Abstract
Surgery has increasingly become a technology-driven specialty. Robotic assistance is considered one innovation within abdominal surgery over the past decade that has the potential to compensate for the drawbacks of conventional laparoscopy. The dramatic evolution of robotic surgery over the past 10 years is likely to be eclipsed by even greater advances over the next decade. We review the current status of robotic technology in surgery. The Medline database was searched for the terms “robotic surgery, telesurgery, and laparoscopy.” A total of 2,496 references were found. All references were considered for information on robotic surgery in advanced laparoscopy. Further references were obtained through cross-referencing the bibliography cited in each work. There is a paucity of control studies on a sufficient number of subjects in robot-assisted surgeries in all fields. Studies that meet more stringent clinical trials criteria show that robot-assisted surgery appears comparable to traditional surgery in terms of feasibility and outcomes but that costs associated with robot-assisted surgery are higher because of longer operating times and expense of equipment. While a limited number of studies on the da Vinci robotic system have proven the benefit of this approach in regard to patient outcomes, including significantly reduced blood loss, lower percentage of postoperative complications, and shorter hospital stays, there are mechanical and institutional risks that must be more fully addressed. Robotic assistance will remain an intensively discussed subject since clinical benefits for most procedures have not yet been proven. While the benefit still remains open to discussion, robotic systems are spreading and are available worldwide in tertiary centers.
Keywords: Robotic surgery, Laparoscopy, Minimally invasive surgery
Introduction
Reduced analgesic use, faster recovery, improved cosmesis and reduced wound complications are the major benefits of minimally invasive surgery for the patient. These benefits are the reason for the worldwide distribution of laparoscopy and explain why minimally invasive techniques are considered standard of care for certain operations, such as cholecystectomy, fundoplication, adrenalectomy, and bariatric surgery [1–5]. Minimally invasive techniques have recently broadened their applicability, moving from simple ablative procedures to more sophisticated reconstructive surgery requiring manipulation in a narrow working space or at non-ergonomic angles for conventional laparoscopy [6, 7]. In these cases, the shortcomings of conventional laparoscopy became more evident, especially the limited degrees of freedom (df), two-dimensional (2D) view, restricted ergonomics for the surgeon, and the absence of wrist gear [7]. Robotic systems have recently been introduced in an attempt to reduce the difficulty involved in performing complex laparoscopic procedures, particularly for non-laparoscopic surgeons [8, 9]. The presence of three-dimensional (3D) magnification and tools with 7 df that are able to duplicate hand movements with high accuracy have allowed many surgeons to hypothesise that, despite the absence of tactile feedback, the application of robotic surgery might yield real advantages, not only in terms of shorter learning curves but also in the ability to improve overall outcomes. We review the current status of robotic technology in surgery.
Methods
The Medline database was searched for the terms “robotic surgery, telesurgery, and laparoscopy.” A total of 2,496 references were found. All references were considered for information on robotic surgery in advanced laparoscopy. Further references were obtained through cross-referencing the bibliography cited in each work. Abstract forms, titles, and abstracts of full papers were manually checked for relevance by authors. Based on their judgment, 39 articles were finally considered eligible for inclusion in this review.
Results
Clinical Studies
Although some important handicaps of laparoscopic surgery have been successfully addressed by the da Vinci® surgical system (DVS), in practice new challenges arise, such as more complicated handling of the equipment, high costs and—for the anesthesiologist—impaired access to the patient for certain procedures (i.e., esophageal surgery). Currently, the DVS is routinely used in a variety of settings. Among those, the most important and most prevalent are urology, gynecology and abdominal surgery. In their 2010 Annual Report, Intuitive surgical Inc. clearly states that over 70 % of the overall procedures carried out with the DVS are for prostatectomy and hysterectomy. Other procedures are still less common, with gynecology showing the highest growth rate [10].
Urology
In 2000, Binder et al. performed the first robot-assisted radical prostatectomy, closely followed by other European centers [11]. In 2001, Intuitive Surgical received FDA clearance for the DVS in prostate surgery. At that time, most prostatectomies were performed as open procedures (OPs) because of the technical difficulty of the laparoscopic technique (LP) resulting in a long learning curve. The meticulous nerve-sparing preparation at the prostate and intra-corporeal suturing requires dedicated laparoscopic training due to their high complexity. Therefore, urologists accepted the DVS with delight as it enabled them to perform a laparoscopic robot-assisted approach (RALP). It allowed for a more ergonomic position and an easy handling of sutures due to its additional df.
