Abstract
Objective. MTX is widely used to treat synovitis in PsA without supporting trial evidence. The aim of our study was to test the value of MTX in the first large randomized placebo-controlled trial (RCT) in PsA.
Methods. A 6-month double-blind RCT compared MTX (15 mg/week) with placebo in active PsA. The primary outcome was PsA response criteria (PsARC). Other outcomes included ACR20, DAS-28 and their individual components. Missing data were imputed using multiple imputation methods. Treatments were compared using logistic regression analysis (adjusted for age, sex, disease duration and, where appropriate, individual baseline scores).
Results. Four hundred and sixty-two patients were screened and 221 recruited. One hundred and nine patients received MTX and 112 received placebo. Forty-four patients were lost to follow-up (21 MTX, 23 placebo). Twenty-six patients discontinued treatment (14 MTX, 12 placebo). Comparing MTX with placebo in all randomized patients at 6 months showed no significant effect on PsARC [odds ratio (OR) 1.77, 95% CI 0.97, 3.23], ACR20 (OR 2.00, 95% CI 0.65, 6.22) or DAS-28 (OR 1.70, 95% CI 0.90, 3.17). There were also no significant treatment effects on tender and swollen joint counts, ESR, CRP, HAQ and pain. The only benefits of MTX were reductions in patient and assessor global scores and skin scores at 6 months (P = 0.03, P < 0.001 and P = 0.02, respectively). There were no unexpected adverse events.
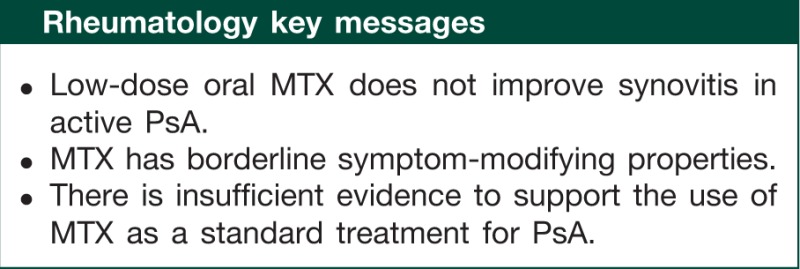
Conclusions. This trial of active PsA found no evidence for MTX improving synovitis and consequently raises questions about its classification as a disease-modifying drug in PsA.
Trial registration. Current Controlled Trials, www.controlled-trials.com, ISRCTN:54376151.
Keywords: psoriatic arthritis, methotrexate, placebo, randomized controlled trial
Introduction
Randomized controlled trials (RCTs) involving placebos help identify if new treatments are effective. They are also crucial in identifying widely used standard treatments that are actually ineffective [1]. Oral MTX has become a standard treatment for the PsA and is recommended in all recent guidelines [2–6]. Furthermore, in active PsA, the UK National Institute for Health and Clinical Excellence (NICE) recommends MTX be used before treatments of proven effectiveness, notably TNF inhibitors [7]. However, all these recommendations have been made on the basis of experts' consensus. The efficacy of oral MTX in PsA has not been convincingly proven in a placebo-controlled RCT.
Active PsA should be treated by drugs or biologic treatments that reduce joint inflammation, lower acute-phase markers and improve disability. In RA, such drugs are grouped together as DMARDs. Biologics, like TNF inhibitors, are highly effective in PsA; their value has been shown in a large number of placebo-controlled RCTs [8–12]. LEF has also been shown to be effective in a placebo-controlled RCT [13]. There is only weak evidence that other conventional drugs like gold injections and SSZ are effective and there is no definitive RCT evidence for oral MTX.
MTX can cause serious adverse events [14, 15]. Its continuing widespread use in PsA is questionable in the absence of supporting evidence from placebo-controlled RCTs. The Methotrexate in Psoriatic Arthritis (MIPA) trial specifically addresses this previously unresolved question.
Methods
Trial design
MIPA was a 6-month, double-blind, parallel-group RCT in which patients with active PsA were randomized to receive MTX (target dose 15 mg/week) or matched placebo. The allocation ratio of active to placebo treatment was 1 : 1.
Patients
MIPA enrolled males and females aged at least 18 years with PsA currently attending UK specialist rheumatology clinics.
Inclusion criteria
These comprised: (i) clinically apparent psoriasis (skin or nails) and active inflammatory synovitis involving at least one peripheral joint (adapted from the two mandatory criteria of Bennett [16], following the approach of Gladman [17] and Salvarani et al. [18]); (ii) a constant level of NSAID therapy for at least 1 month; (iii) previous DMARD therapy discontinued for at least 1 month and (iv) willing and able to give informed consent.
Exclusion criteria
These comprised: (i) other inflammatory arthropathies or arthritis mutilans; (ii) systemic steroid therapy currently or within the last 3 months; (iii) previous or current treatment with MTX; (iv) other serious medical disorders including liver, renal and cardiac disease; (v) women of childbearing potential not taking adequate contraceptive precautions; and (vi) abnormal full-blood counts and liver function tests or other contraindications to MTX therapy.
Treatments
Experimental treatment
Patients were seen monthly to adjust their trial medication and for safety monitoring. MTX was given initially at 7.5 mg/week, increased at 4 weeks to 10 mg/week and at 8 weeks to the target dose of 15 mg/week. In patients with persistently active disease, the dosage could be increased at the discretion of the supervising rheumatologist to 20 mg/week at 4 months and 25 mg/week at 5 months.
Control treatment
Patients received matched placebos that were increased similarly.
Concomitant therapy
All patients received oral folic acid (5 mg weekly) and anti-emetic therapy as needed. They continued their current NSAIDs and analgesics at unchanged dosages. Oral or i.m. steroids were not used and only one IA steroid was allowed.
Outcomes
Patients were assessed at baseline, 3 and 6 months. The primary outcome measure was the PsA response criteria (PsARC) [19]. Global secondary outcome assessments comprised ACR 20% improvement criteria (ACR20) [20] and DAS for 28 joints (DAS-28) [21]. Individual secondary outcome measures comprised swollen and tender joint counts (66/68 joints based on European League Against Rheumatism (EULAR)/ACR standard methods) [22]; pain score, patient global assessment and assessor global assessment (using 100-mm visual analogue scores); ESR and CRP; function assessed using the HAQ; PsA skin index (PASI) and the nail disease score of Jones et al. [23]; withdrawal from treatment and adverse reactions.
