Abstract
Incidentally discovered gallbladder cancer (IGBC) is defined as the gallbladder cancer (GBC) diagnosed during or after the cholecystectomy done for unsuspected benign gallbladder disease. Laparoscopic cholecystectomy (LC) is the most common procedure performed for benign gallbladder disease worldwide. Majority of GBC patients have associated gallstones. With the advent of ultrasonography more patients are being diagnosed with gallstones and are being subjected to cholecytectomy. IGBC is found in 0.2–2.9 % of all cholecytectomies done for gallstone disease. It represents 27–41 % of all GBC. Patients with IGBC having Tis and T1a stage, with negative cystic duct margin can be treated by simple cholecystectomy alone. Patients with stage T1b and beyond should undergo restaging, and should be treated with radical re - resection (R0). Residual disease is found in 40–76 % patients on re-exploration. The survival rates of patients undergoing re resection for IGBC is similar to those undergoing primary radical surgery. LC is contraindicated in patients with GBC. Patients presenting post LC should undergo radical re- resection and additional port site excision, as they have a high incidence of port site metastasis. At cholecystectomy for benign gallbladder disease all gallbladder specimens should be opened before closing abdomen and if available all suspicious specimens should be sent for immediate frozen section. All gallbladder specimens should be subjected to histopathology examination to avoid missing GBC. The surgeon should have a high index of suspicion for GBC if encountering difficult cholecystectomy for a benign disease, and in patients with atypical clinical and ultrasound findings in high incidence areas.
Keywords: Gallbladder cancer, Laparoscopic cholecystectomy, Incidental cancer
Introduction
Gallbladder cancer (GBC) is the fifth most common cancer of the gastrointestinal tract and the most common cancer of the biliary tract. GBC has been associated with a poor prognosis [1]. The prevalence of GBC varies considerably between geographic areas. The incidence is more in Native Americans, South American populations, people from Poland and Northern India [2]. The reports from various Indian population based cancer registries suggest that the GBC is more common in Northern India (Delhi and Bhopal) extending all over from the East to the West (Kolkata, North East and Punjab). It is the 4th commonest cancer in females in Delhi, 5th commonest in Bhopal, and 10th in Mumbai [3]. The incidence is low in Chennai (0.6 per 100 000 population) and in Bangalore (0.8 per 100 000 population), but recently statistically significant increase in GBC incidence rates has been reported for Mumbai, Chennai, and Bangalore [4]. Evarts Graham observed that gallstones were present in 69–100 % of cases of GBC and in turn GBC was found in 4.5–14 % of patients with gallstones [5]. Cholecystectomy (open/laparoscopic) is performed for patients with gallstone disease and benign gallbladder conditions. With greater availability of ultrasonography, cholecystectomy has become the commonest surgical procedure performed worldwide. As a result of this, there is an increase in the number of patients with incidentally discovered gallbladder cancer (IGBC).
Definition and Incidence of Incidental Gallbladder Cancer
The term incidental was coined to denote a ‘histological surprise’ of gallbladder cancer in a patient treated with simple cholecystectomy for gallstone disease, cholecystitis or gallbladder polyps. Incidental gallbladder cancer (IGBC) also called as occult/in apparent/missed GBC is defined as the GBC diagnosed during or after the cholecystectomy done for benign gallbladder disease. It is reported that GBC incidentally detected by histopathological examinations after open or laparoscopic cholecystectomy is encountered in 0.2–2.9 % of patients undergoing cholecystectomy [6]. Of all GBC 27–41 % are IGBC [6]. Most of these cases unsuspected pre-operatively belong to the category of pT1 and pT2 (early GBC) [7]. Many of these patients with disease labeled as IGBC have a radiological diagnosis suspicious for GBC, which has been over looked by the surgeon and the patient has been treated with a simple cholecystectomy alone.
Gallstone Disease (GSD) and Gallbladder Cancer (GBC)
The relative risk of developing GBC is 2–24 times for patients with cholelithiasis compared to those without gallstones [8]. GSD and GBC share same risk factors like female gender, increased age, fecundity and obesity. The odds ratio of developing GBC in patients with gallstones with diameter 2–2.9 cm and ≥ 3 cm compared with ≤1 cm diameter was 2.4 and 10.1 respectively[9]. The relationship to the number of stones is less clear. The dominant mechanism explained for the strong association of gallstones with cancer is the role of chronic inflammatory conditions within the gallbladder, leading to transformation from metaplasia to dysplasia and malignancy, with the inflammatory mediators also playing a major role [10, 11]. In patients with chronic cholecystitis and cholelithiasis a change in symptomatology of pain from intermittent to continuous, a suspicion for GBC should be done [12].
