Abstract
Acute aortic dissection is very uncommon in pregnant women and the acute type A aortic dissection carries a high mortality rate outside specialized centres. There are a few cases reported with successful outcomes for the mother and the foetus from major cardiac centres. We are reporting our first experience of acute aortic dissection during the third trimester of pregnancy in a patient with Marfan features, profound haemodynamic compromise on arrival and a bovine aortic arch. Both the mother and the baby are doing well two years postoperatively.
Keywords: Aortic dissection, Pregnancy, Bovine arch, Haemodynamic instability
INTRODUCTION
Acute type A aortic dissection during pregnancy is an unusual life-threatening emergency associated with sudden death, which carries a high mortality rate if left untreated. A recent study has found an incidence of 0.4/100 000 persons per year in the female population in the age range of 15 to 45 years in Vienna [1]. The predisposing risk factors for acute aortic dissection during pregnancy include hypertension, previous cardiac surgery, bicuspid aortic valve disease and hereditary collagen disease like Marfan syndrome [2, 3]. We are reporting the case of a pregnant woman with Marfan features and a bovine arch, who was referred to our centre for a type A acute aortic dissection with profound haemodynamic compromise.
CASE REPORT
A 29-year old female with no significant past medical history experienced sudden chest and back pain, in her 29th week of pregnancy. Her mother died at the age of 32 after a ruptured aortic aneurysm. A transthoracic echocardiogram revealed an aortic dissection. She was immediately transferred to our tertiary cardiac centre by helicopter. On arrival at the hospital, she was in shock, and Glasgow coma scale was 13/15. Her peripheral pulses were not palpable; she was taken immediately to the operating room. A cardiotocogram showed a normal foetal heartbeat, despite the profound hypotension of the mother, and no signs of distress in the foetus. A caesarean section was first performed under general anaesthesia. The baby, a girl, weighed 1400 g; the Apgar score was 6 both at 5 min and at 10 min. The baby was intubated immediately after birth because of respiratory distress secondary to the drugs administered to the mother, and transferred to the neonatology unit.
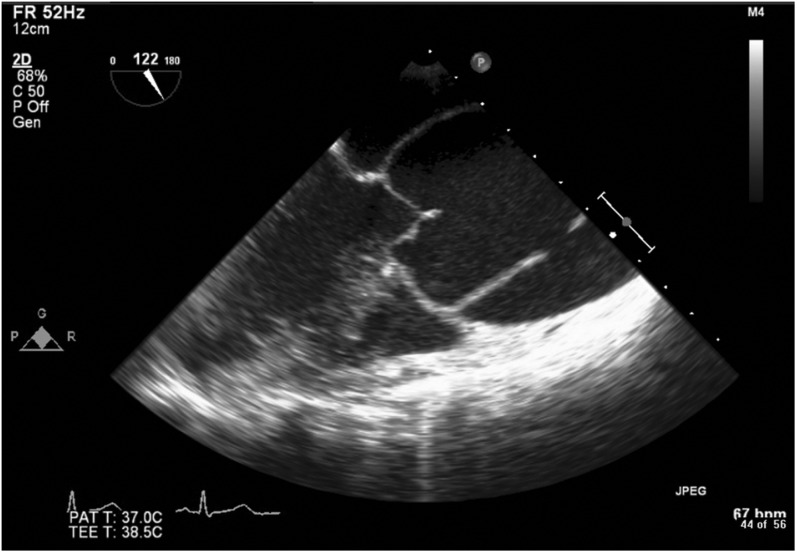
A transoesophageal echocardiogram performed during the cesarean section confirmed the type A aortic dissection from the ascending to the abdominal aorta with an aneurysmal dilatation of the aortic root (Fig. 1). An electrocardiogram performed in the operating room was normal and we proceeded with the cardiopulmonary bypass.
Figure 1:
Cardiac echography showing the aortic dissection. The aortic valve appears normal.
