Abstract
In the era of multidetector high quality CT imaging, it is feasible and critical to use objective criteria to define resectable pancreatic cancer. This allows accurate pretreatment staging and the development of stage-specific therapy. Tumors of borderline resectability have emerged as a distinct subset and the definition has been expanded in the last few years. Borderline resectable tumors are defined as those with tumor abutment of <180degrees (< 50%) of the SMA or celiac axis, short segment abutment or encasement of the common hepatic artery typically at the gastroduodenal artery origin, SMV-PV abutment with impingement and narrowing or segmental venous occlusion with sufficient venous flow above and below the occlusion to allow an option for venous reconstruction. Most of the patients whose cancer meet these CT criteria are candidates for preoperative systemic chemotherapy followed by chemoradiation since they are at a high risk for margin positive resection with upfront surgery. Patients whose imaging studies show radiographic stability or regression proceed to pancreaticoduodenectomy (or pancreatectomy) and this may require vascular resection and reconstruction. Prospective biomarker and functional imaging enriched studies are warranted to determine the best overall treatment strategy for these patients.
Keywords: pancreatic cancer, borderline resectable tumors, preoperative therapies
Introduction
Pancreatic cancer presents as a locally advanced or metastatic cancer in most patients and only about 20-25% of patients present with a potentially resectable cancer. Even in these patients, the 5-year survival rate after a successful pancreaticoduodenectomy (PD) or pancreatectomy is approximately 15-20% (1). Patients who undergo a margin positive resection (R2 or R1) do poorly and their survival is similar to those with locally advanced disease (2)-(5). Given the systemic nature of pancreatic adenocarcinoma, and the morbidity involved with surgery, it is essential to clearly determine the resectability status at the time of initial staging evaluation. This is best accomplished by a computerized tomography (CT) scan optimized for pancreatic imaging (6). Based on this high quality CT imaging, pancreatic tumors are classified as resectable, locally advanced or metastatic. Tumors of “borderline resectability” are emerging as a distinct subset of pancreatic tumors and do not easily fit the traditional categories of resectable or locally advanced pancreatic cancers (7),(8). It is important to make this distinction because these presentations tend to confound the results of clinical trials and misguide treating physicians – i.e. in the absence of objective criteria for preoperative staging, some patients with borderline resectable pancreatic cancer will be treated as if they have resectable cancer (with an increased risk of margin positive resection) while others will be treated as having locally advanced disease (and suggest ‘dramatic’ downstaging and operability). These patients are poor candidates for upfront PD given the high rate of margin positive resection and in selected patients; preoperative therapy can achieve an R0 resection surgery.
This helps select appropriate patients for surgery who have the greatest likelihood of a favorable postoperative outcome. This allows the appropriate candidates suited for surgery to proceed with PD. This article reviews the definition of borderline resectable tumors and provides a framework for preoperative therapeutic options of patients with resectable and borderline resectable pancreatic cancers.
Preoperative staging criteria and the changing paradigm
A multidetector computerized tomography (MDCT) with 3-dimensional reconstruction is the best modality to determine local tumor resectability except for its low sensitivity for low-volume hepatic or peritoneal metastases (in∼20% of patients, CT occult metastatic disease is found on laparoscopy or exploration) (9)-(11). Whenever possible, it is helpful to perform a CT scan prior to biliary decompression procedures since post-procedure pancreatitis, if it occurs, may obliterate the vascular planes and preclude accurate assessment of the extent of disease. Endoscopic ultrasound (EUS) has a higher sensitivity compared to a CT scan to detect small tumors and is indicated in selected patients especially those who are candidates for preoperative therapy.
