breast conserving surgery are relative. Contrary to the traditional teaching, breast conserving surgery is feasible every time it is judged possible to achieve complete surgical excision with good cosmesis. The size of the tumour relative to the breast volume is the deciding factor in determining the suitability of breast conserving surgery. It may even be suitable for women with large breasts in whom the tumour is up to 5 cm or even multifocal tumours confined to the same quadrant and when large operable tumours have been down-staged by neoadjuvant chemotherapy [7]. The use of plastic surgical techniques not only ensures good cosmetic outcome, but also allows the cancer surgeon to remove the tumour with greater volume of surrounding tissue, thus extending the boundaries of breast conserving surgery.
Planning & Choice of Incision
Poor planning in breast conserving surgery can result in unacceptable deformity. Bad cosmetic outcome following breast conserving surgery occurs due to combination of factors such as wrongly placed incision, poor surgical technique resulting in local glandular defect and scar contracture.
The choice of incision is crucial. Radial incisions in the lower part of the breast and circumlinear incisions in the upper half result in least visible scars. The incisions for dealing with lesions in the upper and outer quadrant of the breast should ideally be separate from the axillary incision to prevent scar contracture [8].
Good cosmetic outcome can be obtained if deeper glandular tissue is approximated to obliterate glandular defect. After excision of the lesion, the breast tissue must be mobilized both at the level of the pectoral fascia and the subcutaneous plane to allow tension free approximation of tissues.
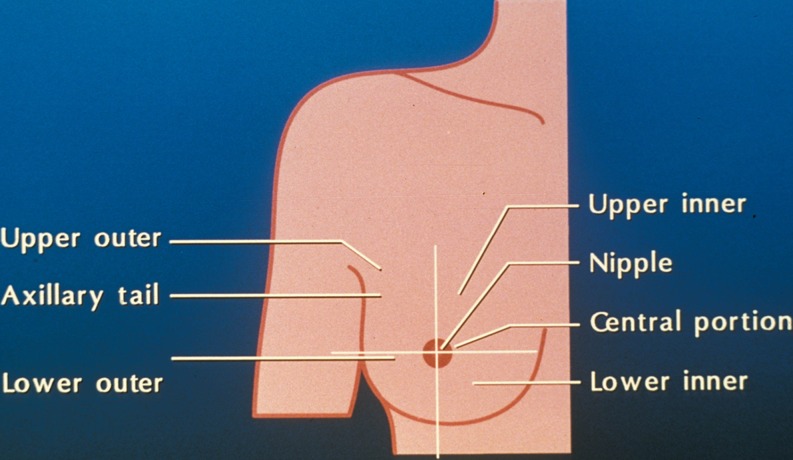
Based on the clock position of the lesion in the left breast, the suggested incisions would be as follows [8, 9] :
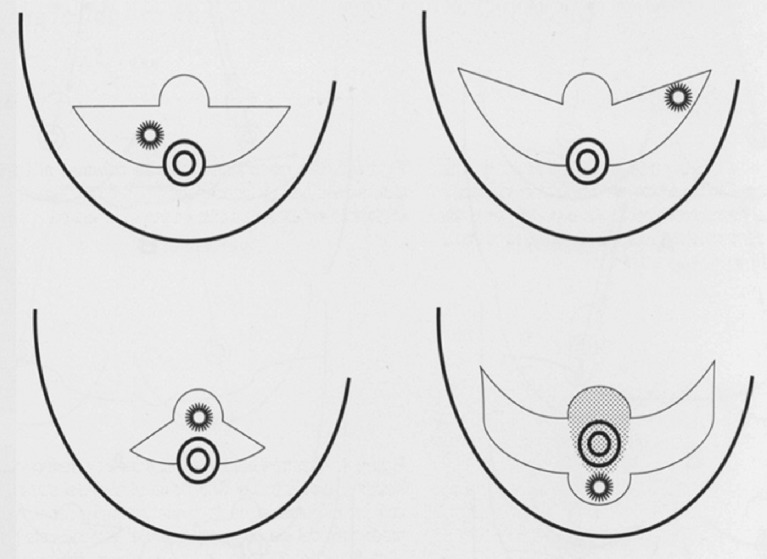
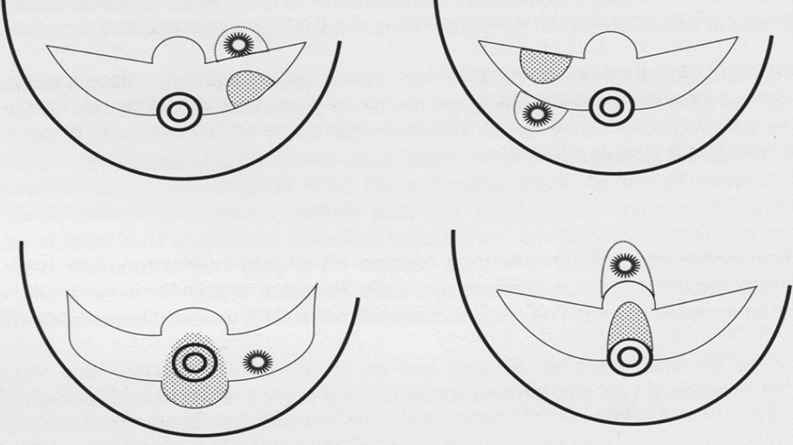
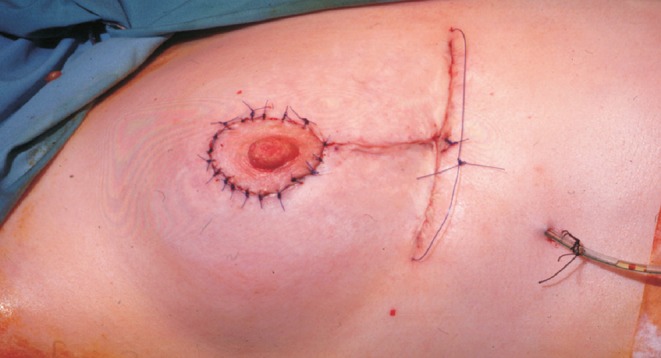
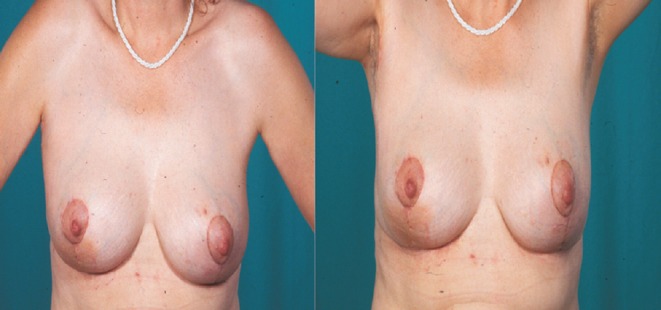
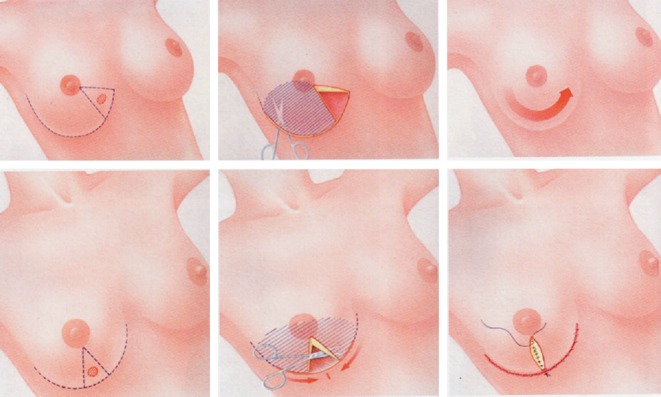
12 o’clock: circumareolar (with or without medial/lateral extensions), circumferential or Round Block technique (Figs. 1, 2, 3 and 4)
1 to 4 o’clock: Radial or lateral mammoplasty; if concomitant axillary dissection is required the axillary incision should be on the lower skin crease of the axilla and border of the pectoralis major muscle. For larger cancers, the two incisions can be joined together to allow better mobilization and reconstruction of the breast parenchyma.
