Abstract
INTRODUCTION
Metastatic spread from non-head and neck tumours to the sinonasal region is exceedingly rare. We present a case of breast cancer metastasis to the nasopharynx, ethmoid and sphenoid sinuses. To date there have been only two similar cases in the literature. We discuss the diagnosis and management of such cases and propose how they may be staged.
PRESENTATION OF CASE
A 75-year-old woman with past medical history of breast carcinoma, presented clinically as having a primary sinonasal malignancy. Magnetic resonance imaging (MRI) demonstrated a lesion involving the spenoid and ethmoid sinuses, nasendoscopy revealed a mass in the nasopharynx. Biopsy from clinic pointed to inverted sinonasal papilloma, however this did not fit with the MRI or the clinical picture. Repeat biopsy under image guidance revealed the lesion to be a breast cancer metastasis.
DISCUSSION
An extensive literature review revealed few cases of spread to the sinonasal region from distant primary malignancy. When such cases do arise, most are from renal tumours. Breast cancer metastases usually present with signs and symptoms of disseminated disease, however our case represents a true isolated metastasis. We discuss the management of our case and suggest the use of the tumour-node-metastasis (TNM) system, in order to stage these rare isolated occurrences.
CONCLUSION
If discovered early, this rare manifestation may be managed by primary surgical resection. Metastases to the region may be more common than previously thought. A high index of suspicion should be employed, especially where there is past medical history of malignancy.
Keywords: Breast cancer, Breast neoplasms, Metastases, Nasopharynx, Naopharyngeal neoplasms
Introduction
Breast cancer metastasis to the nasopharynx is an extremely rare occurrence, with only two cases previously reported in the literature.1,2 We present a recent case of breast cancer metastasis to the naopharynx, ethmoid and sphenoid sinuses. The investigations, subsequent diagnosis and management of this rare case are to be discussed. We also discuss the wider implications, including staging and management of distant primaries metastasising to this region.
Presentation of case
A 75-year-old woman with history of breast cancer was referred to the Ear, Nose and Throat (ENT) department by her general practitioner (GP) with suspected naso-pharyngeal tumour. Two years previously she had a right sided radical mastectomy and axillary node clearance for breast carcinoma. Histological analysis of the specimen found there to be high grade ductal carcinoma in situ with a solid growth pattern, there were also features of invasive lobular carcinoma and some features of invasive ductal carcinoma. The cancerous portion of the specimen measured 30 by 30 millimetres (mm) and did not involve the resection margins. Nine axillary lymph nodes were removed and one of these was positive for breast carcinoma. This lesion was recoded as grade 3 and according to the TNM system was staged at T2 N1 M0. Further analysis revealed the specimen to be oestrogen receptor (ER) and progesterone receptor (PR) positive, while human epidermal growth factor receptor 2 (HER2) protein was negative. Following primary resection she was given radiotherapy to the right chest wall in the amount of 40.5 Gray (Gy) in 15 fractions, this was followed by adjuvant hormone therapy with Anatrozole. Recurrence was continually ruled out at regular follow-up.
She was seen by ophthalmology four months earlier with horizontal diplopia and incomplete left abducens (VI) nerve palsy. An MRI scan was organised to exclude an intra-cranial cause, no evidence of which was apparent. However an ill-defined soft tissue mass measuring 27 mm × 32 mm × 26 mm was demonstrated within the posterior aspect of the ethmoid sinuses, this mass extended into the sphenoid sinuses. A likely diagnosis of naso-pharyngeal tumour was suggested and urgent referral to ENT advised (Figs. 1 and 2).
Fig. 1.

T1 weighted sagittal MRI of the patients head through the midline.
Fig. 2.
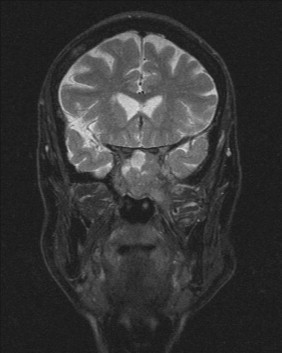
T2 weighted coronal MRI of the patients head at the level of the PNS.