Laparoscopic Cholecystectomy and Port Site Recurrence
Laparoscopic cholecystyectomy (LC) is the most common procedure done for GSD in India. LC in patients with GBC has been associated with an increased incidence of peritoneal metastasis and port site recurrences. The incidence of port site recurrences in IGBC after LC was 0–40 % in various reported series [13–16]. The proposed theories for port site recurrences include gallbladder perforation and bile spillage, direct physical and chemical influence of pneumoperitoneum, improper specimen extraction and increased abdominal pressure on tumour cell diffusion [13, 14, 17]. Paolucci et al. reported an incidence of 17.1 % port site recurrence over a median period of 6 months after LC [14]. In a recent retrospective study from Memorial Sloan Kettering Cancer Centre, 69 patients after LC underwent definitive surgery with port site resection [18]. Port site recurrence was found in 13 patients (19 %) with T2 and T3 tumours. 77 % of patients with positive port site disease had peritoneal metastasis compared to 34 % of patients with no port site disease. They concluded that port site recurrence is associated with peritoneal recurrence and worse prognosis. We routinely excise port sites during radical re-resection after laparoscopic cholecystectomy for IGBC to prognosticate the disease and also to reduce the morbidity of the port site recurrence which might occur if the port sites are not excised.
Staging
International Union Against Cancer (UICC), TNM staging is the commonly used staging system for GBC (Table 1) [19]. GBC is staged according to the depth of invasion into the gallbladder wall and extent of spread to the surrounding structures and lymph nodes.
Table 1.
UICC TNM Staging for Gallbladder cancer (2009) [19]
| Primary Tumour (T): | |||
|---|---|---|---|
| Tx | Primary tumour could not be assessed | ||
| T0 | No evidence of primary tumour | ||
| Tis | Carcinoma in situ | ||
| T1 | Tumour invades lamina propria or muscular layer | ||
| T1a | Tumour invades lamina propria | ||
| T1b | Tumour invades muscular layer | ||
| T2 | Tumour invades perimuscular connective tissue; no extension beyond serosa or in to liver | ||
| T3 | Tumour perforates the serosa (visceral peritoneum) and/or directly invades the liver and/or one another organ or structure, such as the stomach, duodenum, colon, pancreas, omentum, or extra hepatic bile ducts | ||
| T4 | Tumour invades main portal vein or hepatic artery or invades two or more extra hepatic organs or structures | ||
| Regional Lymph Nodes (N): | |||
| Nx | Regional Lymph Nodes cannot be assessed | ||
| N0 | No Regional Lymph Node metastasis | ||
| N1 | Metastases to nodes along the cystic duct, common bile duct, common hepatic artery, and portal vein | ||
| Distant Metastasis (M): | |||
| M0 | No Distant Metastasis | ||
| M1 | Distant Metastasis | ||
| Staging Gruops | |||
| Stage 0 | Tis | N0 | M0 |
| Stage I | T1 | N0 | M0 |
| Stage II | T2 | N0 | M0 |
| Stage IIIA | T3 | N0 | M0 |
| Stage IIIB | T1-3 | N1 | M0 |
| Stage IVA | T4 | Any N | M0 |
| Stage IVB | Any T | Any N | M1 |
Management of Incidental Gallbladder Cancer
Surgical resection is the only potentially curative treatment for GBC. Only 10–30 % of GBC patients have resectable disease on presentation [2, 20]. Radical cholecystectomy is the standard surgical procedure performed for GBC [2]. The management of GBC including IGBC depends on the T stage (depth of invasion) [21, 22].
