Abstract
Introduction
Obesity is associated with poor prognosis of colon cancer and the mechanism for this is unknown. This study tested insulin-caused resistance to oxaliplatin via activation of PI3K/Akt pathway in HT29 cells.
Methods
The effect of insulin on oxaliplatin cytotoxicity was tested by pre-incubation with 1µM insulin followed by addition of oxaliplatin. Phosphorylated Akt was determined by Western blotting.
Results
Addition of 1µM insulin decreased the cytotoxicity of oxaliplatin. PI3K specific inhibitor Ly294002 abolished such an effect of insulin. pAkt were highly activated by insulin plus oxaliplatin and inhibited by addition of Ly294002.
Conclusion
Insulin decreased drug efficacy of oxaliplatin in HT29 cells, which could be mediated by the activation of the PI3K/Akt pathway.
Keywords: colon cancer, HT29 cell, Insulin, PI3K/Akt pathway, Obesity
Introduction
The incidence of obesity is increasing worldwide and it has affected a large proportion of population. In Western world, one third of the population is obese and two thirds are overweight and obese (1). Epidemiological studies showed that obesity is associated with many cancers including colon cancer (2). Obesity is estimated to be responsible for about 30% of colon cancer incidence (3). Recent studies have also shown that obesity leads to poor prognosis of colon cancer (4)-(6). However, the mechanism for obesity-associated poorer prognosis of colon cancer is not known. As the activation of PI3K/Akt signal pathway increases the resistance of several cancer cell lines such ovarian, lung cancer to chemotherapeutic drugs (7),(8), it is possible that PI3K/Akt may also play a role in the poor prognosis of obesity-associated colon cancer. Many altered factors in obesity are known to activate PI3K/Akt pathway including increased blood levels of insulin, Insulin-like growth factor-1, leptin, IL-6, IL-17, TNF-α and decreased blood level of adiponectin (9),(10). Thus, it is possible that these factors can activate PI3K/Akt pathway which in turn increases the resistance to chemotherapy in obesity-associated colon cancer (11).
Increased insulin in obesity may play a key role in obesity-associated carcinogenesis and prognosis of colon cancer (12). In 1990s, Giovannucci et al proposed that prolonged high blood level of insulin is associated with increased colon cancer incidence (13),(14). Epidemiological studies have shown that the serum level of C-peptide is associated with the increased risk of colon cancer (15)-(17). A recent prospective study further demonstrated that fasting blood level of insulin is positively correlated with waist circumference and colon cancer (18). This hypothesis has been demonstrated in animal models. Administration of insulin increased colon cancer cell proliferation and polyp formation in Azoxymethane (AOM)-induced cancer model (19),(20). High level of plasma insulin has also been demonstrated to significantly increase the formation of aberrant crypt foci in obese rat model with injection of AOM (21).
Insulin can stimulate PI3K/Akt activity to increase the carcinogenesis of colon cancer (9). The activation of PI3K/Akt pathway can increase cell survival, cell growth and proliferation (22)-(24). In addition, insulin can also increase IGF-1 (insulin-growth factor -1) by inhibiting production of IGFBPs 1, 2 and 3 (insulin-like growth factor binding proteins) (25). IGF-1 binds to both insulin and IGF-1 receptors to stimulate PI3K/Akt activity (25). However, the effect of insulin has not been studied in colon cancer prognosis although increased insulin level has been regarded as a major factor for the poor prognosis of obesity-associated breast cancer and reduction of insulin by metformin was found to improve treatment outcome (26),(27). It has also been shown that prediagnosis C-peptide and lower levels of plasma IGFBP1 were associated with increased colon cancer mortality (28). Therefore, insulin may also associate with prognosis of colon cancer through the activation of the PI3K/Akt pathway. Activation of PI3K can cause drug resistance which is a major reason of poor outcome of the treatment. At present, colon cancer is treated by oxaliplatin and 5-Fu. The initial response to the therapeutic regime with 5-FU plus oxaliplatin is 50% (29). Oxaliplatin, a third generation of platinum-containing anti-cancer agent, reduces DNA replication by covalently binding to DNA, forming platinum-DNA adducts (30). A sufficient amount of such DNA damage leads to cell-cycle arrest and apoptosis (31). The mechanisms for drug resistance to oxaliplatin are diverse such as apoptosis, DNA repair, transcription factor and drug detoxification (32),(33). Drug detoxification system affects drug metabolism and transportation and thus affects drug availability (34)-(36). Decreased apoptosis could be caused by the activation of survival signal pathways and inhibition of these pathways can increase sensitivity to oxaliplatin (37).