On presentation to the ENT department she had left-sided facial weakness and partial nasal obstruction ipsilaterally. There was no history of discharge or bleeding. On flexible nasendoscopy (FNE) a large swelling was seen in the left post-nasal space (PNS), this was biopsied. Histological analysis described a polypoid mass of complexly folded broad trabeculae of squamous epithelium. There was minimal stroma present with active acute inflammation and numerous inflammatory cells. Although there were sparse mitotic figures, there were no obvious atypical cells. The specimen indicated Schneiderian or inverted sinonasal papilloma. This conclusion was not consistent with the clinical presentation or the extensive disease demonstrated by MRI. For this reason she was referred to a tertiary centre for repeat biopsy under image guidance. The repeat histological analysis revealed that deep to the changes found at first biopsy, there was high grade carcinoma consistent with invasive ductal carcinoma, this was also confirmed to be ER positive.
Her case was discussed at the head and neck oncology multidisciplinary meeting, where it was decided that curative surgery was not an option. It was however recommended that she may benefit from palliative radiotherapy.
Shortly after the definitive histological diagnosis had been made her symptoms deteriorated rapidly and she required admission from clinic just six weeks after initially presentation to ENT. By this point she had additionally developed progressive sensorineural hearing loss, facial sensory deficit, and hypoglossal nerve (XII) palsy on the left. She was also dysphagic to solids and had rapidly lost weight. She was treated with steroids, lorazepam and supportive therapy.
After one week in hospital she was transferred to the regional oncology unit where a face mask was constructed so focused radiotherapy could be delivered. Despite several daily radiotherapy treatments she deteriorated clinically and was admitted to a hospice after one week where she spent her final days.
Discussion
Metastatic spread involving the nose, PNS and paranasal sinuses is extremely rare. When such cases do present they are mostly from renal malignancy.3–5 Recent cases of metastatic hepatocellular carcinoma and Hodgkin Lymphoma to the sphenoid and maxillary sinuses have also been reported.6,7 Our case is only the third case in the English language literature where a patient has presented with intranasal breast cancer metastasis. The first case presented as a choanal polyp,1 the second as a solitary nasal cavity metastasis.2
Breast cancer metastases have a relatively wide distribution, however the most common sites of spread are bone, regional lymphatics, lung, liver and brain.8 The aetiology of primary nasopharyngeal carcinoma (NPC) is well known and includes genetic predisposition, viral infection with Epstein-Barr virus (EBV) and dietary factors.9,10 Metastatic spread from distant primaries to the head and neck (H&N) is a rare occurrence. Since metastasis from breast cancer to the nose and nasopharynx is extremely rare, the aetiology of these sparse cases remains a mystery.
The presentation of this condition is somewhat varied and naturally depends on the extent of spread. Our case and the previous cases essentially presented as a primary NPC. A variety of signs and symptoms may be present and include nasal obstruction, epistaxis and serosanginous discharge, cranial nerve involvement, and Trotter's triad of glue ear, ipsilateral soft palate immobility and trigeminal nerve (V) pain.
The incidence of breast cancer metastases to the H&N region is unknown.11 It has been proposed that many metastases to this region go undetected, as they are ‘obscured’ by more evident metastatic disease at other sites.11 Haematogenous spread is the most likely route, Debois also proposes spread via the classical venous route of Batson along the prevertebral venous plexus.
Investigating nasopharyngeal lesions starts with clinical history and examination and includes tissue diagnosis via biopsy and histopathological analysis. Computerised tomography (CT) is the initial radiological investigation of choice and should include thorax, abdomen and pelvis (particularly if a history of malignancy in these regions is given). MRI provides better delineation and higher resolution when there is need to investigate intracranial and soft tissue spread, including nodal involvement. Positron emission tomography (PET) scanning is potentially useful in cases of advanced NPC at detecting skeletal metastases.12
Although metastatic breast carcinoma presenting in the nose is very rare, such a lesion may exist in isolation with no other distant metastases.1,2 For this reason we propose that such isolated lesions be staged as if they were in fact primary NPC. Although our case was only amenable to palliative therapy, that reported by Liao et al. was successfully treated by surgical resection.2
As with NPC, metastatic spread to the nose may lie in the submucosa and be difficult to visualise. In our case, although FNE demonstrated gross abnormality, initial biopsy did not demonstrate malignant disease. It is also likely that the results of our biopsies were as a result of dual pathology. Only a high index of suspicion and subsequent further investigation provided the definitive diagnosis.