Sample size
The initial sample size was based on the study of SSZ in PsA by Clegg et al. [19], which showed that 45% of patients taking placebo responded to treatment using the PsARC composite index. We considered a 66% response rate for active treatment (50% increased response rate) would constitute a relevant treatment effect. While MIPA was ongoing and since the Clegg trial was published, several more RCTs were completed using the PsARC [13, 24–26]. Based on these new data the MIPA Data and Ethics Committee recommended reducing the response rates for placebo to 35% and reducing the active response rate to 59%; these were average reported response rates for placebo and active treatment in trials of potential DMARDs in PsA. To detect a difference at the 5% level with 90% power between active treatment with a response rate of 59% and placebo treatment with a response rate of 35% requires enrolling 89 patients per group. Allowing for a 20% drop out rate, this meant recruiting 220 cases. The sample size was defined following the approach recommended by Machin et al. [27], and the sample size calculation checked against their most recent recommendations.
Randomization, sequence generation, allocation concealment and implementation
Patients were randomly allocated to receive MTX or placebo. The allocation sequence was generated by the trial statistician using random number tables. Randomization, stratified by centre, used random treatment assignment in blocks of four. In each centre randomization numbers were assigned to patients in chronological order as they passed their screening assessments. Metrologists and the trial coordinator were unaware of the allocation sequence. Treatment assignments were in a locked cabinet in the co-ordinating centre pharmacy for emergency access. The MTX and placebo were identical in appearance. They were pre-packed in identical containers and consecutively numbered for patients by centre according to the randomization schedule. Each patient received the treatment in the corresponding pre-packed container.
Statistical methods
All data management and analyses were done using Stata, version 11.0 (StataCorp, College Station, TX, USA) and the R statistical package (R Development Core Team, 2008). Baseline characteristics were summarized by randomized group. Descriptive summary statistics of each group were presented as mean (s.d.) for continuous normally distributed and median and interquartile range for not normally distributed outcome variables and frequencies and percentages for categorical variables. Initial statistical analysis was blinded with the statistician unaware of the treatment groups.
All participants had observations at baseline. However, some subjects had missing data on the outcome variables at 3 and 6 months or both. All missing data were imputed regardless of the reason(s) the data were missing. For the subjects who had missing outcomes at 3 months, the baseline outcomes and other covariates (treatment group, sex, age and disease duration) were used to impute the missing data at 3 months. For the subjects who had missing outcomes at 6 months, baseline and 3-month outcomes with covariates were used to impute the missing values. If the outcome variables were missing at 3 and 6 months then the outcome variables at 3 months were imputed first, followed by the outcomes at 6 months. Assuming unobserved measurements were missing at random, we imputed missing data by multiple imputation using chained equations with 20 cycles, where at the end of the cycle one imputed data set is created and the process was repeated to create 20 imputed data sets. The 20 data sets were separately analysed and the results combined using Rubin's rules [28–30], and therefore the estimates and s.e.s presented here are the combined ones. As an additional check of the robustness of the analyses performed to the missing-at-random assumption, we further analysed the individual component data that comprise the PsARC and ACR20 (i.e. tender and swollen joint counts, patient's and assessor's global assessment measurements, acute-phase reactant and HAQ) using the linear increments method of Diggle et al. [31, 32] to handle the missingness. As the results obtained using this approach were qualitatively the same as that of the multiple imputation approach adopted, we report only the findings from the standard multiple imputation analyses.
The effects of treatment on PsARC, ACR20 and DAS-28 responder measures were assessed at 3 and 6 months using logistic regression, controlling for age, sex and disease duration. Intention to treat (ITT)-type analyses were performed on the imputed data from all randomized patients. Additionally, completer analyses were performed on those who completed 6 months of treatment. The estimates are presented as odds ratios (OR) with 95% CIs for the effect of MTX. Robust s.e.s were used throughout to adjust for the different geographical regions in the model. A pre-planned subgroup analysis investigating whether the treatment effect varies with disease subtype (i.e. oligoarticular and polyarticular) was performed by adding the interaction term between treatment and disease subtype (oligoarticular and polyarticular) to the models. This was an exploratory pre-planned subgroup analysis, as the study was not powered to take account of these subgroups.
The individual component data (tender and swollen joint counts, patient's and assessor's global assessment measurements, ESR, CRP, pain and HAQ) were evaluated by linear regression models, and the point estimates are β-coefficients with robust s.e.s accounting for geographical clustering. These models controlled for the individual's baseline, age, gender and disease duration. Statistical significance was determined at the 5% level using a two-sided test throughout.
Ethics review
The trial was approved by the South East Multi-Centre Research Ethics Committee and by local research ethics committees at each centre. All enrolled patients gave written informed consent.
Results
Recruitment, patients and treatment
Four hundred and sixty-two patients were screened at 22 rheumatology units from 13 January 2003. Two hundred and forty-one patients were not enrolled; 148 of these were ineligible and 93 did not consent (Fig. 1). Two hundred and twenty-one patients were recruited. Follow-up was completed by 3 July 2008 and the data validated in 2009. One hundred and nine patients were randomized to receive MTX and 112 patients were randomized to receive placebo. Table 1 summarizes the characteristics of the randomized patients.
Fig. 1.
CONSORT flowchart for MIPA trial.
Table 1.