In this study, we tested if insulin can cause drug resistance of colon cancer cell line HT29 cells to oxaliplatin via activation of PI3K/Akt pathway and if PI3K specific inhibitor Ly294002 can re-sensitize the HT29 cells.
Materials and methods
Materials
Insulin, DMEM medium, antibiotics PNS, protease inhibitor cocktail, protein phosphatase inhibitor, glycerophosphate, phenylmethylsulfonyl fluoride, TBST buffer and fetal calf serum were purchased from Sigma-aldrich (Sydney, Australia). Anti-pAkt antibody (Ser473), goat-anti rabbit antibody and Ly294002 was from Cell Signal Technology (Queensland, Australia). Celltiter one solution cell proliferation assay was from Promega (Sydney, Australia). HT29 cell line was bought from ATCC. Oxaliplatin was from Wollongong Hospital, Wollongong NSW 2500, Australia. Immune-blot PVDF membrane, 4-12% Bis-Tris gel from Biorad (Sydney, Australia). ECL Western detection reagents were from GE healthcare (Sydney, Australia).
Methods
Colon cancer HT 29 cells
HT 29 cells were cultured in DMEM medium at 37°C with 10% fetal calf serum under atmosphere of 95% air and 5% CO2 in a 75-ml flask. After treated with trypsin for 5 min, cells were resuspended in medium to make the concentration at 2 x 105/ml. Then 100 µl of cells were added to each well in 96 well plates for drug cytotoxicity assay.
Treatment of HT29 cells with oxaliplatin, insulin and Ly294002
HT29 cells were incubated with serum free medium overnight before treatment. Insulin was added to the medium 15 min before oxaliplatin treatment. Oxaliplatin was mixed in serum free medium at different concentrations that were used to replace the former medium. Ly294002 was tested at the final concentration of 8µM.
Cell viability assay
Cell viability was determined by Celltiter 96 aqueous one solution cell proliferation assay kit according to the kit manual. 2 × 104 cells/ well were cultured in 96-well plates with DMEM medium with or without added agents. After incubation, 20 µl of MTS was added to each well. Cells were incubated for 45min. They were read in 495nm wavelength with a 96-well plate reader to determine absorbance.
Western blotting
Cells from cultures were lysed in NP40 buffer containing 10µl/ml protease inhibitor cocktail, phosphotase inhibitor, 1mM/phenylmethylsulfonyl fluoride by incubating for 30 min at 4°C. Proteins were separated by electrophorsis in 26 well gels by a Bio-Rad apparatus. The proteins were then transferred into PVDF membrane at 100V for 1 hr. The membranes were blocked at room temperature with 5% bovine serum albumin in TBST buffer. After three times of 5 min wash with TBST, the membranes were incubated overnight with phosphorylated Akt antibody (Ser473) at 1:500 dilution. After three times of 5 min wash with TBST, the membranes were incubated for 2 hrs with horseradish peroxidise conjugated goat anti-rabbit antibody at dilution 1:20000. The membrances were exposed to Fujifilm after incubating with ECL for 1 min. Western blots were A evaluated with densitometric analysis by using Biorad quantity one software.
Statistics
The statistics is done by oneway Anova using SPSS (version 15, Chicago, IL, USA) and student t-test. A p< 0.05 is considered significant.