5 and 6 o’clock: slightly comma shaped, superior pedicle reduction or glandular rotation (Fig. 5)
7 and 8 o’clock: Radial, glandular rotation, thoraco-epigastric flap or breast reduction (superior - Figs. 6, 7, 8 and 9 or inferior – Figs. 10–14 pedicle)
9 0’clock: Radial or Round block technique
10 and 11 0’clock: Circumferential or Round Block technique
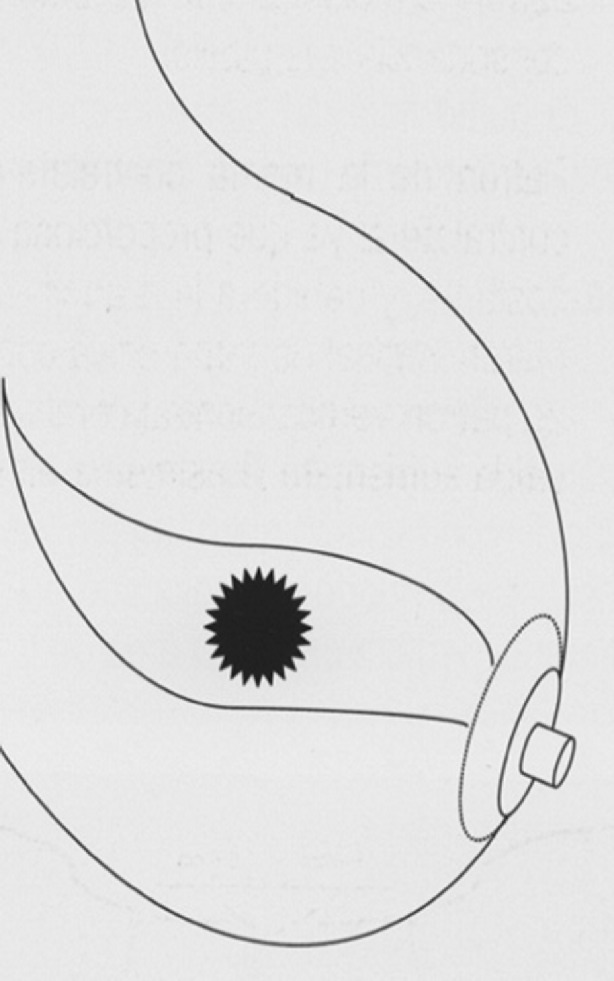
Retro areolar (Central): Grisotti advancement rotation flap (Figs. 15–19)
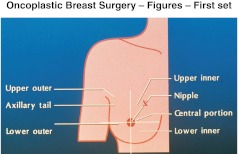
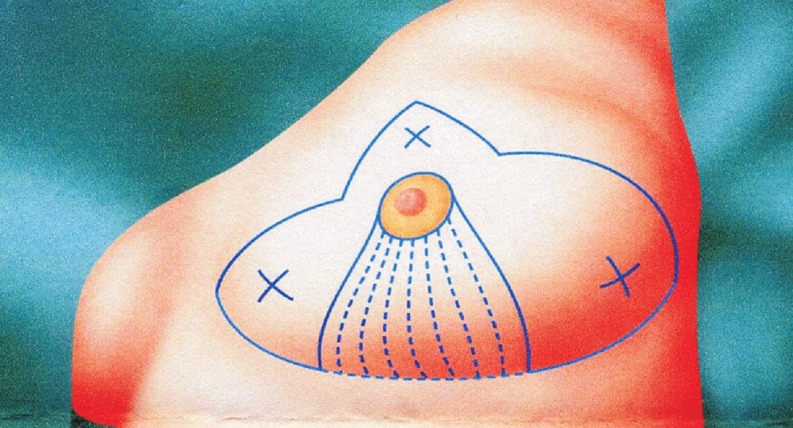
Fig. 1.
