Abstract
Systemic therapy for advanced pancreatic cancer has been largely disappointing owing to the unfavorable pharmacokinetic profile and poor penetration of current chemotherapeutic agents ,as well as the fragile patient population with compromised tolerance to toxic chemotherapies. Nanovectors can provide passive drug delivery through abnormal tumor neo-vasculature microanatomy or active targeting via binding to receptors or macromolecules associated with the tumor. In such a manner, nanovector-based therapy may not only modulate the pharmacokinetics and therapeutic index of chemotherapeutic agents but also provide new treatment options in patients with advanced pancreatic cancer. In this article, we present the rationale and currently available clinical results of nanovector-based therapies to highlight the potential use of this class of agent in patients with advanced pancreatic cancer.
Keywords: nanovector, pancreatic cancer, liposome, PEP02, nab-paclitaxel, EndoTAG-1, nanoplatin, platinum, CPT-11
Introduction
Pancreatic cancer is one of the most detrimental malignancies and the fourth most common cause of cancer-related death in the United Stated. There were 43,140 newly diagnosed cases and 36,800 deaths in 2010 (1). Early detection is uncommon with no more than 15–20% of the patients being amenable for curative intent surgery at the time of diagnosis. Gemcitabine either alone or in combination with erlotinib are the only approved treatments for patients with advanced pancreatic cancer, of whom the overall survival time is generally around 6 months (2)-(5). Recently, Conroy et al showed that a gemcitabine-free triplet chemotherapy, FOLFIRINOX regimen consisting of oxaliplatin, irinotecan and infusional 5-FU/leucovorin, could achieve significantly better tumor response rate, progression-free survival and overall survival than gemcitabine monotherapy in patients with metastatic pancreatic cancer in a randomization phase III trial (6),(7). However, the application of either doublet of triplet combination chemotherapy in patients with advanced pancreatic cancer is often hindered by their toxicity and the performance status of the patients.
New treatment strategies are mandatory to improve the therapeutic outcomes of patients with advanced pancreatic cancer. Recently, two major potential new approaches are emerging that may have the chance to change our practice in treating advanced pancreatic cancer. The first one is molecular targeted agent targeting on dysregulated signaling pathway and the second is the use of nanovector drug delivery system to provide “passive” or “active” targeting drug delivery thus to modulate the pharmacokinetics and therapeutic index of chemotherapeutic agents in pancreatic cancer (8).
This review will focus on the selective nanovector treatments in pancreatic cancer, especially those with available clinical data, including albumin-bound nanoparticles, liposome-encapsulation nanoparticle, cationic liposomal nanoparticle, polymeric micellar agents, and a non-replicating, retroviral vector delivered gene therapy construct.
Albumin-bound Nanoparticle Paclitaxel (Nab-paclitaxel)
Albumin is a particular vehicle for drug delivery in oncology because it is a natural carrier of hydrophobic molecules with reversible, noncovalent binding characteristics and able to enhance the delivery of drug into the extravascular space through a process of receptor-mediated endothelial transcytosis. Such process is initiated by the binding of albumin to an endothelium surface, 60-kDa glycoprotein (gp60) receptor (albondin), which will then bind with an intracellular protein (caveolin-1) to result in the invagination of the endothelium membrane to form transcytotic vesicles, the caveolae (9). The caveolae will subsequently move across the cytoplasm and release the albumin and its conjugated compound into the extracellular space (the peritumoral microenvironment) where the albumin will bind to SPARC (secreted protein acid and rich in cysteine), an extracellular matrix albumin-binding glycoprotein that is structurally and functionally closely related to gp60, and overexpressed in a variety of cancers, including breast cancer, gastric cancer and pancreatic cancer.
Nab-paclitaxel (Abraxane®) is a cremophor (CrEL)-free, albumin-bound, nanoparticle formulation of paclitaxel. Its CrEL-free formulation permits nab-paclitaxel to be administered within a shorter infusion period of time (30 minutes) and without the requirement of routine pre-medications for preventing the hypersensitivity reactions in association with the administration of cremophor solvent-based paclitaxel (10). In preclinical study, the transport of radiolabeled paclitaxel across the endothelial cell monolayer in vitro, and intratumor paclitaxel accumulation after equal doses of paclitaxel in vivo were both significantly enhanced by 4.2-folds (P < 0.0001) and 33% (P < 0.0001), respectively, for nab-paclitaxel as compared with CrEL-paclitaxel with an increase 4.2 folds. In addition, endothelial transcytosis was completely inhibited by inhibitor of gp60/caveolar transport, methyl ß-cyclodextrin (11). These observations supported that gp60-mediated transcytosis and SPARC-aided sequestration may be an important biological pathway to target tumor cells by novel albumin-bound therapeutics.
In a phase I trial, the maximum tolerated dose (MTD) of intravenous injection nab-paclitaxel monotherapy, every 3 weeks in 19 patients with standard therapy-failure solid tumors was 300 mg/m2. No acute hypersensitivity reactions were observed. The most frequent toxicities were myelo-suppression, sensory neuropathy, nausea/vomiting, arthralgia and alopecia (12). The drug has subsequently approved for the treatment of metastatic breast cancer after failure of combination chemotherapy or relapse within 6 months of adjuvant chemotherapy. The commonly used dose/schedule was 260 mg/m2, 30-min intravenous injection, every 3 weeks.