Results
Oxaliplatin caused dose-and time-dependent cytotoxicity B on HT29 cells
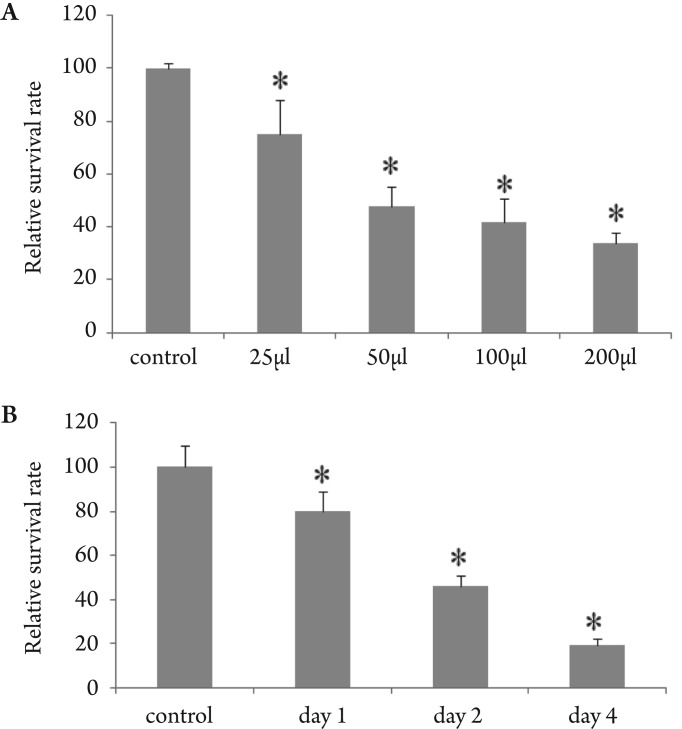
We first tested the effect of oxaliplatin on HT29 cells. As shown in Fig 1A, addition of oxaliplatin caused a dose-dependent cytotoxicity on HT29 cells. 25µg/ml of oxaliplatin reduced cell survival rate to 75% of control. With increased dose of oxaliplatin, the survival rates were further decreased to 48% at dose of 50 µg/ml, 42% at 100 µg/ml and 34% at 200µg/ml. We then choose the dose 50 µg/ml to test whether a time-dependent effect exists. As shown in (Fig 1B), at day 1, it decreased activity to 80% of control and 19% at day 3.
Figure 1. Time- and dose-dependent effect of oxaliplatin on the survival of HT29 cells. Data represent mean ± SD, n=6, * is p < 0.05 compared with control. Panel A is dose-dependent after 48 hrs treatment of different concentration of oxaliplatin. Panel B is time-dependent of 50µg/ml of oxaliplatin.
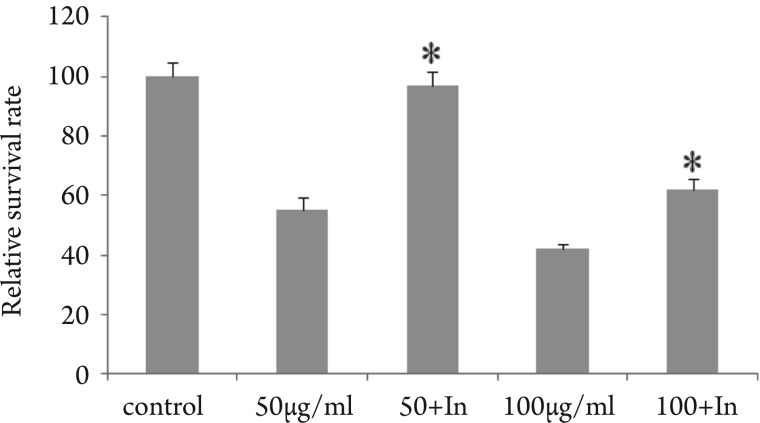
Insulin-induced resistance to oxaliplatin
Then we examined the effect of insulin on the cytotoxicity of oxaliplatin on HT29 cells. Addition of 1 µM insu significantly increased HT29 resistant to oxaliplatin (Fig 2). After addition of insulin, 100µg/ml of oxaliplatin can on reduce cell survival rate to 62% of control compared to 42 when using oxaliplatin alone. 50µg/ml of oxaliplatin can n reduce HT29 cell survival rate with the addition of insulin
Figure 2. Insulin abrogated the killing effect of the oxaliplatin on HT29 cells. Data represent mean ± SD, n=4, * is p<0.05 compared with cells treated with oxaliplatin.
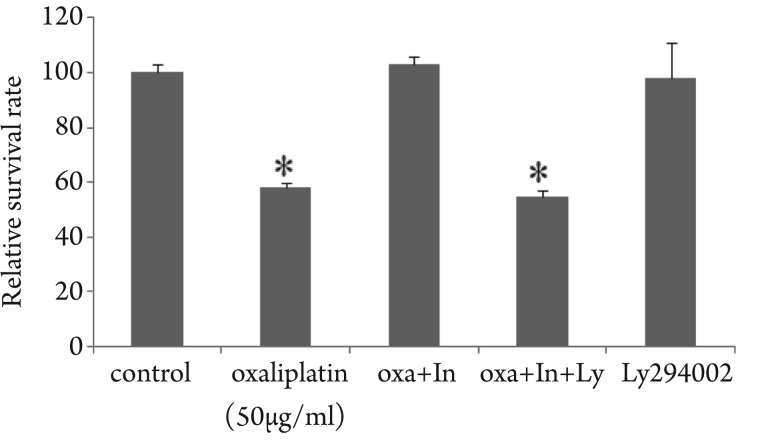
Inhibitory effect of PI3K specific inhibitor Ly294002
Due to the important role of the PI3K/Akt pathway insulin-caused drug resistance, we tested the effect of PI specific inhibitor Ly294002. Addition of 8µM Ly2940 restored HT29 sensitivity to 50µg/ml oxaliplatin in the condition of insulin effect (Fig 3). However, Ly294002 alone did not cause any cell death.