The American Joint Committee on Cancer (AJCC) TNM (Tumor, Nodes, Metastasis) staging for pancreatic cancer was revised in 2002 (6th edition), to reflect the fact local tumor resectability can be determined by high quality CT imaging and these criteria are unchanged in the latest AJCC edition (12). Based on the AJCC criteria, patients with stages 3 and 4 pancreatic adenocarcinoma are considered to have unresectable disease. Criteria for resectability include the absence of tumor extension to the celiac artery (CA) and superior mesenteric artery (SMA), a patent superior mesenteric vein (SMV) and portal vein (PV), and no distant metastases. Locally advanced, surgically unresectable tumors are defined as those that encase the adjacent arteries (celiac axis, SMA, common hepatic artery) or that occlude the SMV, PV, or SMPV confluence. With sophisticated imaging, there is a paradigm shift and a growing category of borderline resectability and the attempt to standardize the definition of borderline resectable pancreatic cancer is work in progress, being modified with time.
Borderline resectable criteria: NCCN, MDACC and AHPBA guidelines
Even though there is some consistency in the AJCC definitions of resectability, these become blurred when describing borderline resectable pancreatic adenocarcinoma. At the University of Texas M.D. Anderson Cancer Center (MDACC), patients with (anatomic) borderline resectable pancreatic cancer were originally defined to include those whose tumors exhibit: short-segment encasement of the hepatic artery which is amenable to resection and reconstruction without evidence of tumor extension to the celiac axis; abutment of the SMA to involve less than or equal to180 degrees of the circumference of the artery; or short-segment occlusion of the SMV, PV, or SMPV confluence with a suitable option for vascular reconstruction due to a normal SMV below, and PV above the area of tumor involvement (7). Since then the criteria have been extended to include additional patients where the surgery could prove to be technically challenging. The American hepato-pancreatico-biliary (AHPBA) association consensus conference on pancreatic cancer (2009) expanded the venous involvement criteria to allow tumor abutment of the SMV/PV with or without impingment and narrowing of the lumen (in addition to venous encasement or short segment occlusion). NCCN has adopted some of these AHPBA guidelines in its most recent version (2.2011) and allows SMV/portal vein abutment with impingment and narrowing of the lumen (13)-(16). The criteria for arterial involvement (SMA and hepatic artery) are clear and similar across the board.
The above definitions describe the anatomic subset of borderline resectability that deal only with tumor-vessel orientation (referred to as type A). Katz and colleagues have described two additional subsets, types B and C, which attempt to define additional criteria for borderline resectability beyond the imaging based principles (17). Most physicians encounter patients with operable pancreatic cancer who are not quite ready for immediate surgery and require extra time off to sort out host or tumor related concerns. Some of these patients have subtle indeterminate subcentimeter liver lesions or peritoneal / omental nodules that are suspicious for metastatic disease they are too small to proceed with a diagnostic FNA- biopsy or additional imaging tests (PET-CT or MRI). These patients fit the MDACC type B definition of borderline resectable pancreatic cancer. Type B patients may have had a technically resectable or a borderline resectable primary tumor as defined on CT images. Another subset of patients is those who have associated medical comorbidities that need time to evaluate or a reversible borderline performance status (typically ECOG 3). Good examples of these presentation is a patient who has a small asymptomatic pulmonary embolism on routine imaging or a patient with a low prealbumin and decline in nutrition and performance status in the presence of obstructive jaundice and cholangitis though progress is noted after biliary decompression and a close eye on nutritional supplementation. This subset constitutes Type C category (and patients in this category may also have had a radiographic potentially resectable or a borderline resectable primary tumor).
Rationale for preoperative therapy in patients with resectable and borderline resectable (types A, B, C) pancreatic cancer
The rationale for delivering preoperative therapy in early pancreatic cancer includes potential for down staging in order to maximize the chances for an R0/R1 resection, using this approach to gauge the cancer's biology and allow appropriate candidates suited for surgery to proceed with PD, treat micrometastatic disease early, and lastly, deliver “adjuvant” therapy in a preoperative setting when it is better tolerated. This has been studied at several institutions in a phase II setting (18)-(22). Our group has completed two gemcitabine based chemoradiation trials in patients with potentially resectable pancreatic cancer (18),(21). In the 176 patients from both trials (Gem-XRT and Gem-Cis-XRT) isolated tumor progression at the time of preoperative restaging was rare with the rate of local tumor progression precluding surgery 0.6% (1 of 176 patients). We have used a similar preoperative strategy for borderline resectable pancreatic cancer with the exception that therpay lasts longer prior to planned PD (the original dataset of 176 patients did not include any patients with MDACC criteria for borderline resectability). Since patients with borderline resectable pancreatic cancer (type A) are at a high risk for margin positive resection and poor survival, these patients are ideal candidates for a prolonged course of preoperative therapy.