Because SPARC is frequently overexpressed and associated with poor clinical outcomes in pancreatic cancer, Von Hoff et al conducted a phase I/II study to evaluate the MTD of weekly nab-paclitaxel (100 – 150 mg/m2/week) in combination with gemcitabine (1000 mg/m2/week), and the therapeutic efficacies of the regimen. Both agents were given on day 1, 8, and 15 every 28 days ((13)). A total of 67 patients were treated. Despite MTD of nab-paclitaxel was determined as 125 mg/m2/week, dose reduction was required in 30% (6/20), 18% (8/44) and 33% (1/3) of patients receiving 100 mg/m2, 125 mg/m2 and 150 mg/m2, respectively. The most common grade 3-4 toxicity at the MTD dose were fatigue 23%, neutropenia 59% (grade 4 in 23%), thrombocytopenia 20% (grade 4 in 9%) and sensory neuropathy in 9%. Of the 58 patients whose CT image were revaluated with RECIST criteria by independent reviewer, the best tumor response was partial response in 40% and stable disease in 37%, with an overall disease control rate of 78%. The median progression-free and overall survival of the intent-to-treat (N=67) patients were 6.9 months and 10.3 months, respectively; while the survival parameters for the 44 patients receiving MTD dose were 7.9 months and not yet reached, respectively. Of 54 patients with available CA19.9 level, 42 (77.8%) patients had a more than 50% reduction of CA19.9 level after the treatment (14). The therapeutic efficacy of nab-paclitaxel in combination with vandetanib, a potent inhibitor of VEGF2, RET and EGFR, has also been evaluated in a phase I trial with expansion cohort of patients with pancreatic cancer (15). The MTD of vandetanib in combination with two different schedule of nab-paclitaxel, either 100 mg/m2 weekly or 260 mg/m2 every 3 weeks, was 300 mg daily. Of the 29 enrolled gemcitabine-refractory pancreatic cancer patients, the best tumor was partial response in 6 (20.7%) and stable disease in 10 (34.5%), and the median progression-free survival and overall survival were 5.3 (95% CI: 3.7 to 7.3) months and 8.2 (95% CI: 6.2 to 11.5) months, respectively. No statistical significant correlation between SNP (rs1059829 and rs3210714) of SPARC and clinical outcomes was observed.
Liposome-based Drugs
A liposome is often a spherical vesicle with a bilayer membrane whose size typically ranges from ∼40 nanometers to several microns. Because the micro- or nanoparticles can form spontaneously and are generally easier to prepare compared to viral-mediated systems, this nontoxic phospholipid-based drug carrier has become a favorable drug delivery system for various purposes since the 1970s. However, so-called conventional liposomes are easily bound with insoluble circulating plasma protein, i.e. opsonins and lipoproteins, and the complex will be subsequently eliminated from the circulation by reticuloendothelial cells system. Stealth liposome technology, with incorporationof high molecular weight polymers (i.e., polyethylene-glycol (PEG)) to the liposome surface, can effectively protect the liposome from circulating protein binding and subsequently phagocytosis by RER system, and thus improving its plasma clearance, prolonging the circulation time, and enhancing drug delivery efficacy.
Besides its characteristic slow-release pharmacokinetic property, liposome encapsulated drugs can potentially provide improved tumor localization via the “enhanced permeability and retention” (EPR) effect. Such agents can therefore, (i) lower drug elimination to increase systemic circulation time, (ii) lower maximum plasma concentration (Cmax) to reduce drug side effects, (iii) enhance tumor tissue uptake and exposure to the anti-cancer drug; these principles can in turn yield an improved therapeutic index for cancer therapy.
Several liposomal formulated cancer drugs have been evaluated in various cancers, but only a limited number have been applied to pancreatic cancer.
Liposomal Doxorubicin
The first liposomal anti-cancer drug approved by the Food and Drug Administration (FDA) was pegylated liposomal doxorubicin (Caelyx®/Doxil®) in 1995 for Karposi's sarcoma (16)-(18). It has been subsequently approved for the treatment of multiple myeloma and recurrent epithelial ovarian cancer as well. It also has been evaluated for the treatment of pancreatic cancer in animal xenograft model and in clinical trials. In a preclinical study, Vagge et al showed that pegylated liposomal doxorubicin was significantly more effective in inhibiting the growth of human pancreatic cancer xenograft in nude mice as compared to free form doxorubicin (19). Using confocal laser scanning microscopy and microfluorimetry to quantitate the uptake of intravenously injected doxorubicin in tumor tissue, the authors found that the content of doxorubicin in tumor site of animal receiving liposomal formulated drug was 6 folds or higher compared to free doxorubicin. Based on the results, Halford et al conducted a phase II trial to evaluate the therapeutic efficacy of Caelyx® in 22 chemo-naïve patients with unresectable pancreatic carcinoma. The dose was escalated from 30 mg/m2 (in the first two patients) to 50 mg/m(2) intravenous injection every 3 weeks (20). Of the 20 patients received the treatment, the most common grade 3 toxicity were stomatitis (20%) and nausea (10%), the best tumor response was stable diseases in 6 (30%), and the median overall survival was 3.2 months with one year survival rate of 10%. These finding excluded the use of Caelyx® monotherapy in the treatment of advanced pancreatic cancer.
The combination of Caelyx® with infusional 5-FU/leucovorin and mitomycin-C has been evaluated in a phase I trial in patients with upper gastrointestinal cancer. In that study, escalating dose of Caelyx® (15 – 35 mg/m2) day 1 and 29 in combination with weekly 24-hour infusion of 5-FU and leucovorin (2,000 and 500 mg/m2, respectively) for 6 weeks, and mitomycin-C 7 mg/m2 day 8 and 36, every 8 weeks as one cycle. The most common grade 3-4 toxicities were nausea/vomiting (29%), diarrhea (18%) and leucopenia (12%). Of the 14 accruals with pre-treated pancreatic cancer, the best tumor response was partial response in one and minor response in 2, and the overall survival after the study treatment was 6.5 months (21).
Liposomal Platinum
Platinum is one of the most active and wildly used anti-cancer agents in the world, including in combination with gemcitabine to treat non-small cell lung cancer and pancreatic cancer. Although each single trial had failed to demonstrate the superiority of gemcitabine/platinum combination over gemcitabine single agent in the prolongation of the survival in patients with advanced pancreatic cancer, however, the survival benefit of gemcitabine/platinum doublets was demonstrated in a pooled, meta-analysis survival with a hazard ratio of 0.81, p = 0.031 (22).
It is also well known that the use of cisplatin is frequently limited by its nephrotoxicity, peripheral sensory neuropathy, ototoxicity and the aggravation of hematological toxicity while in combination with other cytotoxic agents. Therefore, several liposomal formulations of cisplatin have been developed aiming to reduce its toxicity profile and hopefully to enhance it activity. Based on previous experience of gemcitabine/cisplatin combination and the result of meta-analysis, several liposomal formulated cisplatin have been evaluated in patients with pancreatic cancer.
