Abstract
The aim was to describe how to avoid technical difficulties during venous femoral cannula insertion for extracorporeal membrane oxygenation (ECMO) in a woman in late pregnancy.
A 28-year old pregnant woman presented at 32 weeks of gestation after developing an acute respiratory distress syndrome (ARDS) of an unknown origin that required venovenous ECMO insertion via the femoral vein. A cannula insertion by the Seldinger visual control technique was impossible in the supine position. A left lateral tilt between 15° and 30° was performed by placing a wedge-shaped cushion under the right hip permitting the cannula insertion. We proposed a systematic 15°–30° left lateral tilt position during the ECMO femoral cannula insertion in late pregnancy cases needing ECMO. This precaution should avoid an injury to the vessels due to multiple insertion attempts.
Keywords: Extracorporeal membrane oxygenation, Acute respiratory distress syndrome, Pregnancy, Aortocaval, compression, Left tilt
INTRODUCTION
Late pregnancy aortocaval compression in the supine position has previously been demonstrated by a cavogram [1]. This feature has been recognized to be minor at least in 50% of the patients. In a small number of cases it leads to a supine hypotensive syndrome [2].
Extracorporeal membrane oxygenation (ECMO) support is instituted for the management of children and adults with life-threatening pulmonary and/or cardiac weakness when other treatment modalities fail [3,4]. Pregnant women may rarely develop acute respiratory distress syndrome (ARDS) and benefit from this kind of management [5]. We report a 28-year old pregnant woman at 32 weeks of gestation who developed ARDS in whom ECMO implantation was a challenge.
TECHNIQUE
A 28-year old pregnant woman (gravida 2, para 1, in the 32nd week of gestation) was admitted to the obstetric unit with a 2-day history of a uterine contraction. During her hospital stay, she developed fever and an acute inflammatory syndrome (Leucocytosis 26.800, CRP 33 mg/dl). Blood and urine cultures were done. Escherichia coli was found to be the germ in the urine cultures. Piperacillin-Tazobactam (4 g every 6 h intravenously) and oseltamivir (75 mg twice daily via an oral gastric tube) were started empirically. On the fourth day, the patient started to have dyspnoea, tachypnoea and respiratory distress. Her blood gases worsened (pH = 7.5, PaO2 = 62, PaCO2 = 27, oxygen saturation = 96% (with oxygen mask 50%); so she was transferred to the intensive care unit. She was in ARDS (severe hypoxaemia, PaO2/FiO2 120 mmHg, the four quadrants showing diffuse alveolar infiltrates on a chest X-ray film) and required immediate intubation. After 24 h of mechanical ventilation, her pulmonary functions continued to deteriorate (Murray Score = 3.5 : PaO2/FiO2 = 60 mmHg, the four quadrants showing diffuse alveolar infiltrates on a chest X-ray film, PEEP 14 mmHg, thoracic compliance 30); so a venovenous ECMO was indicated. As usual the device was placed bedside in a standard sterile fashion. The cannula insertion began with the patient in the supine position. A guide wire was introduced using visual control in the vena cava through the left femoral vein. Then, with the Seldinger technique, we tried to introduce 22F and 21F cannulas, but failed, as they seemed to bump into an obstacle even after dilatation. The same difficulty was found in the right femoral vein. Then we decided to tilt the patient by placing a wedge-shaped cushion under the right hip. In this position, the cannula advanced easily. A long 22F cannula was inserted in the right femoral vein and a 21F short cannula in the left femoral vein; the two were linked by a Y 3/8 joint and connected to the pump. Placing a 19F cannula in the left internal jugular vein under echography control completed the circuit. The system flow rate was 3l/min and after 2 days the patient's condition improved, permitting weaning off the device (arterial blood gases before ECMO removal: Mechanical ventilation with FiO2 = 50%; pH = 7.43, PaO2 = 89 mmHg, PaCO2 = 37 mmHg). No bacterial or viral pathogens were detected in the blood culture, endotracheal aspirates and lavages. A polymerase chain reaction was negative for current viruses including AH1N1 Influenza.
