Abstract
INTRODUCTION
Intraneural lipoma and fibrolipomatous hamartoma of the nerve are rare soft tissue tumors that most commonly occur in the forearm and the wrist, and particularly within the median nerve. When the lesions are large enough, they may cause progressive compression neuropathy. They are distinct entities each other with different clinical and radiological findings and thereby need different surgical treatments.
PRESENTATION OF CASE
We report here 3 cases of intraneural lipomatous tumors of the median nerve (1 case of intraneural lipoma and 2 cases of fibrolipomatous hamartoma).
DISCUSSION
All patients were surgically treated successfully with complete excision for intraneural lipoma and with carpal tunnel releases for the both fibrolipomatous hamartomas.
CONCLUSION
A careful preoperative planning is necessary for the optimal treatment by distinguishing whether it is a resectable or non-resectable tumor based on the clinical and radiological findings, because they have characteristic findings each other.
Keywords: Intraneural lipoma, Fibrolipomatous hamartoma of the nerve
1. Introduction
Intraneural lipoma and fibrolipomatous hamartoma of the nerve are rare soft tissue tumors that most commonly occur in the forearm and the wrist, and particularly within the median nerve. When the lesions are large enough, they may cause progressive compression neuropathy. The term intraneural lipoma means encapsulated lipoma, which can be shelled out or enucleated from the surrounding structures, and microscopic examination reveals that these lesions are composed of adipose tissue without neural elements. On the other hand, various terms have been used to describe fibrolipomatous hamartoma of the nerve, including fatty infiltration, lipofibroma, fibrofatty proliferation, and intraneural lipofibroma.1 It is pathologically composed of a fatty and fibrous tissue with intermingling nerve fibers.
Significant differences do exist between intraneural lipoma and fibrolipomatous hamartoma of the nerve.2 Intraneural lipomas are usually well encapsulated with nerve fibers that run on the outer surface of the mass; thus, complete excision without damage to the adjoining nerve is possible. On the other hand, fibrolipomatous hamartoma of the nerve is composed of fibrous tissues, fatty tissues, and normal nerve fibers, making complete excision without nerve damage difficult. Although the World Health Organization (WHO) grouped intraneural lipoma, fibrolipomatous hamartoma of the nerve, fatty infiltration, and neural fibrolipoma under lipomatosis of the nerve in 2002,3 the clinical findings and treatments of these conditions differ. We report 3 cases of intraneural lipomatous tumor: 1 intraneural lipoma of the median nerve and 2 neural fibrolipomatous hamartoma of the median nerve, all of which caused carpal tunnel syndrome. We present these 3 cases with special emphasis on the clinical and radiological findings and surgical treatments.
2. Presentation of cases
2.1. Case 1
A 56-year-old woman presented with progressive swelling of the right forearm over a 6-month period. Physical examination revealed a 10 × 8-cm soft elastic mass at the palmar aspect of the right forearm. There was no history of trauma. She did not have any motor symptoms, hypoesthesia, or pain. There was no tenderness on palpation and no Tinel-like sign. Magnetic resonance imaging (MRI) demonstrated the presence of a well-circumscribed soft tissue mass measuring 4 cm on the radial side of the right forearm. On T1- and T2-weighted images, the signal intensities of the mass were found to be markedly high, and the mass intensities on short tau inversion recovery (STIR) images changed to low (Fig. 1A–D). We performed an open biopsy and made a pathological diagnosis of lipoma. At the time of the biopsy, the patient felt some numbness and pain at the median nerve area. Exploration revealed a well-encapsulated lipomatous tumor spreading the fibers of the easily identifiable median nerve (Fig. 1E). Complete excision of the tumor was comparatively easy. Histological examination revealed a lipomatous tumor composed of mature adipocytes without intermingling nerve fibers (Fig. 1F). At 6 months after the excision, the numbness and pain had disappeared. We diagnosed this patient as intraneural lipoma based on the clinical and pathological findings.
Fig. 1.