Treatment schema
After reviewing the patient's pancreas protocol CT scan in a multidisciplinary conference with radiologists and surgical, medical and radiation oncologists, patients' cancers are categorized as borderline resectable types A, B, C or a combination of these. Most patients are candidates for initial gemcitabine based systemic therapy for 2-4 months. Patients with an ECOG PS of 0-1 are considered for combination chemotherapy, often with gemcitabine and a platinum agent. A restaging CT scan is reviewed after approximately 8 weeks of systemic therapy and patients with radiographic response or a biochemical response in the presence of stable disease are candidates for more systemic therapy followed by chemoradiation or may proceed to chemoradiation. After a break of 4-6 weeks from their radiation therapy, patients who continue to show disease stability or response are candidates for surgery. Gemcitabine or capecitabine are the common radiation sensitizers used in this setting. After a break of 4-6 weeks from their radiation therapy, patients who continue to show disease stability or response are candidates for surgery.
Given the high rate of systemic relapse in patients with resected pancreatic cancer, the “best” systemic therapy available may be applicable in the neoadjuvant setting in selected patients. The recent phase 3 study published by Conroy and colleagues reports on FOLFIRINOX superiority over gemcitabine in the treatment of metastatic pancreatic cancer and has gathered interest (23). 342 patients with a PS of 0 or 1 were randomly assigned to receive FOLFIRINOX or gemcitabine. Six months of chemotherapy were recommended in both groups in patients who had a response. The primary end point was overall survival. The median overall survival was 11.1 months in the FOLFIRINOX group as compared with 6.8 months in the gemcitabine group (hazard ratio for death, 0.57; 95% confidence interval [CI], 0.45 to 0.73; P<0.001). Median progression-free survival was 6.4 months in the FOLFIRINOX group and 3.3 months in the gemcitabine group (P<0.001). The objective response rate was 31.6% in the FOLFIRINOX group versus 9.4% in the gemcitabine group (P<0.001). The authors concluded that FOLFIRINOX is an option for the treatment of patients with metastatic pancreatic cancer and good performance status. There has been some interest from cooperative groups and single institutions to propose FOLFIRINOX based systemic therapy followed by chemoradiation for patients with upfront unresectable (but borderline criteria) pancreatic cancer to potentially maximize their chance of resectability and improve survival after preoperative therapy. Though, it is important to note that beside an excellent PS, >50% of patients in the FOLFIRINOX study had pancreatic tail tumors and the triple drug regimen was not without toxicity (especially in patients with biliary stents/ those prone to cholangitis).
Katz and colleagues have published the largest to date retrospective report of 160 patients with borderline resectable pancreatic cancer (from a prospective database, 1999 -2006) (17). Of these, 125 (78%) received preoperative therapy with mostly chemotherapy followed by chemoradiation and 66 (41%) underwent PD. Twenty seven percent (18 of 66) required vascular resections and in 94% of the patients this was an R0 resection. The median survival was 40 months for patients who underwent preoperative therapy followed by surgery and 13 months for patients who did not undergo PD (p<0.001). Interestingly, the percent change in CA 19-9 over the course of preoperative therapy was associated with overall survival. When compared to patients who had a > 50% decrease in serum CA 19-9, patients with an increase in serum CA 19-9 had a greater than 2-fold risk of death (HR = 2.4, p = 0.02, 95 % CI [1.2, 4.9]). In practice, the radiographic stability (or response), patient's tolerability to therapy and performance status as well as the Ca19-9 trend is factored into making a therapy decision. Prospective data on the role of CA19-9 as a predictive marker is needed before we consider using it as a part of the ‘resectability criteria’ in treated patients.