Most studies, therefore, tend to show the benefits of laparoscopic surgery transferred on to the formerly open prostatectomy. In a series of 60 patients, Ahlering et al. found reduced hospital stay (1.0 vs. 2.2 days), less blood loss (103 vs. 418 ml), while cancer control was not significantly different [12]. Similarly, in a prospective analysis of 30 patients, Menon et al. showed faster recovery and return to normal activities as well as lower postoperative pain levels compared to OP [13]. In a matched-pair analysis of 120 patients, Rocco et al. affirmed that RALP resulted in shorter hospital stay (3 vs. 6 days) and less blood loss (200 vs. 800 ml) as well as equally effective cancer control. They also stated a faster return of urinary function in terms of return of continence for RALP compared to OP at 3 months (70 % vs. 63 %) and 12 months (97 % vs. 88 %). In addition, the potency recovery rate of RALP was better than OP at 3 months (31 % vs. 18 %) and 12 months (61 % vs. 41 %) postoperatively [14]. This was confirmed by Ficarra et al. in a prospective trial of 105 patients. The mean time of continence for LP compared with OP was 75 vs. 25 days; and at the 12-month follow-up, 81 % of RALP patients who underwent bilateral nerve-sparing recovered erectile function compared to 49 % of OP. There was no difference in terms of oncologic outcome [15]. Both studies revealed a longer operative time.
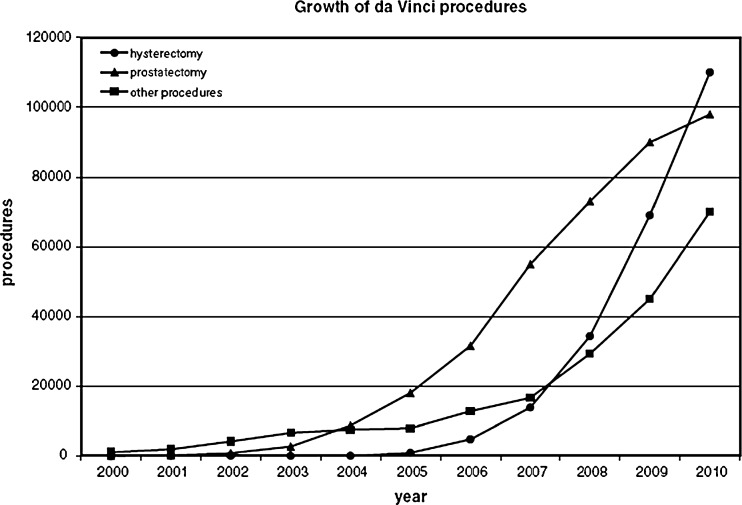
Additionally, good marketing of Intuitive Surgical Inc. led to high patient demand. This also led to a rapid increase of robotic prostatectomies worldwide (Fig. 1). The market share of robotic prostatectomy compared to laparoscopic and open prostatectomy is estimated as exceeding 80 % in the USA, according to the manufacturer of the DVS [10]. Other procedures such as partial nephrectomy, cystectomy, and pyeloplasty are increasingly being performed with robotic assistance. Interestingly, the growth of robotic prostatectomy was exponential, reaching its saturation in recent years. This was visible by a declining rate of growth, as seen in Fig. 1.
Fig. 1.
Growth rates of DVS procedures; data, Intuitive Surgical Inc.[10]
Gynecology
Robotic surgery was adapted relatively late for gynecology, starting in 2006. Operations performed in gynecology comprise hysterectomy, myomectomy plus sacrocolpopexy. In general, the standard laparoscopic technique in the pelvis requires extensive training and technical skills due to restricted working field, particularly when intracorporal suturing is necessary. In particular, improved ergonomics and the easier performance of sutures has led to a rapid increase of robotic procedures in gynecology, predominantly for hysterectomy [16]. In a series of 20 patients, Fiorentino et al. found that robot- assisted laparoscopic hysterectomies (RALH) are safe and feasible, and that suturing is more easily performed with the robot [17]. In a case–control study of 100 patients comparing laparoscopic hysterectomy (LH) with RALH, Payne et al. showed that RALH led to reduced blood loss (113 vs. 61 ml) and shorter hospital stay (1.6 vs. 1.1 days).