DISCUSSION
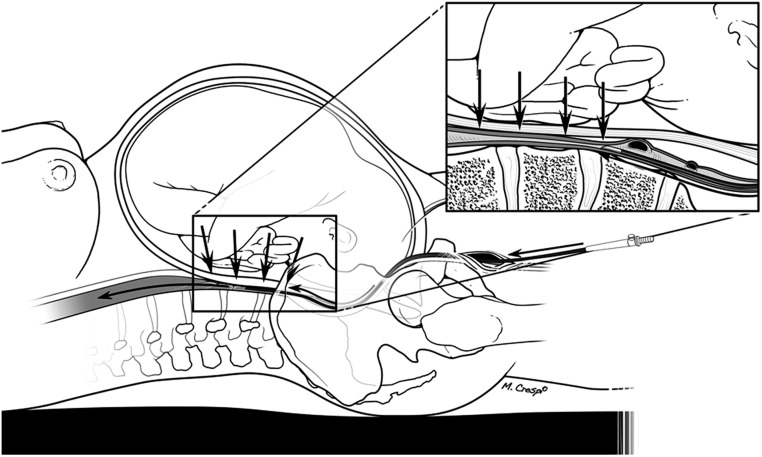
ECMO has become one of the treatments of choice for cardiopulmonary failure [3,4]. Open or percutaneous cannula insertion is codified and can be easily performed through the femoral vessels [6,7]. Our case firstly underlines the possible challenges that are presented by ECMO cannula insertion in a pregnant woman. In fact, during late pregnancy, a situation that is well known to obstetricians and anaesthesiologists, the foetus may compress the vena cava leading to adverse effects such as the reduction of maternal cardiac output and foetal oxygenation. This condition may explain the difficulty faced in advancing a cannula through the guide wire in the vena cava (Fig. 1). Crawford proposed a 15° left lateral tilt to reduce the aortocaval compression during a caesarean section [8]. The left lateral tilt has also been recommended for the same reason in cardiopulmonary resuscitation in pregnant women [9]. Since a pregnant woman may present with a pulmonary or a cardiac failure (or both) and may derive benefit from ECMO implantation, physicians must be aware of the potential technical issues caused by the aortocaval compression. In some institutes, the double-lumen bi-caval cannula (Avalon Elite), which allows single-site cannulation through the internal jugular vein, if present, could be another solution for such a situation [10].
Figure 1:
Vena cava compression avoiding the femoral cannula advancement.
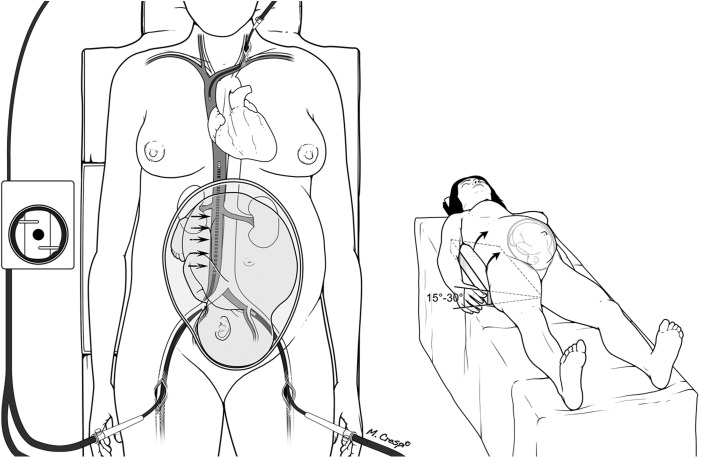
We conclude that it would be better for a pregnant woman to use the left lateral tilt position 15°–30° by the use of a rolled-up blanket, pillow, wedge-shaped cushion, inflatable device or a table tilt during femoral cannula insertion (Fig. 2). This precaution should avoid an injury to the vessels due to multiple insertion attempts. Further studies should be done to ascertain its reliability in mitigating the aforementioned technical difficulty.
Figure 2:
Left lateral tilt by a wedge-shaped cushion and the cannula in place.
Conflict of interest: None declared.
REFERENCES
- 1.Kerr MG, Scott DB, Samuel E. Studies of the inferior vena cava occlusion in late pregnancy. Br Med J. 1964;1:522–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Howard BK, Goodson JH, Mengert WF. Supine hypotensive syndrome in late pregnancy. Obstet Gynecol. 1953;1:371–7. [PubMed] [Google Scholar]
- 3.Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. CESAR trial collaboration. Efficacy and economic assessment of conventional ventilator support versus extracorporeal membrane oxygenation for severe adult respiratory failure: A multicentre randomised controlled trial. Lancet. 2009;374:1351–63. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 4.Combes A, Leprince P, Luyt CE, Bonnet N, Trouillet JL, Léger P, et al. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med. 2008;36:1643–4. doi: 10.1097/CCM.0b013e31816f7cf7. [DOI] [PubMed] [Google Scholar]
- 5.The ANZIC influenza Investigators and Australasian Maternity Outcomes Surveillance System. Critical illness due to 2009 A/H1N1 influenza in pregnant and post partum women: Population based cohort study. BMJ. 2010;340:c1979. doi: 10.1136/bmj.c1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y-S, Ko W-J, Lin F-Y. Insertion of percutaneaous ECMO cannula. Am J Emerg Med. 2000;18:184–5. doi: 10.1016/s0735-6757(00)90015-9. [DOI] [PubMed] [Google Scholar]
- 7.Falcoz P-E, Longrois D. ECMO et SDRA: Cannulation. IRBM. 2010;31:S35–45. [Google Scholar]
- 8.Crawford JS. Principles and Practice of Obstetric Anesthesia. 5th edn. Oxford: Blackell Scientific; 1984. [Google Scholar]
- 9.AHA Guidelines for CPR. Part 10.8: Cardiac arrest associated with pregnancy. Circulation. 2005;112:IV-150–153. [Google Scholar]
- 10.Javidfar J, Brodie D, Ibrahimiye AN, Yang J, Zwischenberger JB, Sonett J, et al. Use of bicaval dual- lumen catheter for adult venovenous extracorporeal membrane oxygenation. Ann Thorac Surg: 2011;91:1763–8. doi: 10.1016/j.athoracsur.2011.03.002. [DOI] [PubMed] [Google Scholar]