Understandably, there is an inherent selection bias given that the prolonged course of therapy which selects for better tumor biology, though the role of radiation in this setting needs further evaluation. When our systemic agents and biomarker based techniques to select patients improve, it will provide additional justification for the need for prolonged therapy prior to locoregional options.
Barriers to preoperative therapy for borderline resectable cancer
It is mandatory for patients with resectable or borderline resectable pancreatic cancer to proceed with a cytologic diagnosis of adenocarcinoma (via EUS-guided FNA biopsy) prior to initiating preoperative therapy (16). On rare occasion, this can lead to pancreatitis. In the preoperative therapy setting, when the duration of therapy exceeds 8 weeks, patients with plastic stents are at risk for stent occlusion and cholangitis (especially in the radiation phase). In a clinical trial of 79 patients undergoing chemotherapy with Gemcitabine in combination with Cisplatin followed by Gemcitabine based chemoradiation, at least one stent exchange was necessary in 46 (75%) of the 61 patients who entered the protocol with a plastic biliary stent and self-expandable metal stents which ultimately were placed in 36 (46%) of 79 patients (18),(21).
Biomarker based selection and sequencing of preoperative therapies: Are we there yet?
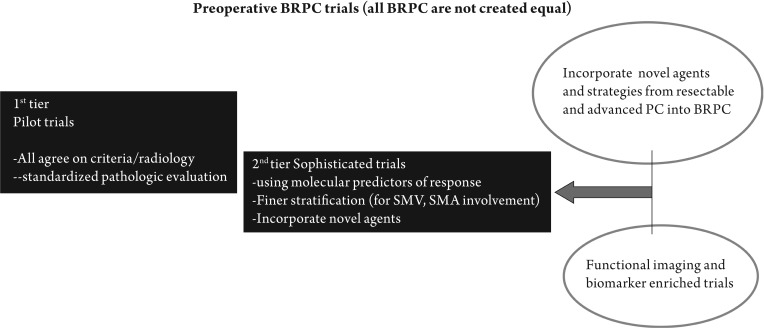
A significant challenge to the management of pancreatic cancer (PC) patients is resistance to a broad range of therapies. There is an emerging consensus that poor intratumoral drug levels may be related to high stromal density, hypoperfusion, and/or drug transport/metabolism within the tumor (24). These factors have been evaluated in animal models but not understood in patients. E.g. gemcitabine, the standard first-line therapy for advanced disease and a drug used in our preoperative management is an incompletely understood drug with little data demonstrating levels of gemcitabine (dFdC) or its active metabolite within human tissue or evaluating factors affecting penetration or lack of activity in many patients. We have some emerging biomarker data, albeit of retrospective nature (from prospective trials) and we need to exploit this information to generate new knowledge and plan elegant next-generation studies (Figure 1). A few of these are discussed below:
Figure 1. Schema for borderline resectable pancreatic cancer trials: looking ahead. BRPC: borderline resectable pancreatic cancer; SMV: superior mesenteric vein; SMA: superior mesenteric artery; PC: pancreatic cancer.
Human equilibrative nucleoside transporter (hENT1) protein
The hNET-1 transports gemcitabine into cells (25),(26). Farrell and colleagues studied the predictive value of hENT1 levels in patients from RTOG9704, a large prospective randomized adjuvant treatment trial comparing gemcitabine to 5-fluorouracil (5FU) as systemic therapy in patients getting 5FU based chemoradiation (27),(28). In this study, 538 patients were assigned randomly, after surgical resection, to either gemcitabine or 5-FU. HENT1 immunohistochemistry was performed on 229 tissue microarrays and scored as having no staining, low staining, or high staining. HENT1 expression was associated with overall survival in a univariate (P = .02) and multivariate model in the gemcitabine arm (P= .004) and hENT1 expression was not associated with survival in the 5FU arm. The authors concluded that this report supports preclinical data and that hENT1 is relevant predictive marker of benefit from gemcitabine in patients with resected pancreatic cancer. Prospective trials in the neoadjuvant and adjuvant setting are warranted to understand its utility as a predictive biomarker.