Details of patients enrolled
| MTX (n = 109) | Placebo (n = 112) | |
|---|---|---|
| Gender, females : males, n (%) | 53 (49) : 56 (51) | 44 (39) : 68 (61) |
| Ethnicity, white European/other, n (%) | 105 (96)/4 (4) | 109 (97)/3(3) |
| Age, mean (s.d.), years | 46 (13) | 51 (11) |
| Disease duration, years | 1 (1–5) | 1 (1–6) |
| Smoking status | ||
| Never, n (%) | 57 (53) | 51 (45) |
| Previous, n (%) | 23 (21) | 38 (34) |
| Current, n (%) | 28 (26) | 23 (21) |
| Height, cm | 170 (162–177) | 170 (162–178) |
| Weight, kg | 83 (74–96) | 86 (74–97) |
| Pattern of arthritis, oligoarticular/polyarticular disease, n (%) | 38 (35)/71 (65) | 41 (37)/71 (63) |
| Previous SSZ treatment, n (%) | 25 (23) | 22 (20) |
| Concomitant analgesics, n (%) | 10 (9) | 13 (12) |
| Concomitant NSAIDs, n (%) | 89 (82) | 90 (80) |
| Tender joint count, range 0–68 | 9 (4–15) | 11 (6–18) |
| Swollen joint count, range 0–66 | 6 (3–12) | 6 (2–11) |
| ESR, mm/h | 15 (7–28) | 12 (6–24) |
| CRP, mg/dl | 7 (5–16) | 9 (5–19) |
| HAQ, range 0–3 | 0.88 (0.38–1.50) | 1.13 (0.63–1.63) |
| Patient's global assessment, 100-mm VAS | 47 (30–70) | 49 (28–69) |
| Assessor's global assessment, 100-mm VAS | 39 (28–56) | 41 (30–57) |
| Pain, 100-mm VAS | 36 (25–59) | 42 (27–65) |
Medians (interquartile range) are shown for clinical variables, unless otherwise mentioned.
Follow-up, reported in accordance with Consolidated Standards of Reporting Trials (CONSORT) recommendations, is shown in Fig. 1. Forty-four patients were lost to follow-up (21 receiving MTX and 23 receiving placebo). Twenty-six patients discontinued treatment (14 receiving MTX and 12 receiving placebo). Overall 23% of follow-up data were missing at 6 months. The missing data were imputed for the ITT analysis.
The target dose of 15 mg weekly MTX was achieved at some point in the trial by >90% of patients receiving active treatment. At 3 months, 93% of patients receiving MTX were taking 15 mg weekly. At Month 5, 78% were taking 15 mg with 11% receiving higher dosages (17.5 and 20 mg weekly) and 11% lower doses (7.5, 10 and 12.5 mg weekly). One hundred and seventy-nine (81%) patients received concomitant NSAIDs (89 patients receiving MTX and 90 placebo). Commonly used NSAIDs were diclofenac (59 patients) and ibuprofen (35 patients); 35 patients received coxibs.
Global indices in all randomized patients
ITT analyses of global indices using logistic regression (adjusted for age, sex and disease duration) found no statistically significant treatment effect with PsARC (OR 1.77, 95% CI 0.97, 3.23) after 6 months of MTX treatment (Table 2). There was also no evidence of significant treatment effects with ACR20 (OR 2.00, 95% CI 0.65, 6.22) or DAS-28 (OR 1.70, 95% CI 0.90, 3.17). No global index showed significant treatment effects at 3 months.
Table 2.
Effect of MTX on PsARC and other global indices in ITT analysis of all randomized patients
| Global index | OR (95% CI) | P-value |
|---|---|---|
| PsARC | 1.77 (0.97, 3.23) | 0.06 |
| ACR20 responders | 2.00 (0.65, 6.22) | 0.23 |
| DAS-28 responders | 1.70 (0.90, 3.17) | 0.10 |
ORs were adjusted for age, sex and disease duration.
Individual outcome measures in all randomized patients
ITT analyses using linear regression models (adjusted for age, sex, disease duration and individual baseline score) showed no evidence of a significant treatment effect of MTX on joint counts, ESR, CRP, pain and HAQ scores after 6 months treatment (Table 3). There were statistically significant treatment effects on assessor global assessments (coefficient −8.0, 95% CI −13.6, −2.4, P = 0.01) and patient global assessments (coefficient −9.2, 95% CI −17.0, −1.4, P = 0.02). No individual measure showed a statistically significant treatment effect at 3 months.
Table 3.
Individual outcome measures in ITT analysis of all randomized patients
| MTX (n = 109) |
Placebo (n = 112) |
Linear regression |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Measures | Initial | 3 months | 6 months | Change 0–6 | Initial | 3 months | 6 months | Change 0–6 | Adjusteda, β-coefficient (95% CI) | P-value |
| Tender joint count | 11.9 (9.8, 14.0) | 7.9 (6.1, 9.6) | 7.7 (5.7, 9.7) | 4.2 (2.1, 6.3) | 13.6 (11.6, 15.7) | 9.9 (7.8, 11.9) | 10.0 (7.5, 12.5) | 3.7 (1.2, 6.4) | −1.1 (−3.8, 1.5) | 0.41 |
| Swollen joint count | 8.7 (7.2, 10.1) | 5.7 (4.3, 7.1) | 4.6 (3.1, 6.0) | 4.1 (2.3, 5.9) | 8.0 (6.5, 9.5) | 5.4 (4.3, 6.6) | 5.2 (3.8, 6.6) | 2.8 (1.1, 4.5) | −0.9 (−2.7, 1.2) | 0.48 |
| ESR | 20.9 (16.7, 25.0) | 17.8 (13.0, 22.6) | 14.7 (11.3, 18.1) | 6.2 (2.5, 9.9) | 19.3 (15.1, 23.2) | 18.3 (14.0, 22.5) | 15.6 (11.8, 19.4) | 3.6 (−0.6, 7.7) | −0.9 (−5.0, 3.7) | 0.71 |
| CRP | 11.5 (9.4, 13.5) | 9.6 (7.6, 11.6) | 9.4 (6.9, 12.0) | 2.0 (−0.7, 4.7) | 15.2 (11.6, 18.9) | 11.9 (9.4, 14.4) | 11.7 (8.4, 14.9) | 3.6 (−0.3, 7.4) | −0.6 (−4.2, 2.9) | 0.73 |
| Pain | 40.5 (36.2, 44.8) | 33.6 (28.2, 39.1) | 28.8 (23.2, 34.4) | 11.7 (5.9, 17.5) | 46.4 (41.8, 50.9) | 37.7 (31.8, 43.6) | 38.3 (31.8, 44.8) | 8.1 (1.3, 14.9) | −7.0 (−15.3, 1.2) | 0.09 |
| HAQ | 0.9 (0.8, 1.1) | 0.7 (0.6, 0.8) | 0.7 (0.6, 0.9) | 0.2 (0.1, 0.4) | 1.2 (1.02, 1.28) | 1.0 (0.9, 1.2) | 1.0 (0.9, 1.2) | 0.1 (0.0, 0.3) | −0.1 (−0.3, 0.02) | 0.10 |
| Patient global assessment | 49.8 (45.1, 54.4) | 36.6 (31.3, 41.8) | 31.8 (25.9, 37.7) | 18.0 (12.0, 24.0) | 49.7 (45.1, 54.4) | 41.5 (35.8, 47.1) | 42.2 (36.4, 48.0) | 7.5 (0.9, 14.1) | −9.2 (−17.0, −1.4) | 0.02 |
| Assessor's global assessment | 41.1 (37.7, 44.5) | 30.4 (25.9, 34.8) | 23.3 (19.9, 26.6) | 17.9 (13.9, 21.8) | 43.7 (40.2, 47.2) | 33.7 (29.3, 40.0) | 33.0 (28.5, 37.5) | 10.7 (5.9, 15.4) | −8.0 (−13.6, −2.4) | 0.01 |
Mean disease activity measures (95% CIs) are shown initially and at 3 and 6 months together with changes >6 months.