Figure 3. PI3K inhibitor Ly294002 abolished the insulininduced resistance to oxaliplatin in HT29 cells. Data represent mean ± SD, n=4, * is p<0.05 compared with control.
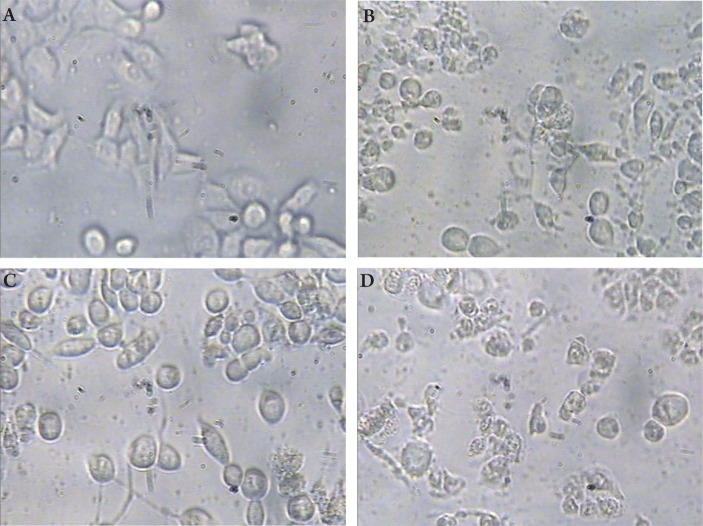
HT29 cell morphological changes
After 48 hrs incubation with 50µg/ml oxaliplatin, the HT29 cell morphological changes were observed under microscopy. As seen in Fig 4B, 50µg/ml oxaliplatin caused HT29 cell shrinkage, rupture of cells into debris compared with control (Fig 4A). This is rescued by addition of 1µM insulin (Fig 4C) and re-sensitized by 8µM Ly294002 (Fig 4D).
Figure 4. HT29 cell morphological changes under treatment of oxaliplatin. Panel A is from control; B treated with 50µg/ml of oxaliplatin; C treated with oxaliplatin and insulin and D treated with oxaliplatin, insulin and Ly294002.
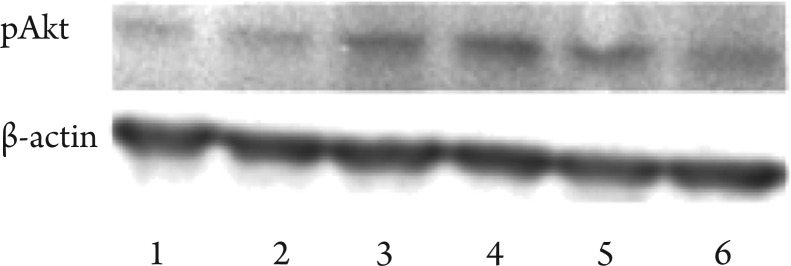
Examination of pAkt levels after addition of insulin, oxaliplatin and Ly294002
To further examine the role of the PI3K/Akt in insulin-induced drug resistance, HT29 cells were plated in 24 well plates. After changed to FBS free medium and incubated overnight, the cells were incubated for 15 min with 50µg/ml oxaliplan, insulin, oxaliplatin plus insulin and oxaliplatin plus insulin plus Ly294002. As shown in Fig 5, insulin alone activated pAkt level in HT29 cells. It also activated pAkt when oxaliplatin was present to 3 folds of control. This activation was inhibited by addition of Ly294002 by 40%. The results indicate an important role of the PI3K/Akt in insulin-induced drug resistance to oxaliplatin in HT29 cells.
Figure 5. pAkt after treatment with insulin, oxaliplatin and ly294002. The levels of pAkt in HT29 cells under different treatments were detected by Western blotting. Lane 1 is control; lane 2: oxaliplatin treatment; lane 3: insulin alone; lane 4: insulin plus oxaliplatin; lane 5: insulin + oxaliplatin + ly294002; lane 6: Ly294002 alone. The figure represents one of three independent experiments.