Gemcitabine single nucleotide polymorphisms
Okazaki and colleagues evaluated 17 single nucleotide polymorphisms (SNPs) of gemcitabine metabolism genes, including CDA, dCK, DCTD, RRM1, hCNT1, hCNT2, hCNT3, and hENT1 genes in 154 patients with potentially resectable pancreatic adenocarcinoma who were enrolled in clinical trials at the UTMDACC from February 1999 to January 2006 (29),(30). Patients received neoadjuvant concurrent gemcitabine and radiation therapy with or without gemcitabine-cisplatin induction therapy. They found that none of the 17 SNPs, individually, had a significant association with OS. A combined genotype effect on OS was observed. Patients carrying 0 to 1 (n = 43), 2 to 3 (n = 77), or 4 to 6 (n = 30) variant alleles had median survival time of 31.5, 21.4, and 17.5 months, respectively. The hazard ratio of dying was 1.71 (95% confidence interval, 1.06-2.76) and 3.16 (95% confidence interval, 1.77-5.63) for patients carrying two to three or four to six at-risk genotypes (P = 0.028 and P < 0.001), respectively, after adjusting for clinical predictors. Four SNPs mainly, CDA C111T, dCK C-1205T, dCK A9846G, and hCNT3 A25G had a significant association with neutropenia toxicity (individually and combined). The authors concluded that these observations suggest that polymorphic variations of drug metabolic genes may be associated with toxicity of gemcitabine-based therapy and OS of patients with resectable pancreatic cancer.
Rapid autopsy based DPC4 data
Recent rapid autopsy data presented by Dr. Iacobuzio-Donahue and colleagues suggest that pancreatic cancers can present with distinct genetic subtypes with different patterns of failure (31). In their study, patients with DPC4 intact tumors were more likely to die of locally destructive disease (30% of patients) and those with DPC4 mutated tumors with a distant widespread metastatic disease (70%). These distinct patterns of failure (locally destructive versus metastatic) were unrelated to clinical stage at presentation, treatment history, and histopathologic features. There is significant interest in understanding if this data holds true in patients being treated (prospectively) and eventually use this information to guide therapy based on sub-groups of patients (locally destructive or wildly metastatic phenotypes). The feasibility of determining DPC4 status on diagnostic cytology specimens was tested recently in patients with locally advanced pancreatic cancer using immunohistochemical staining though patient numbers were small and additional validation studies are warranted (32).
Summary
Preoperative management of pancreatic cancer is an important and evolving field especially with the enlarging definition of borderline resectability. Clearly this effort needs a multidisciplinary working group of surgeons, radiation and medical oncologists, gastroenterologists, radiologists and a pathologist committed to research-driven patient care and is best suited to a high volume center with surgical expertise in vascular resections and interposition grafting. Currently, we lack functional imaging or biomarker based knowledge that can reliably provide data that suggests or predicts response to therapy. This is important going forward since it may have an impact on sequencing of therapies (chemotherapy, chemoradiation) and can help select patients for specific therapies and for surgery.
Footnotes
No potential conflict of interest.