In a retrospective analysis comparing open with robot- assisted myomectomy in 58 patients, Advincula et al. revealed that blood loss (196 ml vs. 365 ml) and length of stay (1.5 vs. 3.6 days) were significantly lower for RALH. The operative time for the robotic group, however, was significantly longer (231 vs. 154 min) [18].
The robotic technique for sacrocolpopexy also permits the replacement of formerly open procedures by the laparoscopic technique on a larger scale. Elliott et al. stated that suturing and handling of the tissue was easier for robotic abdominal sacrocolpopexy [19].
In a recent meta-analysis, Reza et al. assessed the current state of robotics in gynecology, reviewing 21 controlled studies, though none of the studies included were randomized. In this review, robotic procedures showed a shorter hospital stay and less blood loss when compared to open surgery. Compared to conventional laparoscopic surgery robotically assisted laparosocpic surgery showed reduced blood loss and less frequent conversion for the staging of endometrial cancer [16].
The increase in gynecological procedures in recent years is substantial, and in its growth rate gynecology exceeds the adoption of robotic technology in urology. In addition, in terms of procedures carried out, robotic hysterectomy outnumbered robotic prostatectomy in 2010. The saturation has not been reached yet and the growth of robotic use for gynecological procedures is still exponential (Fig. 1)
Abdominal Surgery
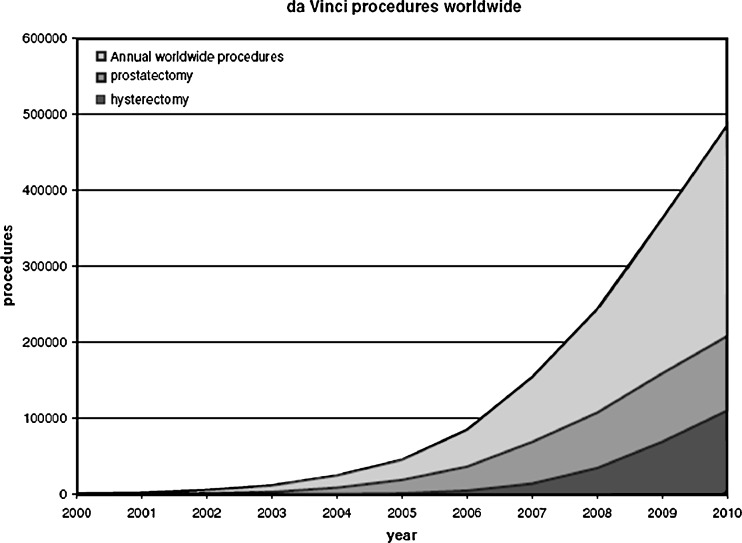
The first experiences with the da Vinci system have been made in general surgery. Though in terms of patients treated, gynecology and urology far outweigh abdominal surgery (Fig. 2). The benefits of robotic technology include the improvement of orientation and dexterity, especially in small spaces when suturing is needed or the instruments are in un-ergonomic angles. For general surgery, specifically fundoplication, rectal resection and gastric bypass pose these difficulties.
Fig. 2.
Cumulative da Vinci procedures worldwide; data, Intuitive Surgical Inc. [10]
In a recent meta-analysis of robotic vs. laparoscopic Nissen fundoplication, Maeso et al. conducted six randomized controlled trials with a total of 226 patients [20]. They found no significant difference in terms of need for reoperation, postoperative mortality, postoperative dysphagia, hospital stay, or operative complications. They found longer operative time although the results in the studies showed a high heterogeneity. In one of the reviewed studies, Morino et al. reported in a randomized controlled trial on robotic versus conventional laparoscopic Nissen fundoplication in 50 patients the robotic technique to be safe, feasible, and with a similar outcome. Especially suturing tasks were performed easier. Although he reported that mean total operation time (131.3 vs. 91.1 min) as well as skin-to-skin time (78.0 vs. 63.5 min) were longer. In terms of length of hospital stay as well as clinical and functional outcomes, there was no significant difference found between the groups [21]. In another reviewed randomized controlled trial in 40 patients, Muller-Stich et al. found a significantly reduced operation time of the robotic system (88 vs. 102 min), which was explained by trained personnel operating on patients [22].