Round block technique for cancers in the upper inner quadrant of the breast. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
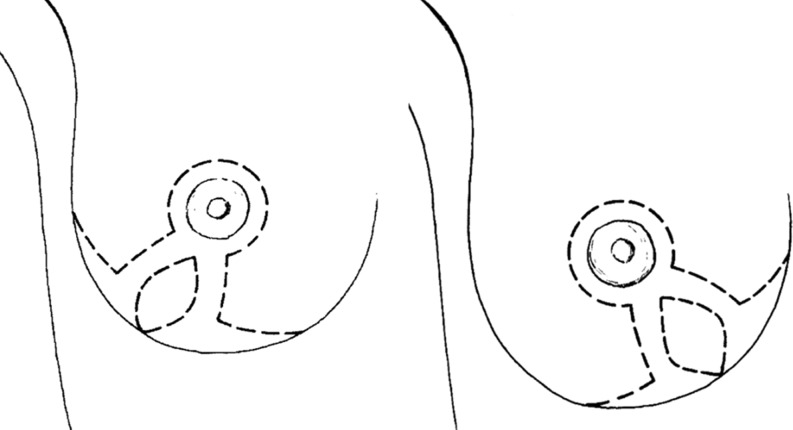
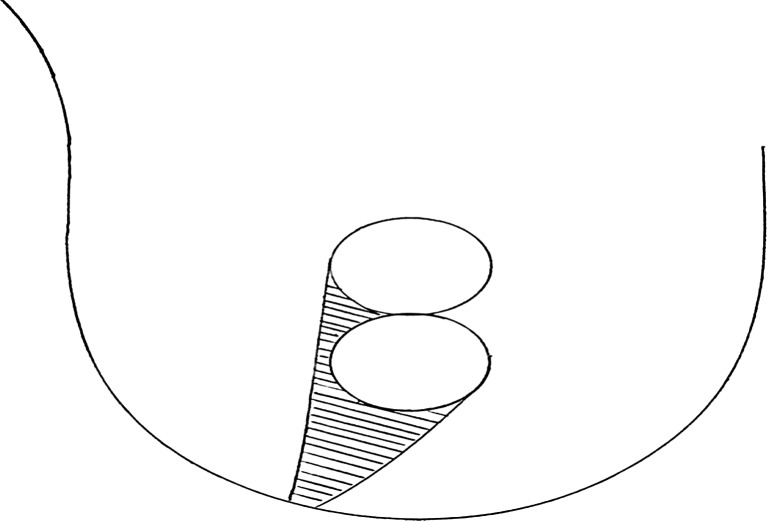
Fig. 2.

Round block technique – skin marking. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 3.

Round block technique – view after completion of operation. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 4.

Round block technique – postoperative view. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
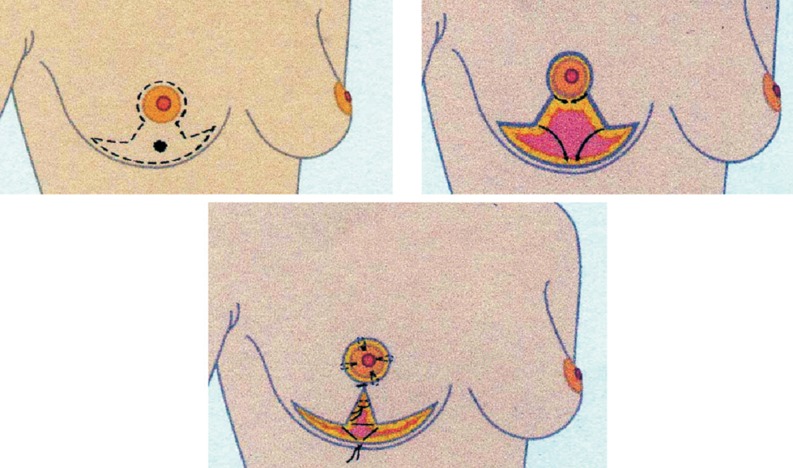
Fig. 5.
Comma-shaped breast mammoplasty breast reduction or mastoplexy. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 6.
Superior pedicle breast reduction for cancers in the lower part of the breast. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 7.

Superior pedicle breast reduction – skin marking and extent of excision. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 8.
Superior pedicle breast reduction. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 9.
Superior pedicle breast reduction – postoperative view. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Key Points 4–6
Proper patient selection and careful planning after proper radiological and clinical assessment are the two essential prerequisites before undertaking oncoplastic breast conserving surgery.
Bad cosmetic outcome following breast conserving surgery occurs due to combination of factors such as wrongly placed incision, poor surgical technique resulting in local glandular defect and scar contracture.