References
- 1.Kuhlmann KF, de Castro SM, Wesseling JG, ten Kate FJ, Offerhaus GJ, Busch OR, et al. Surgical treatment of pancreatic adenocarcinoma; actual survival and prognostic factors in 343 patients. Eur J Cancer. 2004;40:549–58. doi: 10.1016/j.ejca.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 2.Takai S, Satoi S, Toyokawa H, Yanagimoto H, Sugimoto N, Tsuji K, et al. Clinicopathologic evaluation after resection for ductal adenocarcinoma of the pancreas: a retrospective, single-institution experience. Pancreas. 2003;26:243–9. doi: 10.1097/00006676-200304000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Neoptolemos JP, Stocken DD, Dunn JA, Almond J, Beger HG, Pederzoli P, et al. Influence of resection margins on survival for patients with pancreatic cancer treated by adjuvant chemoradiation and/or chemotherapy in the ESPAC-1 randomized controlled trial. Ann Surg. 2001;234:758–68. doi: 10.1097/00000658-200112000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sohn TA, Yeo CJ, Cameron JL, Koniaris L, Kaushal S, Abrams RA, et al. Resected adenocarcinoma of the pancreas-616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg. 2000;4:567–79. doi: 10.1016/s1091-255x(00)80105-5. [DOI] [PubMed] [Google Scholar]
- 5.Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J Gastrointest Surg. 2006;10:1199–210;discussion 1210-1. doi: 10.1016/j.gassur.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Faria SC, Tamm EP, Loyer EM, Szklaruk J, Choi H, Charnsangavej C. Diagnosis and staging of pancreatic tumors. Semin Roentgenol. 2004;39:397–411. doi: 10.1016/j.ro.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 7.Varadhachary GR, Tamm EP, Abbruzzese JL, Xiong HQ, Crane CH, Wang H, et al. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann Surg Oncol. 2006;13:1035–46. doi: 10.1245/ASO.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 8.Brown KM, Siripurapu V, Davidson M, Cohen SJ, Konski A, Watson JC, et al. Chemoradiation followed by chemotherapy before resection for borderline pancreatic adenocarcinoma. Am J Surg. 2008;195:318–21. doi: 10.1016/j.amjsurg.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Tamm E, Charnsangavej C, Szklaruk J. Advanced 3-D imaging for the evaluation of pancreatic cancer with multidetector CT. Int J Gastrointest Cancer. 2001;30:65–71. doi: 10.1385/IJGC:30:1-2:065. [DOI] [PubMed] [Google Scholar]
- 10.Pisters PW, Lee JE, Vauthey JN, Charnsangavej C, Evans DB. Laparoscopy in the staging of pancreatic cancer. Br J Surg. 2001;88:325–37. doi: 10.1046/j.1365-2168.2001.01695.x. [DOI] [PubMed] [Google Scholar]
- 11.Mayo SC, Austin DF, Sheppard BC, Mori M, Shipley DK, Billingsley KG. Evolving preoperative evaluation of patients with pancreatic cancer: does laparoscopy have a role in the current era? J Am Coll Surg. 2009;208:87–95. doi: 10.1016/j.jamcollsurg.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Edge Stephen B., Fritz April G., Byrd David R., editors. AJCC Cancer Staging Handbook seventh edition. New York: Springer-Verlag; 2010. AJCC Cancer staging Manual. [Google Scholar]
- 13.National Comprehensive Cancer Network NCCN practice guidelines for pancreatic cancer, Version 2. 2011. Available online: http://www.nccn.org/professionals/physician_gls/recently_updated.asp.
- 14.Vauthey JN, Dixon E. AHPBA/SSO/SSAT Consensus Conference on Resectable and Borderline Resectable Pancreatic Cancer: rationale and overview of the conference. Ann Surg Oncol. 2009;16:1725–6. doi: 10.1245/s10434-009-0409-5. [DOI] [PubMed] [Google Scholar]
- 15.Abrams RA, Lowy AM, O'Reilly EM, Wolff RA, Picozzi VJ, Pisters PW. Combined modality treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1751–6. doi: 10.1245/s10434-009-0413-9. [DOI] [PubMed] [Google Scholar]
- 16.Callery MP, Chang KJ, Fishman EK, Talamonti MS, William Traverso L, Linehan DC. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1727–33. doi: 10.1245/s10434-009-0408-6. [DOI] [PubMed] [Google Scholar]