Radical cholecystecyomy (also called as extended cholecystectomy) includes en bloc removal of gallbladder and 2 cms or greater wedge resection of gallbladder bed (segments IV and V) and lymphnode dissection. Lymphadenectomy includes the clearance of all nodes along the portal structures (portal vein, hepatic artery and common bile duct), gastrohepatic ligament, retroduodenal, peripancreatic and coeliac axis lymphnodes. Some authors advocate bile duct resection for adequate nodal clearance but this procedure increases post operative morbidity. Common bile duct resection with hepatico-jejunostomy is recommended in IGBC when cystic duct margin is reported positive. The extent of liver resection for GBC is controversial and it ranges from non-anatomical (wedge resection) to anatomical liver resections including segments IVB and V resection, segments IV,V and VIII resection, right hepatectomy and trisegmentectomy (IV,V,VI,VII,VIII). Right hepatectomy is not recommended due to involvement of gallbladder bed which involves left lobe also (segment IV) [2, 23, 24]. The aim is to have negative margins of resection (R0). If the primary procedure was laparoscopic cholecystectomy, all ports should be excised in full thickness because of the possibility of port site dissemination and recurrence [25, 26].
For management guidelines, patients with IGBC can be divided into two clinical groups:
Those with GBC discovered during laparoscopic or open cholecystectomy for assumed benign disease.
Patients with GBC diagnosed histo-pathologically after simple cholecystectomy (open/laparoscopic) for benign gallbladder disease.
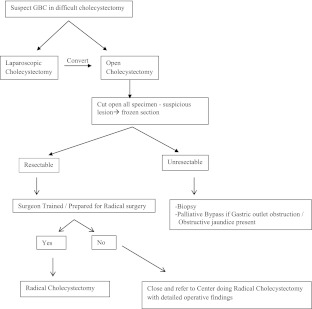
Algorithmic Approach for IGBC Discovered During Cholecystectomy
Preoperative diagnosis of early gall bladder cancer is difficult due to vague symptoms and signs as seen in GSD and chronic cholecystitis, lack of specific signs and equivocal imaging findings. Gallbladder cancer should be suspected on ultrasonography if there is a mass lesion (40–65 %), a polyp of size >10 mm (15–25 %) and focal or diffuse asymmetric wall thickening (20–30 %) or a porcelain gallbladder with wall calcifications [27].The algorithm for management of GBC discovered incidentally during cholecystectomy for GSD is given in Fig. 1. The surgeons should have a high index of suspicion for GBC in high incidence areas (Northern India) while operating benign gallbladder disease especially with atypical clinical and ultrasound findings. GBC should be suspected if the cholecystectomy is difficult, and if laparoscopic procedure is being done it should be converted to open surgery. All gallbladders removed for stone disease should always be cut opened and examined carefully for any suspicious lesions before closing incision. If suspicious lesion is present, the gallbladder should be sent for immediate frozen section for diagnosis and assessment of depth of invasion. If the GBC is confirmed and the surgeon is trained, radical cholecystectomy should be done. If not, the abdomen should be closed and patient should be referred to a higher centre for radical surgery with detailed description of operative findings. All gallbladder removed for gallstone disease should be subjected to histopathology examination.
Fig. 1.
Algorithmic approach for IGBC discovered during cholecystectomy for gallstone disease
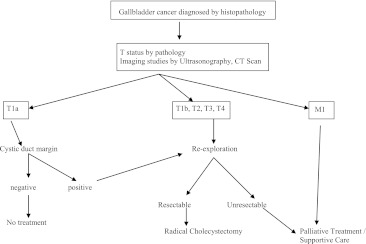
Algorithmic Approach for Incidental GBC After Cholecystectomy (Fig. 2)
Fig. 2.
Management of incidentally discovered carcinoma gallbladder on pathologic examination
Patients referred or seen with IGBC after simple cholecystectomy should get their pathological specimen or blocks reviewed for identification of the depth of invasion (T stage). Grade and location of the tumour (liver side/free peritoneal side), lymphatic, vascular and perineural invasion, positive cystic duct margin, or cystic duct node involvement are additional important information which should be looked for in the pathology report. The depth of invasion is important for planning further surgical treatment. Clinical examination of the patient should include assessment of performance status, presence of anemia and icterus, nutritional status, left supraclavicular (Virchow’s) node, hepatomegaly, mass in the abdomen, scar (port site) recurrence, ascites and per rectal examination for pelvic deposits. Liver function tests should be routinely performed. Contrast enhanced triphasic computed tomography (CT) scan/Magnetic resonance imaging (MRI) and chest x-ray should be done to look for residual disease, lymph nodes spread, metastasis and resectability. Multidetector CT (MDCT) has a reported accuracy of 85 % in the evaluation of the extent of local disease and in predicting resectability [28]. Positron emission tomography and computed tomography (PET-CT) does not have a role in routine imaging in GBC but has the potential to detect unsuspected metastasis, regional lymphadenopathy, peritoneal metastasis and residual disease in gallbladder bed (post cholecystectomy), but needs further investigation [29]. Prospective studies comparing CT/MRI/PET-CT to diagnose and stage GBC have not been performed. Serum CEA and CA 19.9 do not have any role in diagnosing residual disease in IGBC.