Lipoplatin is one of the pegylated liposome cisplatin, whose nanoparticulate liposomes are reverse-miscelles, composed of dipalmitoyl phosphatidyl glycerol (DPPG), soy phosphatidyl choline (SPC-3), cholesterol and methoxy- polyethylene glycol-distearoyl phosphatidylethanolamine (mPEG2000-DSPE). Lipoplatin exhibits the fundamental pharmacologic characteristics of pegylated liposomal agents, for example, protecting from the engulfment of reticuloendotheralial system to prolong circulating time, and extravasating from the fenestrate between endothelial cells of tumor vasculature to preferentially localize in per-tumor interstitial tissue and uptake by tumor cells. The anionic, fusogenic nature of the DPPG lipids enables lipoplatin to cross cell membranes more easily than native cisplatin. In addition, with intraperitoneal injection of a “sheath” liposomes wrapped reporter β-galactosidase gene, which had same structure like lipoplatin, into human tumor bearing nude mice, Boulikas et al were able to demonstrate the preferential expression of the reporter gene in the tumor and the tumor neo-vasculature. The findings indicate the potential antiangiogenic activity of the lipoplatin (23).
In phase I trial of lipoplatin monotherapy, the drug was diluted in 5% glucose water and administered as 8 hour intravenous infusion every 14 days. The dose was escalated from 25 mg/m2 to 125 mg/m2. Even at the targeted dose of 125 mg/m2, only grade 1-2 gastrointestinal and hematological toxicities were observed, but neither nephrotoxicity nor neuropathy. Higher doses, 200, 250 and 300 mg/m2, were also tested in one each patient, respectively. The half-life of lipoplatin was estimated ranging from 60 – 117 hours. Of the 27 accruals (19 with pretreated, advanced pancreatic cancer) in this phase I trial, the objective tumor response rate and disease control rate were 11.1% and 63.0%, respectively. Based on the exciting results, the drug has been further tested in combination with gemcitabine in non-small cell lung cancer and pancreatic cancer patient cohorts (24).
In a phase I/II study, Stathopoulos GP et al evaluated the maximum tolerated dose of lipoplatin in combination with gemcitabine in patients with previously treated advanced pancreatic cancer (25). Lipoplatin was given as an 8-hour infusion followed by 60 minutes infusion of 1,000 mg/m2 of gemcitabine at day 1 and 15 every 28 days. The dose of lipoplatin was stepwise escalated from 25 mg/m2 to 125 mg/m2. Of the 24 enrolled patients, two of four patients at 125 mg/m2 experienced grade 3-4 neutropenia. Therefore, the MTD of lipoplatin in this combination was determined to be 100 mg/m2. In this dose escalating study, there were two (8.3%) partial responders and 14 (58.3%) disease stabilizers, and the median overall survival was 4 month. Further randomized phase II/III trial against gemcitabine monotherapy is under evaluation.
Liposome-entrapped cis-bisneodecanoato-trans-R,R-1,2-diaminocyclohexane (DACH) platinum(II) (L-NDDP, Aroplatin™) is a lipophilic cisplatin analog that has been formulated in relatively large-size multi-lamellar liposomes measuring from 1 to 3 µm in diameter. L-NDDP has been demonstrated to be non–cross-resistant with cisplatin in cisplatin-resistant Lovo DDP 3.0 (human colon cancer cells) and L1210/PPD (human leukemia cells) both in vitro and in vivo models. In a phase I study, L-NDDP was given intravenously once every 4 weeks, ranging from 7.5 mg/m2 to 390 mg/m2 (26). The infusion rate was set at 4 mg NDDP per minute for all cases. In this particular study, intra-patient dose escalation was allowed. Grade 1-2 nausea/vomiting, diarrhea and fever were frequently observed in patients receiving 100 mg/m2 or higher dose of L-NDDP. Six out of the 10 patients who had 390 mg/m2 experienced grade 4 hematological toxicities manifesting as thrombocytopenia, granulocytopenia or both. The MTD of intravenous L-NDDP every 4 weeks was determined as 300 mg/m2. In 2004, Aronex Pharmaceuticals had registered a phase I/II study of L-NDDP and gemcitabine combination in patients with advanced pancreatic cancer resistant to standard therapy in a public clinical trial registration website, the clinicaltrials.gov, with an indentifier of NCT00081549. Unfortunately, the latest trial information was updated in June 2005, and no further publication on this trial can be found.
Liposomal Irinotecan (Nanoliposomal CPT-11, PEP02, MM-398)
Irinotecan hydrochloride (CPT-11) is a water-soluble semi-synthetic derivative of camptothecin targeting topoisomerase I, and has been an approved agent for the treatment of metastatic colorectal cancer worldwide, and also for gastric cancer (Japan and Korea), non-small cell lung cancer, small cell lung cancer, cervical cancer, and non-Hodgkin's lymphoma in Japan. In pancreatic cancer, earlier trial showed that combination of gemcitabine and CPT-11 did not provide any survival benefit over gemcitabine monotherapy in patients with advanced pancreatic cancer, and thus CPT-11 has not been considered to be a clinically useful drug in this disease. However, in the recent PRODIGE 4/ACCORD 11 trial, Conroy et al demonstrated that a gemcitabine-free, CPT-11-containing regimen, FOLFIRINOX (CPT-11, oxaliplatin plus intermittent infusion of 5-FU/leucovorin), provided significantly better objective tumor response rate, progression-free survival and overall survival versus gemcitabine monotherapy in patients with metastatic pancreatic cancer. Notable and not unexpectedly, this triplet regimen is associated with significant hematologic toxicity including higher rates of grade-3/4 febrile neutropenia. The results of the PRODIGE/ACCORD 11 trial have revived interest in CPT-11-based therapy in advanced pancreatic cancer (6),(7).
Although the original CPT-11 drug is now of interest in pancreatic cancer management, potentially superior versions incorporating drug delivery technologies offer a next generation approach. CPT-11 exhibits well-known pharmacologic liabilities and significant associated toxicities, which in turn make it an obvious candidate for drug delivery strategies The camptothecins exist in a pH-dependent equilibrium between an inactive carboxylate form (predominant at neutral-to-basic pH) and an active lactone form (predominant under acidic conditions); hence, intravenous injection of free CPT-11 results in rapid inactivation as well as clearance. Furthermore, CPT-11 is largely a prodrug which is converted into the much more potent metabolite SN-38. Hepatic activation and hepatobiliary excretion of SN-38 result in substantial risk of GI injury, especially in individuals having impaired SN-38 glucuronidation. These metabolic conversions contribute to notable heterogeneities in both efficacy and toxicity, and ultimately to a rather narrow therapeutic index. The concept of nanoparticle delivery of CPT-11 is thus very attractive based on potential advantages including: overcoming solubility limitations of the camptothecins; protecting drug in the active lactone configuration; chaperoning drug away from sites of toxicity such as the GI tract; prolonging circulation time and increasing tumor accumulation via the enhanced permeability and retention (EPR) effect; and providing sustained release and prolonged tumor exposure.