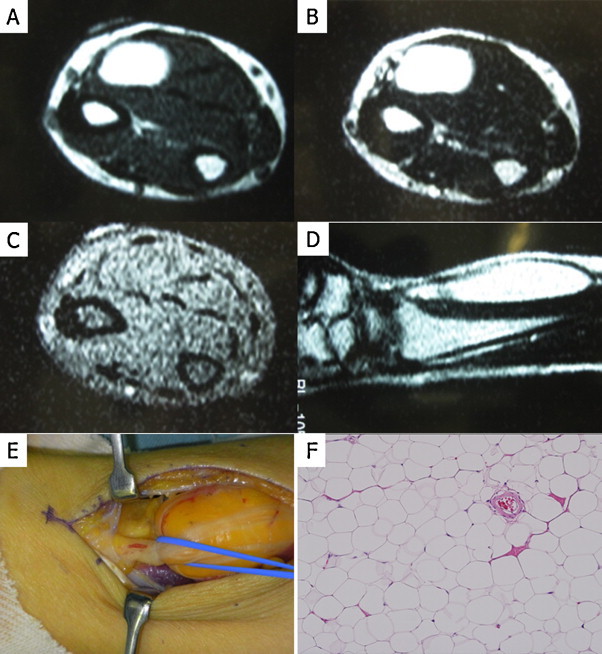
MRI, macro- and microscopic findings in Case 1. The mass shows high signal intensities on T1 (A)- and T2 (B)-weighted images, and the intensities changes to low on short tau inversion recovery (STIR) images (C). The sagittal image also shows high-intensity mass (D). Well-encapsulated lipoma by which the median nerve fibers were spread (E). The resected specimen shows a proliferation of mature adipocytes without nerve fibers (F).
2.2. Case 2
A 17-year-old boy had a mass on his right hand since childhood, and he had received no treatment for it. He had felt continual numbness on the volar side of his right hand for the past year. The numbness had been gradually getting worse; therefore, he had visited our hospital. He had no history of trauma. Physical examination revealed a 4 × 2-cm elastic soft mass at the volar aspect of the right distal forearm and hand. On palpation, decreased perception was noted in the middle finger in addition to disordered thumb opposition movement. Digital enlargement was not evident in this patient. On MRI, the mass measured 4 cm on the center of the hand. On T1- and T2-weighted images, the mass had an alveolar structure in which thickened nerve bundles appeared as hypointensive tubular structures (Fig. 2A–C). On sagittal view, bowing of the flexor retinaculum and displacement of the flexor tendons were observed in the carpal tunnel. On exploration, there was a large lipomatous tumor under the flexor retinaculum that was enlarging the median nerve (Fig. 2D). We judged total excision of the tumor impossible, and thus, performed carpal tunnel release and a biopsy. Histological analysis showed a mixture of collagenous fiber and fatty tissue (Fig. 2E). Numbness was improved and the patient's condition had not relapsed at the time of 6-months follow-up. Although the intermingled nerve fascicles were not observed in the biopsy sample, we diagnosed this patient with fibrolipomatous hamartoma of the median nerve.
Fig. 2.
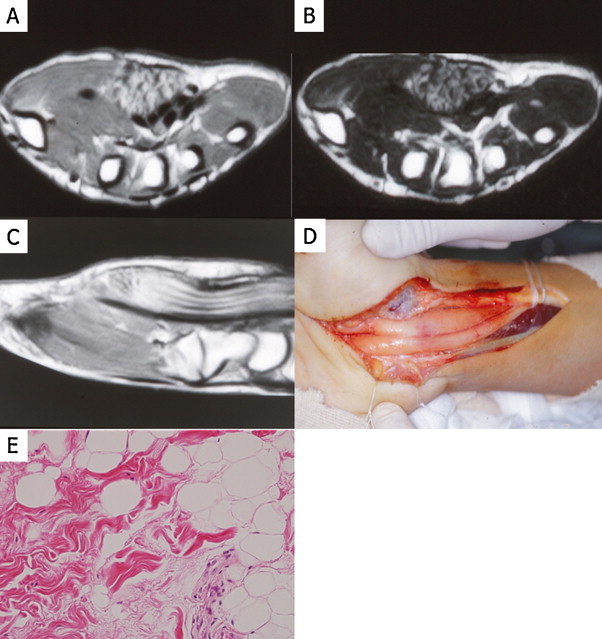
MRI, macro- and microscopic findings in Case 2. The mass showed alveolar structures on both T1 (A)- and T2 (B)-weighted images. The “spaghetti-like” appearance in sagittal section (C). Large lipomatous lesions under the flexor retinaculum look like hypertrophic nerve (D). Biopsy specimen shows a mixture of collagen fibers and fatty tissue without intermingling nerve fibers (E).