For patients with pTis and pT1a disease (only mucosal invasion) with the negative cystic duct margin, simple cholecystectomy is sufficient as the probability of nodal involvement is 0–2.5 % [30]. The 5 year survival rate after simple cholecystectomy itself reaches up to 100 % in pTis and pT1a patients [31–33]. In patients with positive cystic duct margin, re-exploration and bile duct resection should be done. Patients with pT1b (muscle invasion) tumours and beyond should undergo re-exploration and radical re-resection. The risk of lymph node metastasis is 16 % in pT1b disease [30]. There has been controversy regarding management of T1b IGBC. Wakai and colleagues reported that simple cholecystectomy in T1b disease has a 10 year survival rate of 87 % [33]. However others have reported that radical cholecystectomy for pT1b disease has a better outcome and increased survival (72–100 %) compared to simple cholecystectomy [20, 30, 34, 35]. Ouchi et al. [34] reported a 100 % survival following radical cholecystectomy for T1b GBC compared to 42 % following simple cholecystectomy. In a German registry report for IGBC [35] radical re- resection improved 5 year survival for T1b IGBC from 40 % for simple cholecystectomy to 72 %. Majority recommend radical re - resection for T1b cancers.
Patients with pT2 tumours (perimuscular connective tissue invasion) should be treated with radical cholecystectomy in the form of segment IVB, V liver resection along with lymphadenectomy. Since there is no serosal layer at the gallbladder fossa and the thicker cystic plate is invariably left behind after simple cholecystectomy, IVB and V segment resection is mandatory [36]. The reported incidence of lymph node metastasis in pT2, T3 and T4 stages were 39–54 %, 62 % and 69 % respectively [37, 38]. Residual tumour is found in 40–76 % of patients during re-explorations in pT2 patients [31, 39]. Radical cholecystectomy increased the 5 year survival rate from 20 % (simple cholecystectomy) to 70 % (radical cholecystectomy) in T2 disease [32]. Involvement of adjacent organs like colon and duodenum are not contraindications to radical re-resections [2, 24]. Radical re-resection with extended liver resections and pancreatico-duodenectomies in a few subsets of selected pT3 and pT4 patients has shown survival benefit with high rates of morbidity and mortality [2, 12, 24, 37]. Patients with pT3 and pT4 disease who are unresectable on re-exploration or having metastatic disease should be treated with palliative chemotherapy if the performance status is acceptable. Patients with gastric outlet obstruction due to duodenal infiltration can be palliated surgically with gastrojejunostomy bypass and those with jaundice can be palliated endoscopically with biliary stenting. There is no definitive role for adjuvant chemotherapy in GBC, but should be considered in high risk cases [2]. Since GBC has local and distant spread there is no role of radiotherapy in adjuvant and palliative settings. Gemcitabine and cisplatin have shown good response and survival benefit in advanced GBC in a palliative setting [40].
There are no guidelines for the timing for re-resection; patients should be taken for surgery as early as possible. We re-explore patients presenting with IGBC within 3 months of simple cholecystectomy.
Survival Rates After Re-resection for IGBC (Table 2)
Table 2.