To realize the potential advantages of nanoparticle delivery, a novel liposome-based construct termed “nanoliposomal CPT-11 (nLs-CPT-11)” was developed, which encapsulates CPT-11 with unprecedented efficiency and stability (27). PK studies showed long circulation times for the carrier and undetectable drug release in plasma. Furthermore, nanoliposomal CPT-11 provides protection of drug in its active lactone form within the liposome aqueous interior, preventing its hydrolysis as well as premature conversion to the potent and toxigenic metabolite, SN-38. This contrasts markedly with free CPT-11, which is rapidly cleared from circulation, is subject to immediate hydrolysis of the lactone ring, and is also converted to SN-38 contributing to its dose-limiting GI toxicity.
In a series of preclinical studies, nanoliposomal CPT-11 demonstrated significantly superior efficacy when compared to free CPT-11 at the same or higher dose, including frequent cures in some models. The superiority of nanoliposomal CPT-11 over free CPT-11 has been observed in different tumor models including colorectal, gastric, breast, cervical, glioma, pancreatic and lung cancer models. In addition to superior efficacy, nanoliposomal CPT-11 has shown a more favorable pharmacologic profile and reduced toxicity in multiple preclinical models.
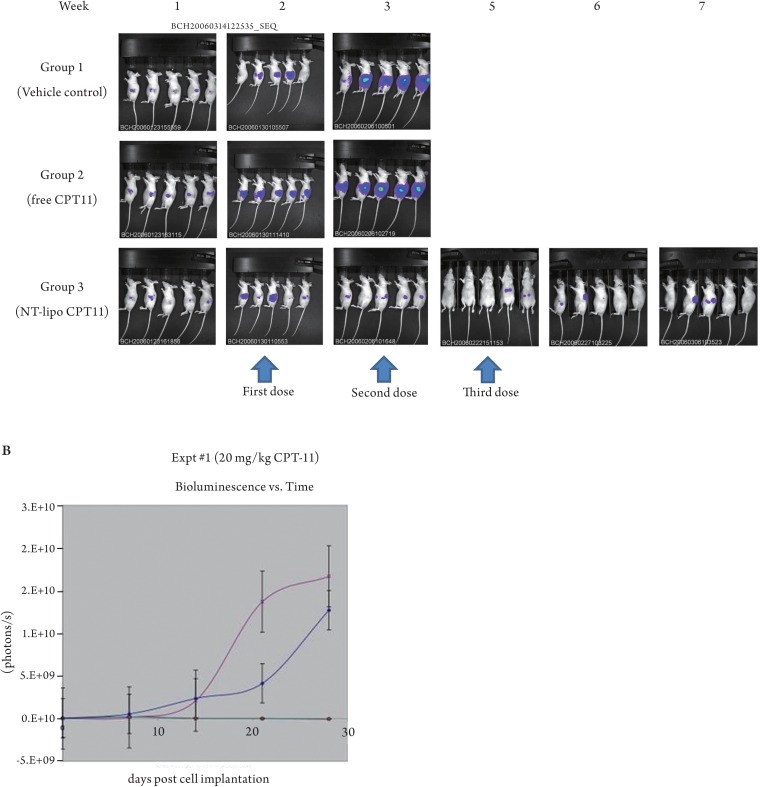
In order to evaluate this novel agent as a potential therapy for pancreatic cancer, a bioluminescence-based orthotopic xenograft model of pancreas cancer was developed (28). COLO357, a human pancreatic cell line, was passaged multiple times in vivo to generate the subline L3.6pl. This cell line was then modified by lentiviral transduction (L3.6pl-T) to express firefly luciferase. L3.6pl-T cells were implanted during open surgery directly into the pancreas of a nude mouse to form an orthotopic tumor xenograft. Therapeutic studies in this model compared nanoliposomal CPT-11 versus free drug at the equivalent dose, along with vehicle control (Figure 1). All treatments were administered intravenously by tail vein beginning at 7 days post-tumor implantation and continued weekly for a total of 3 planned treatments. At 20 mg/kg, free CPT-11 showed some tumor growth inhibition, but all mice required euthanization after 2 doses due to massive tumor progression. In contrast, nanoliposomal CPT-11 at the equivalent 20 mg/kg dose showed potent antitumor activity, including complete tumor inhibition during the entire post-treatment period. Systemic toxicity was not observed with any treatment. These studies indicated that nanoparticle- mediated delivery via nanoliposomal CPT-11 greatly enhances antitumor efficacy in the COLO357/L3.6pI-T orthotopic pancreatic xenograft model.
Figure 1. Nude mice were orthotopically implanted with COLO357/L3.6pI-T xenografts into the pancreas. Following ip administration of luciferin, animals were immediately imaged using a Xenogen IVIS 100 bioluminescence system, and subsequently imaged at weekly intervals. The signal was quantified by defining regions of interest (ROIs) and measuring photons/sec/str. Quantitative BLI values at post implantation day 7 were used to assign mice to treatment groups of five mice per group. Treatments included nanoliposomal CPT-11 at 20 mg/kg, free CPT-11 at 20 mg/kg or vehicle control. All treatments were administered i.v. by tail vein injection beginning at 7 days post- tumor implantation and continued weekly for a total of 3 planned treatments. (A) Bioluminescence images of nude mice on weeks 1-7. (B) BLI values over time. Free CPT-11 treatment (diamonds) produced partial inhibition of tumor growth at initial time points, followed by rapid growth approaching that of the vehicle control group (+). Nanoliposomal CPT-11 treatment (circles) produced complete inhibition of tumor growth at all time points.