Good cosmetic outcome can be obtained if deeper glandular tissue is approximated to obliterate glandular defect. After excision of the lesion, the breast tissue must be mobilized at the level of the pectoral fascia and the subcutaneous plane to allow tension free approximation of tissues.
Volume Displacement and Replacement
Oncoplastic surgery involves both volume displacement and volume replacement techniques. However, volume displacement is more common in the context of breast conserving surgery, which is done at the same sitting rather than as delayed procedure. When the tumour is large in a relatively large breast, Reduction mammoplasty (breast reducing surgery) can be fashioned using the nipple areola pedicle based either superiorly or inferiorly.
Volume Displacement Techniques
The commonly used volume displacement procedures [8, 9] are:
Superior pedicle breast reduction for cancers in the lower part of the breast (Figs. 6, 7, 8 and 9)
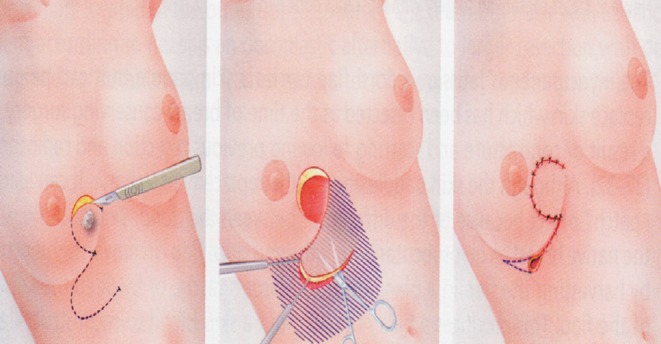
- Inferior pedicle breast reduction for cancers above the nipple or in the lower medial or lateral quadrants (Figs. 10–14)
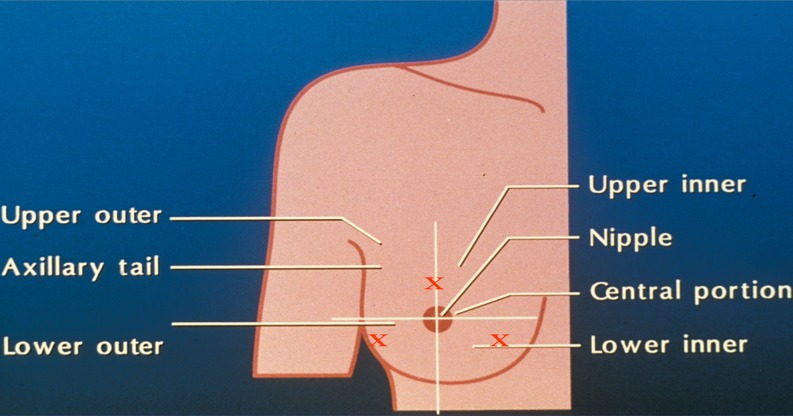
Fig. 11.
Inferior pedicle breast reduction. Dotted lines represent the inferior pedicle and ‘X’ the extent of excision (reduction). Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa HealthcareFig. 12.
 Inferior pedicle breast reduction – skin marking and extent of excision. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Inferior pedicle breast reduction – skin marking and extent of excision. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa HealthcareFig. 13.
 Inferior pedicle breast reduction – postoperative view. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Inferior pedicle breast reduction – postoperative view. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare - Grisotti advancement rotation flap for small tumours in the central quadrant of the breast (retro areolar region) (Figs. 15–19)
Fig. 16.
Grisotti advancement (rotation flap) for Central quadrant tumours – Line diagram. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa HealthcareFig. 17.
 Grisotti advancement – skin marking. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Grisotti advancement – skin marking. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa HealthcareFig. 18.