Robotic-assisted colorectal dissection has been reported to be safe and feasible by several authors. At present, there is only one single randomized controlled trial by Baik et al. [21]. When comparing robotic vs. laparoscopic mesorectal excision in 36 patients, they found no significant difference in terms of operating time, hemoglobin change, and conversion rate while showing equal oncological radicality. However, a reduced hospital stay was found within the robotic group (6.9 vs. 8.7 days). In a comparative study of robotic vs. laparoscopic gastric bypass surgery involving 90 patients, Hubens et al. reported on the benefits of robotic systems, especially regarding suturing abilities, for the creation of the gastrojejunostomy. They found a significantly reduced operation time for the laparoscopic technique (127 vs. 212 min) but reported that the learning curve was comprised in this data, and that the last ten cases showed similar operation times to the laparoscopic technique. They also noted a higher conversion rate for the robotic technique. Postoperative complications showed no difference between the groups [22].
In a recent systematic review, Mirnezami et al. evaluated 17 studies (9 case series, 7 comparative studies, and 1 randomized controlled trial) involving 288 patients, comparing robotic vs. laparoscopic colorectal surgery. Due to the heterogeneity of the performed procedures and insufficient evidence levels, a meta-analysis could not be performed. The data showed high heterogeneity in terms of operative time and hospital stay. Blood loss, however, seemed to be reduced. Nevertheless, robotic colorectal surgery in general was considered to be safe and feasible [23].
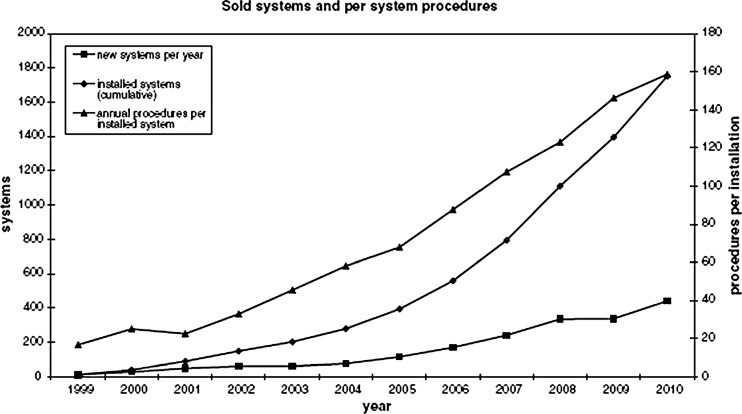
Cost Analysis
A new da Vinci Si® surgical system with HD vision costs around €1.7 million, plus the yearly maintenance cost of about 10 % of the initial purchase. Several cost analyses have been performed and have indicated that robotic surgery is more costly than conventional open surgery. The initial, maintenance, and instrument costs thus result in a more expensive procedure. In a recent analysis of 643 cases (262 RALP, 220 LP, and 161 OP), Bolenz et al. reported that the robotic approach is 1.5 times more expensive than the open approach, based on an average of 126 patients per year. The main difference was seen in surgical supply cost that was ten times higher and operating room costs that were 1.7 times higher, caused by longer operation times. When considering purchase and maintenance costs for the robot, the financial burden increased by $2,698 per patient, given an average of 126 cases per year [24]. Muller-Stich et al., however, found for fundoplication that also in the case of a shorter operation time compared to the conventional technique the cost of the robotic procedure are still higher by 18 % (3,244 € vs. 2,743 €) [20]. Nonetheless, the DV is a very expensive tool Intuitive Surgical Inc. succeeds in selling more systems each year. In 2010, an additional 441 systems were sold and 1,752 systems were installed worldwide. In terms of cost effectiveness, all studies showed higher efficiency when utilization was high. In Fig. 3, it can be seen that the amount of systems installed per year has been growing steadily. Also procedures per installed system are increasing, peaking at 159 per year for 2010, suggesting higher overall utilization.
Fig. 3.