Discussion
Drug resistance is a major problem for the treatment of colon cancer. Many genes have been found to be associated with oxaliplatin resistance (38),(39). DNA polymerase beta (POLB) gene is shown to cause oxaliplatin resistance and cause poor prognosis in colon cancer (40). Phosphoserine aminotransferase PSAT1 over-expression has been also shown to increase resistance to oxaliplatin (41). In addition, drug accumulation is also related with resistance to oxaliplatin (42). In this study we showed that insulin can cause drug resistance in HT29 cells which is different from gene mutations and may account for the poor prognosis of obesity-associated colon cancer. In addition, this phenomenon also happens in another colon cancer cell line LS174T cells. Our preliminary data showed that insulin increased LS174T cell resistance to cytotoxin cycloheximide. Thus, insulin-induced drug resistance could be universal in colon cancer.
Obesity has been associated with poor outcome of colon cancer treatment. Thus, it is urgent to identify the mechanisms for this. Our study provides the evidence that the increased risk factors in obesity may cause drug resistance to chemotherapy. Among many factors changed in obesity, insulin is of important role. It is known to activate the survival pathway PI3K/Akt pathway to promote carcinogenesis (43). We showed that addition of insulin into colon cancer cell line HT29 increased the cells to resist the chemotherapeutic drug oxaliplatin. The role of the PI3K/Akt pathway in insulin-induced drug resistance is also indicated by Western blotting detection of pAkt levels after various treatments of HT29 cells. Thus, insulin-activated PI3K/Akt pathway at least patially account for the poor prognosis of colon cancer caused by obesity. Other factors may also have similar effect and synergize the effect of insulin making the situation worse.
We have also shown that PI3K specific inhibitor Ly294002 can restore the sensitivity to oxaliplatin at a low concentration which did not cause HT29 cells death. This may indicate that PI3K activated by insulin sensitized the cells to the inhibitor of the pathway. It provides an opportunity for the obesity-associated colon cancer for better treatment by incorporating the inhibitor into the current regime.
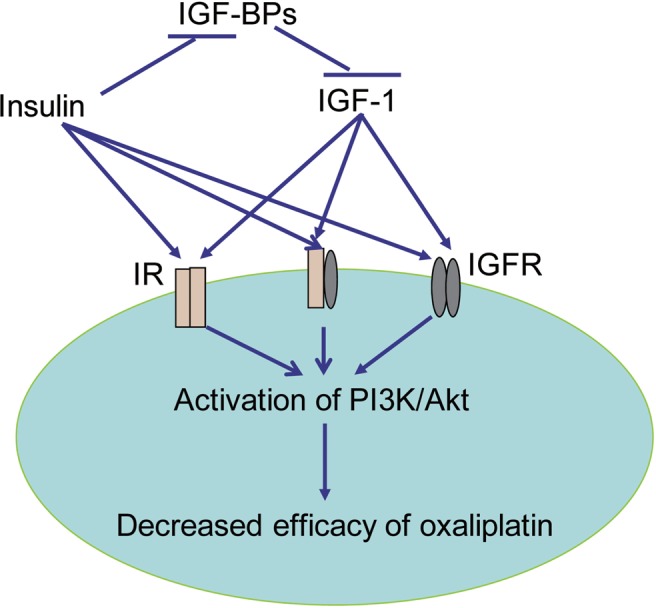
We propose that insulin mediated activation of PI3K/Akt pathway may be direct or indirect (Fig 6). Insulin can bind to IR, IGF and hybrid receptors to activate PI3K/Akt. It also inhibits IGFBPs to increase IGF1. IGFs are involved in insulin action (44). IGF-1 share 40% amino acid sequence homology with insulin and has stronger anti-apoptosis effect than insulin. The increase of IGF-1 is positively related with incidence of colon cancer while IGFBPs are inversely related with the disease (45)-(48).
Figure 6. The effect of insulin in drug-resistance. Insulin and bind directly to insulin receptor (IR), IGF-1 receptor (IGFR) and insulin and IGFR hybridised receptor to activated PI3K/Akt pathway. It can also block IGF binding proteins (IGFBPs) to increase free IGF-1 which also binds to above receptors to activate the PI3K/Akt. Activated PI3K/Akt in turn decreased the cytotoxicity efficacy of oxaliplatin on HT29 cells.
Overall, our study provided evidence to support the hypothesis that risk factors in obesity may cause drug resistance via the activation of the PI3K/Akt pathway in obesity-associated colon cancer. The inhibition of the pathway could have therapeutic effect.
Footnotes
No potential conflict of interest.
