Abstract
INTRODUCTION
Thoracolithiasis is quite rare with only 18 cases reported in the literature.
PRESENTATION OF CASE
The 65-year-old female was referred to us for the abnormality on the chest X-ray. The serial computed tomographic (CT) scans showed a mobile calcified nodule of about 10 mm in diameter. Exploratory thoracoscopy was performed. A 15 mm pearl-like pleural stone was removed with uneventful postoperative course.
DISCUSSION
Thoracolithiasis is very rare, and its etiology as well as its epidemiology still remains to be unclear. Preoperative diagnosis is always difficult. However, specific radiological findings could let us recognize the probability of that lesion and avoid unnecessary major operation.
CONCLUSION
Thoracolithiasis should never be overlooked as a differential diagnosis in a pulmonary calcified nodule.
Keywords: Thoracolithiasis, Pleural stone, Pleurolith, Intrathoracic calculus
1. Introduction
Thoracolithiasis, which is also known as pleurolith or intrathoracic calculus, is quite rare with a frequency of 0.086%.1 Since the first case of thoracolithiasis was reported by Dias et al. in 1968, 18 cases have been reported in the literature.2,3
2. Presentation of case
A 65-year-old female patient with the past medical history of hypertension and chronic renal failure was referred for the evaluation of a lung nodule of about 10 mm in diameter in the left thoracic cavity. Over a month's period of follow-up with CT scan, the homogenously calcified nodule had not changed in size and appearance, but that was found in a different location within the left thorax (Fig. 1). Exploratory VATS (video-assisted thoracoscopic surgery) was performed and a pearl-like calcified nodule was removed (Fig. 2). No other abnormality was detected. Chemical analysis of the removed stone showed that the constituent was purely calcium (15% of calcium phosphate and 85% of fatty acid calcium salt). The postoperative recovery was uneventful.
Fig. 1.

The serial CT scan shows a mobile calcified nodule in the left thoracic cavity.
Fig. 2.
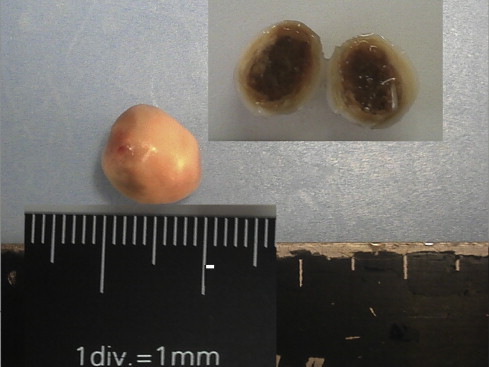
Macroscopic findings of the removed stone. The yellowish core surrounded by the shiny white capsule.
3. Discussion
According to the report by Kosaka et al., the definition of thoracolithiasis is that it is a condition in which one or more free bodies with or without calcifications exists in the thoracic cavity without any previous trauma, intervention or pleurisy.4
The epidemiology of this condition remains unclear; however, the great majority of these reports are from Japan with one case from Germany and the other from Canada.5 A few hypotheses regarding its etiology have been suggested. These are pericardial/pleural fat necrosis, pericardial/pleural fat tearing off in the pleural cavity, old tuberculous foci, or aggregation of macrophages phagocytosing dust.4,6,7 Most pleural stones (approximately 75%) have been found on the left side, of which finding might well support the pericardial fat necrosis theory.5 In our case, the stone was made of purely calcium without any fatty component, which makes it difficult to understand etiologically.
Almost all of the patients with thoracolithiasis were reported to be asymptomatic, and all cases were discovered during surgery or detected on chest radiographies (chest X-rays and/or CT scan).5 Radiologically, a small mobile calcified nodular lesion is quite characteristic to a pleural stone.
Irrespective of its distinctive radiological findings, definite diagnosis usually requires surgical removal of the stone. Trans-thoracic or endobronchial biopsy often fails to obtain diagnosis because of its hard consistency and loose fixation within the pleural cavity.
4. Conclusion
Thoracolithiasis is very difficult to diagnose preoperatively. If we are well familiar with the radiological findings of this lesion, we could go ahead with minimally invasive surgery like VATS for diagnostic and therapeutic purpose. All thoracic surgeons should keep in mind the possibility of thoracolithiasis as a differential diagnosis in a pulmonary calcified nodule.
Conflict of interest statement
The authors have no conflict of interest, financial or otherwise in the publication of this journal.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Teruya Komatsu contributed to the collection of the clinical data and writing of the manuscript. Terumasa Sowa and Takuji Fujinaga contributed to the writing and editing of the manuscript.
References
- 1.Kinoshita F., Saida Y., Okajima Y., Honda S., Sato T., Hayashibe A. Thoracolithiasis: 11 cases with a calcified intrapleural loose body. J Thorac Imaging. 2010;25(1):64–67. doi: 10.1097/RTI.0b013e3181a4ba03. [DOI] [PubMed] [Google Scholar]
- 2.Dias A.R., Zerbini E.J., Curi N. Pleural stone. A case report. J Thorac Cardiovasc Surg. 1968;56(1):120–122. [PubMed] [Google Scholar]
- 3.Dadrich M., Schneider T., Puderbach M., Kauczor H.U., Heussel C.P. Moving pleural mass. Med Klin Intensivmed Notfmed. 2012 doi: 10.1007/s00063-012-0076-3. [DOI] [PubMed] [Google Scholar]
- 4.Kosaka S., Kondo N., Sakaguchi H., Kitano T., Harada T., Nakayama K. Thoracolithiasis. Jpn J Thorac Cardiovasc Surg. 2000;48(5):318–321. doi: 10.1007/BF03218148. [DOI] [PubMed] [Google Scholar]
- 5.Bolca C., Trahan S., Frechette E. Intrapleural thoracolithiasis: a rare intrathoracic pearl-like lesion. Thorac Cardiovasc Surg. 2011;59(7):445–446. doi: 10.1055/s-0030-1270757. [DOI] [PubMed] [Google Scholar]
- 6.Pineda V., Caceres J., Andreu J., Vilar J., Domingo M.L. Epipericardial fat necrosis: radiologic diagnosis and follow-up. AJR Am J Roentgenol. 2005;185(5):1234–1236. doi: 10.2214/AJR.04.1310. [DOI] [PubMed] [Google Scholar]
- 7.Iwasaki T., Nakagawa K., Katsura H., Ohse N., Nagano T., Kawahara K. Surgically removed thoracolithiasis: report of two cases. Ann Thorac Cardiovasc Surg. 2006;12(4):279–282. [PubMed] [Google Scholar]