aDifferences between treatments are shown as assessed by linear regression analyses adjusted for age, gender, disease duration and individual baseline score.
Effects on skin and nails in all randomized patients
Baseline mean PASI scores were similar in the MTX (mean 3.76, 95% CI 2.83, 4.78) and placebo groups (3.79, 95% CI 2.79, 4.78). Despite these low initial PASI scores, the ITT analysis showed mean PASI scores in all randomized patients fell to 2.22 (95% CI 1.62, 2.82) with MTX and 3.13 (95% CI 2.34, 3.92) with placebo. Linear regression analysis, adjusted for age, sex, disease duration and baseline PASI score, showed a significant reduction with MTX compared with placebo (adjusted treatment difference −0.93; 95% CI −1.71, −0.15; P = 0.02).
We also analysed PASI-75 response rates and nail scores. The ITT analysis showed no significant differences in PASI-75 response rates using logistic regression analyses (adjusted for age, sex and disease duration) (OR 1.26, 95% CI 0.58, 2.72). Nail scores showed no evidence of a treatment effect in any patient group at 3 and 6 months.
Valid compliant completer analyses
These analyses excluded patients who were lost to follow-up, discontinued treatment or who met a pre-defined reason for exclusion from analysis (Fig. 1). Logistic regression (adjusted for age, sex and disease duration) showed that at 6 months the OR of PsARC responses with MTX in these patients reached statistical significance (OR 2.33, 95% CI 1.13, 4.84, P = 0.02). However, there was no evidence of a treatment effect on ACR20 (OR 1.67, 95% CI 0.74, 3.78, P = 0.22) and DAS-28 responses (OR 2.07, 95% CI 0.98, 4.38, P = 0.06). There was no evidence of a significant treatment effect in any global index at 3 months. A more detailed completer analysis is given in supplementary Section SA, available as supplementary data at Rheumatology Online.
Impact of polyarticular disease
We examined whether effect of treatment on global indices (PsARC, ACR20, DAS-28) varied between disease subtype: polyarticular disease (initially more than four swollen joints) and oligoarticular disease (initially four or less swollen joints). We included an interaction term between treatment and disease subtype on each global index in the ITT analysis of all randomized patients. This showed that treatment effect on global indices did not vary between disease subtype (P = 0.574 for interaction). Details of the effect of disease subtype on individual outcome measures are given in supplementary Section SB, available as supplementary data at Rheumatology Online.
Adverse effects
In 16 patients, adverse effects were the principal reason for withdrawal from the trial (9 MTX, 7 placebo); they were also a secondary reason in 3 other patients (2 MTX, 1 placebo) in whom problems with persisting disease activity stopped them from continuing treatment. Seven withdrawals (five MTX, two placebo) were attributed to potential MTX toxicity. Common adverse events (>5% of one treatment arm) comprised nausea and vomiting (38 patients receiving MTX, 16 patients receiving placebo), respiratory tract infections (31 MTX, 25 placebo), abdominal pain (16 MTX, 6 placebo) and abnormal liver function tests (12 MTX, 2 placebo).
Discussion
Our ITT analysis of all randomized patients in MIPA found no statistically significant evidence that 6 months of MTX treatment was more likely than placebo to improve any rheumatology-related global response index in PsA, although the effect sizes were in the direction of improvement. In addition, there was no evidence that MTX had significant benefits on objective measures of synovitis including joint counts, ESR and CRP levels. We consequently conclude that there is presently no evidence that MTX improves inflammatory synovitis in active PsA; this would be required for a true disease-modifying effect. However, MTX did significantly improve assessors' and patients’ global assessments, suggesting it may have symptom-modifying effects. It also showed a positive effect on psoriasis skin scores, consistent with its known efficacy in psoriasis; the benefit was relatively limited in our patient group because of their relatively low initial skin scores [33].
Valid compliant completer analyses are generally regarded as suboptimal because they tend to overestimate treatment effects due to selective withdrawal for lack of efficacy in the placebo group. Conversely, this means they are extremely sensitive at detecting any evidence for a treatment effect. In our analysis of valid compliant completers, the PsARC, which is particularly sensitive to changes in patients' global responses, showed borderline improvement. However, ACR20 and DAS-28 scores, which place greater emphasis on joint counts, continued to show no significant treatment benefits. New global measures for PsA are being developed, which may provide different perspectives on treatment in the future [34–37].