Overview of sold systems, installations, and procedures per DVS per year; data, Intuitive Surgical Inc. [10]
Conclusion
For both prostatectomy and hysterectomy, the robotic approach allow the benefits of laparoscopic surgery such as fewer blood loss, less postoperative pain, better cosmesis, and a faster return to physical activity to the formerly open procedures. Thus, the well-known benefits of laparoscopy over open surgery account for better results in clinical studies. Similarly, in abdominal surgery, the robotic and conventional laparoscopic approaches can be regarded as equivalent in terms of patient care. But regarding cost, the robotic approach is more expensive. However, despite not having shown their difference in a sufficient number of high quality clinical studies, it is the most commonly performed operation in the USA for complex pelvic procedures, such as hysterectomy and prostatectomy. Prostatectomy was the most well known robotic procedure for a long time and is still seen as a prototype for robotic surgery. However, in terms of numbers, in 2010, robotic hysterectomy overtook LARP, and the curve progression of procedures does not suggest a narrowing peak.
The most important drawbacks of the DVS are its long setup time, mostly longer operation time and high cost. Using trained personnel can lower setup and operation time.
Robotic assistance will remain an intensively discussed subject since clinical benefits for most procedures have not yet been proven. While the benefit still remains open to discussion, robotic systems are spreading and are available worldwide in tertiary centers.
Acknowledgments
Conflicts of interest
None
References
- 1.Assalia A, Gagner M. Laparoscopic adrenalectomy. Br J Surg. 2004;91(10):1259–1274. doi: 10.1002/bjs.4738. [DOI] [PubMed] [Google Scholar]
- 2.Catarci M, Gentileschi P, Papi C, Carrara A, Marrese R, Gaspari AL, Grassi GB. Evidence-based appraisal of antireflux fundoplication. Ann Surg. 2004;239(3):325–337. doi: 10.1097/01.sla.0000114225.46280.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sauerland S, Angrisani L, Belachew M, Chevallier JM, Favretti F, Finer N, Fingerhut A, Garcia Caballero M, Guisado Macias JA, Mittermair R, Morino M, Msika S, Rubino F, Tacchino R, Weiner R, Neugebauer EA. Obesity surgery: evidence-based guidelines of the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2005;19(2):200–221. doi: 10.1007/s00464-004-9194-1. [DOI] [PubMed] [Google Scholar]
- 4.Gupta PK, Natarajan B, Pallati PK, Gupta H, Sainath J, Fitzgibbons RJ., Jr Outcomes after laparoscopic adrenalectomy. Surg Endosc. 2011;25(3):784–794. doi: 10.1007/s00464-010-1256-y. [DOI] [PubMed] [Google Scholar]
- 5.Keus F, Jong JA, Gooszen HG, Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;4:CD006231. doi: 10.1002/14651858.CD006231. [DOI] [PubMed] [Google Scholar]
- 6.Frede T, Stock C, Renner C, Budair Z, Abdel-Salam Y, Rassweiler J. Geometry of laparoscopic suturing and knotting techniques. J Endourol. 1999;13(3):191–198. doi: 10.1089/end.1999.13.191. [DOI] [PubMed] [Google Scholar]
- 7.Kenngott HG, Muller-Stich BP, Reiter MA, Rassweiler J, Gutt CN. Robotic suturing: technique and benefit in advanced laparoscopic surgery. Minim Invasive Ther Allied Technol. 2008;17(3):160–167. doi: 10.1080/13645700802103381. [DOI] [PubMed] [Google Scholar]
- 8.Rassweiler J, Safi KC, Subotic S, Teber D, Frede T. Robotics and telesurgery—an update on their position in laparoscopic radical prostatectomy. Minim Invasive Ther Allied Technol. 2005;14(2):109–122. doi: 10.1080/13645700510010908. [DOI] [PubMed] [Google Scholar]
- 9.Carswell CM, Clarke D, Seales WB. Assessing mental workload during laparoscopic surgery. Surg Innov. 2005;12(1):80–90. doi: 10.1177/155335060501200112. [DOI] [PubMed] [Google Scholar]