In the first-in-human phase I trial, patients with standard therapy-failure solid tumor were enrolled to determine the maximum tolerated dose, safety profile and pharmacokinetics of nanoliposomal CPT-11 (formerly PEP02, PharmaEngine, Inc., Taiwan, and now under the designation of MM-398, Merrimack Pharmaceuticals, Inc, USA). The drug was delivered intravenously for 90 minutes, once every 3 weeks, with starting dose of 60 mg/m2. The maximum tolerated dose was 120 mg/m2. Two patients achieved partial response including cervical cancer in one and pancreatic cancer in one (29). The observation was further extended in a phase I trial for nanoliposomal CPT-11in combination with weekly 24-hour infusion of high-dose 5-FU/LV (HDFL). In the two phase I trials, 7 pancreatic cancer patients who failed gemcitabine/HDFL +/- platinum had received PEP02 with or without HDFL. The best response was partial response in one, stable disease in 4 and progressive disease in 2, which indicated a potential activity of PEP02 in treating gemcitabine-refractory advanced pancreatic cancer. Based on these clinical observations and preclinical results, clinical testing of nanoliposomal CPT-11 was pursued in patients with gemcitabine-based chemotherapy failure advanced pancreatic cancer in an international phase II trial with the target of the primary end-point of 3-month overall survival rate (OS3-month) = 65%. The results have been presented at the 2011 ASCO meeting (30). Of the 40 treated patients, more than three fourths had failed to first-line gemcitabine-based doublet or triplet chemotherapy. Mean cycle of treatment was 5.4 (range, 1 – 26) cycles. The most common G3/4 toxicities were: neutropenia (30%), leucopenia (22.5%), anemia (15%), diarrhea (7.5%), and fatigue (7.5%). Dose modification due to adverse events was required in 10 (25%) patients. The best tumor response rate was partial response in 7.5% and stable disease in 40% (overall disease control rate of 47.5%). The overall survival was 5.2 months with a 3-month and 6-month survival rate of 75% and 42.5%, respectively. The results highlight the feasibility and activity of nanoliposomal CPT-11 in previously heavily treated patients with gemcitabine-refractory advanced pancreatic cancer, which deserves further exploration.
Cationic Liposome Encapsulated Paclitaxel (EndoTAG™-1)
Tumor angiogenesis, the formation of neovasculature from pre-existed peri-tumor vessels, is a crucial process in supporting the development and growth of tumor mass, and the dissemination of tumor metastases. Tumor angiogenesis is mainly triggered by growth factors that are secreted by tumor cells per se and/or by miscellaneous types of cell within the microenvironment, for example, tumor associated macrophages or fibroblasts. Tumor vessels are often dilated and torturous, and characterized by large inter-endothelial cell gap (up to 100 – 600 nm versus < 6 nm in normal vessels), aberrant pericytes and basement membrane coverage, overexpression of specific surface receptor or antigen, and the presence of negative charged macro-molecules for example, anionic phospholipids and glycoprotein. Based on these characters, several strategies have been used to develop neo-vascular targeting liposomal drugs, which include conjugating with specific antibody again surface antigen or receptor and modified, non-functional receptor binding ligand, or incorporating positive (cationic) charged molecules in the surface of liposome. Of them, cationic liposome is a unique and interesting approach (31). In a preclinical study, Kalra and Campbell showed 5-FU and doxorubicin-loaded cationic liposome could preferentially bind with human endothelial (HMEC-1 and HUVEC) rather than pancreatic cancer cells. (HPAF-II and Capan-1)(32). Subsequently, Eichhorn et al showed that both cationic lipid complexed paclitaxel (EndoTAG™-1) and camptothecin (EndoTAG™-2) could preferentially bind at endothelial cells of neo-vasculature in solid tumor preclinical model (33)-(35). The selectively targeting of both agents on tumor microvasculature was confirmed by quantitative fluorescence microscopy. Further study suggested the anti-vascular effect of cationic liposome encapsulated paclitaxel (EndoTAG™-1) is schedule-dependent with metronomic schedule better than the maximum tolerated dose schedule. In addition, the combination of EndoTAG™-1 and gemcitabine could significantly inhibit the incidence of metastatsis in L3.6pl orthotopic pancreatic cancer mice model.
Based on these data, EndoTAG™-1, a cationic liposome (prepared from 1,2 dioleoyl-3-trimethyl- ammonium-propane (DOTAP) and 1,2 dioleoyl-sn-glycero-3- phosphocholine (DOPC)) encapsulated paclitaxel, has been used in combination with gemcitabine to treat chemo-naïve pancreatic cancer patients. The latest follow-up data of the four-arm randomized, phase II trial comparing weekly gemcitabine 1,000 mg/m2 alone versus gemcitabine plus twice weekly EndoTAG™-1 at three different doses, 11, 22 and 44 mg/m2) was presented in the 2009 ASCO Annual Meeting (36). Of the 200 chemo-naïve advanced pancreatic cancer patients who participated the study, 80% had metastatic diseases and 20% had locally advanced diseases. Disease-control rates in the gemcitabine monotherapy arm and the three gemcitabine plus EndoTAG-1 arms was 43% and ranging from 53% to 69%, respectively. The median progression-free survival time in corresponding group of patients were 2.7 months versus 4.1 to 4.6 months, respectively. The median overall survival time of patients receiving gemcitabine plus either high-dose (44 mg/m2) or intermediate-dose of EndoTAG-1 were 9.4 months and 8.7 months, respectively, as compared with the 7.2 months in the gemcitabine monotherapy arm. The adjusted hazard ratio for overall survival for either arm was 0.72 (95% CI, 0.46 to 1.13) and 0.67 (95% CI, 0.43 to 1.07), respectively. The data is exciting but large-scale study to validate the data is mandatory.
Polymeric Micelles
Polymeric micelles-based anticancer drug, consisting of the incorporation of chemotherapeutic agent into polymeric micelles in size of 20–100 nm, was originally developed by Professor Kataoka(37). The polymeric micelle has two major components, a polyethylene glycol (PEG) constituted hydrophilic outer shell and a cytotoxic chemotherapeutic agent incorporated hydrophobic inner core. The main action mechanism of the polymeric micelles is similar to lipomosal agents and through the passive targeting based on the enhanced permeability of tumor neo-vasculature and the impeding clearance of macromolecules from lymphatic-deficient tumor interstitial tissue. Several cytotoxic chemotherapy-incorporating polymeric micellar nanoparticles have been in clinical trials, including paclitaxel-incorporating PEG-polyaspartate (NK105), cisplatin-incorporating PEG-polyglutamate/cisplatin complex (NC-6004) and SN-38-incorporating PEG-ployglutamate/SN-38 (NK012). Of them, NC-6004 is currently evaluated in a phase Ib/II trial for patients with advanced pancreatic cancer, and will be discussed (38)-(41).