References
- 1.Wikipedia [Internet] Florida: Wikimedia Foundation, Inc.; [cited 2010 Oct 15]. Available from: http://en.wikipedia.org/wiki/Obesity. [Google Scholar]
- 2.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–91. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 3.Larsson SC, Wolk A. Obesity and colon and rectal cancer risk: a metaanalysis of prospective studies. Am J Clin Nutr. 2007;86:556–65. doi: 10.1093/ajcn/86.3.556. [DOI] [PubMed] [Google Scholar]
- 4.Sinicrope FA, Foster NR, Sargent DJ, O'Connell MJ, Rankin C. Obesity is an independent prognostic variable in colon cancer survivors. Clin Cancer Res. 2010;16:1884–93. doi: 10.1158/1078-0432.CCR-09-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healy LA, Ryan AM, Sutton E, Younger K, Mehigan B, Stephens R, et al. Impact of obesity on surgical and oncological outcomes in the management of colorectal cancer. Int J Colorectal Dis. 2010;25:1293–9. doi: 10.1007/s00384-010-0963-0. [DOI] [PubMed] [Google Scholar]
- 6.Parr CL, Batty GD, Lam TH, Barzi F, Fang X, Ho SC, et al. Body-mass index and cancer mortality in the Asia-Pacific Cohort Studies Collaboration: pooled analyses of 424,519 participants. Lancet Oncol. 2010;11:741–52. doi: 10.1016/S1470-2045(10)70141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Page C, Lin HJ, Jin Y, Castle VP, Nunez G, Huang M, et al. Overexpression of Akt/AKT can modulate chemotherapy-induced apoptosis. Anticancer Res. 2000;20:407–16. [PubMed] [Google Scholar]
- 8.Brognard J, Clark AS, Ni Y, Dennis PA. Akt/protein kinase B is constitutively active in non-small cell lung cancer cells and promotes cellular survival and resistance to chemotherapy and radiation. Cancer Res. 2001;61:3986–97. [PubMed] [Google Scholar]
- 9.Huang XF, Chen J. Obesity, the PI3K/Akt signal pathway and colon cancer. Obes Rev. 2009;10:610–6. doi: 10.1111/j.1467-789X.2009.00607.x. [DOI] [PubMed] [Google Scholar]
- 10.Gislette T, Chen J. The possible role of IL-17 in obesity-associated cancer. ScientificWorldJournal. 2010;10:2265–71. doi: 10.1100/tsw.2010.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J. The Src/PI3K/Akt signal pathway may play a key role in decreased drug efficacy in obesity-associated cancer. J Cell Biochem. 2010;110:279–80. doi: 10.1002/jcb.22572. [DOI] [PubMed] [Google Scholar]
- 12.Rose DP, Komninou D, Stephenson GD. Obesity, adipocytokines, and insulin resistance in breast cancer. Obes Rev. 2004;5:153–65. doi: 10.1111/j.1467-789X.2004.00142.x. [DOI] [PubMed] [Google Scholar]
- 13.Giovannucci E. Insulin and colon cancer. Cancer Causes Control. 1995;6:164–79. doi: 10.1007/BF00052777. [DOI] [PubMed] [Google Scholar]
- 14.McKeown-Eyssen G. Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol Biomarkers Prev. 1994;3:687–95. [PubMed] [Google Scholar]
- 15.Kaaks R, Toniolo P, Akhmedkhanov A, Lukanova A, Biessy C, Dechaud H, et al. Serum C-peptide, insulin-like growth factor (IGF)-I, IGF-binding proteins, and colorectal cancer risk in women. J Natl Cancer Inst. 2000;92:1592–600. doi: 10.1093/jnci/92.19.1592. [DOI] [PubMed] [Google Scholar]
- 16.Ma J, Giovannucci E, Pollak M, Leavitt A, Tao Y, Gaziano JM, et al. A prospective study of plasma C-peptide and colorectal cancer risk in men. J Natl Cancer Inst. 2004;96:546–53. doi: 10.1093/jnci/djh082. [DOI] [PubMed] [Google Scholar]
- 17.Wei EK, Ma J, Pollak MN, Rifai N, Fuchs CS, Hankinson SE, et al. A prospective study of C-peptide, insulin-like growth factor-I, insulin-like growth factor binding protein-1, and the risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev. 2005;14:850–5. doi: 10.1158/1055-9965.EPI-04-0661. [DOI] [PubMed] [Google Scholar]