Two previous placebo-controlled RCTs evaluated MTX in PsA. High-dose (1–3 mg/kg) i.v. MTX, studied in 21 patients, reduced joint swelling and tenderness and the ESR. However, seven patients had treatment-related leucopenia and one died, suggesting unacceptable toxicity [38]. Low-dose oral MTX (7.5–15 mg/week) was studied in 37 patients. Only physician global assessments and skin psoriasis improved with treatment, replicating the findings in MIPA [39]. Another RCT of 35 patients compared immediate MTX with treatment delayed by 3 months in early PsA [40]. All clinical variables improved over time and there was evidence that tender and swollen joint counts improved more rapidly with early MTX. Another RCT, also involving 35 patients, compared MTX with ciclosporin and found similar improvements with both [41]. A final RCT of 72 patients compared the impact of adding ciclosporin to MTX therapy in PsA. In that trial, both groups improved, and the only significant treatment effect was on PASI scores [42]. None of these five trials provides strong evidence in favour of MTX in PsA. Systematic reviews of MTX in PsA also underline the paucity of evidence [43, 44].
We consider that effective DMARDs in PsA should reduce joint counts in direct head-to-head comparisons with placebo. MIPA shows no evidence that oral MTX has such effects. There was also no evidence that MTX reduced joint counts in the only comparable trial of oral MTX [39], five trials of SSZ and one trial of auranofin [19, 45–49]. The LEF trial in PsA did show treatment significantly improved swollen and tender joint counts compared with placebo [13]. We conclude that the evidence that either MTX or SSZ has DMARD-like effects in PsA is inconclusive. Despite the negative results seen in MIPA, it is possible that MTX might be effective in some circumstances in patients with PsA. First, giving higher doses of MTX for longer periods of time might have given positive results. However, in RA, placebo-controlled RCTs show 15 mg weekly or less MTX is effective within 3 months [50], suggesting a major treatment effect is unlikely to be overlooked at the doses and duration used in MIPA. Secondly, the inclusion criteria for MIPA allowed patients with fewer active joints to be enrolled compared with some other PsA trials. For example, trials of SSZ [19], MTX [39] and LEF [13] all required at least three active joints. However, most patients in MIPA were more active than the minimum entry requirement and, as discussed in detail below, patients with polyarticular PsA did not show a better response to MTX. MIPA was designed as a pragmatic trial evaluating the use of MTX in current clinical care, and in this context it is important to note that it enrolled similar patients to those reported in observational studies of routine practice [51]. Finally, MIPA might have been too small to detect the effect of MTX. The sample size calculation for MIPA used PsARC responder rates from previous PsA trials. However, using multiple imputation methods makes it inappropriate to give individual responder rates in the analysis of all randomized patients, as the imputation methods create 20 imputations. Consequently, we have used OR to report a point estimate for the imputed data. The initial sample size calculation would have given an OR of 2.7, which is the minimal OR given by agents thought to be effective in PsA on the basis of published trials. The results of MIPA lay between ORs of 1.8 and 2.3 (for all patients and completers, respectively). In contrast, trials of effective agents give strong effects; for example, the LEF trial achieved an OR of 3.4 [13] and an etanercept trial reported an OR >20 [8]. Although MIPA many have been too small to detect minimal improvements in the PsARC, the clinical benefit of such effects is questionable. We believe a larger trial would not only be impractical but also would be unwarranted in the face of more effective alternatives.
The subgrouping of PsA patients creates complex analytical issues. Our pre-specified subgroup analyses did not provide strong evidence that disease subtype (polyarticular or oligo-articular) had a major impact on treatment outcomes. However, there are other PsA subgroups, including some patients who meet criteria conventionally used to define trial active RA [52]. Further subgroup analyses provide some evidence that the subgroup of PsA patients who meet the criteria for trial active RA MTX had more impact on tender joint counts. Conventional concerns about subgroup analysis [53] mean caution is required in drawing conclusions from our subgroup analyses. However, it is possible that the positive results in the LEF trial in PsA reflect a greater preponderance of RA-like PsA patients in that trial.
Withdrawals and the imputation of missing data might explain our negative results. However, the placebo 6-month completion rate in MIPA was better than the 45% reported in the LEF trial [13], though lower than the 78% reported in the SSZ trial [19]. Overall, there is no evidence that completion rates were particularly low in MIPA. We used multiple imputation methods to account for missing data and adjusted our analyses for baseline variables. Additionally, the robustness of our imputation analyses to missing data was assessed by carrying out further sensitivity analyses using the linear increments method. We consider it unlikely that the missing-at-random assumption or other aspects of the imputation method are likely to explain the non-significant findings of MIPA.
MIPA took a decade from inception to completion. Many specialists were unwilling to participate because they believed that the efficacy of MTX was established and believed a placebo-controlled trial was unwarranted. With treatments of proven efficacy the case for placebo-controlled trials is weak [54, 55], but this is not the case for MTX in PsA. Ineffective treatments in PsA expose patients to risks of adverse events that may cause more harm than short-term placebo therapy [56]. Observational studies cannot replace placebo-controlled RCTs because, in a variable disease like PsA, treatment effects cannot be disentangled from regression to the mean. Observational studies of MTX in PsA [51, 57] mirror the changes in MIPA, suggesting their effects are best explained by regression to the mean.
There is strong evidence that low-dose oral MTX is effective in adults with RA [50]. It is also effective in juvenile arthritis [58]. We have found no evidence that MTX is effective in other forms of adult non-rheumatoid inflammatory arthritis. MIPA provides no evidence that it is effective in PsA, and other RCTs suggest that oral MTX is ineffective in early undifferentiated arthritis [59] and AS [60]. In contrast, biologics like TNF inhibitors appear effective in a broad range of inflammatory arthropathies. As MTX is not licensed for PsA and two RCTs have now provided insubstantial evidence of its benefit for treating synovitis, we therefore believe PsA is best managed using effective licensed conventional drugs like LEF or biologics. We also think that guidelines for treating PsA need to be revisited so that the sequencing of conventional drugs before biologics are used is re-evaluated.