Cisplatin-incorporating Polymeric Micelles, NC-6004
In animal study, NC-6004 showed characteristic delayed total body clearance and higher area-under curve as compared with free cisplatin with a ratio of 1/19 and 65 folds, respectively (42). In addition, both histopathological and biochemical studies suggested NC-6004 significantly reduced cisplatin-associated nephrotoxicity. In phase I trial for patients with refractory advanced solid tumor, escalating dose of NC-6004 was administered intravenously every 3 weeks. Despite the implantation of pre-medication and post-therapy hydration, nephrotoxicity and allergic reaction were observed in patients receiving 120 mg/m2 and further dose escalation was withheld. The MTD and the recommended dose were determined as 120 mg/m2 and 90 mg/m2, respectively. Pharmacokinetic study showed the maximum plasma concentration and area under curve of ultra-filterable platinum after 120 mg/m2 of NC-6004 were 1/34 and 8.5 folds of those with free cisplatin (43). Seven out of 17 accruals achieved stable diseases, including two of two pancreatic cancer patients who had NC-6004 at dose level of 90 mg/m2. Perhaps owing to earlier meta-analysis showed he combination of gemcitabine and platinum could significantly improved the overall survival of advanced pancreatic cancer patients as compared to gemcitabine monotherapy, NC-6004 is currently proceeded into a phase Ib/II trial to evaluate the maximum tolerated dose of NC-6004 in combination with gemcitabine and the therapeutic efficacy of the combination in patients with chemo-naïve advanced pancreatic cancer, clinicaltrials.gov identifier NCT00910741.
Rexin-G
Rexin-G is a highly engineered, nonreplicating retroviral vector displaying a von Willebrand factor–derived collagen-binding motif at its amphotropic envelope, and expressing a dominant negative cyclin G1 gene (44)-(46). This Willebrand factor-derived collagen-binding motif on the retrovector's surface enables the nanoparticle drug to seek and be selectively delivered to primary and secondary tumor sites where angiogenesis and collagen matrix exposure characteristically occur. The encoded dominant negative cyclin G1 gene will thus to disrupt tumor cell cyclin G1 activity to lead to the destruction and/or growth inhibition of tumor.
There were two dose escalating phase I trials evaluating different dose/schedule of Rexin-G in patients with gemcitabine-failed advanced pancreatic cancer. The first trial evaluating 3 dose levels of Rexin-G administered intravenously, level I, 7.5 x 109 colony forming units (CFU) per day, days 1-7 and 15-21 every 28 days; level II, 1.1 x 1010 CFU per day, days 1-7 and 15-21 every 28 days; and level III, 3 x 1010 CFU per day, 5 days per week x 4 weeks/cycle with 6 weeks rest between two cycles. A total of 12 patients were enrolled, only one patient with dose-limiting toxicity manifesting as grade 3 transaminitis was observed at dose level II. However, the best tumor response was stable disease in one (8.3%) and the median time to tumor progression and overall survival of intent-to-treat population were 32 days and 3.5 months, respectively (47). In the second trial, the dose of Rexin-G was increased to 1 x 1011 CFU per day, twice or thrice per week for 4 weeks as one cycle (dose levels 0 and I), and 2 x 1011 CFU per day, thrice per week for 4 weeks as one cycle (dose levels II). A total of 13 patients were enrolled, 6 in dose level 0-I and 7 in dose level II. There was no DLT observed. On intent-to –treat analysis, the tumor control rate was 50% (3/6) and 85.7% (6/7 with one partial responder) of patients at dose level 0-I and II, respectively. The median overall survival in corresponding group of patients was 2.6 months and 9.3 months, respectively (48). Based on the results, the US FDA has granted Rexin-G fast-track designation as second-line treatment for pancreatic cancer in June 2009. Currently, a phase II/III pivotal two-arm randomized study aiming to validate the survival benefit of Rexin-G monotherapy versus physician's choice in gemcitabine-refractory pancreatic cancer is under discussion.
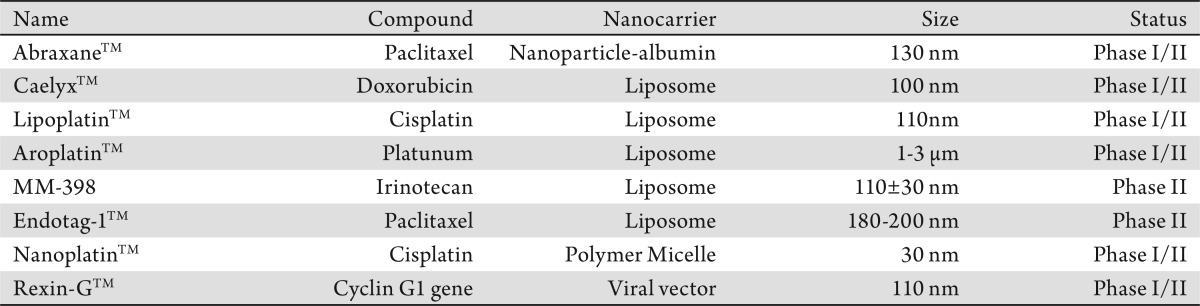
Table 1. Nanovectors in pancreatic cancer treatment.
Conclusion
Systemic therapy for advanced pancreatic cancer has been largely disappointed owing to the unfavorable pharmacokinetic profile and poor penetration of current chemotherapeutic agents and the fragile patient population hard to tolerate toxic combination chemotherapy. Nanovector can provide passive or active targeting drug delivery to reduce the system exposure and enhance local drug retention in tumor tissue. In this review, we provide pre-clinical and clinical evidence to support the potential use of nanovector-based therapy in patients with advanced pancreatic cancer. Unfortunately, most of trials reported here are relatively small and without control group. Prospective, large-scale randomization trials are warranted to confirm their efficacy in this difficult tumor. In addition, the combination of the relatively low toxic nanoparticle drug with conventional cytotoxic agent and/or recently emergent molecular targeted agent should also be investigated to improve the clinical outcomes of patients with advanced pancreatic cancer.