- 10.Annual report 2010 (2011) Intuitive Surgical Inc
- 11.Binder J, Kramer W. Robotically assisted laparoscopic radical prostatectomy. BJU Int. 2001;87(4):408–410. doi: 10.1046/j.1464-410x.2001.00115.x. [DOI] [PubMed] [Google Scholar]
- 12.Ahlering TE, Woo D, Eichel L, Lee DI, Edwards R, Skarecky DW. Robot-assisted versus open radical prostatectomy: a comparison of one surgeon’s outcomes. Urology. 2004;63(5):819–822. doi: 10.1016/j.urology.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 13.Menon M, Tewari A, Baize B, Guillonneau B, Vallancien G. Prospective comparison of radical retropubic prostatectomy and robot-assisted anatomic prostatectomy: the Vattikuti Urology Institute experience. Urology. 2002;60(5):864–868. doi: 10.1016/S0090-4295(02)01881-2. [DOI] [PubMed] [Google Scholar]
- 14.Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, Mastropasqua M, Santoro L, Detti S, Cobelli O. Robotic vs. open prostatectomy in a laparoscopically naive centre: a matched-pair analysis. BJU Int. 2009;104(7):991–995. doi: 10.1111/j.1464-410X.2009.08532.x. [DOI] [PubMed] [Google Scholar]
- 15.Ficarra V, Novara G, Fracalanza S, D’Elia C, Secco S, Iafrate M, Cavalleri S, Artibani W. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009;104(4):534–539. doi: 10.1111/j.1464-410X.2009.08419.x. [DOI] [PubMed] [Google Scholar]
- 16.Reza M, Maeso S, Blasco JA, Andradas E. Meta-analysis of observational studies on the safety and effectiveness of robotic gynaecological surgery. Br J Surg. 2010;97(12):1772–1783. doi: 10.1002/bjs.7269. [DOI] [PubMed] [Google Scholar]
- 17.Fiorentino RP, Zepeda MA, Goldstein BH, John CR, Rettenmaier MA. Pilot study assessing robotic laparoscopic hysterectomy and patient outcomes. J Minim Invasive Gynecol. 2006;13(1):60–63. doi: 10.1016/j.jmig.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Advincula AP, Xu X, St G, Ransom SB. Robot-assisted laparoscopic myomectomy versus abdominal myomectomy: a comparison of short-term surgical outcomes and immediate costs. J Minim Invasive Gynecol. 2007;14(6):698–705. doi: 10.1016/j.jmig.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 19.Elliott DS, Krambeck AE, Chow GK. Long-term results of robotic assisted laparoscopic sacrocolpopexy for the treatment of high grade vaginal vault prolapse. J Urol. 2006;176(2):655–659. doi: 10.1016/j.juro.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 20.Muller-Stich BP, Reiter MA, Wente MN, Bintintan VV, Koninger J, Buchler MW, Gutt CN. Robot-assisted versus conventional laparoscopic fundoplication: short-term outcome of a pilot randomized controlled trial. Surg Endosc. 2007;21(10):1800–1805. doi: 10.1007/s00464-007-9268-y. [DOI] [PubMed] [Google Scholar]
- 21.Baik SH, Ko YT, Kang CM, Lee WJ, Kim NK, Sohn SK, Chi HS, Cho CH. Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc. 2008;22(7):1601–1608. doi: 10.1007/s00464-008-9752-z. [DOI] [PubMed] [Google Scholar]
- 22.Hubens G, Balliu L, Ruppert M, Gypen B, Tu T, Vaneerdeweg W. Roux-en-Y gastric bypass procedure performed with the da Vinci robot system: is it worth it? Surg Endosc. 2008;22(7):1690–1696. doi: 10.1007/s00464-007-9698-6. [DOI] [PubMed] [Google Scholar]
- 23.Mirnezami AH, Mirnezami R, Venkatasubramaniam AK, Chandrakumaran K, Cecil TD, Moran BJ. Robotic colorectal surgery: hype or new hope? A systematic review of robotics in colorectal surgery. Colorectal Dis. 2010;12(11):1084–1093. doi: 10.1111/j.1463-1318.2009.01999.x. [DOI] [PubMed] [Google Scholar]
- 24.Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA, Roehrborn CG, Lotan Y. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol. 2010;57(3):453–458. doi: 10.1016/j.eururo.2009.11.008. [DOI] [PubMed] [Google Scholar]