 Grisotti advancement – wound completely closed. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Grisotti advancement – wound completely closed. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare Round block technique for cancers in the upper and inner quadrant of the breast or in the 12 o/c position (Figs. 1, 2, 3 and 4)
Local glandular flaps: Glandular rotation for tumours in the lower inner quadrant and 6o/c position (Fig. 21). Thoraco-epigastric flap for tumours in the lower inner quadrants (Fig. 20)
Lateral mammoplasty for tumours in the upper outer quadrants (but not in the 12 o/c position in which case a Round block is preferable, Fig. 22)
Horizontal mammoplasty for tumors above the level of the nipple but at least 18–20 cm below the clavicle (Figs. 23 and 24)
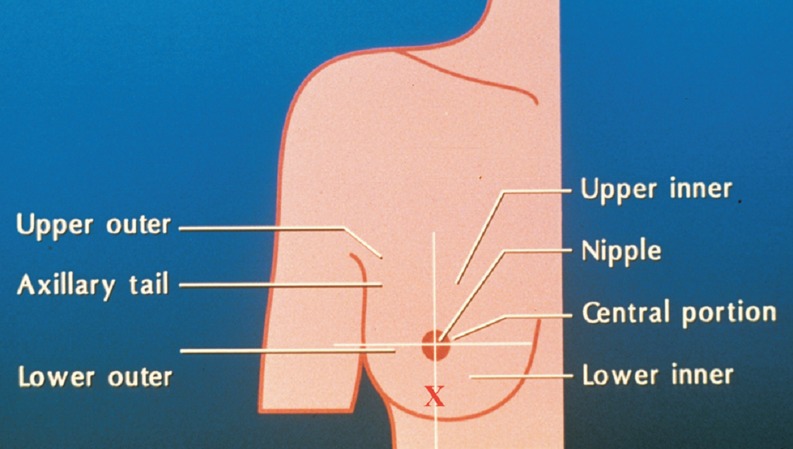
Fig. 10.
Inferior pedicle breast reduction for cancers above the nipple or in the lower medial or lateral quadrants. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 14.
Inferior pedicle breast reduction – postoperative view with contralateral reduction. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 15.
Grisotti advancement (rotation flap) for central quadrant tumours. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 19.

Grisotti advancement – postoperative view. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 21.
Glandular rotation after breast-conserving surgery. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 20.
Thoraco-epigastric flap after breast-conserving surgery. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 22.
Lateral mammoplasty. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 23.
Horizontal mammoplasty. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Fig. 24.
Horizontal mammoplasty. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Key Points 7–9
Oncoplastic surgery involves both volume displacement and volume replacement techniques. The indications for cosmetically acceptable breast conserving surgery can be safely extended to tumours involving all the quadrants of the breast, thus expanding the armamentarium of Oncoplastic Surgery.
The use of plastic surgical techniques not only ensures good cosmetic outcome, but also allows the cancer surgeon to remove the tumour with greater volume of surrounding tissue, thus extending the boundaries of breast conserving surgery.
The need for adjustment of contralateral breast should also be anticipated at the time of planning breast conserving surgery. The primary aim is to correct any asymmetry between the operated breast and contralateral one. Contralateral oncoplastic surgery can be done either at the same time as breast cancer surgery or as a delayed setting.
Volume Replacement Techniques
Extensive resection in the breast could be replaced with volume (Volume replacement procedure). Mini latisimus dorsi (LD) flap is the commonly used flap to cover these defects. Patients should be counseled about an additional scar in the donor area, differences of colour and feel of the Latisimus dorsi flap compared to the normal breast and that the option of Latisimus dorsi flap reconstruction will not be available in the event of the patient developing a recurrence requiring completion mastectomy [8].
Oncoplastic Surgery After Radiotherapy
Oncoplastic breast surgery following radiotherapy is more complex. The breast tissue is less robust and less vascular; hence surgery is associated with potential complications. Contralateral breast reduction should be considered as an option to deal with breast asymmetry following radiotherapy and surgery should be avoided on the irradiated breast. Should there be gross deformity following radiotherapy to the breast, volume replacement technique, such as mini latisimus dorsi flap should be employed to correct the defect [8]. Myocutaneous flap, like the Latisimus dorsi flap is best suited in this scenario as it brings fresh blood supply to the area.
