Abstract
INTRODUCTION
Triple assessment of a suspicious breast lesion may not always provide a definite diagnosis. We report a case of epidermoid cyst of breast, which caused diagnostic dilemma in spite of a thorough triple assessment and entailed mastectomy.
PRESENTATION OF CASE
A 69-year-old woman presented with a large painful retroareolar left breast mass. Clinical examination, ultrasound and mammography were highly suspicious of malignancy. However, core biopsy suggested a benign lesion. Due to size of the lesion and diagnostic uncertainty, various options were discussed with the patient. She opted for a simple mastectomy. The histology confirmed a large epidermoid cyst.
DISCUSSION
It is rare for an epidermoid cyst to present as such an advanced lesion, mimicking carcinoma. Excision of such a large retroareolar ‘benign’ lesion, however, may sometime entail mastectomy. This is the first reported case of an epidermoid cyst of breast necessitating mastectomy.
CONCLUSION
Diagnostic dilemma while dealing with a suspected breast cancer is not rare. Involvement of multidisciplinary team as well as patient is important in the decision-making. The report illustrates a rare presentation of a deep seated large epidermoid cyst of breast, which mimicked carcinoma, caused diagnostic confusion and entailed mastectomy. We strongly advocate the option of breast reconstruction in such cases.
Keywords: Epidermoid cyst, Breast cyst, Breast neoplasm, Mastectomy, Breast reconstruction
1. Introduction
A discreet lump in the breast is a recognised indication of referral to the breast clinic. Triple assessment of a breast lump helps assess the lump and aids in further management. However if the findings of triple assessment contradict each other, this can cause diagnostic dilemma and surgical excision of lesions are often contemplated. In such circumstances, breast conservation surgery, rather than mastectomy are usually attempted. Involvement of multidisciplinary team and patient are important before making a decision. We report a case where a simple mastectomy was performed for a breast lesion, which mimicked carcinoma but turned out to be completely benign.
2. Case report
A 69-year-old woman attended the one-stop breast clinic with history of a painful lump in the left breast of three months’ duration. There was no history of nipple discharge. She had not suffered from any breast condition in the past. Her menarche was at age twelve. She had never been pregnant and had never been on oral contraceptive pill or hormone replacement therapy. She had undergone hysterectomy at age 44 for heavy periods but was unsure whether her ovaries were retained. She gave a history of trauma to left breast nineteen years ago following a road traffic accident. There was no family history of breast or ovarian cancer. She was not on any regular medication. General examination was unremarkable. Examination of right breast was normal. Examination of left breast revealed a retro-areolar firm tender mass measuring 6 cm × 6 cm with associated nipple retraction (P4). There was no axillary or cervical lymphadenopathy. Breast size was noted to be 32 BB.
She underwent bilateral double-view mammography and ultrasound scan of both breasts. Imaging findings were highly suspicious of malignancy in the left breast with extension into the duct system (M4 and U4) (Figs. 1 and 2). A core biopsy of the lump was performed, which showed features of lobular and fibro fatty elements, with mixed lymphoplasmacytic intralobular and periductal infiltrate, foci of epitheloid and giant cells with accompanying stromal sclerosis and fragments of acanthotic squamous epithelium. Foreign body type multinucleated giant cells were seen around the ruptured ducts with foci of fat necrosis and extension of inflammatory cells into fatty tissue. The picture was consistent with periductal mastitis and duct ectasia with no evidence of malignancy (B2) (Fig. 3). The case was discussed in the multidisciplinary team (MDT), which suggested re-biopsy of the lesion. Core biopsy was repeated, which confirmed the same histological findings.
Fig. 1.

Mammogram of the left breast (medio-lateral oblique view) showing a central mass with some lack of clarity of the margin and ductal prominence anteriorly (M4).
Fig. 2.

Ultrasound scan of the left breast showing a solid mass with extension into the duct system (U4).
Fig. 3.
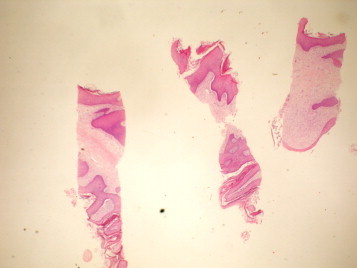
Core biopsies of the lesion of the left breast (H & E; 40×) showing periductal mastitis, duct ectasia, fragments of acanthotic squamous epithelium with no evidence of malignancy.
The matter was discussed further in the MDT. Clinicians and radiologists were strongly of the opinion that the lesion was probably malignant (P4, M4 and U4). Pathological findings were, however, benign (B2). The plan was to consider excision biopsy of the lesion at the first instance and consider mastectomy at a later stage, should the lesion turn out to be malignant.