The intraoperative findings were as follows. There was an aortic root dilatation of up to 60 mm, the ascending aorta and the arch appeared to have normal dimensions, and she had a bovine aortic arch. Arterial cannulation was done on the right subclavian artery and venous cannulation via the right atrium. The aorta was opened and we found dissections of the right coronary sinus off the aorta and off the left subclavian artery; the aortic valve was normal. We used a prosthesis graft to replace the proximal aorta; the distal anastomosis was done using the elephant trunk technique; we ligated the left subclavian artery; and the reimplantation of the innominate artery was done using a Dacron patch prosthesis of 8-mm in diameter. The dilated aortic root was replaced by a Valsalva prosthesis, by a David procedure with reimplantation of the left coronary sinus to the graft and a saphenous graft bypass between the graft and the right coronary artery.
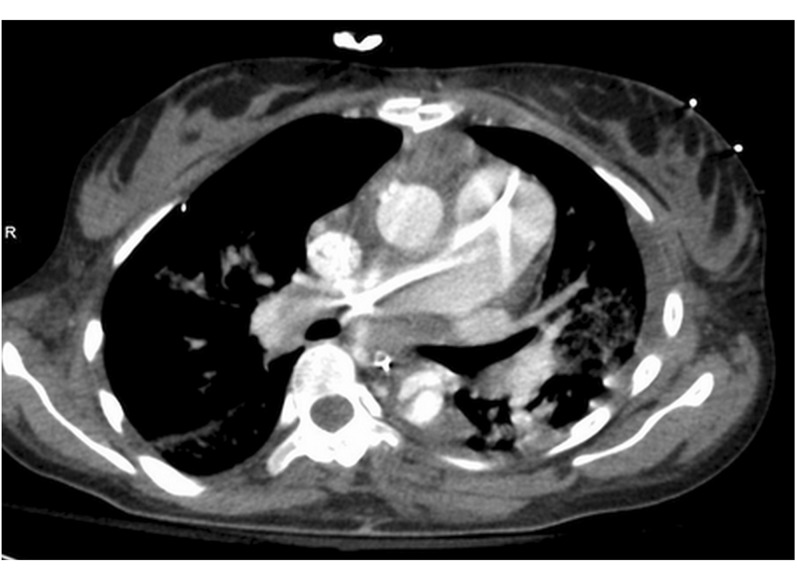
The total bypass time was 253 min, the cross-clamping time was 182 min and the cardiac arrest time with cerebroplegia was 56 min. Postoperatively, the ejection fraction dropped to 30% due to an unknown cause. She was taken back to the operating room three weeks after the surgery and an endoprosthesis was placed to treat a stenosis of the distal end of the elephant trunk (Fig. 2), which acted like an intimal flap with a clinical sign of coarctation. She remained in the intensive care unit for 2 months, and was discharged from the hospital to a revalidation centre where she fully recovered and was discharged home three and a half months after the surgery. The last echocardiogram done one year postoperatively showed an ejection fraction of 70% and near to normal cardiac valve function. The pathological analysis showed a cystic necrosis in the media of the ascending aorta, a feature compatible with Marfan syndrome, but the eye examination was normal.
Figure 2:
Chest CT Scan of the patient 17 days postoperatively showing the tail of the elephant trunk in the lumen of the aorta acting like an intimal flap or a coarctation of the aorta. There was a pressure gradient of 60 mmHg between the upper and the lower limbs. There is a left lower lobe infiltrate and the persistence of the dissection of the descending aorta.
The baby stayed in the hospital until the mother returned home. The mother and her baby are being followed up regularly at the clinics and both are doing very well.
DISCUSSION
This is the first case of a type A acute aortic dissection during pregnancy in our centre. An acute type A aortic dissection during pregnancy is a rare occurrence and most of the few reported cases usually occur during the third trimester of pregnancy. Many of these patients died before reaching a hospital where they could undergo surgery. Our patient was transferred in shock and may not have survived had she been brought to our centre by an ambulance covering a distance of 100 km. The other reason of her survival is the rapid management provided by our multidisciplinary team as reported by others [3]. What is striking is that the long period of profound hypotension in the mother did not have any influence on the foetus, which remained stable until delivery, making us hypothesize that the foetus may be autoregulated by an intrinsic mechanism which sustains it and enables it to resist major stress affecting the mother, as postulated by Pomini et al. [4]. The hypothalamic–pituitary–adrenal axis is essential for maintaining homoeostsis in the foetus [5]. This autoregulation is mediated by the baroreceptor and chemoreceptor reflexes and the cerebral ischaemia, furthermore, the activity of the prostaglandin is an important component of the foetal response to hypotension [6].