5 year Survival rates* of patients with Gallbladder cancer
| T Stage | LN Metastasis (%) | 5 year SR after SC | 5 year SR after RC | 5 year SR after Re-resection |
|---|---|---|---|---|
| pT1a | 2.5 % [30] | 85–100 % [33, 34], 71 % [34] | 100 % [34] | - |
| pT1b | 16 % [30] | 42 % [34], 40 % [35] 87 % (10 year survival) [33] | 100 % [34] | 79 % [35] |
| pT2 | 39–54 % [38] 47 % [37, 38] | 19–40 % [31, 38], 20 % [32], 19 % [37], 50 % [7] | 70 % [32], 61 % [37], 100 % [7] | 80–90 % [31, 37] |
| pT3 | 62 % [37, 38] | 0 % [41] | 15–63 % [30] | 21 % [37] |
| pT4 | 69 % [37, 38] | 0 % [41] | 7–25 % [30] | 28 % [37] |
*References in square brackets
Abbreviations - LN (lymph node metastasis), RC (radical cholecystectomy), SC (simple cholecystectomy), SR (survival rates)
Foster et al. [41] studied the survival following radical resection and re-resection in GBC patients with T2, 3, 4 diseases. Of the 64 patients evaluated, 8 (T3) patients were unresectable,18 patients (10 T2, 8 T3) underwent simple cholecystectomy, 10 patients (2 T2, 2 T3 and 6 T4) patients underwent radical cholecystectomy and 9 patients (7 T2, 2 T3) radical re-resection. The estimated 5 year survival was 78 % with radical cholecystectomy and 38 % with simple cholecystectomy for T2 patients; and 25 % with radical surgery and 0 % with simple cholecystectomy for T3 patients. There was no significant survival difference in primary radical versus radical re-resection groups in T2 and T3 patients [41]. Similarly, Fong et al. showed that there was no statistically significant difference in long term survival after curative radical resection as single procedure versus two procedures (radical re-resection after simple cholecystectomy) and also there was no survival difference in delayed versus immediate re-resection groups [37]. Several studies have shown an increase in the 5 year survival rates of T2 patients from 19 % to 61 % [37], and 20 % to 70 % [32] following simple versus radical cholecystectomy respectively. The 5 year survival rates of T3 and T4 patients are poor after simple cholecystectomy as shown in Table 2.
Conclusion
Gallbladder cancer is one of the commonest cancers in North India. With the greater availability of ultrasonography, cholecystectomy has become the commonest procedure performed worldwide and hence an increase in the incidence of IGBC also. For patients with stage Tis and T1a GBC without positive cystic duct margin, a simple cholecystectomy is sufficient. For stages T1b and beyond, re-exploration and radical re-resection is the standard procedure of choice. If the primary procedure is LC, then all the port sites should be excised during re-resection. The survival rates are better for patients undergoing radical re- resection than simple cholecystectomy for stages T1b and beyond. Survival rates for primary radical surgery and re-resection surgery are equivalent. Controversies exist regarding the timing of re-surgery. Role of adjuvant chemotherapy in GBC needs to be studied. Gemcitabine and cisplatin have shown survival benefit in advanced GBC. Surgeons should maintain a high index of suspicion while performing cholecystectomy for gallstone disease especially in high incidence areas.
Acknowledgments
Conflicts of Interest
Authors have no conflicts of interest.
Source of Support
Nil
References
- 1.Piehler JM, Crichlow RW. Primary carcinoma of the gallbladder. Surg Gynecol Obstet. 1978;147:929–942. [PubMed] [Google Scholar]
- 2.Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003;4:167–176. doi: 10.1016/S1470-2045(03)01021-0. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Registry Programme (ICMR) (2008) Two-year report of the population based cancer registries: 2004–2005 Bangalore, India
- 4.Murthy NS, Rajaram D, Gautam MS, et al. Trends in incidence of gallbladder cancer – Indian scenario. Gastrointestinal Cancer: Targets and Therapy. 2011;1:1–9. [Google Scholar]