2.3. Case 3
A 15-year-old boy felt numbness in the middle finger of his right hand while playing baseball. After 6 months, he visited our hospital because he noticed a mass on his right hand. On examination, diffuse swelling around the muscles and slight tenderness was observed. On palpation, there was no decreased perception or finger movement. MRI showed a 3-cm mass at the center of the hand, and the other findings were similar to those of Case 2 (Fig. 3A–D). On coronal view, tubular structures were seen in the carpal tunnel. Because his chief complaint was numbness, he had been under observation for 3 months; however, because his symptoms had been getting worse, we performed a carpal tunnel release and biopsy for diagnosis. Operative and histological findings resembled those of Case 2 (Fig. 3E and F). Numbness was improved and the patient's symptoms had not relapsed at time of 4-years follow-up. We diagnosed this patient with fibrolipomatous hamartoma of the median nerve.
Fig. 3.
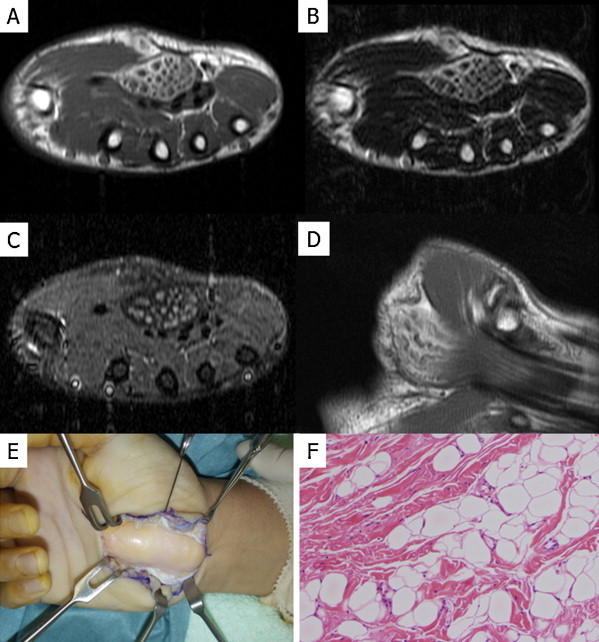
MRI, macro- and microscopic findings in Case 3. The mass showed alveolar structures on both T1 (A)- and T2 (B)-weighted images. The “coaxial cable-like” appearance in cross-section (C) and “spaghetti-like” appearance in longitudinal section (D), respectively. Operative and histological findings in Case 3 (E and F) resembled those of Case 2. The feature was not enough informative for the diagnosis of fibrolipomatous hamartoma.
3. Discussion
Lipomatous tumors arising in the peripheral nerves are rare. Morley reported the first case of intraneural lipoma in 1964.4 The tumors that could be separated from the neural elements and showed the pathological characteristics of a benign lipoma without intermingling with neural elements were termed as “true intraneural lipoma” by Rusko and Larson.5
To our knowledge, not so many cases have been reported in the English literature as intraneural lipomas.2,4–9 The intraneural lipoma tends to occur in the fourth and fifth decades and has a female predominance. Most of the intraneural lipoma occurs in the median nerve, while also reported to occur in the radial nerve,2 sciatic nerve,7 ulnar nerve,8 and posterior interosseous nerve.9 The maximum size of the intraneural lipoma was reported to be 200 × 100 mm9 and the minimum to be 25 × 40 mm.4 A history of trauma was reported in only 1 case.5 Pathological findings of lipomas include proliferation of mature adipocytes without intermingled nerve fibers. The patient in Case 1 of this manuscript is older as one with fibrolipomatous hamartoma which arises in a younger age group. Therefore, clinical information is also important for the diagnosis, because even the biopsy sample cannot always be obtained from the appropriate lesion for a diagnosis where the involved nerve fibers exist if it is an infiltrative fibrolipomatous hamartoma.