One would expect our patient to be aware of the possible risk of ascending aorta abnormalities from prenatal counselling as recommended by the European Society of Cardiology [2, 7, 8]. The Marfan features of the patient had been unknown and unscreened in the family despite the death of her mother at a young age; she also had an unreported bovine aortic arch with aortic dissection in pregnancy. The long-standing postoperative heart failure could be explained by the bypass under hypothermic conditions and also by preoperative shock with the effects of the acidosis and hypoperfusion on the contractility of the myocardium [9].
CONCLUSION
The foetus is stronger than usually thought and may have adaptative measures in the face of intense stress in the mother. A multidisciplinary approach is necessary for the management of these critical patients.
Conflict of interest: none declared.
REFERENCES
- 1.Thalmann M, Sodeck GH, Domanovits H, Grassberger M, Loewe C, Grimm M, et al. Acute Type A aortic dissection and pregnancy: a population-based study. Eur J Cardiothorac Surg. 2011;39:159–63. doi: 10.1016/j.ejcts.2010.12.070. [DOI] [PubMed] [Google Scholar]
- 2.Meijboom LJ, Vos FE, Timmermans J, Boers GH, Zwinderman AH, Mulder BJM. Pregnancy and aortic root growth in the Marfan syndrome: a prospective study. Eur Heart J. 2005;26:914–20. doi: 10.1093/eurheartj/ehi103. [DOI] [PubMed] [Google Scholar]
- 3.Immer FF, Bansi AG, Immer-Bansi AS, McDougall J, Zehr KJ, Schaff HV, et al. Aortic dissection in pregnancy: Analysis of risk factors and outcome. Ann Thorac Surg. 2003;76:309–14. doi: 10.1016/s0003-4975(03)00169-3. [DOI] [PubMed] [Google Scholar]
- 4.Pomini F, Mercogliano D, Cavalletti C, Caruso A, Pomini P. cardiopulmonary bypass in pregnancy. Ann Thorac Surg. 1996;61:259–68. doi: 10.1016/0003-4975(95)00818-7. [DOI] [PubMed] [Google Scholar]
- 5.Ng PC. Effect of stress on the hypothalamic-pituitary-adrenal axis in the fetus and newborn. J Pediatr. 2011;158(2 Suppl):41–3. doi: 10.1016/j.jpeds.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Wood CE, Powers Fraites M, Keller-Wood M. Blockade of PGHS-2 inhibits the hypothalamus-pituitary-adrenal axis response to cerebral hypoperfusion in the sheep fetus. Am J Physiol Regul Integr Comp Physiol. 2009;296:1813–9. doi: 10.1152/ajpregu.90917.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Society of Gynecology; Association for European Paediatric Cardiology; German Society for Gender Medicine; Authors/Task Force Members, Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:3147–97. doi: 10.1093/eurheartj/ehr218. [DOI] [PubMed] [Google Scholar]
- 8.Sakaguchi M, Kitahara H, Seto T, Furusawa T, Fukui D, Yanagiya N, et al. Surgery for acute type A aortic dissection in pregnant patients with Marfan Syndrome. Eur J Cardiothorac Surg. 2005;28:280–5. doi: 10.1016/j.ejcts.2005.02.047. [DOI] [PubMed] [Google Scholar]
- 9.Guo C, Xu D, Wang C. Successful treatment for acute dissection in pregnancy: Bentall Procedure concomitant with cesarean Section. J Cardiothorac Surg. 2011;6:139. doi: 10.1186/1749-8090-6-139. [DOI] [PMC free article] [PubMed] [Google Scholar]