- 5.Graham E. The prevention of carcinoma of the gallbladder. Ann Surg. 1931;93:317–322. doi: 10.1097/00000658-193101000-00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toyonaga T, Chijiiwa K, Nakano K, et al. Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma. World J Surg. 2003;27:266–271. doi: 10.1007/s00268-002-6609-9. [DOI] [PubMed] [Google Scholar]
- 7.Wakai T, Shirai Y, Hatakeyama K. Radical second resection provides survival benefit with T2 gallbladder carcinoma first discovered after laparoscopic cholecystectomy. World J Surg. 2002;26:867–871. doi: 10.1007/s00268-002-6274-z. [DOI] [PubMed] [Google Scholar]
- 8.Gurleyik G, Gurleyik E, Ozturk A, et al. Gallbladder carcinoma associated with gallstones. Acta Chir Belg. 2002;102:203–206. doi: 10.1080/00015458.2002.11679296. [DOI] [PubMed] [Google Scholar]
- 9.Diehl AK. Gallstone size and the risk of gallbladder cancer. JAMA. 1983;250:2323–2326. doi: 10.1001/jama.1983.03340170049027. [DOI] [PubMed] [Google Scholar]
- 10.Tazuma S, Kajiyama G. Carcinogenesis of malignant lesions of the gall bladder. The impact of chronic inflammation and gallstones. Langenbecks Arch Surg. 2001;386:224–229. doi: 10.1007/s004230100220. [DOI] [PubMed] [Google Scholar]
- 11.Duarte I, Llanos O, Domke H, et al. Metaplasia and precursor lesions of gallbladder carcinoma. Frequency, distribution, and probability of detection in routine histologic samples. Cancer. 1993;72:1878–1884. doi: 10.1002/1097-0142(19930915)72:6<1878::AID-CNCR2820720615>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 12.Misra NC, Misra S, Chaturvedi A. Epidemiology, etiology and new perspective in carcinoma gallbladder. Indian J Surg. 1998;60:167–175. [Google Scholar]
- 13.Varshney S, Buttirini G, Gupta R. Incidental carcinoma of the gallbladder. Eur J Surg Oncol. 2002;28:4–10. doi: 10.1053/ejso.2001.1175. [DOI] [PubMed] [Google Scholar]
- 14.Paolucci V. Port-site recurrences after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2001;8:535–543. doi: 10.1007/s005340100022. [DOI] [PubMed] [Google Scholar]
- 15.Lundberg O, Kristoffersson A. Port site metastases from gallbladder cancer after laparoscopic cholecystectomy. Results of a Swedish survey and review of published reports. Eur J Surg. 1999;165:215–222. doi: 10.1080/110241599750007072. [DOI] [PubMed] [Google Scholar]
- 16.Hu JB, Sun XN, Xu J, He C. Port site and distant metastases of gallbladder cancer after laparoscopic cholecystectomy diagnosed by positron emission tomography. World J Gastroenterol. 2008;14:6428–6431. doi: 10.3748/wjg.14.6428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouvy ND, Marquet RL, Jeekel H, Bonjer HJ, Collin J, Encke A, Johnson AG. Impact of gas(less) laparoscopy and laparotomy on peritoneal tumour growth and abdominal metastases. Ann Surg. 1996;224:694–701. doi: 10.1097/00000658-199612000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maker AV, Butte JM, Oxenberg J, Kuk D, Gonen M, Fong Y, Dematteo RP, D'Angelica MI, Allen PJ, Jarnagin WR. Is port site resection necessary in the surgical management of gallbladder cancer? Ann Surg Oncol. 2012;19:409–417. doi: 10.1245/s10434-011-1850-9. [DOI] [PubMed] [Google Scholar]
- 19.Sobin LH, Gospodarowicz MK, Wittekind Ch (2009) Digestive system: gallbladder. TNM classification of malignant tumours, seventh edition-Wiley-Blackwell publication; Digestive system tumours, Gallbladder cancer: pp 118–121
- 20.Misra S, Chaturvedi A, Misra NC. Gallbladder cancer. Curr Treat Options Gastroenterol. 2006;9:95–106. doi: 10.1007/s11938-006-0028-1. [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi K, Tsuncyoshi M. Subclinical gallbladder carcinoma. Am J Surg. 1992;16:382–386. doi: 10.1016/0002-9610(92)90038-S. [DOI] [PubMed] [Google Scholar]
- 22.Onoyama H, Yamamoto M, Tseng A, Ajiki T, Saitoh Y. Extended cholecystectomy for carcinoma of the gallbladder. World J Surg. 1995;19:758–763. doi: 10.1007/BF00295925. [DOI] [PubMed] [Google Scholar]
- 23.Misra NC, Misra S, Chaturvedi A (1997) Carcinoma of the Gallbladder. – “Recent Advances in Surgery -20. Editors - C.D. Johnson, I Taylor. Publisher -Churchill Livingstone, London, pp 69–87