On the other hand, fibrolipomatous hamartoma was first described in 1953 by Mason.10 Various terms describe fibrolipomatous hamartoma of the nerve such as fatty infiltration, fibrofatty proliferation, intraneural fibrolipoma, lipofibroma, and fibrolipomatosis. The pathology of fibrolipomatous hamartoma of the nerve usually shows a mixture of collagenous fibers and fatty tissue, and nerve fibers are noticed in cases of partial resection. The etiology of fibrolipomatous hamartoma of the nerve remains unclear, however, several potential etiologic factors have been described such as abnormal development of flexor retinaculum in children,11 history of trauma,12 and chronic nerve inflammation.13 It has been reported that fibrolipomatous hamartoma tend to arise in younger age groups before the third decade and have no sexual predominance.2 Two patients (Cases 2 and 3) in this manuscript had suffered a mass on his hand since childhood. However, the digital enlargement was not evident in both cases, although it has been reported that patients with fibrolipomatous hamartoma often had digital enlargement due to an increase in perineural soft tissue and skin.14,15 Especially, the it has been demonstrated that patients early in their childhoods present with macrodactyly, and later in adolescence present with a volar forearm mass.14,15
In addition to the clinicopathological difference, it would be also very important to note that intraneural lipoma and fibrolipomatous hamartoma of the nerve have crucial differences in MR imaging since their surgical treatments differ as well. On T1- and T2-weighted images, the intraneural lipoma intensities are markedly high. However, on STIR images, intensities change to low, a level that is equal to that of normal lipoma. These findings suggest that intraneural lipoma is a pure lipoma occurring only in the nerve bundles and that the nerve fibers run on the outer surface of the mass. On the other hand, MR imaging of fibrolipomatous hamartoma of the nerve has a characteristic “coaxial cable-like” appearance in cross-section or “spaghetti-like” appearance in longitudinal section.9 MR imaging show serpentine nerve bundles with low signal intensity embedded within excessive fatty tissue, which appears hyperintense on both T1- and T2-weighted images.16 Transverse sections show thin hypointense septa within the fat tissue that separate some nerve bundles,16 what we refer to as the “lotus sign.” These septa may represent thickened perineurium, a characteristic pathological finding.16 These differences in MR imaging would be useful for the differential diagnosis between intraneural lipoma and fibrolipomatous hamartoma of the nerve, because even the biopsy data might be sometimes not informative.
Treatment of intraneural lipoma involves total excision, which was also performed in our Case 1. Cut of the nerve fibers is also reported in case they were involved in the huge intraneural lipoma.8 On the other hand, the gold standard treatments for fibrolipomatous hamartoma of the nerve are usually conservative approaches including decompression and debulking of the fibrofatty sheath, microsurgical dissection of the neural elements and observation for asymptomatic patients.2 In case of fibrolipomatous hamartoma associated with macrodactyly, excision of the involved nerve segment with or without nerve grafting, or amputation of the finger is recommended.2,16 Treatment should focus on alleviating the patients’ symptoms, and complete excision of these tumors is not recommended if clinically significant motor or sensory deficits are anticipated.17 Objective evaluations of pre-operative and post-operative hand functions using some kinds of scoring have not performed for either of 3 cases. However, the symptoms of 3 patients reported here improved or disappeared after surgery, and no complication was observed after surgery in all cases. Furthermore, relapse of tumor and patients’ symptoms have not been observed so far at 6-months (Cases 1 and 2) and 4-years (Case 3) follow-up. In contrast, Louis et al. reported in 1985 long-term follow-up of 4 cases in which decompression was performed, although their symptoms were described to be deteriorating.18 In cases in which the mass has already led to major motor disturbance, simple decompression or decreasing the bulk of the mass may not improve nerve function, and it may be necessary to perform a resection of the involved nerves and then reconstruct them as necessary to restore function.
4. Conclusion
Finally, when MRI findings suggest a lipoma in the forearm, the possibility of intraneural lipoma should be considered and treated with care. When MRI findings indicate fibrolipomatous hamartoma of the nerve, careful preoperative planning of reconstruction for long-term reactivation of motor or sensory deficits should be performed.
Conflict of interest statement
None.
Funding
This work was supported in part by a Grant-in-Aid for General Scientific Research from the Ministry of Education, Science, Sports and Culture, Tokyo, Japan (#23590434 to Tsuyoshi Saito and #24590429 to Hiroyuki Mitomi).
Ethical approval
Written informed consent was obtained from each patient for publication of this case report and accompanying images. A copy of the written consents is available for review by the Editor-in-Chief of this journal on request.
Author contributions
All authors have contributed significantly, and that all authors are in agreement with the content of the manuscript.
Tatsuya Takagi, Tomoaki Torigoe, Yoshiyuki Suehara, Hirohisa Katagiri, Hideki Murata, Mitsuru Takahashi, and Kazuo Kaneko performed operation at least one of these 3 cases; Tsuyoshi Saito, Hiroyuki Mitomi, and Ichiro Ito diagnosed these 3 cases; and Taketo Okubo, Tsuyoshi Saito, and Takashi Yao wrote the paper.