Key Point 10
Extensive resection in the breast could be replaced with volume (Volume replacement procedure). The mini latisimus dorsi flap is the commonly used flap to cover these defects. The clinician and the patient must, however, bear in mind that, in case of a future need for a mastectomy, this type of breast reconstruction will no longer be available
Contralateral Breast Surgery
Contralateral breast surgery aims to correct asymmetry between the operated breast and the contralateral one. Contralateral surgery involves one of the following procedures. (i) Adjustment of nipple areola complex. (ii) Mastopexy (a procedure that lifts the breast and increases projection). (iii) Reduction mammoplasty (breast reduction). (iv) Augmentation mammoplasty (breast enlargement) [9]
Immediate Versus Delayed
Contralateral oncoplastic surgery can be done either at the same time as breast cancer surgery or as a delayed setting [10]. It may become apparent at the stage of doing the oncoplastic procedure on the side affected with cancer that symmetry cannot be achieved without contralateral reduction. Being aware of this possibility will ensure that the contralateral breast reduction can be done at the same sitting, which would avoid further major surgery and a second general anesthetic.
Some surgeons prefer doing contralateral surgery as a delayed setting when the final shape of the reconstructed breast is better known. Delayed contralateral surgery is also performed when the volume of the reconstructed breast is difficult to predict, particularly in patients requiring radiotherapy
For tumours involving the lower medial or lower lateral part of a large ptotoc breast, inferior pedicle based breast reconstruction may be used and symmetry could be achieved by performing a similar procedure on the contralateral breast [9].
Minor asymmetry in the position of the nipple-areoa complex can be corrected using circumferential zone of de-epithelization. Greater degrees of asymmetry of nipple position can be corrected by mastopexy to achieve symmetry [9].
The final decision regarding the choice of oncoplastic procedures employed to achieve symmetry and whether contralateral surgery is performed at the time of undertaking primary surgery (immediate procedure) or as a delayed setting should be made after detailed counseling, taking into consideration patient expectations and objective assessment by the Oncoplastic breast surgeon.
Conclusions
In this era of Oncoplastic breast surgery, it would be unreasonable to remove a breast lesion and allow a seroma to fill the wound resulting in subsequent deformity. There is clearly a growing demand for cosmetically acceptable breast conserving surgery the world over. Breast cancer surgery must be carried out with due consideration to cosmetic outcome without oncological compromise as disfiguring and mutilating excisions are neither justified nor acceptable (Fig. 25).
Fig. 25.
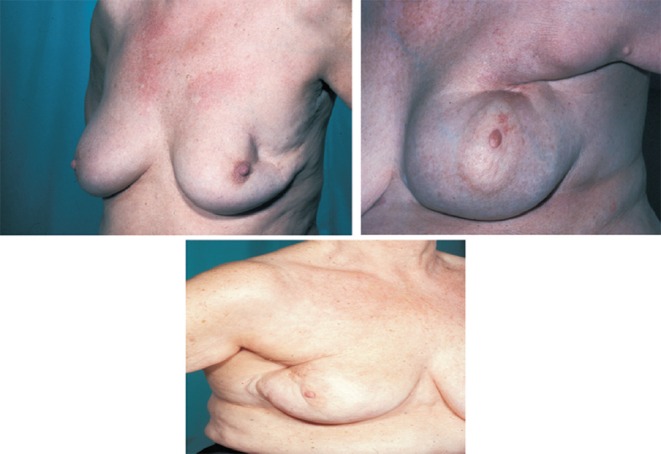
Poor outcomes following breast-conserving surgery. Reprinted from Oncoplastic and Reconstructive Surgery of the Breast published by Informa Healthcare (2004). Copyright Informa Healthcare
Oncoplastic Breast Surgery is an innovative and sophisticated subspecialty within Breast Surgery & is an essential skill for the dedicated Breast Specialist.
We would like to end with a quotation from Prof. Umberto Veronesi, who is considered to be the ‘godfather’ of modern breast surgery:
“Women aware of breast cancer issues and who participate in early detection programmes should be rewarded with gentle and appropriate care and not punished with heavy and often unjustified treatments”
Key Points for Clinical Practice
Over the recent years, Breast cancer care has been enhanced by the emergence of Specialist Breast Surgeon with training in Oncoplastic Surgical skills – Oncoplastic Breast Surgeon.
The aims of Oncoplastic surgery are wide local excision of the cancer coupled with partial reconstruction of the defect to achieve a cosmetically good result. Avoidance of mastectomy and consequent reduction of psychological morbidity are the principal goals in the development of various oncoplastic techniques.