- 24.Misra S, Chaturvedi A, Misra NC. Gallbladder cancer: surgical management. Ind J Med Ped Oncol. 2005;26:46–53. [Google Scholar]
- 25.Fong Y, Heffernan N, Blumgart LH. Gallbladder carcinoma discovered during laparoscopic cholecystectomy: aggressive reresection is beneficial. Cancer. 1998;83:423–427. doi: 10.1002/(SICI)1097-0142(19980801)83:3<423::AID-CNCR9>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 26.Misra NC, Misra S, Chaturvedi A, et al (2002) Epidemiology, aetiology and multimodal therapy in cancer gallbladder with special reference to radical surgery and newer chemotherapy protocols: A prospective study of 631 patients. Proceedings of the American Society of Clinical Oncology Pan Asia Cancer conference, New Delhi, India. pp 85–87
- 27.Furlan A, Ferris JV, Hosseinzadeh K, Borhani AA. Gallbladder carcinoma update: multimodality imaging evaluation, staging, and treatment options. AJR Am J Roentgenol. 2008;191:1440–1447. doi: 10.2214/AJR.07.3599. [DOI] [PubMed] [Google Scholar]
- 28.Kalra N, Suri S, Gupta R, Natarajan SK, Khandelwal N, Wig JD, Joshi K. MDCT in the staging of gallbladder carcinoma. AJR Am J Roentgenol. 2006;186:758–762. doi: 10.2214/AJR.04.1342. [DOI] [PubMed] [Google Scholar]
- 29.Corvera CU, Blumgart LH, Akhurst T, DeMatteo RP, D'Angelica M, Fong Y, Jarnagin WR. 18 F-fluorodeoxyglucose positron emission tomography influences management decisions in patients with biliary cancer. J Am Coll Surg. 2008;206:57–65. doi: 10.1016/j.jamcollsurg.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Ogura Y, Mizumoto R, Isaji S, et al. Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg. 1991;15:337–343. doi: 10.1007/BF01658725. [DOI] [PubMed] [Google Scholar]
- 31.Shirai Y, Yoshida K, Tsukada K, et al. Inapparent carcinoma of the gallbladder: an appraisal of a radical second operation after simple cholecystectomy. Ann Surg. 1992;215:326–331. doi: 10.1097/00000658-199204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aretxabala X, Roa IS, Burgos LA, et al. Curative resection in potentially resectable tumours of the gallbladder. Eur J Surg. 1997;163:419–426. [PubMed] [Google Scholar]
- 33.Wakai T, Shirai Y, Yokoyama N, et al. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001;88:675–678. doi: 10.1046/j.1365-2168.2001.01749.x. [DOI] [PubMed] [Google Scholar]
- 34.Ouchi K, Suzuki M, Tominaga T, et al. Survival after surgery for cancer of the gallbladder. Br J Surg. 1994;81:1655–1657. doi: 10.1002/bjs.1800811131. [DOI] [PubMed] [Google Scholar]
- 35.Goetze TO, Paolucci V. Immediate re-resection of T1 incidental gallbladder carcinomas: a survival analysis of the German Registry. Surg Endosc. 2008;22:2462–2465. doi: 10.1007/s00464-008-9747-9. [DOI] [PubMed] [Google Scholar]
- 36.Gall FP, Kockerling F, Scheels J, et al. Radical operations for carcinoma of the gallbladder: present in Germany. World J Surg. 1991;15:328–336. doi: 10.1007/BF01658724. [DOI] [PubMed] [Google Scholar]
- 37.Fong Y, Jarnagin W, Blumgart LH. Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg. 2000;232:557–569. doi: 10.1097/00000658-200010000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yildirim E, Celen O, Gulben K, et al. The surgical management of incidental gallbladder carcinoma. Eur J Surg Oncol. 2005;31:45–52. doi: 10.1016/j.ejso.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 39.De-Aretxabala X, Roa I, Burges L, et al. Gallbladder cancer in Chile: a report on 54 potentially resectable tumours. Cancer. 1992;69:60–65. doi: 10.1002/1097-0142(19920101)69:1<60::AID-CNCR2820690112>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 40.Misra S, Chaturvedi A, Misra NC. Gemcitabine (G) plus cisplatin (C) in advanced carcinoma gallbladder - A large single centre experience. J Clin Oncol. 2005;23:341. [Google Scholar]
- 41.Foster JM, Hoshi H, Gibbs JF, Iyer R, Javle M, Chu Q, Kuvshinoff B. Gallbladder cancer: defining the indications for primary radical resection and radical re-resection. Ann Surg Oncol. 2007;14:833–840. doi: 10.1245/s10434-006-9097-6. [DOI] [PubMed] [Google Scholar]