- 18.Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, et al. Insulin, insulin-like growth factor-I, endogenous estradiol, and risk of colorectal cancer in postmenopausal women. Cancer Res. 2008;68:329–37. doi: 10.1158/0008-5472.CAN-07-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran TT, Medline A, Bruce WR. Insulin promotion of colon tumors in rats. Cancer Epidemiol Biomarkers Prev. 1996;5:1013–5. [PubMed] [Google Scholar]
- 20.Tran TT, Naigamwalla D, Oprescu AI, Lam L, McKeown-Eyssen G, Bruce WR, et al. Hyperinsulinemia, but not other factors associated with insulin resistance, acutely enhances colorectal epithelial proliferation in vivo. Endocrinology. 2006;147:1830–7. doi: 10.1210/en.2005-1012. [DOI] [PubMed] [Google Scholar]
- 21.Lasko CM, Bird RP. Modulation of aberrant crypt foci by dietary fat and caloric restriction: the effects of delayed intervention. Cancer Epidemiol Biomarkers Prev. 1995;4:49–55. [PubMed] [Google Scholar]
- 22.Chen J. Is Src the key to understanding metastasis and developing new treatments for colon cancer? Nat Clin Pract Gastroenterol Hepatol. 2008;5:306–7. doi: 10.1038/ncpgasthep1141. [DOI] [PubMed] [Google Scholar]
- 23.Ozes ON, Mayo LD, Gustin JA, Pfeffer SR, Pfeffer LM, Donner DB. NFkappaB activation by tumour necrosis factor requires the Akt serine-threonine kinase. Nature. 1999;401:82–5. doi: 10.1038/43466. [DOI] [PubMed] [Google Scholar]
- 24.Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–84. doi: 10.1016/j.cell.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 25.Keku TO, Lund PK, Galanko J, Simmons JG, Woosley JT, Sandler RS. Insulin resistance, apoptosis, and colorectal adenoma risk. Cancer Epidemiol Biomarkers Prev. 2005;14:2076–81. doi: 10.1158/1055-9965.EPI-05-0239. [DOI] [PubMed] [Google Scholar]
- 26.Goodwin PJ, Pritchard KI, Ennis M, Clemons M, Graham M, Fantus IG. Insulin-lowering effects of metformin in women with early breast cancer. Clin Breast Cancer. 2008;8:501–5. doi: 10.3816/CBC.2008.n.060. [DOI] [PubMed] [Google Scholar]
- 27.Goodwin PJ, Ligibel JA, Stambolic V. Metformin in breast cancer: time for action. J Clin Oncol. 2009;27:3271–3. doi: 10.1200/JCO.2009.22.1630. [DOI] [PubMed] [Google Scholar]
- 28.Wolpin BM, Meyerhardt JA, Chan AT, Ng K, Chan JA, Wu K, et al. Insulin, the insulin-like growth factor axis, and mortality in patients with nonmetastatic colorectal cancer. J Clin Oncol. 2009;27:176–85. doi: 10.1200/JCO.2008.17.9945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adlard JW, Richman SD, Seymour MT, Quirke P. Prediction of the response of colorectal cancer to systemic therapy. Lancet Oncol. 2002;3:75–82. doi: 10.1016/s1470-2045(02)00648-4. [DOI] [PubMed] [Google Scholar]
- 30.Saif MW, Choma A, Salamone SJ, Chu E. Pharmacokinetically guided dose adjustment of 5-fluorouracil: a rational approach to improving therapeutic outcomes. J Natl Cancer Inst. 2009;101:1543–52. doi: 10.1093/jnci/djp328. [DOI] [PubMed] [Google Scholar]
- 31.Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer. 2007;7:573–84. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- 32.Wakasugi T, Izumi H, Uchiumi T, Suzuki H, Arao T, Nishio K, et al. ZNF143 interacts with p73 and is involved in cisplatin resistance through the transcriptional regulation of DNA repair genes. Oncogene. 2007;26:5194–203. doi: 10.1038/sj.onc.1210326. [DOI] [PubMed] [Google Scholar]
- 33.Torigoe T, Izumi H, Ishiguchi H, Yoshida Y, Tanabe M, Yoshida T, et al. Cisplatin resistance and transcription factors. Curr Med Chem Anticancer Agents. 2005;5:15–27. doi: 10.2174/1568011053352587. [DOI] [PubMed] [Google Scholar]
- 34.Chen J, Raymond K. Nuclear receptors, bile-acid detoxification, and cholestasis. Lancet. 2006;367:454–6. doi: 10.1016/S0140-6736(06)68156-7. [DOI] [PubMed] [Google Scholar]