Several unanswered questions remain. First, treating PsA involves managing all its different components [61] and also its skin involvement, which responds to MTX. Therefore many patients with PsA may need to receive MTX. Secondly, there is some evidence that MTX may be beneficial when used in combination with biologics in PsA. The Swedish register shows that it increases the time patients remain on treatment [62]. Thirdly, MTX might be effective as part of an intensive treatment strategy alongside other DMARDs. This possibility is currently being evaluated in an ongoing UK trial: Tight Control of Psoriatic Arthritis (TICOPA; NCT01106079). Finally, PsA patients with a rheumatoid-like pattern of disease may respond to MTX. As a consequence, there are justifiable reasons for treating some patients with PsA with MTX, even though there is insufficient evidence for it being a standard treatment for all patients with PsA who need their synovitis to be suppressed.
Supplementary data
Supplementary data are available at Rheumatology Online.
Acknowledgements
We are grateful to the following UK collaborators who, in addition to the clinical authors, entered patients into the trial: Dr M. Bukhari, Lancaster; Dr A. Coulson, Withybush; Dr C. Deighton, Derby; Dr N. Cheung, London; Dr D. Doyle, London; Dr C. Erhardt, London; Dr P. Hickling, Plymouth; Dr S. Jones, Cardiff; Dr L. Kay, Newcastle; Dr A. Keat, London; Dr A. Leak, Margate; Prof. I. McInnes, Glasgow; Dr F. McKenna, Manchester; Dr S. Patel, London; Dr P. Williams, Medway. We are also grateful for further statistical advice from Caroline Dore, MRC Clinical Trials Unit.
Funding: The trial was supported by a Clinical Trial Grant from Arthritis Research UK (grant number 15607). Research support costs were provided by the London South Comprehensive Local Research Network of the National Institute for Health Research. Active and placebo MTX tablets were provided by Wyeth (UK). D.L.S. was an NIHR Senior Investigator. B.D.M.T. and A.G.O. were funded by the UK Medical Research Council (grant number U.1052.00.009). King's College London was the sponsor of the trial.
Disclosure statement: N.J.M. has received honoraria for advisory boards or speaking or his Institute has received grant support from Abbott Laboratories and Pfizer. All other authors have declared no conflicts of interest.
References
- 1.Alderson P, Groves T. What doesn't work and how to show it. BMJ. 2004;328:473. doi: 10.1136/bmj.328.7438.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ritchlin CT, Kavanaugh A, Gladman DD, et al. Treatment recommendations for psoriatic arthritis. Ann Rheum Dis. 2009;68:1387–94. doi: 10.1136/ard.2008.094946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyle S, Chandler D, Griffiths CE, et al. Guideline for anti-TNF-alpha therapy in psoriatic arthritis. Rheumatology. 2005;44:390–7. doi: 10.1093/rheumatology/keh514. [DOI] [PubMed] [Google Scholar]
- 4.Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 4. Guidelines of care for the management and treatment of psoriasis with traditional systemic agents. J Am Acad Dermatol. 2009;61:451–85. doi: 10.1016/j.jaad.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 5.Gottlieb A, Korman NJ, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 2. Psoriatic arthritis: overview and guidelines of care for treatment with an emphasis on the biologics. J Am Acad Dermatol. 2008;58:851–64. doi: 10.1016/j.jaad.2008.02.040. [DOI] [PubMed] [Google Scholar]
- 6.Dernis E, Lavie F, Salliot C, et al. Pharmacological treatment (biotherapy excluded) of peripheral psoriatic arthritis: development of recommendations for clinical practice based on data from the literature and experts opinion. Joint Bone Spine. 2009;76:524–31. doi: 10.1016/j.jbspin.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 7.NICE technology appraisal guidance 104. Etanercept and Infliximab for the Treatment of Adults with Psoriatic Arthritis. London, UK: NICE; 2006. [Google Scholar]
- 8.Mease PJ, Goffe BS, Metz J, et al. Etanercept in the treatment of psoriatic arthritis and psoriasis: a randomised trial. Lancet. 2000;356:385–90. doi: 10.1016/S0140-6736(00)02530-7. [DOI] [PubMed] [Google Scholar]
- 9.Mease PJ, Kivitz AJ, Burch FX, et al. Etanercept treatment of psoriatic arthritis: safety, efficacy, and effect on disease progression. Arthritis Rheum. 2004;50:2264–72. doi: 10.1002/art.20335. [DOI] [PubMed] [Google Scholar]
- 10.Antoni CE, Kavanaugh A, Kirkham B, et al. Sustained benefits of infliximab therapy for dermatologic and articular manifestations of psoriatic arthritis: results from the infliximab multinational psoriatic arthritis controlled trial (IMPACT) Arthritis Rheum. 2005;52:1227–36. doi: 10.1002/art.20967. [DOI] [PubMed] [Google Scholar]
- 11.Mease PJ, Gladman DD, Ritchlin CT, et al. Adalimumab for the treatment of patients with moderately to severely active psoriatic arthritis: results of a double-blind, randomized, placebo-controlled trial. Arthritis Rheum. 2005;52:3279–89. doi: 10.1002/art.21306. [DOI] [PubMed] [Google Scholar]
- 12.Saad AA, Symmons DP, Noyce PR, et al. Risks and benefits of tumor necrosis factor-alpha inhibitors in the management of psoriatic arthritis: systematic review and metaanalysis of randomized controlled trials. J Rheumatol. 2008;35:883–90. [PubMed] [Google Scholar]
- 13.Kaltwasser JP, Nash P, Gladman D, et al. Efficacy and safety of leflunomide in the treatment of psoriatic arthritis and psoriasis: a multinational, double-blind, randomized, placebo-controlled clinical trial. Arthritis Rheum. 2004;50:1939–50. doi: 10.1002/art.20253. [DOI] [PubMed] [Google Scholar]