We should not forget that although breast cancer is mostly epithelial derived and therefore is similar to primary NPC, it and other metastases to the H&N may require specific treatments, and for this reason multidisciplinary team involvement is advised early on.
Conclusion
In the rare instance of truly isolated sinonasal breast cancer metastases, primary surgical resection may be curative.2 It is likely that although still rare, metastases arising from distant sites to this region are more common than was previously thought. A high index of suspicion must be employed, especially where there is past history of malignancy.
Conflict of interest statement
There were no conflicts of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient's next of kin (patient deceased) for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Mr Shaun Davey is the primary author of this report.
Mr Simon Baer was the consultant in charge of the patient's care and was also involved in writing the case.
Acknowledgements
There are no acknowledgements and no sources of funding.
References
- 1.Sismanis A., Ruffy M.L., Polisar I.A., Torno R. Metastatic breast carcinoma presenting as a choanal polyp. Ear, Nose & Throat Journal. 1980;59(3):130–133. [PubMed] [Google Scholar]
- 2.Liao H.S., Hsueh C., Chen S.C., Chen I.H., Liao C.T., Huang S.F. Solitary nasal cavity metastasis of breast cancer. Breast Journal. 2010;16(3):321–322. doi: 10.1111/j.1524-4741.2009.00894.x. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto Y., Yanagihara N. Renal clear cell carcinoma metastatic to the nose and paranasal sinuses. Laryngoscope. 1982;92(10 Pt 1):1190–1193. [PubMed] [Google Scholar]
- 4.Simo R., Sykes A.J., Hargreaves S.P., Axon P.R., Birzgalis A.R., Slevin N.J. Metastatic renal cell carcinoma to the nose and paranasal sinuses. Head & Neck. 2000;22(7):722–727. doi: 10.1002/1097-0347(200010)22:7<722::aid-hed13>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 5.Fyrmpas G., Adeniyi A., Baer S. Occult renal cell carcinoma manifesting with epistaxis in a woman: a case report. Journal of Medical Case Reports. 2011;5:79. doi: 10.1186/1752-1947-5-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tandon S., Nair A., Sawkar A., Balasubramanya A.M., Hazarika D. Hepatocellular carcinoma presenting as an isolated sphenoid sinus lesion: a case report. Ear, Nose & Throat Journal. 2012;91(1):E10–E13. doi: 10.1177/014556131209100116. [DOI] [PubMed] [Google Scholar]
- 7.Peterson J.L., Hayostek C.J., Garvey C., Menke D.M., Rivera C.E. Hodgkin lymphoma of the maxillary sinus: an unusual occurrence. Ear, Nose & Throat Journal. 2012;91(1):E16–E19. doi: 10.1177/014556131209100118. [DOI] [PubMed] [Google Scholar]
- 8.Klein A., Olendrowitz C., Schmutzler R., Hampl J., Schlag P.M., Maass N. Identification of brain- and bone-specific breast cancer metastasis genes. Cancer Letters. 2009;276(2):212–220. doi: 10.1016/j.canlet.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 9.Chien Y.C., Chen J.Y., Liu M.Y., Yang H.I., Hsu M.M., Chen C.J. Serologic markers of Epstein-Barr virus infection and nasopharyngeal carcinoma in Taiwanese men. The New England Journal of Medicine. 2001;345(26):1877–1882. doi: 10.1056/NEJMoa011610. [DOI] [PubMed] [Google Scholar]
- 10.Chen L., Gallicchio L., Boyd-Lindsley K., Tao X.G., Robinson K.A., Lam T.K. Alcohol consumption and the risk of nasopharyngeal carcinoma: a systematic review. Nutrition and Cancer. 2009;61(1):1–15. doi: 10.1080/01635580802372633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Debois J.M. Kluwer Academic Publishers; Boston: 2002. TxNxM1: the anatomy and clinics of metastatic cancer. [Google Scholar]
- 12.Liu F.Y., Chang J.T., Wang H.M., Liao C.T., Kang C.J., Ng S.H. [18F]fluorodeoxyglucose positron emission tomography is more sensitive than skeletal scintigraphy for detecting bone metastasis in endemic nasopharyngeal carcinoma at initial staging. Journal of Clinical Oncology. 2006;24(4):599–604. doi: 10.1200/JCO.2005.03.8760. [DOI] [PubMed] [Google Scholar]