Footnotes
No potential conflict of interest.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Cleary SP, Gryfe R, Guindi M, Greig P, Smith L, Mackenzie R, et al. Prognostic factors in resected pancreatic adenocarcinoma: analysis of actual 5-year survivors. J Am Coll Surg. 2004;198:722–31. doi: 10.1016/j.jamcollsurg.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Atlanta: American Cancer Society; 2010. Society AS: Cancer Facts & Figures 2010. [Google Scholar]
- 4.Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–77. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- 5.Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25:1960–6. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 6.Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817–25. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 7.Kim R. FOLFIRINOX: a new standard treatment for advanced pancreatic cancer? Lancet Oncol. 2011;12:8–9. doi: 10.1016/S1470-2045(10)70237-0. [DOI] [PubMed] [Google Scholar]
- 8.Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol. 2007;2:751–60. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 9.Schnitzer JE. gp60 is an albumin-binding glycoprotein expressed by continuous endothelium involved in albumin transcytosis. Am J Physiol. 1992;262:H246–54. doi: 10.1152/ajpheart.1992.262.1.H246. [DOI] [PubMed] [Google Scholar]
- 10.Gradishar WJ, Tjulandin S, Davidson N, Shaw H, Desai N, Bhar P, et al. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J Clin Oncol. 2005;23:7794–803. doi: 10.1200/JCO.2005.04.937. [DOI] [PubMed] [Google Scholar]
- 11.Schnitzer JE, Oh P. Antibodies to SPARC inhibit albumin binding to SPARC, gp60, and microvascular endothelium. Am J Physiol. 1992;263:H1872–9. doi: 10.1152/ajpheart.1992.263.6.H1872. [DOI] [PubMed] [Google Scholar]
- 12.Ibrahim NK, Desai N, Legha S, Soon-Shiong P, Theriault RL, Rivera E, et al. Phase I and pharmacokinetic study of ABI-007, a Cremophor-free, protein-stabilized, nanoparticle formulation of paclitaxel. Clin Cancer Res. 2002;8:1038–44. [PubMed] [Google Scholar]
- 13.Von Hoff D, Board M, Ramanathan R, Smith L, Drengler R, Wood T, et al. Promising clinical activity of a NAB paclitaxel plus gemcitabine combination in a disease-specific phase I trial in patients with advanced pancreatic cancer[abstract] AACR Annual Meeting. 2008:4179. [Google Scholar]
- 14.Hoff DDV, Ramanathan R, Borad M, Laheru D, Smith L, Wood T, et al. SPARC correlation with response to gemcitabine (G) plus nab-paclitaxel (nab-P) in patients with advanced metastatic pancreatic cancer: A phase I/II study[abstract] J Clin Oncol. 2009;27:4525. [Google Scholar]
- 15.El-Khoueiry AB, Iqbal S, Lenz H, Gitlitz BJ, Yang D, Cole S, et al. A phase I study of two different schedules of nab-paclitaxel (nab-P) with ascending doses of vandetanib (V) with expansion in patients (Pts) with pancreatic cancer (PC)[abstract] J Clin Oncol. 2011;29:4124. [Google Scholar]
- 16.Presant CA, Scolaro M, Kennedy P, Blayney DW, Flanagan B, Lisak J, et al. Liposomal daunorubicin treatment of HIV-associated Kaposi's sarcoma. Lancet. 1993;341:1242–3. doi: 10.1016/0140-6736(93)91147-e. [DOI] [PubMed] [Google Scholar]
- 17.Masood R, Husain SR, Rahman A, Gill P. Potentiation of cytotoxicity of Kaposi's sarcoma related to immunodeficiency syndrome (AIDS) by liposome-encapsulated doxorubicin. AIDS Res Hum Retroviruses. 1993;9:741–6. doi: 10.1089/aid.1993.9.741. [DOI] [PubMed] [Google Scholar]
- 18.Tulpule A, Yung RC, Wernz J, Espina BM, Myers A, Scadden DT, et al. Phase II trial of liposomal daunorubicin in the treatment of AIDS-related pulmonary Kaposi's sarcoma. J Clin Oncol. 1998;16:3369–74. doi: 10.1200/JCO.1998.16.10.3369. [DOI] [PubMed] [Google Scholar]
- 19.Vaage J, Donovan D, Uster P, Working P. Tumour uptake of doxorubicin in polyethylene glycol-coated liposomes and therapeutic effect against a xenografted human pancreatic carcinoma. Br J Cancer. 1997;75:482–6. doi: 10.1038/bjc.1997.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halford S, Yip D, Karapetis CS, Strickland AH, Steger A, Khawaja HT, et al. A phase II study evaluating the tolerability and efficacy of CAELYX (liposomal doxorubicin, Doxil) in the treatment of unresectable pancreatic carcinoma. Ann Oncol. 2001;12:1399–402. doi: 10.1023/a:1012522120294. [DOI] [PubMed] [Google Scholar]
- 21.Hofheinz RD, Willer A, Weisser A, Gnad U, Saussele S, Kreil S, et al. Pegylated liposomal doxorubicin in combination with mitomycin C, infusional 5-fluorouracil and sodium folinic acid. A phase-I-study in patients with upper gastrointestinal cancer. Br J Cancer. 2004;90:1893–7. doi: 10.1038/sj.bjc.6601786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heinemann V, Labianca R, Hinke A, Louvet C. Increased survival using platinum analog combined with gemcitabine as compared to single-agent gemcitabine in advanced pancreatic cancer: pooled analysis of two randomized trials, the GERCOR/GISCAD intergroup study and a German multicenter study. Annals of oncology. 2007;18:1652–9. doi: 10.1093/annonc/mdm283. [DOI] [PubMed] [Google Scholar]
- 23.Boulikas T. Molecular mechanisms of cisplatin and its liposomally encapsulated form, Lipoplatin™. Lipoplatin™ as a chemotherapy and antiangiogenesis drug. Cancer Therapy. 2007;5:351–76. [Google Scholar]
- 24.Stathopoulos GP, Boulikas T, Vougiouka M, Deliconstantinos G, Rigatos S, Darli E, et al. Pharmacokinetics and adverse reactions of a new liposomal cisplatin (Lipoplatin): phase I study. Oncol Rep. 2005;13:589–95. [PubMed] [Google Scholar]
- 25.Stathopoulos GP, Boulikas T, Vougiouka M, Rigatos SK, Stathopoulos JG. Liposomal cisplatin combined with gemcitabine in pretreated advanced pancreatic cancer patients: a phase I-II study. Oncol Rep. 2006;15:1201–4. [PubMed] [Google Scholar]