- 35.Ekblad L, Kjellstrom J, Johnsson A. Reduced drug accumulation is more important in acquired resistance against oxaliplatin than against cisplatin in isogenic colon cancer cells. Anticancer Drugs. 2010;21:523–31. doi: 10.1097/CAD.0b013e328337b867. [DOI] [PubMed] [Google Scholar]
- 36.Lee W, Belkhiri A, Lockhart AC, Merchant N, Glaeser H, Harris EI, et al. Overexpression of OATP1B3 confers apoptotic resistance in colon cancer. Cancer Res. 2008;68:10315–23. doi: 10.1158/0008-5472.CAN-08-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kopetz S, Lesslie DP, Dallas NA, Park SI, Johnson M, Parikh NU, et al. Synergistic activity of the SRC family kinase inhibitor dasatinib and oxaliplatin in colon carcinoma cells is mediated by oxidative stress. Cancer Res. 2009;69:3842–9. doi: 10.1158/0008-5472.CAN-08-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boyer J, Allen WL, McLean EG, Wilson PM, McCulla A, Moore S, et al. Pharmacogenomic identification of novel determinants of response to chemotherapy in colon cancer. Cancer Res. 2006;66:2765–77. doi: 10.1158/0008-5472.CAN-05-2693. [DOI] [PubMed] [Google Scholar]
- 39.Plasencia C, Martinez-Balibrea E, Martinez-Cardus A, Quinn DI, Abad A, Neamati N. Expression analysis of genes involved in oxaliplatin response and development of oxaliplatin-resistant HT29 colon cancer cells. Int J Oncol. 2006;29:225–35. doi: 10.3892/ijo.29.1.225. [DOI] [PubMed] [Google Scholar]
- 40.Iwatsuki M, Mimori K, Yokobori T, Tanaka F, Tahara K, Inoue H, et al. A platinum agent resistance gene, POLB, is a prognostic indicator in colorectal cancer. J Surg Oncol. 2009;100:261–6. doi: 10.1002/jso.21275. [DOI] [PubMed] [Google Scholar]
- 41.Vie N, Copois V, Bascoul-Mollevi C, Denis V, Bec N, Robert B, et al. Overexpression of phosphoserine aminotransferase PSAT1 stimulates cell growth and increases chemoresistance of colon cancer cells. Mol Cancer. 2008;7:14. doi: 10.1186/1476-4598-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hector S, Bolanowska-Higdon W, Zdanowicz J, Hitt S, Pendyala L. In vitro studies on the mechanisms of oxaliplatin resistance. Cancer Chemother Pharmacol. 2001;48:398–406. doi: 10.1007/s002800100363. [DOI] [PubMed] [Google Scholar]
- 43.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–28. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 44.Douglas JB, Silverman DT, Pollak MN, Tao Y, Soliman AS, Stolzenberg-Solomon RZ. Serum IGF-I, IGF-II, IGFBP-3, and IGF-I/IGFBP-3 molar ratio and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiol Biomarkers Prev. 2010;19:2298–306. doi: 10.1158/1055-9965.EPI-10-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wei EK, Ma J, Pollak MN, Rifai N, Fuchs CS, Hankinson SE, et al. A prospective study of C-peptide, insulin-like growth factor-I, insulinlike growth factor binding protein-1, and the risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev. 2005;14:850–5. doi: 10.1158/1055-9965.EPI-04-0661. [DOI] [PubMed] [Google Scholar]
- 46.Palmqvist R, Hallmans G, Rinaldi S, Biessy C, Stenling R, Riboli E, et al. Plasma insulin-like growth factor 1, insulin-like growth factor binding protein 3, and risk of colorectal cancer: a prospective study in northern Sweden. Gut. 2002;50:642–6. doi: 10.1136/gut.50.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ma J, Giovannucci E, Pol lak M, Stampfer M. RESPONSE: Re: Prospective Study of Colorectal Cancer Risk in Men and Plasma Levels of Insulin-Like Growth Factor (IGF)-I and IGF-Binding Protein-3. J Natl Cancer Inst. 1999;91:2052. doi: 10.1093/jnci/91.23.2052. [DOI] [PubMed] [Google Scholar]
- 48.Giovannucci E, Pollak MN, Platz EA, Willett WC, Stampfer MJ, Majeed N, et al. A prospective study of plasma insulin-like growth factor-1 and binding protein-3 and risk of colorectal neoplasia in women. Cancer Epidemiol Biomarkers Prev. 2000;9:345–9. [PubMed] [Google Scholar]