The findings and outcome of MDT decision were discussed in full with the patient. This was a particularly difficult issue due to large size of the lesion in a relatively small breast. She opted for simple mastectomy without breast reconstruction. Given her wishes, a simple mastectomy was performed. The postoperative recovery was uneventful.
Histology demonstrated a cystic lesion measuring 85 mm in maximum diameter (Fig. 4). The cyst was lined by keratinised stratified squamous epithelium and filled with necrotic debris and keratin. The lining squamous epithelium was acanthotic and contained granular layer in some places. The surrounding tissue showed dense mixed inflammatory cell infiltrate with foreign body multinucleated giant cells. In few places, part of the cyst was lined by single layer of cuboidal epithelium. The findings were consistent with large epidermoid cyst of the breast (Fig. 5).
Fig. 4.

Macrophotographs of the left mastectomy specimen (suture marking superior border) showing the lesion near the centre of the breast.
Fig. 5.

Microphotograph of the histology (H & E; 40×) of the left breast lesion showing cyst, lined by squamous keratinised epithelium, suggestive of an epidermoid cyst.
3. Discussion
According to current guidelines, a non-operative breast cancer diagnosis should be achieved by triple assessment.1 However, in some cases excision biopsies are undertaken due to continued diagnostic uncertainty. If further surgery is required, attempts are made to preserve breasts. Although this remains the case in vast majority of cases, there are occasions where decision-making can be difficult and patient may opt for mastectomy at the first instance.
The case reported illustrates such a dilemma. The patient underwent triple assessment of her breast lump and two components (clinical and radiological) were highly suggestive of breast carcinoma. However the third component (histology) suggested a benign lesion. The members of the MDT were divided in their opinion. The matter was discussed in full with the patient. An excision biopsy would entail further surgery (i.e., mastectomy), should the final diagnosis confirm a carcinoma. Per-operative frozen section was an option but was not performed for various reasons. Current surgical guideline discourages frozen sections with immediate pathological reporting of surgical breast biopsies.1 Determining exact pathology and the desirable resection margin of a large lesion on frozen section can be tedious, time consuming and has intrinsic false negative rates.2 Moreover, excision of a large lesion in a relatively small breast would leave the patient with unacceptable cosmetic appearance, necessitating further surgery. The patient felt that she was not prepared to take the risk and go through the possibility of second operation. Hence she opted for a simple mastectomy. The final diagnosis was an epidermoid cyst of the breast. To the best of our knowledge, no case of epidermoid cyst of breast necessitating mastectomy has been reported in the literature before. This makes the case report unique.
Epidermoid cysts arise from the proliferation of epidermal cells within a circumscribed space of the dermis. Aetiology may be congenital, traumatic following implantation of epithelium or developmental following squamous metaplasia of normal columnar cells within a dilated duct in cases of fibrocystic disease.3,4 Indeed, the woman in this case reported a history of trauma to the breast. However, exact relevance of such history is difficult to discern. Epidermal cysts have also been reported following reduction mammoplasty due to implantation of torn fragments of epidermis deep within the breast tissue.5 Microscopically, they are lined with stratified squamous epithelium and filled with laminated keratin which is usually a thick, white, and flaky material.6,7
Epidermoid cysts of the breast are rare compared to similar lesions occurring in other parts of the human body such as the scalp, back and neck. Malignant transformation has been reported in 0.5–19% of cases.8,9 As the incidence of epidermoid cyst occurring in the breast parenchyma is small, with variable reports on the incidence of its malignant change, the actual percentage is uncertain.2 Preoperative differentiation between benign and malignant epidermoid cyst is not always possible.10,11 Mammographic and sonographic features of epidermoid breast cyst may vary. An intermediate to high T2 signal mass with occasional low signal debris associated with no central enhancement on Magnetic Resonance Imaging (MRI) has been reported to be helpful in strengthening the diagnosis.12 Initial misdiagnosis of epidermal cyst can be due to its ill-defined borders and heterogenous echogenicity.6,13
Excision of such lesions should be offered to relieve symptoms, prevent complications and in some cases, for cosmetic reasons. The pros and cons of surgery, alternatives, and risks of surgery should be discussed with the patient in full. An unrestricted Medline search revealed that it is rare for an epidermoid cyst of breast to present as such an advanced lesion. It is recommended that such a lesion should be excised because of underlying malignant potential. Excision of a large ‘benign’ lesion, however, may sometime entail mastectomy, particularly in a relatively small breast. We strongly advocate that patients should be offered the option of breast reconstruction in such cases. However reconstruction was not an option in this case as the patient did not wish to have further procedure.