- 26.Perez-Soler R, Lopez-Berestein G, Lautersztain J, al-Baker S, Francis K, Macias-Kiger D, et al. Phase I clinical and pharmacological study of liposome-entrapped cis-bis-neodecanoato-trans-R,R-1,2-diaminocyclohexane platinum(II) Cancer Res. 1990;50:4254–9. [PubMed] [Google Scholar]
- 27.Drummond DC, Noble CO, Guo Z, Hong K, Park JW, Kirpotin DB. Development of a highly active nanoliposomal irinotecan using a novel intraliposomal stabilization strategy. Cancer Res. 2006;66:3271–7. doi: 10.1158/0008-5472.CAN-05-4007. [DOI] [PubMed] [Google Scholar]
- 28.Hann B, Peth K, Wang D, Gysin S, Li S, Kullberg E, et al. Lipidic nanoparticle CPT-11 in a bioluminescent orthotopic pancreas cancer model[abstract] AACR Meeting Abstracts. 2007:5648. [Google Scholar]
- 29.Chen L, Chang T, Cheng A, Yang C, Shiah H, Chang J, et al. Phase I study of liposome encapsulated irinotecan (PEP02) in advanced solid tumor patients[abstract] J Clin Oncol. 2008;26:2565. [Google Scholar]
- 30.Ko AH, Tempero MA, Shan Y, Su W, Lin Y, Dito E, et al. A multinational phase II study of liposome irinotecan (PEP02) for patients with gemcitabine-refractory metastatic pancreatic cancer. J Clin Oncol. 2011;29:s4. doi: 10.1038/bjc.2013.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmitt-Sody M, Strieth S, Krasnici S, Sauer B, Schulze B, Teifel M, et al. Neovascular targeting therapy: paclitaxel encapsulated in cationic liposomes improves antitumoral efficacy. Clin Cancer Res. 2003;9:2335–41. [PubMed] [Google Scholar]
- 32.Kalra AV, Campbell RB. Development of 5-FU and doxorubicin-loaded cationic liposomes against human pancreatic cancer: Implications for tumor vascular targeting. Pharm Res. 2006;23:2809–17. doi: 10.1007/s11095-006-9113-3. [DOI] [PubMed] [Google Scholar]
- 33.Eichhorn ME, Ischenko I, Luedemann S, Strieth S, Papyan A, Werner A, et al. Vascular targeting by EndoTAG-1 enhances therapeutic efficacy of conventional chemotherapy in lung and pancreatic cancer. Int J Cancer. 2010;126:1235–45. doi: 10.1002/ijc.24846. [DOI] [PubMed] [Google Scholar]
- 34.Eichhorn ME, Luedemann S, Strieth S, Papyan A, Ruhstorfer H, Haas H, et al. Cationic lipid complexed camptothecin (EndoTAG-2) improves antitumoral efficacy by tumor vascular targeting. Cancer Biol Ther. 2007;6:920–9. doi: 10.4161/cbt.6.6.4207. [DOI] [PubMed] [Google Scholar]
- 35.Strieth S, Eichhorn ME, Sauer B, Schulze B, Teifel M, Michaelis U, et al. Neovascular targeting chemotherapy: encapsulation of paclitaxel in cationic liposomes impairs functional tumor microvasculature. Int J Cancer. 2004;110:117–24. doi: 10.1002/ijc.20083. [DOI] [PubMed] [Google Scholar]
- 36.Loehr M, Bodoky G, Fölsch U, Märten A, Karrasch M, Lilla C, et al. Cationic liposomal paclitaxel in combination with gemcitabine in patients with advanced pancreatic cancer: A phase II trial. JCO suppl. 2009:abstr 4526. [Google Scholar]
- 37.Yokoyama M, Okano T, Sakurai Y, Suwa S, Kataoka k. Introduction of cisplatin into polymeric micelle. Journal of Controlled Release. 1996;39:351–356. [Google Scholar]
- 38.Hamaguchi T, Kato K, Yasui H, Morizane C, Ikeda M, Ueno H, et al. A phase I and pharmacokinetic study of NK105, a paclitaxel-incorporating micellar nanoparticle formulation. Br J Cancer. 2007;97:170–6. doi: 10.1038/sj.bjc.6603855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matsumura Y. Preclinical and clinical studies of NK012, an SN-38-incorporating polymeric micelles, which is designed based on EPR effect. Adv Drug Deliv Rev. 2011;63:184–92. doi: 10.1016/j.addr.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 40.Saito Y, Yasunaga M, Kuroda J, Koga Y, Matsumura Y. Enhanced distribution of NK012, a polymeric micelle-encapsulated SN-38, and sustained release of SN-38 within tumors can beat a hypovascular tumor. Cancer Sci. 2008;99:1258–64. doi: 10.1111/j.1349-7006.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saito Y, Yasunaga M, Kuroda J, Koga Y, Matsumura Y. Antitumour activity of NK012, SN-38-incorporating polymeric micelles, in hypovascular orthotopic pancreatic tumour. Eur J Cancer. 2010;46:650–8. doi: 10.1016/j.ejca.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 42.Uchino H, Matsumura Y, Negishi T, Koizumi F, Hayashi T, Honda T, et al. Cisplatin-incorporating polymeric micelles (NC-6004) can reduce nephrotoxicity and neurotoxicity of cisplatin in rats. Br J Cancer. 2005;93:678–87. doi: 10.1038/sj.bjc.6602772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Plummer R, Wilson RH, Calvert H, Boddy AV, Griffin M, Sludden J, et al. A Phase I clinical study of cisplatin-incorporated polymeric micelles (NC-6004) in patients with solid tumours. Br J Cancer. 2011;104:593–8. doi: 10.1038/bjc.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gordon EM, Hall FL. The ‘timely’ development of Rexin-G: first targeted injectable gene vector (review) Int J Oncol. 2009;35:229–38. [PubMed] [Google Scholar]
- 45.Gordon EM, Hall FL. Rexin-G, a targeted genetic medicine for cancer. Expert Opin Biol Ther. 2010;10:819–32. doi: 10.1517/14712598.2010.481666. [DOI] [PubMed] [Google Scholar]
- 46.Gordon EM, Hall FL. Noteworthy clinical case studies in cancer gene therapy: tumor-targeted Rexin-G advances as an efficacious anti-cancer agent. Int J Oncol. 2010;36:1341–53. doi: 10.3892/ijo_00000619. [DOI] [PubMed] [Google Scholar]
- 47.Galanis E, Carlson SK, Foster NR, Lowe V, Quevedo F, McWilliams RR, et al. Phase I trial of a pathotropic retroviral vector expressing a cytocidal cyclin G1 construct (Rexin-G) in patients with advanced pancreatic cancer. Mol Ther. 2008;16:979–84. doi: 10.1038/mt.2008.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chawla SP, Chua VS, Fernandez L, Quon D, Blackwelder WC, Gordon EM, et al. Advanced phase I/II studies of targeted gene delivery in vivo: intravenous Rexin-G for gemcitabine-resistant metastatic pancreatic cancer. Mol Ther. 2010;18:435–41. doi: 10.1038/mt.2009.228. [DOI] [PMC free article] [PubMed] [Google Scholar]