- 14.Katchamart W, Trudeau J, Phumethum V, et al. Efficacy and toxicity of methotrexate (MTX) monotherapy versus MTX combination therapy with non-biological disease-modifying antirheumatic drugs in rheumatoid arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2009;68:1105–12. doi: 10.1136/ard.2008.099861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salliot C, van der Heijde D. Long-term safety of methotrexate monotherapy in patients with rheumatoid arthritis: a systematic literature research. Ann Rheum Dis. 2009;68:1100–4. doi: 10.1136/ard.2008.093690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bennett RM. Psoriatic arthritis. In: McCarty DJ, editor. Arthritis and Allied Conditions. Philadelphia: Lea and Febiger; 1979. pp. 642–55. [Google Scholar]
- 17.Gladman DD. Psoriatic arthritis: recent advances in pathogenesis and treatment. Rheum Dis Clin North Am. 1992;18:247–56. [PubMed] [Google Scholar]
- 18.Salvarani C, Olivieri I, Cantini F, et al. Psoriatic arthritis. Curr Opin Rheumatol. 1998;10:299–305. doi: 10.1097/00002281-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Clegg DO, Reda DJ, Mejias E, et al. Comparison of sulfasalazine and placebo in the treatment of psoriatic arthritis. Arthritis Rheum. 1996;39:2013–20. doi: 10.1002/art.1780391210. [DOI] [PubMed] [Google Scholar]
- 20.Felson DT, Anderson JJ, Boers M, et al. The American College of Rheumatology preliminary core set of disease activity measures for rheumatoid arthritis clinical trials. Arthritis Rheum. 1993;36:729–40. doi: 10.1002/art.1780360601. [DOI] [PubMed] [Google Scholar]
- 21.Dougados M, Aletaha D, van Riel P. Disease activity measures for rheumatoid arthritis. Clin Exp Rheumatol. 2007;25(5 Suppl. 46):S22–9. [PubMed] [Google Scholar]
- 22.van Reil PLCM, Scott DL. EULAR Handbook of Clinical Assessment in Rheumatoid Arthritis. Leiden, The Netherlands: Van Zuiden Communications; 2000. [Google Scholar]
- 23.Jones SM, Armos JB, Cohen MG, et al. Psoriatic arthritis: outcome of disease subsets and relationship of joint disease to nail and skin disease. Br J Rheum. 1994;33:834–9. doi: 10.1093/rheumatology/33.9.834. [DOI] [PubMed] [Google Scholar]
- 24.Fraser AD, van Kuijk AW, Westhovens R, et al. A randomised, double blind, placebo controlled, multicentre trial of combination therapy with methotrexate plus ciclosporin in patients with active psoriatic arthritis. Ann Rheum Dis. 2005;64:859–64. doi: 10.1136/ard.2004.024463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalbeth N, Yeoman S, Dockerty JL, et al. A randomised placebo controlled trial of delipidated, deglycolipidated Mycobacterium vaccae as immunotherapy for psoriatic arthritis. Ann Rheum Dis. 2004;63:718–22. doi: 10.1136/ard.2003.007104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madland TM, Bjorkkjaer T, Brunborg LA, et al. Subjective improvement in patients with psoriatic arthritis after short-term oral treatment with seal oil. A pilot study with double blind comparison to soy oil. J Rheumatol. 2006;33:307–10. [PubMed] [Google Scholar]
- 27.Machin D, Campbell MJ, Tan SB, et al. Sample Size Tables for Clinical Studies. 3rd edn. Chichester: Wiley-Blackwell; 2009. [Google Scholar]
- 28.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–90. [Google Scholar]
- 29.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd edn. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- 30.Schafer JL. Analysis of Incomplete Multivariate Data. 1st edn. London, UK: Chapman & Hall; 1997. [Google Scholar]
- 31.R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; http://www.project.org (23 January 2012, date last accessed) [Google Scholar]
- 32.Diggle P, Farewell D, Henderson R. Analysis of longitudinal data with drop-out: objectives, assumptions and a proposal. J R Stat Soc C. 2007;56:499–550. [Google Scholar]
- 33.Schmitt J, Zhang Z, Wozel G, et al. Efficacy and tolerability of biologic and nonbiologic systemic treatments for moderate-to-severe psoriasis: meta-analysis of randomized controlled trials. Br J Dermatol. 2008;159:513–26. doi: 10.1111/j.1365-2133.2008.08732.x. [DOI] [PubMed] [Google Scholar]
- 34.Gladman DD, Landewé R, McHugh NJ, et al. Composite measures in psoriatic arthritis: GRAPPA 2008. J Rheumatol. 2010;37:453–61. doi: 10.3899/jrheum.090956. [DOI] [PubMed] [Google Scholar]
- 35.Gladman DD, Tom BD, Mease PJ, et al. Informing response criteria for psoriatic arthritis I: discrimination models based on data from three anti-TNF randomized studies. J Rheumatol. 2010;37:1892–7. doi: 10.3899/jrheum.091172. [DOI] [PubMed] [Google Scholar]
- 36.Gladman DD, Tom BD, Mease PJ, et al. Informing response criteria for psoriatic arthritis II: further considerations and a proposal—the PsA Joint Activity Index (PsAJAI) J Rheumatol. 2010;37:2559–65. doi: 10.3899/jrheum.100479. [DOI] [PubMed] [Google Scholar]
- 37.Schoels M, Aletaha D, Funovits J, et al. Application of the DAREA/DAPSA score for assessment of disease activity in psoriatic arthritis. Ann Rheum Dis. 2010;69:1441–7. doi: 10.1136/ard.2009.122259. [DOI] [PubMed] [Google Scholar]
- 38.Black RL, O'Brien WM, Van Scott EJ, et al. Methotrexate therapy in psoriatic arthritis. Double-blind study on 21 patients. J Am Med Assoc. 1964;189:743–7. [PubMed] [Google Scholar]
- 39.Willkens RF, Williams HJ, Ward JR, et al. Randomized, double-blind, placebo controlled trial of low-dose pulse methotrexate in psoriatic arthritis. Arthritis Rheum. 1984;27:376–81. doi: 10.1002/art.1780270403. [DOI] [PubMed] [Google Scholar]