British Association of Surgical Oncology (BASO) guidelines clearly emphasises the importance of involving multidisciplinary team in making decisions while dealing with suspected breast cancers.1 It is possible that MDT members may fail to reach a consensus in some complex cases. Furthermore, General Medical Council states that as part of the informed consent process, patients must receive sufficient information, in a way that they can understand, to enable them make informed decisions about their care.14 The patient in this case, was given options of diagnostic open excision, followed by mastectomy, should it confirm the lesion to be a cancer. She was not prepared to have a second procedure and opted for mastectomy.
4. Conclusions
Diagnostic dilemma while dealing with a suspected breast cancer is not rare. Involvement of multidisciplinary team as well as patient is important in the decision-making. A breast-conservative surgery is considered appropriate in most of such situations. However, mastectomy may play a role in certain circumstances. The case reported illustrates such a situation, where the patient opted for mastectomy for an uncertain breast lesion, which turned out to be a benign epidermoid cyst of the breast. The report also exemplifies the rare presentation of a deep seated large epidermoid cyst of breast, which mimicked carcinoma and caused diagnostic confusion. No such case of epidermoid cyst of the breast necessitating mastectomy has been reported before. In such cases, patients should be offered the option of breast reconstruction.
Contribution
All the aforementioned authors had access to the data, and a role in writing the manuscript.
Conflicts of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- 1.Association of Breast Surgery at BASO Surgical guidelines for the management of breast cancer. European Journal of Surgical Oncology. 2009;35(Suppl. 1):S1–S22. doi: 10.1016/j.ejso.2009.01.008. http://www.cancerscreening.nhs.uk/breastscreen/publications/ABS-BASO-guidelines.pdf [DOI] [PubMed] [Google Scholar]
- 2.Chiu M.Y., Ho S.T. Squamous cell carcinoma arising from an epidermal cyst. Hong Kong Medical Journal. 2007;13(6):482–484. [PubMed] [Google Scholar]
- 3.Lam S.Y., Kasthoori J.J., Mun K.S., Rahmat K. Epidermal inclusion cyst of the breast:a rare benign entity. Singapore Medical Journal. 2010;51(12):e191–e194. [PubMed] [Google Scholar]
- 4.Warvi W.N., Gates O. Epithelial cysts and cystic tumours of the skin. American Journal of Pathology. 1943;19(5):765–783. [PMC free article] [PubMed] [Google Scholar]
- 5.Fajardo L.L., Bessen S.C. Epidermal inclusion cyst after reduction mammoplasty. Radiology. 1993;186(1):103–106. doi: 10.1148/radiology.186.1.8416547. [DOI] [PubMed] [Google Scholar]
- 6.Kowand L.M., Verhulst L.A., Copeland C.M., Bose B. Epidermal cyst of the breast. Canadian Medical Association Journal. 1984;131(3):217–219. [PMC free article] [PubMed] [Google Scholar]
- 7.Morris P.C., Cawson J.N., Balasubramanium G.S. Epidermal cyst of the breast:detection in a screening programme. Australasian Radiology. 1999;43(1):12–15. doi: 10.1046/j.1440-1673.1999.00618.x. [DOI] [PubMed] [Google Scholar]
- 8.Otto H., Breining H. Benign and malignant breast tumours with squamous cell differentiation. Der Radiologe. 1987;27(4):196. [PubMed] [Google Scholar]
- 9.Menville J.G. Simple dermoid cysts of the breast. Annals of Surgery. 1936;103(1):49–56. doi: 10.1097/00000658-193601000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chantra P.K., Tang J.T., Stanley L.W. Circumscribed fibrocystic mastopathy with formation of an epidermal cyst. American Journal of Roentgenology. 1994;163(4):831–832. doi: 10.2214/ajr.163.4.8092018. [DOI] [PubMed] [Google Scholar]
- 11.Bergmann-Koester C.U., Kolberg H.C., Rudolf I., Krueger S., Gellissen J., Stoeckelhuber B.M. Epidermal cyst of the breast mimicking malignancy:clinical, radiological and histological correlation. Archives of Gynaecology and Obstetrics. 2006;273(5):312–314. doi: 10.1007/s00404-005-0019-9. [DOI] [PubMed] [Google Scholar]
- 12.Kim H.K., Kim S.M., Lee S.H., Racadio J.M., Shin M.J. Subcutaneous epidermal inclusion cysts:ultrasound (US) and MR imaging findings. Skeletal Radiology. 2011;40(11):1415–1419. doi: 10.1007/s00256-010-1072-4. [DOI] [PubMed] [Google Scholar]
- 13.Chatterjee P.K., Roy S.N. Large epidermal cyst of breast simulating malignant growth. British Medical Journal. 1979;1(6157):167–168. doi: 10.1136/bmj.1.6157.167-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.General Medical Council. Consent: patients and doctors making decisions together Guidance for doctors. 2008:1–60. http://www.gmc-uk.org/static/documents/content/Consent_2008.pdf.