Oncoplastic surgery should not be confused with breast reconstructive surgery after mastectomy. Oncoplastic Breast Surgeon requires the combination of knowledge in thee different specialties: Surgical oncology, Plastic surgery and Breast radiology.
Proper patient selection and careful planning after proper radiological and clinical assessment are the two essential prerequisites before undertaking oncoplastic breast conserving surgery.
Bad cosmetic outcome following breast conserving surgery occurs due to combination of factors such as wrongly placed incision, poor surgical technique resulting in local glandular defect and scar contracture.
The primary aim of contralateral breast surgery is to achieve symmetry between the operated breast and the contralateral one, which can be done at the same time as breast cancer surgery or as a delayed setting
Extensive resection in the breast could be replaced with volume (volume replacement procedure). The Mini latisimus dorsi flap is commonly used to cover these defects. The Clinician and the patient must, however, bear in mind that, in case of a future need for mastectomy, this type of breast reconstruction will no longer be available
Good cosmetic outcome can be obtained if deeper glandular tissue is approximated to obliterate the glandular defect. After excision of the lesion, the breast tissue must be mobilized at the level of the pectoralis fascia and the subcutaneous plane to allow tension-free approximation of tissues.
Oncoplastic surgery involves both volume displacement and volume replacement techniques. The indications for cosmetically acceptable breast conserving surgery can be safely extended to tumours involving all the quadrants of the breast, thus expanding the armamentarium of Oncoplastic Surgery.
The use of plastic surgical techniques not only ensures good cosmetic outcome, but also allows the cancer surgeon to remove the tumour with greater volume of surrounding tissue, thus extending the boundaries of breast conserving surgery.
Footnotes
REPRODUCED BY PERMISSION OF HODDER EDUCATION With Acknowledgements to: Recent Advances in Surgery 32 Authors: Irving Taylor & Colin Johnson Permission Reference number: PERM/P/080312/PILLARISETTI
References
- 1.Skillman JM, Humzah MD, Brown IM, et al. The future of Breast Surgery: A new Subspecialty of oncoplastic breast surgeons. Breast. 2003;12:161–162. doi: 10.1016/S0960-9776(03)00023-7. [DOI] [PubMed] [Google Scholar]
- 2.Dobson AR. Subspecialty of oncoplastic breast surgery is needed to meet demand. BMJ. 2003;326:1165–1167. doi: 10.1136/bmj.326.7400.1165. [DOI] [Google Scholar]
- 3.McGlothin TDQ. Breast surgery as a specialized practice. Am J Surg. 2005;190:264–268. doi: 10.1016/j.amjsurg.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 4.Fisher B, Anderson S, Bryant J, et al. Twenty year follow up of a randomized trial comparing total mastectomy, lumpectomy and lumpectomy plus radiation for treatment of invasive breast cancer. N Eng J Med. 2002;347:1233–1241. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 5.Veronesi U, Cascinelli N, Mariani L, et al. Twenty year follow up of randomized study comparing breast conserving surgery with radical mastectomy for early breast cancer. N Eng J Med. 2002;347:1227–1232. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 6.Clarke M, Collins R, Darby S, et al. Effects of Radiotherapy and extent of surgery for early breast cancer on local recurrence and 15 year survival: an overview of randomized trials. Lancet. 2005;366(9503):2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 7.Petit J, Youssef O, Garusi C (2004) Oncoplastic and reconstructive surgery of the breast, Taylor Francis (text book), 10: 101
- 8.Petit J, Youssef O, Garusi C. Oncoplastic and reconstructive surgery of the breast. Taylor Francis (text book) 2004;10:102–108. [Google Scholar]
- 9.Nannelli A, Calabrese C, Cataliotti L, Querci della Rovere G. Oncoplastic and reconstructive surgery of the breast, vol 12. New York: Taylor Francis; 2004. pp. 115–125. [Google Scholar]
- 10.Masetti R, Pirulli PG, Magno S, et al. Oncoplastic techniques in conservative surgical treatment of the breast. Breast cancer. 2000;7:276–280. doi: 10.1007/BF02966389. [DOI] [PubMed] [Google Scholar]