- 17.Katz MH, Pisters PW, Evans DB, Sun CC, Lee JE, Fleming JB, et al. Borderline resectable pancreatic cancer: the importance of this emerging stage of disease. J Am Coll Surg. 2008;206:833–46;discussion 846-8. doi: 10.1016/j.jamcollsurg.2007.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans DB, Varadhachary GR, Crane CH, Sun CC, Lee JE, Pisters PW, et al. Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26:3496–502. doi: 10.1200/JCO.2007.15.8634. [DOI] [PubMed] [Google Scholar]
- 19.Pisters PW, Wolff RA, Janjan NA, Cleary KR, Charnsangavej C, Crane CN, et al. Preoperative paclitaxel and concurrent rapid-fractionation radiation for resectable pancreatic adenocarcinoma: toxicities, histologic response rates, and event-free outcome. J Clin Oncol. 2002;20:2537–44. doi: 10.1200/JCO.2002.11.064. [DOI] [PubMed] [Google Scholar]
- 20.Talamonti MS, Small W, Jr, Mulcahy MF, Wayne JD, Attaluri V, Colletti LM, et al. A multi-institutional phase II trial of preoperative full-dose gemcitabine and concurrent radiation for patients with potentially resectable pancreatic carcinoma. Ann Surg Oncol. 2006;13:150–8. doi: 10.1245/ASO.2006.03.039. [DOI] [PubMed] [Google Scholar]
- 21.Varadhachary GR, Wolff RA, Crane CH, Sun CC, Lee JE, Pisters PW, et al. Preoperative gemcitabine and cisplatin followed by gemcitabine-based chemoradiation for resectable adenocarcinoma of the pancreatic head. J Clin Oncol. 2008;26:3487–95. doi: 10.1200/JCO.2007.15.8642. [DOI] [PubMed] [Google Scholar]
- 22.White RR, Tyler DS. Neoadjuvant therapy for pancreatic cancer: the Duke experience. Surg Oncol Clin N Am. 2004;13:675–84,ix-x. doi: 10.1016/j.soc.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 23.Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817–25. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 24.Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457–61. doi: 10.1126/science.1171362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackey JR, Mani RS, Selner M, Mowles D, Young JD, Belt JA, et al. Functional nucleoside transporters are required for gemcitabine influx and manifestation of toxicity in cancer cell lines. Cancer Res. 1998;58:4349–57. [PubMed] [Google Scholar]
- 26.Nakano Y, Tanno S, Koizumi K, Nishikawa T, Nakamura K, Minoguchi M, et al. Gemcitabine chemoresistance and molecular markers associated with gemcitabine transport and metabolism in human pancreatic cancer cells. Br J Cancer. 2007;96:457–63. doi: 10.1038/sj.bjc.6603559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Regine WF, Winter KA, Abrams RA, Safran H, Hoffman JP, Konski A, et al. Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: a randomized controlled trial. Jama. 2008;299:1019–26. doi: 10.1001/jama.299.9.1019. [DOI] [PubMed] [Google Scholar]
- 28.Farrell JJ, Elsaleh H, Garcia M, Lai R, Ammar A, Regine WF, et al. Human equilibrative nucleoside transporter 1 levels predict response to gemcitabine in patients with pancreatic cancer. Gastroenterology. 2009;136:187–95. doi: 10.1053/j.gastro.2008.09.067. [DOI] [PubMed] [Google Scholar]
- 29.Okazaki T, Javle M, Tanaka M, Abbruzzese JL, Li D. Single nucleotide polymorphisms of gemcitabine metabolic genes and pancreatic cancer survival and drug toxicity. Clin Cancer Res. 2010;16:320–9. doi: 10.1158/1078-0432.CCR-09-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka M, Javle M, Dong X, Eng C, Abbruzzese JL, Li D. Gemcitabine metabolic and transporter gene polymorphisms are associated with drug toxicity and efficacy in patients with locally advanced pancreatic cancer. Cancer. 2010;116:5325–35. doi: 10.1002/cncr.25282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iacobuzio-Donahue CA, Fu B, Yachida S, Luo M, Abe H, Henderson CM, et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol. 2009;27:1806–13. doi: 10.1200/JCO.2008.17.7188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crane CH, Varadhachary GR, Yordy JS, Staerkel GA, Javle MM, Safran H, et al. Phase II Trial of Cetuximab, Gemcitabine, and Oxaliplatin Followed by Chemoradiation With Cetuximab for Locally Advanced (T4) Pancreatic Adenocarcinoma: Correlation of Smad4(Dpc4) Immunostaining With Pattern of Disease Progression. J Clin Oncol. 2011 doi: 10.1200/JCO.2010.33.8038. Jun27.[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]