- 40.Scarpa R, Peluso R, Atteno M, et al. The effectiveness of a traditional therapeutical approach in early psoriatic arthritis: results of a pilot randomised 6-month trial with methotrexate. Clin Rheumatol. 2008;27:823–6. doi: 10.1007/s10067-007-0787-7. [DOI] [PubMed] [Google Scholar]
- 41.Spadaro A, Riccieri V, Sili-Scavalli A, et al. Comparison of cyclosporin A and methotrexate in the treatment of psoriatic arthritis: a one-year prospective study. Clin Exp Rheumatol. 1995;13:589–93. [PubMed] [Google Scholar]
- 42.Fraser AD, van Kuijk AW, Westhovens R, et al. A randomised, double blind, placebo controlled, multicentre trial of combination therapy with methotrexate plus ciclosporin in patients with active psoriatic arthritis. Ann Rheum Dis. 2005;64:859–64. doi: 10.1136/ard.2004.024463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ravindran V, Scott DL, Choy EH. A systematic review and meta-analysis of efficacy and toxicity of disease modifying anti-rheumatic drugs and biological agents for psoriatic arthritis. Ann Rheum Dis. 2008;67:855–9. doi: 10.1136/ard.2007.072652. [DOI] [PubMed] [Google Scholar]
- 44.Ceponis A, Kavanaugh A. Use of methotrexate in patients with psoriatic arthritis. Clin Exp Rheumatol. 2010;28(5 Suppl. 61):S132–7. [PubMed] [Google Scholar]
- 45.Combe B, Goupille P, Kuntz JL, et al. Sulphasalazine in psoriatic arthritis: a randomized, multicentre, placebo-controlled study. Br J Rheumatol. 1996;35:664–8. doi: 10.1093/rheumatology/35.7.664. [DOI] [PubMed] [Google Scholar]
- 46.Farr M, Kitas GD, Waterhouse L, et al. Sulphasalazine in psoriatic arthritis: a double-blind placebo-controlled study. Br J Rheumatol. 1990;29:46–9. doi: 10.1093/rheumatology/29.1.46. [DOI] [PubMed] [Google Scholar]
- 47.Fraser SM, Hopkins R, Hunter JA, et al. Sulphasalazine in the management of psoriatic arthritis. Br J Rheumatol. 1993;32:923–5. doi: 10.1093/rheumatology/32.10.923. [DOI] [PubMed] [Google Scholar]
- 48.Gupta AK, Grober JS, Hamilton TA, et al. Sulfasalazine therapy for psoriatic arthritis: a double blind, placebo controlled trial. J Rheumatol. 1995;22:894–8. [PubMed] [Google Scholar]
- 49.Carette S, Calin A, McCafferty JP, et al. A double-blind placebo-controlled study of auranofin in patients with psoriatic arthritis. Arthritis Rheum. 1989;32:158–65. doi: 10.1002/anr.1780320208. [DOI] [PubMed] [Google Scholar]
- 50.Suarez-Almazor ME, Belseck E, Shea B, et al. Methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2000;(2):CD000957. doi: 10.1002/14651858.CD000957. [DOI] [PubMed] [Google Scholar]
- 51.Lie E, van der Heijde D, Uhlig T, et al. Effectiveness and retention rates of methotrexate in psoriatic arthritis in comparison with methotrexate-treated patients with rheumatoid arthritis. Ann Rheum Dis. 2010;69:671–6. doi: 10.1136/ard.2009.113308. [DOI] [PubMed] [Google Scholar]
- 52.Kingsley GH, Khoshaba B, Smith CM, et al. Are clinical trials in rheumatoid arthritis generalizable to routine practice? A re-evaluation of trial entry criteria. Rheumatology. 2005;44:629–32. doi: 10.1093/rheumatology/keh565. [DOI] [PubMed] [Google Scholar]
- 53.Sleight P. Debate: subgroup analyses in clinical trials: fun to look at - but don't believe them! Curr Control Trials Cardiovasc Med. 2000;1:25–7. doi: 10.1186/cvm-1-1-025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stein CM, Pincus T. Placebo-controlled studies in rheumatoid arthritis: ethical issues. Lancet. 1999;353:400–3. doi: 10.1016/S0140-6736(98)01373-7. [DOI] [PubMed] [Google Scholar]
- 55.Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. Part 1: ethical and scientific issues. Ann Intern Med. 2000;133:455–63. doi: 10.7326/0003-4819-133-6-200009190-00014. [DOI] [PubMed] [Google Scholar]
- 56.Finniss DG, Kaptchuk TJ, Miller F, et al. Biological, clinical, and ethical advances of placebo effects. Lancet. 2010;375:686–95. doi: 10.1016/S0140-6736(09)61706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chandran V, Schentag CT, Gladman DD. Reappraisal of the effectiveness of methotrexate in psoriatic arthritis: results from a longitudinal observational cohort. J Rheumatol. 2008;35:469–71. [PubMed] [Google Scholar]
- 58.Woo P, Southwood TR, Prieur AM, et al. Randomized, placebo-controlled, crossover trial of low-dose oral methotrexate in children with extended oligoarticular or systemic arthritis. Arthritis Rheum. 2000;43:1849–57. doi: 10.1002/1529-0131(200008)43:8<1849::AID-ANR22>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 59.van Dongen H, van Aken J, Lard LR, et al. Efficacy of methotrexate treatment in patients with probable rheumatoid arthritis: a double-blind, randomized, placebo-controlled trial. Arthritis Rheum. 2007;56:1424–32. doi: 10.1002/art.22525. [DOI] [PubMed] [Google Scholar]
- 60.Chen J, Liu C, Lin J. Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev. 2006;4:CD004524. doi: 10.1002/14651858.CD004524.pub3. [DOI] [PubMed] [Google Scholar]
- 61.Ritchlin CT, Kavanaugh A, Gladman DD, et al. Treatment recommendations for psoriatic arthritis. Ann Rheum Dis. 2009;68:1387–94. doi: 10.1136/ard.2008.094946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kristensen LE, Gülfe A, Saxne T, et al. Efficacy and tolerability of anti-tumour necrosis factor therapy in psoriatic arthritis patients: results from the South Swedish Arthritis Treatment Group register. Ann Rheum Dis. 2008;67:364–9. doi: 10.1136/ard.2007.073544. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