References
- 1.Paletta F.X., Rybka F.J. Treatment of hamartoma of the median nerve. Annals of Surgery. 1972;176:217–222. doi: 10.1097/00000658-197208000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balakrishnan C., Bachusz R.C., Balakrishnan A., Elliot D., Careaga D. Intraneural lipoma of the radial nerve presenting as Wartenberg syndrome: a case report and review of literature. Canadian Journal of Plastic Surgery. 2009;17:e39–e41. [PMC free article] [PubMed] [Google Scholar]
- 3.Fletcher C., Unni K., Mertens F. IARCP Press; Lyon, France: 2002. WHO classification pathology and genetics tumours of soft tissue and bone. p. 24–25. [Google Scholar]
- 4.Morley G.H. Intraneural lipoma of the median nerve in the carpal tunnel. Report of a case. Journal of Bone & Joint Surgery. 1964;46B:734–735. [PubMed] [Google Scholar]
- 5.Rusko R.A., Larson R.D. Intraneural lipoma of the median nerve: case report and literature review. Journal of Hand Surgery (American Volume) 1981;6:388–391. doi: 10.1016/s0363-5023(81)80050-0. [DOI] [PubMed] [Google Scholar]
- 6.Watson-Jones R. Encapsulated lipoma of the median nerve at the wrist. Journal of Bone & Joint Surgery. 1964;46B:736. [PubMed] [Google Scholar]
- 7.Balakrishnan C., Saini M.S., Demercurio J. Intraneural lipoma of the ulnar nerve: a case report and review of literature. Canadian Journal of Plastic Surgery. 2006;14:49–50. doi: 10.1177/229255030601400107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsuo T., Sugita T., Shimose S., Kubo T., Yasunaga Y., Ochi M. Intraneural lipoma of the posterior interosseous nerve. Journal of Hand Surgery (American Volume) 2007;32:1530–1532. doi: 10.1016/j.jhsa.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 9.Nardone R., Venturi A., Ladurner G., Golaszewski S., Psenner K., Tezzon F. Obturator mononeuropathy caused by lipomatosis of the nerve: a case report. Muscle and Nerve. 2008;38:1046–1048. doi: 10.1002/mus.21002. [DOI] [PubMed] [Google Scholar]
- 10.Mason M.L. Presentation of cases: proceedings of the American Society for Surgery of the Hand. Journal of Bone and Joint Surgery. 1953;35:273–274. [Google Scholar]
- 11.Rowland S.A. Case report: ten year follow-up of lipofibroma of the median nerve in the palm. Journal of Hand Surgery American Volume. 1977;176:217–222. doi: 10.1016/s0363-5023(77)80135-4. [DOI] [PubMed] [Google Scholar]
- 12.Guthikonda M., Rengachary S.S., Balko M.G., Van Loveren H. Lipofibromatous hamartoma of the median nerve: case report with magnetic resonance imaging correlation. Neurosurgery. 1994;35:127–132. doi: 10.1227/00006123-199407000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Callison J.R., Thoms O.J., White W.L. Fibrofatty proliferation of the median nerve. Plastic and Reconstructive Surgery. 1968;42:403–413. [PubMed] [Google Scholar]
- 14.Silverman T.A., Enzinger F.M. Fibrolipomatous hamartoma of nerve: a clinicopathologic analysis of 26 cases. American Journal of Surgical Pathology. 1985;9:7–14. doi: 10.1097/00000478-198501000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Amadio P.C., Reiman H.M., Dobyns J.H. Lipofibromatous hamartoma of nerve. Journal of Hand Surgery American Volume. 1988;13:65–75. doi: 10.1016/0363-5023(88)90203-1. [DOI] [PubMed] [Google Scholar]
- 16.De Maeseneer M., Jaovisidha S., Lenchik L., Witte D., Schweitzer M.E., Sartoris D.J. Fibrolipomatous hamartoma: MR imaging findings. Skeletal Radiology. 1997;26:155–160. doi: 10.1007/s002560050212. [DOI] [PubMed] [Google Scholar]
- 17.Razzaghi A., Anastakis D.J. Lipofibromatous hamartoma: review of early diagnosis and treatment. Canadian Journal of Surgery. 2005;48:394–399. [PMC free article] [PubMed] [Google Scholar]
- 18.Louis D.S., Hankin F.M., Greene T.L., Dick H.M. Lipofibromas of the median nerve: long-term follow-up of four cases. Journal of Hand Surgery. 1985;10A:403–408. doi: 10.1016/s0363-5023(85)80044-7. [DOI] [PubMed] [Google Scholar]


